Abstract
Titanium dioxide nanoparticles (NPs-TiO2 or TiO2-NPs) have been employed in many commercial products such as medicines, foods and cosmetics. TiO2-NPs are able to carry antibiotics to target cells enhancing the antimicrobial efficiency; so that these nanoparticles are generally used in antibiotic capsules, like lincomycin, added as a dye. Lincomycin is usually used to treat pregnancy bacterial vaginosis and its combination with TiO2-NPs arises questions on the potential effects on fetus health. This study investigated the potential impact of TiO2-NPs and lincomycin co-exposure on human amniocytes in vitro. Cytotoxicity was evaluated with trypan blue vitality test, while genotoxic damage was performed by Comet Test, Diffusion Assay and RAPD-PCR for 48 and 72 exposure hours. Lincomycin exposure produced no genotoxic effects on amniotic cells, instead, the TiO2-NPs exposure induced genotoxicity. TiO2-NPs and lincomycin co-exposure caused significant increase of DNA fragmentation, apoptosis and DNA damage in amniocytes starting from 48 exposure hours. These results contribute to monitor the use of TiO2-NPs combined with drugs in medical application. The potential impact of antibiotics with TiO2-NPs during pregnancy could be associated with adverse effects on embryo DNA. The use of nanomaterials in drugs formulation should be strictly controlled in order to minimize risks.
Keywords: titanium dioxide nanoparticles, lincomycin, human amniotic cells, in vitro genotoxicity, apoptosis, DNA damage
1. Introduction
The toxicology and safe application of the recently developed nanoparticles (NPs) have raised great interest in the last years. There is a growing demand on the use of these NPs in different industries due to some physicochemical properties: small size, large surface area, redox potential, photocatalytic and quantum properties [1,2,3,4]. NPs can easily be released and enter human body during the use of commercial products. It has emerged that all types of NPs tested are able to cross the placental barrier [5,6,7]. Notably, the pregnant women cannot avoid exposing to them. Several studies have shown toxicity and genotoxicity of a wide range of engineered nanoparticles [8,9,10,11,12,13], consequently this aspect has raised concerns regarding the health of exposed organisms. Among nanomaterials, titanium dioxide nanoparticles (TiO2-NPs) are the most commonly used. TiO2-NPs are applied in medicine as photosensitizer for photodynamic therapy [2,14], drug delivery [15,16] biomedical ceramics [17] and implant biomaterials [18], in foods [19], in cosmetics as sunscreen, toothpaste and personal care products [20,21,22], in sterilization and in paint industry [23,24]. NPs-TiO2 are inert and poorly soluble nanoparticles that can be absorbed by living organisms generally by oral ingestion, this is the main way of absorption as they are used a food additive, in toothpaste, capsules, and various foods [25]. Regarding the extensive application of TiO2-NPs in everyday life, the question arises as to whether this nanoparticle has detrimental effects on human health. Human exposure to TiO2-NPs may also occur through inhalation and ingestion, and then penetrate into the circulatory system and reach other organs (liver, spleen, lungs, brain and testis) [26,27,28]. TiO2-NPs exposure causes ovarian and female reproductive system dysfunction in mice [29]. These nanoparticles, like all types of tested NPs, are able to cross the placental barrier and induce damage [6]. TiO2-NPs prenatal exposure could increase the risk of gestational diabetes, in fact nanoparticles increase maternal fasting blood glucose levels due to gut microbiota alterations [30]. Some studies have also shown that TiO2-NPs can be transferred from pregnant mice to their offspring and affect mice hippocampus by degeneration, necrosis, and the absence of axonal outgrowth of offspring neurons. This suggested that maternal exposure to TiO2-NPs caused learning and memory decline in offspring by decreasing the number of neurons and inhibiting axonal and dendritic outgrowth of hippocampal neurons [31]. Furthermore, the TiO2-NPs induce behavioral deficits related to autism spectrum disorder and neurodevelopmental disorders [32]. The gestational exposure to TiO2-NPs impairs the growth and development of placenta in mice with a mechanism that seems to be involved in vascularization, proliferation and apoptosis pathways [33]. These alterations cause pregnancy complications, fetal growth retardation and adverse birth outcomes [34], associated with embryonic and bone toxicity due to TiO2-NPs accumulation in fetal mice. These effects may be due to the direct or indirect role of TiO2-NPs interfering with Ca, Zn, and other metabolic processes [35]. NPs-TiO2 induce cytotoxicity and reduce mitotic index in human amniotic fluid cells perturbing cells adhesion ability [36]. One of the most worrying characteristics of NPs-TiO2, as for all NPs, is their ability to carry any type of substances to the target cells, thus determining a greater effectiveness of the molecule carried, which does not spread throughout the body, but acts directly on the intended target. At the same time, the transport of a toxic substance could improve its toxicity and/or genotoxicity (“Trojan horse” effect) [13,37,38,39,40]. The substances, potentially carried by NPs, can be environmental pollutants such as heavy metals or even drugs. This effect is also used in medicine to deliver drugs to target organs. In fact, one approach for increasing the antimicrobial efficacy of antibiotics, without raising the overall dose, is to increase the local targeting concentration by conjugating antibiotics with nanoparticles [41,42]. So, the application of nanoparticles has emerged as an option in the control of bacterial infections in many drugs, that present titanium dioxide as a coloring additive of the capsule, such as lincomycin.
Lincomycin and its derivatives (clindamycin) are antibiotics widely used in clinical practice for the treatment of bacterial infections, in particular those caused by anaerobic species. Lincomycin is bacteriostatic, inhibiting protein synthesis in sensitive bacteria (especially Gram-positive and also protozoans), and bactericidal if used at higher concentrations [43]. Lincomycin and clindamycin are usually used in treatment for bacterial vaginosis in pregnancy, where the normal vaginal microbiota is replaced by a mixed anaerobic microbiota. Bacterial vaginosis may be associated with an increased risk of spontaneous preterm delivery and other complications during pregnancy [44,45], and then the treatment is necessary.
Given the importance of maternal and fetus health during pregnancy, investigation on possible effect of TiO2-NPs on amniotic fluid cells will give important information about TiO2-NPs biohazards [36,46]. Therefore, the amniotic cells have been chosen as a model in this study with the aim to assess the effects of titanium dioxide nanoparticles and lincomycin. Lincomycin has been used alone and in combination with TiO2-NPs to demonstrate the ability of nanoparticles to influence the antibiotic action and also to detect the possible “Trojan horse” effect. Cytological effects and genotoxic damage have been evaluated through the trypan blue vitality test, Comet and Diffusion Assay and the RAPD-PCR technique for two exposure times (48 and 72 h).
2. Materials and Methods
2.1. Chemicals
Titanium dioxide nanoparticles (Aeroxide) were supplied by Evonik Degussa (Essen, Germany; Lot. 614061098). Aeroxide has been 99.9% pure certified and is a blend of 75% rutile and 25% anatase forms with a dimensional average of 21 nm. The preparation of the TiO2-NPs stock solution (10.0 mg/L) was performed according to literature data [13,38]. Briefly, TiO2-NPs solution underwent, ultrasonication to disperse nanoparticles and to eliminate agglomeration. Sonication was carried out in medium (Millipore) for 3 h (40 kHz frequency, Dr. Hielscher UP 200S, Germany). UV–Vis spectra were acquired in the range of 200–600 nm by a Shimadzu UV-1700 double beam spectrophotometer. No absorption was detected in the range 300–400 nm, where characteristic peaks for TiO2-NPs nanoparticles aggregates are known to appear [11,13]. Lincomycin (CAS 7179-49-9, 99% purity) was provided from Sigma-Aldrich. This product was provided as delivered and specified by the issuing Pharmacopoeia. All the substances tested were dissolved in DMSO (dimethylsulfoxide, CAS. 67-68-5).
2.2. Chromatographic Analysis
Chromatographic analysis was carried out using an Agilent 1260 Infinity II HPLC system equipped with 1260 Infinity II VL quaternary pump, and 1260 Infinity II DAD WR diode array detector. CDS LC ChemStation OpenLAB Software was used for data acquisition and analysis.
Separation was achieved using Phenomenex Luna Phenyl-Hexyl, 150 × 2 mm i.d. column (3.0 μm particle size) using a gradient of water (A) and acetonitrile (B), both with 0.1% formic acid. Starting with 10% B, a linear gradient was followed to 25% B in 6.0 min, and held at 25% B for other 1.0 min. Finally, starting conditions were restored and the system re-equilibrated for other 1 min. The total analysis time was 8.0 min, the flow rate was 0.3 mL min−1. Injection volume was 5.0 μL.
2.3. Cell Culture and Exposure Procedure
The human amniotic cells were collected from amniotic fluid of pregnant women undergoing prenatal diagnosis for possible chromosomal abnormalities as a routine procedure during the mid-trimester (15–18 weeks of gestation) at Sant’ Anna e San Sebastiano Hospital (Caserta, Italy). Amniotic fluid was collected from pregnant women after written informed consent which was obtained from all participants or their legal guardians, in compliance with the Declaration of Helsinski. Amniotic fluid samples were centrifugate at 1500 rpm for 10 min and suspended into a medium specific for amniocytes growth (Amniomed ® Plus, EuroClone). This medium is a complete medium which contains L-glutamine, FBS, phenol red, sodium bicarbonate, antibiotics and all the necessary growth factors for optimal and selective amniocytes growth. The conditions for the proliferation of amniocyte clones (temperature: 37 °C; pH: between 7.2–7.4; CO2: 5%) onto a plastic culture flask (surface of 25 cm2) are selected according to Ascar and collaborator, 2015 [36]. The obtained primary culture amniotic cell was tripsinized, harvested for metaphase spreads and analysed for prenatal diagnosis. After performing prenatal diagnosis, 32 secondary culture amniotic cell (sub-cultures) were then allowed to expand until clones >50 cells formed reaching the cell confluence. Clones were pooled, centrifuged at 1500 rpm for 10 min and suspended into medium and replated on plastic culture flask. When the sub-cultures reached the confluence, the cells were trypsinized with 1 mL of 1 X trypsin-EDTA (Microgem Cat. L0930-100) and divided in four experimental groups: one flask treated with 10 μg/L of TiO2-NPs, one with 100 mg/L of lincomycin, one with 10 μg/L of TiO2-NPs plus 100 mg/L of lincomycin, and the last one with 20 µl of DMSO as negative control. As a positive control, 10 mM of H2O2 was used. We used a single concentration of TiO2-NPs antibiotic according to our previous genotoxic studies [11,47]. Time exposure were 48 and 72 h. The same cells pool has been used across all assays and experiments. Incubation was performed as described above. All experiments were performed in triplicate.
2.4. Viability Assay
Amniotic cell viability was assessed by blue trypan assay according to literature data [48]. A cell suspension was mixed with 0.4% dye and examined on a slide with optical microscope to discriminate cells that incorporate the dye from cells that exclude it. A viable cell will have a clear cytoplasm whereas a nonviable cell will have a blue cytoplasm.
2.5. Comet Assay
DNA strand breaks in human amniotic cells have been evaluated by Comet assay [49]. The Comet assay provided the trypsinization of cell samples and then centrifugation at 2000 rpm for 5 min, the pellet was re-suspended in 200 μL of physiological solution. So, the amniotic cells have been mix with the Low Melting Point Agarose (0.5%) and were included into Normal Melting Agarose (1%) layers on slides. After overnight incubation in the cold lysis solution (NaCl 2.5 M, Na2EDTA 0.1 M, Tris-Base 0.4 M, TRITON-X100 1%, DMSO 10%, pH 10), the slides were site for 10 min in alkaline buffer (NaOH 10N, EDTA 200 mM, pH 12.1), then were exposed to electrophoresis (25V,300 mA) for 15 min. Finally, the slides were fixed in cold methanol, stained with 30% ethidium bromide and observed by the fluorescence microscope with 60X magnification (Nikon Eclipse E-600). Comet assay was performed in triplicate. The images were acquired by means of the “OpenComet” software [50]. The parameter considered was the percentage of damaged DNA present in the comet tail (% Tail DNA). Highly damaged cells, also known as ghost cells or clouds, have been excluded from analysis because they artifactually increase the apparent DNA fragmentation due to actual genotoxicity. In fact, the ghost cells detected after the treatments were due both to the genotoxic damage and to the apoptosis induced by these substances, so they do not allow to discriminate the two processes [51].
2.6. Diffusion Assay
Diffusion assay protocol is the same as the Comet Assay, but the cell slides do not undergo electrophoresis. This assay showed the apoptotic cells that are characterized by irregular contours with nuclei with highly dispersed DNA. The nuclei of the necrotic cells, on the other hand, are larger and not well defined [52]. Diffusion assay was performed in triplicate. The Diffusion assay slides were scored by subdividing the degree of DNA diffusion pattern in five classes of damage as reported by Cantafora and collaborator in 2014 [53] and we considered only class 5 (apoptotic cell).
2.7. RAPD-PCR Technique
Amniotic cell DNA was isolated from 200 µl of all treated cell suspension using the High pure PCR template preparation Kit (ROCHE Diagnostics) according to the manufacturer’s instructions to guarantee a sufficiently pure extraction to produce a good quality RAPD-PCR profile. The amplification DNA protocol was conducted through primer 6 (5′-d[CCCGTCAGCA]-3′) [54]. The amplification program provides one first step at 94 °C for 2 min, then 1 min at 95 °C, 1 min at 36 °C and 2 min at 72 °C, for 45 cycles. The reaction products were analysed by means of electrophoresis on 1,5% agarose gel and examined after gel staining with 1% ethidium bromide. The RAPD-PCR profiles have polymorphic patterns that allow the calculation of the template genomic stability (GTS%) as follows:
| GTS = (1 − a/n) × 100 |
where a is the average number of polymorphic bands found in each treated sample and n is the total number of bands in the negative control. Appearance of new bands and disappearance of bands are polymorphism detected in RAPD-PCR profiles, which are analysed by comparison to the control sample. The average is calculated for each sample exposed to different molecules. The variations of these values are estimated as a percentage respect to the control set to 100% [13].
2.8. Statistical Analysis
The data were expressed as mean and standard deviation (SD). Differences in the percentage of cell viability, DNA damage and apoptosis genomic stability among the experimental groups were analyzed with the unpaired Student’s t-test using GraphPad Prism 6. Only results with p-value ≤ 0.05 were considered statistically significant.
3. Results
3.1. Characterization and Analytical Determinations
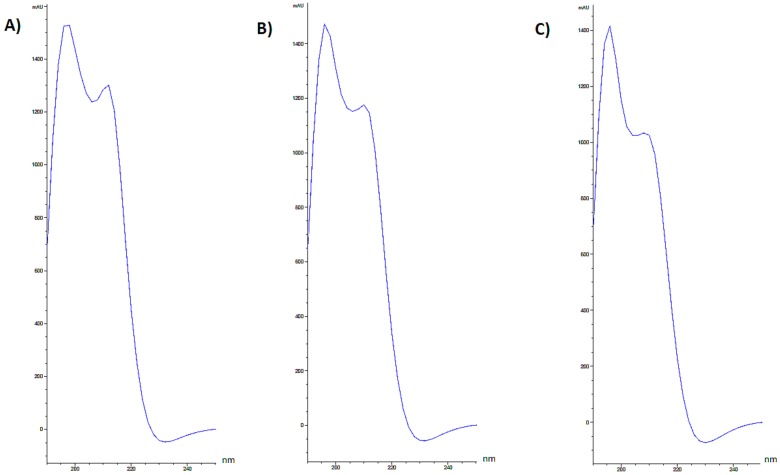
Culture media respectively enriched in lincomycin, TiO2-NPs and TiO2-NPs combined with lincomycin underwent chromatographic separation (Figure 1) and UV spectra for chromatographic peaks were extracted. The spectrum of pure lincomycin showed a weak absorbance, with a maximum at 195 nm.
Figure 1.
Representative chromatograms of lincomycin, TiO2-NPs and TiO2-NPs + −72h.
In order to verify TiO2-NPs and lincomycin interactions, TiO2-NPs absorbance was also acquired in the range 190–250 nm. Two bands were detected, the first one (herein described as Band I) was at 196 nm, whereas the second (Band II) at 240 nm (Figure 2).
Figure 2.
Extracted UV spectra of lincomycin (A), and TiO2-NPs (B) in the range 190–250 nm.
Extracted UV spectra of TiO2-NPs and lincomycin combination showed a hyperchromic effect. In fact, a single peak was detect, with a retention time almost superimposable to that of TiO2-NPs. Indeed, it was observed that a time-dependent increase of TiO2-NPs Band I absorbance (Figure 3).
Figure 3.
Extracted UV spectra of TiO2-NPs + lincomycin in the range 190–250 nm at (A) t = 0h; (B) t = 48h; (C) t = 72h.
3.2. TiO2-NPs Reduces Amniotic Cells Viability
48 and 72 exposure hours to TiO2-NPs statistically significant reduced amniotic cell viability. The exposure to TiO2-NPs plus lincomycin did not induce a statistically significant changes in viability (Figure 4).
Figure 4.
Percentage of alive amniotic cells (ordinate) after 48 h exposure time (A) and after 72 h exposure time (B) to TiO2-NPs, lincomycin and their combination (abscissa). The dark bar is negative control; the white bar is 10 μg/L TiO2-NPs treated cells; the dark grey bar is 100 mg/L lincomycin treated cells; the light grey bar is 10 μg/L TiO2-NPs + 100 mg/L lincomycin treated cells; the striped bar is 10 mM H2O2 treated cells. * p ≤ 0.05.
3.3. TiO2-NPs and Lincomycin Co-Exposure Induces an Increase of Amniocyte DNA Fragmentation
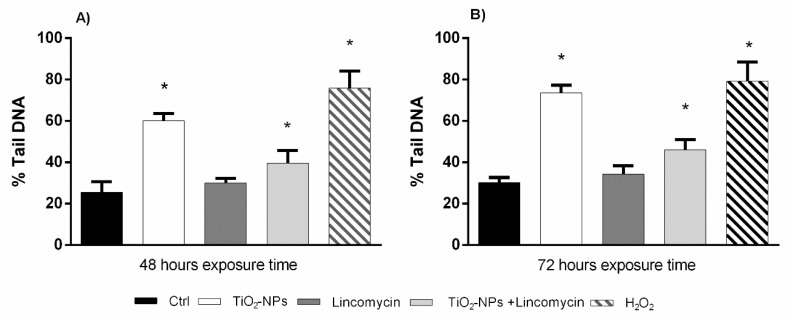
The results from Comet Assay showed a statistically significant increase of cell DNA fragmentation after 48 and 72 h exposure to TiO2 nanoparticles alone and in combination with lincomycin. The exposure to lincomycin did not show statistically significant DNA damage (Figure 5).
Figure 5.
Percentage of DNA in the tail of the comet in amniotic cells (ordinate) after 48 h exposure time (A) and after 72 h exposure time (B) to TiO2-NPs, lincomycin and their combination (abscissa). The dark bar is negative control; the white bar is 10 μg/L TiO2-NPs treated cells; the dark grey bar is 100 mg/L lincomycin treated cells; the light grey bar is 10 μg/L TiO2-NPs + 100 mg/L lincomycin treated cells; the striped bar is 10 mM H2O2 treated cells. * p ≤ 0.05.
3.4. TiO2-NPs in Combination with Lincomycin Cause Amniotic Cells Apoptosis
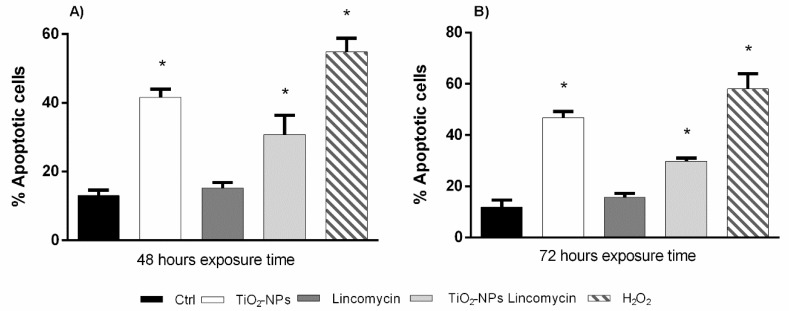
The data from Diffusion assay did not show statistically significant apoptotic damage induced by lincomycin. The exposure to TiO2-NPs and co-exposure to TiO2-NPs and lincomycin after 48 and 72 h induced a statistically significant increase of apoptotic amniotic cells (class 5) with respect to the negative control (Figure 6).
Figure 6.
Percentage of apoptotic cells after (ordinate) after 48 h exposure time (A) and after 72 h exposure time (B) to TiO2-NPs, lincomycin and their combination (abscissa). The dark bar is negative control; the white bar is 10 μg/L TiO2-NPs treated cells; the dark grey bar is 100 mg/L lincomycin treated cells; the light grey bar is 10 μg/L TiO2-NPs + 100 mg/L lincomycin treated cells; the striped bar is 10 mM H2O2 treated cells. * p ≤ 0.05.
3.5. TiO2-NPs and Lincomycin Determines a Change of DNA Polymorphic Profiles
The RAPD-PCR analysis showed a variation of the polymorphic profiles of the amniotic cell DNA exposed to TiO2-NPs and lincomycin after 48 and 72 exposure hours respect to the DNA of the not-treated amniotic cells. 48 h exposure to lincomycin and TiO2-NPs induced the variation of one and two bands respect to control polymorphic profiles respectively. Co-exposure to lincomycin and TiO2-NPs induced the loss of two bands respect to the control. 72 h exposure to lincomycin determined the gain of a band, instead TiO2-NPs treatment caused three bands variation; lincomycin and TiO2-NPs combination showed the variation of two bands (Table 1).
Table 1.
Molecular sizes (bp) of appeared and disappeared bands after amplification with primer P6 in amniotic cell DNA exposed to the TiO2-NPs and lincomycin. *Control bands are at: 200, 300, 320, 400, 500, 520, 700, 950 bp.
| Substances Concentration | Hours of Exposure | Gained Bands * | Lost Bands * |
|---|---|---|---|
| TiO2-NPs 10 µg/L | 48 72 |
850, 530 650 |
- 320, 400 |
| Lincomycin 100 mg/L | 48 72 |
- 650 |
400 - |
| TiO2-NPs 10 µg/L + Lincomycin 100 mg/L |
48 72 |
- 650 |
400, 520 300 |
3.6. TiO2-NPs and Lincomycin Co-Exposure Decreases Amniotic Cells Genomic Stability
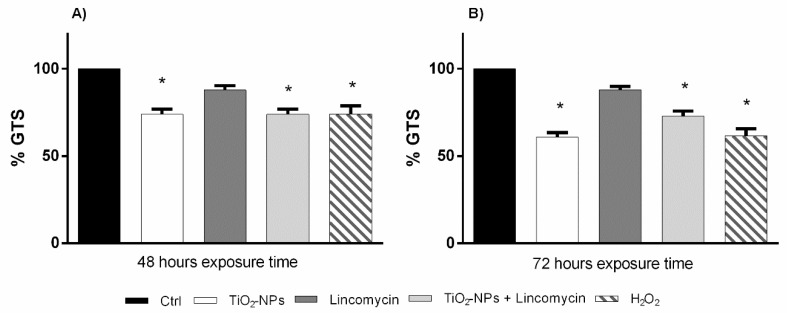
The polymorphic profiles obtained by RAPD-PCR were used to evaluate the percentage of genome stability in human amniotic cells exposed to TiO2-NPs alone and in combination with lincomycin in vitro. 48- and 72 h exposure to TiO2 nanoparticles and co-exposure with lincomycin induced a statistically significant reduction in genomic stability (Figure 7).
Figure 7.
Changes in percentage of Genome Template Stability (ordinate) in amniotic cell DNA after 48 h exposure times (A) and after 72 h exposure time (B) to TiO2-NPs, lincomycin and their combination (abscissa). The dark bar is negative control; the white bar is 10 μg/L TiO2-NPs treated cells; the dark grey bar is 100 mg/L lincomycin treated cells; the light grey bar is 10 μg/L TiO2-NPs + 100 mg/L lincomycin treated cells; the striped bar is 10 mM H2O2 treated cells. * p < 0.05.
4. Discussion
The nanoparticles large-scale application has raised the attention on the possible adverse effects on the exposed organism’s health. Titanium dioxide is among the most used nanoparticles in different industrial sectors. NPs-TiO2 can penetrate in different internal organs through inhalation and ingestion and consequently accumulate inducing DNA damage, ROS production, apoptosis and change in cell cycle and nuclear membranes [55,56,57,58]. TiO2-NPs are able to diffuse through the protective cellular barriers, such as a placental barrier, and may also involve risks to human health. On that regard it is needed an in-depth investigation of their possible toxicological effects. In an ex-vivo human placental perfusion model, Wick and collaborators [59] demonstrated the uptake of nanosized fluorescently labeled polystyrene beads of 50, 80, 240, and 500 nm across the placental barrier. Also, in animal models, the translocation of TiO2-NPs has been reported in brain of prenatally exposed mice. Since the blood barriers are underdeveloped in the fetus, the nanoparticles could easily pass into brain during the early stages of fetal development [60]. In the study conducted by Saquib and collaborators [46], the DLS data revealed the formation of TiO2-NPs aggregates in the RPMI cell culture medium, which were also found to be internalized in the TEM images of the treated human amniotic cell lines. These aggregated NPs, in culture medium, have been reported to enter into cells, such as human amniotic cells, mainly through endocytosis. Their localization in the vacuoles and cell cytoplasm of the exposed cells corresponds well with the observations of Hussain and collaborators [61,62]. In order to safeguard and protect pregnant women and fetus health, the knowledge of the toxic/genotoxic mechanisms of NPs-TiO2 and their association with drugs is very important. The unnecessary supplementation of drugs and commercial products with TiO2-NPs should be restrained during pregnancy until its detrimental effects on embryo development have been clarified. The present work investigated the genotoxic effect of titanium dioxide-NPs and lincomycin on human amniotic fluid cells in vitro. The results show that lincomycin exposure has no toxic/genotoxic effects on amniotic cells; differently, TiO2-NPs exposure induced an increase of DNA strand breaks, a reduction of cells viability, a loss of DNA stability and apoptosis for each time tested (48–72 h). Each type of cell has its own vulnerability to NPs; in fact, the metabolic rate, the antioxidant enzyme machinery and DNA repair capabilities of each cell type responded differently based on the concentration of TiO2-NPs, which induced different toxicity levels. Moreover, several crystalline forms of NP-TiO2 and the aggregation of NPs determined a change in their effects due to the increase in their size. Sadhukha and collaborators [63] showed how particle size is a determining factor in biological functions, demonstrating how well-dispersed nanoparticles induce apoptosis while aggregates show different effects.
In order to protect the cell, we suggest that DNA repair activity would be activated as a consequence of DNA damage in cells exposed to TiO2 nanoparticles. This response could be different related to the exposure time and dosage. The results of this study are in accordance with Boland and collaborators [64] who only investigated the effect of short-term exposure to TiO2-NPs and demonstrated how titanium dioxide nanoparticles are harmful to cell survival by activating an exuberant apoptotic response. The latter, to be activated, it requires the internalization of the TiO2 nanoparticles since the accumulation in lysosomes leads to their rupture and to the release of hydrolases such as cathepsins and intracellular ROS production. The primary mechanism of NPs induced toxicity is due to oxidative stress, resulting in damage to cellular membranes and biological macromolecules [65,66,67,68]. Our results have demonstrated that the TiO2-NPs induced DNA damage in amniocytes at a concentration of 10 μg/L. Thus, the dose comparison of our study with earlier reports [69,70] suggests the induction of oxidative stress in human amniotic derived fluid cells at relatively lesser concentrations of TiO2-NPs. Furthermore, the nanomaterials released in the cytoplasm allow their access to essential biomolecules causing damage. In addition, the nanoparticles can reach the nucleus, in fact, a high fragmentation was also found by Patel and collaborators in 2017 [71]. The authors showed that exposure to ·OH significantly increases damage to the DNA, which was quantified as a moment and as a percentage of DNA in the tail, in peripheral blood lymphocytes. NPs-TiO2 could induce ·OH radicals which are probably responsible for the DNA damage in the exposed cells [72]. There are contradicting results in literature on exposure with different NPs at different stages of embryo development and also with the differences in experimental models [73,74,75]. This raises a concern for pregnant women who could be exposed unconsciously due to the environmental spread of these nanoparticles, in fact, one of the main exposures for the general population is through food consumption products, even from food packaging [76]. This study investigation shows that the co-exposure TiO2-NPs and lincomycin induced genotoxic effects without any cytotoxic one; in fact the co-exposure times affected the cell survival and induced changes in genetic material which do not cause cytotoxic effects. However, this mechanism has not been clarified and needs further investigations. Human amniocyte co-treated with TiO2-NPs and lincomycin showed the increase of DNA fragmentation, induction of apoptotic process and DNA damage. The results of Comet Assay demonstrate that the co-exposure induced a statistically significant increase of DNA strand breaks starting from 48 exposure hour. The data obtained by Diffusion assay highlighted the increase of amniotic cell apoptosis from 48 to 72 exposure hours after TiO2-NPs and lincomycin co-exposure. Similarly, the DNA genomic stability was statistically reduced after the co-exposure.
However, we stress that although co-exposure induces genotoxic effects, the latter are still lower than the exposure to TiO2-NPs alone. The results of this work suggested that the combination of TiO2-NPs and lincomycin cause an intermediate level of genotoxicity to amniocytes compared to the exposure of each single compound which by themselves are quite toxic to these cells. Nevertheless, the combination tested produce less toxicity that the same quantity of NPs probably because the co-exposure could affect the bioavailability of the NPs or their biophysical characteristics (e.g., aggregability). In fact, extracted UV spectra of lincomycin and TiO2-NPs showed that when media with TiO2-NPs combined with lincomycin was injected, in each chromatogram, a single peak was detected and its retention time seemed almost superimposable to that of TiO2-NPs. The observation of this hyperchromic effect, together with the disappearance in the HPLC chromatogram of the peak related to pure lincomycin, allowes us to hypothesize the interactions have been established. Therefore, the results demonstrate that the combination of TiO2-NPs and lincomycin leads to the aggregate formation reducing the genotoxcity compared with the dispersed nanoparticles.
The loss or gain of genotoxicity drugs and/or pollutants carried by titanium dioxide nanoparticles could depend on the molecule carried and media, determining or not the “Trojan horse effect”. However, the experimental evidence on “Trojan horse effect” is conflicting, in fact, it has been demonstrated no interaction of the TiO2-NPs with organic pollutants (CdCl2 and dioxin) in Dicentrarchus labrax in sea water [38,39]. Instead, TiO2-NPs reduced CdCl2-induced effects and DNA damage in Mytilus galloprovincialis, whereas, additive effects were no observed [31]. According to these reports, our results suggest the absence of synergistic effect after co-exposure to TiO2-NPs and lincomycin on human amniotic cells, rather co-exposure reduces the TiO2-NPs genotoxicity. Considering that Trojan horse effect is controversial, it could be hypothesized that these nanoparticles could influence the activity of the lincomycin in such a way that could improve its efficacy and thus lead to dosage reduction.
The exposure to TiO2-NPs during pregnancy should be thoroughly investigated and exposure to NPs must be prevented or minimized. Nevertheless, it must be considered that the behavior of the substances tested is relative to an in vitro system that use a single concentration substances, so, it is necessary to complement the in vitro testing by performing a complete genotoxicity assay on a large range of concentrations and by accurately assessing the level of cytotoxicity; then, by performing methodologies able to display relevant genetic events (mutagenesis, chromosomal aberrations). In this way, a complete in vitro genotoxicity profile will be available. As a result, further studies on other in vivo models could be considered to clarify this aspect, so as to carry out prevention interventions on maternal exposure. The data assume that the genotoxicity studies of NPs must be recommended during a comprehensive assessment of the safety of TiO2-NPs and novel types of NPs and nanomaterials.
Acknowledgments
The authors would like to express their gratitude to Professor Vincenzo Stingo for his valuable advices; his long experience as professor and scientific researcher have been a great help in executing and writing this paper. In addition, we thank Doctor Alessandro Costanzo for his assistance in revising the english of this manuscript.
Author Contributions
F.M. designed the study, acquired and analyzed the data and drafted the manuscript. C.I. carried out Comet and Diffusion Assays. M.S. performed RAPD-PCR experiments. M.L.R. set up cell cultures and different treatments. S.P. performed characterization and analytical determinations. L.C. collected amniotic fluids. L.R. coordinated the study and helped to draft and to revise the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by Valere project, University of Campania “Luigi Vanvitelli”.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Brown S.C., Boyko V., Meyers G., Voetz M., Wohlleben W. Toward advancing nano-object count metrology: A best practice framework. Environ. Health Perspect. 2013;121:1282. doi: 10.1289/ehp.1306957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ackroyd R., Kelty C., Brown N., Reed M. The history of photodetection and photodynamic therapy. Photochem. Photobiol. 2001;74:656–669. doi: 10.1562/0031-8655(2001)074<0656:THOPAP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Colvin V.L. The potential environmental impact of engineered nanomaterials. Nat. Biotechnol. 2003;21:1166. doi: 10.1038/nbt875. [DOI] [PubMed] [Google Scholar]
- 4.Chen X., Mao S.S. Titanium dioxide nanomaterials: Synthesis, properties, modifications, and applications. Chem. Rev. 2007;107:2891–2959. doi: 10.1021/cr0500535. [DOI] [PubMed] [Google Scholar]
- 5.Yin F., Zhu Y., Zhang M., Yu H., Chen W., Qin J. A 3D human placenta-on-a-chip model to probe nanoparticle exposure at the placental barrier. Toxicol. In vitro. 2019;54:105–113. doi: 10.1016/j.tiv.2018.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Muoth C., Aengenheister L., Kucki M., Wick P., Buerki-Thurnherr T. Nanoparticle transport across the placental barrier: Pushing the fiel forward! Nanomedicine. 2016;11:941–957. doi: 10.2217/nnm-2015-0012. [DOI] [PubMed] [Google Scholar]
- 7.Taylor U., Barchanski A., Garrels W., Klein S., Kues W., Barcikowski S., Rath D. Toxicity of gold nanoparticles on somatic and reproductive cells. Adv. Exp. Med. Biol. 2012;733:125–133. doi: 10.1007/978-94-007-2555-3_12. [DOI] [PubMed] [Google Scholar]
- 8.Jorge de Souza T.A., Rosa Souza L.R., Franchi L.P. Silver nanoparticles: An integrated view of green synthesis methods, transformation in the environment, and toxicity. Ecotoxicol. Envron. Saf. 2019;171:691–700. doi: 10.1016/j.ecoenv.2018.12.095. [DOI] [PubMed] [Google Scholar]
- 9.Singh S. Zinc oxide nanoparticles impacts: Cytotoxicity, genotoxicity, developmental toxicity, and neurotoxicity. Toxicol. Mech. Methods. 2019;29:300–311. doi: 10.1080/15376516.2018.1553221. [DOI] [PubMed] [Google Scholar]
- 10.Charles S., Jomini S., Fessard V., Bigorgne-Vizade E., Rousselle C., Michel C. Assessment of the in vitro genotoxicity of TiO2 nanoparticles in a regulatory context. Nanotoxicology. 2018;12:357–374. doi: 10.1080/17435390.2018.1451567. [DOI] [PubMed] [Google Scholar]
- 11.Santonastaso M., Mottola F., Colacurci N., Iovine C., Pacifico S., Cammarota M., Cesaroni F., Rocco L. In vitro genotoxic effects of titanium dioxide nanoparticles (n-TiO2) in human sperm cells. Mol. Reprod. Dev. 2019 doi: 10.1002/mrd.23134. [DOI] [PubMed] [Google Scholar]
- 12.Wang R., Song B., Wu J., Zhang Y., Chen A., Shao L. Potential adverse effects of nanoparticles on the reproductive system. Int. J. Nanomed. 2018;13:8487–8506. doi: 10.2147/IJN.S170723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rocco L., Santonastaso M., Mottola F., Costagliola D., Suero T., Pacifico S., Stingo V. Genotoxicity assessment of TiO2 nanoparticles in the teleost Danio rerio. Ecotoxicol. Environ. Saf. 2015;113:223–230. doi: 10.1016/j.ecoenv.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 14.Ren W., Zeng L., Shen Z., Xiang L., Gong A.N., Zhang J., Mao C., Li A., Paunesku T., Woloschak G.E., et al. Enhanced doxorubicin transport to multidrug resistant breast cancer cells via TiO2 nanocarriers. RSC Adv. 2013;3:20855–20861. doi: 10.1039/c3ra42863j. [DOI] [Google Scholar]
- 15.Ortiz-Benítez E.A., Velázquez-Guadarrama N., Durán Figueroa N.V., Quezada H., Olivares-Trejo J.J. Antibacterial mechanism of gold nanoparticles on Streptococcus pneumoniae. Metallomics. 2019 doi: 10.1039/C9MT00084D. [DOI] [PubMed] [Google Scholar]
- 16.Du Y., Ren W., Li Y., Zhang Q., Zeng L., Chi C., Wu A., Tian J. The enhanced chemotherapeutic effects of doxorubicin loaded PEG coated TiO2 nanocarriers in an orthotopic breast tumor bearing mouse model. J. Mater. Chem. B. 2015;3:1518–1528. doi: 10.1039/C4TB01781A. [DOI] [PubMed] [Google Scholar]
- 17.Haugen H.J., Will J.C.O., Koehler A.G., Hopfner U., Aigner J., Wintermantel E. Ceramic TiO2-foams: Characterisation of a potential scaffold. J. Eur. Ceram. Soc. 2004;24:661–666. doi: 10.1016/S0955-2219(03)00255-3. [DOI] [Google Scholar]
- 18.Cui C., Liu H., Li Y., Sun J., Wanga R.U., Liu S.A., Greer L. Fabrication and biocompatibility of nano-TiO2/titanium alloys biomaterials. Mater. Lett. 2005;59:3144–3148. doi: 10.1016/j.matlet.2005.05.037. [DOI] [Google Scholar]
- 19.Peters R.J., Bemmel V.G., Herrera-Rivera Z., Helsper H.P., Marvin H.J., Weigel S., Tromp P.C., Oomen A.G., Rietveld A.G., Bouwmeester H. Characterization of titanium dioxide nanoparticles in food products: Analytical methods to define nanoparticles. J. Agric. Food Chem. 2014;62:6285–6293. doi: 10.1021/jf5011885. [DOI] [PubMed] [Google Scholar]
- 20.Lorenz C., Tiede K., Tear S., Boxall A., Von Goetz N., Hungerbühler K. Imaging and characterization of engineered nanoparticles in sunscreens by electron microscopy, under wet and dry conditions. Int. J. Occup. Environ. Health. 2010;16:406–428. doi: 10.1179/oeh.2010.16.4.406. [DOI] [PubMed] [Google Scholar]
- 21.Contado C., Pagnoni A. TiO2 nano-and micro-particles in commercial foundation creams: Field flow-fractionation techniques together with ICP-AES and SQW voltammetry for their characterization. Anal. Methods. 2010;2:1112–1124. doi: 10.1039/c0ay00205d. [DOI] [Google Scholar]
- 22.Weir A., Westerhoff P., Fabricius L., Hristovski K., von Goetz N. Titanium dioxide nanoparticles in food and personal care products. Environ. Sci. Technol. 2012;46:2242–2250. doi: 10.1021/es204168d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mahmoud W.M., Rastogi T., Kümmerer K. Application of titanium dioxide nanoparticles as a photocatalyst for the removal of micropollutants such as pharmaceuticals from water. Curr. Opin. Green Sustain. Chem. 2017;6:1–10. doi: 10.1016/j.cogsc.2017.04.001. [DOI] [Google Scholar]
- 24.Rezaei B., Mosaddeghi H. Applications of titanium dioxide nanoparticles; Proceedings of the Nano-Technology in Environments Conference, Isfahan University of Technology; Isfahan, Iran. 19–20 May 2009. [Google Scholar]
- 25.Shi H., Magaye R., Castranova V., Zhao J. Titanium dioxide nanoparticles: A review of current toxicological data. Part Fibre Toxicol. 2013;15:15. doi: 10.1186/1743-8977-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shakeel M., Jabeen F., Shabbir S., Asghar M.S., Khan M.S., Chaudhry A.S. Toxicity of nano-titanium dioxide (TiO2-NP) through various routes of exposure: A review. Biol. Trace Elem. Res. 2016;172:1–36. doi: 10.1007/s12011-015-0550-x. [DOI] [PubMed] [Google Scholar]
- 27.Elgrabli D., Beaudouin R., Jbilou N., Floriani M., Pery A., Rogerieux F., Lacroix G. Biodistribution and clearance of TiO2 nanoparticles in rats after intravenous injection. PLoS ONE. 2015;10:e012449. doi: 10.1371/journal.pone.0124490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Disdier C., Devoy J., Cosnefroy A., Chalansonnet M., Herlin-Boime N., Brun E., Lund A., Mabondzo A. Tissue biodistribution of intravenously administrated titanium dioxide nanoparticles revealed blood-brain barrier clearance and brain inflammation in rat. Part Fibre Toxicol. 2015;12:27. doi: 10.1186/s12989-015-0102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gao G., Ze Y., Li B., Zhao X., Zhang T., Sheng L., Hu R., Gui S., Sang X., Sun Q., et al. Ovarian dysfunction and gene-expressed characteristics of female mice caused by long-term exposure to titanium dioxide nanoparticles. J. Hazard Mater. 2012;243:19–27. doi: 10.1016/j.jhazmat.2012.08.049. [DOI] [PubMed] [Google Scholar]
- 30.Mao Z., Li Y., Dong T., Zhang L., Zhang Y., Li S., Hu H., Sun C., Xia Y. Exposure to titanium dioxide nanoparticles during pregnancy changed maternal gut microbiota and increased blood glucose of rat. Nanoscale Res. Lett. 2019;14:26. doi: 10.1186/s11671-018-2834-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou Y., Ji J., Chen C., Hong F. Retardation of axonal and dendritic outgrowth is associated with the MAPK signaling pathway in offspring mice following maternal exposure to nanosized titanium dioxide. Agric. Food Chem. 2019;67:2709–2715. doi: 10.1021/acs.jafc.8b06992. [DOI] [PubMed] [Google Scholar]
- 32.Notter T., Aengenheister L., Weber-Stadlbauer U., Naegeli H., Wick P., Meyer U., Buerki-Thurnherr T. Prenatal exposure to TiO2 nanoparticles in mice causes behavioral deficits with relevance to autism spectrum disorder and beyond. Transl. Psychiatr. 2018;8:193. doi: 10.1038/s41398-018-0251-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang L., Xie X., Zhou Y., Yu D., Deng Y., Ouyang J., Yang B., Luo D., Zhang D., Kuang H. Gestational exposure to titanium dioxide nanoparticles impairs the placentation through dysregulation of vascularization, proliferation and apoptosis in mice. Int. J. Nanomed. 2018;13:777–789. doi: 10.2147/IJN.S152400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yamashita K., Yoshioka Y., Higashisaka K., Mimura K., Morishita Y., Nozaki M., Yoshida T., Ogura T., Nabeshi H., Nagano K., et al. Silica and titanium dioxide nanoparticles cause pregnancy complications in mice. Nat. Nanotechnol. 2011;6:321–328. doi: 10.1038/nnano.2011.41. [DOI] [PubMed] [Google Scholar]
- 35.Hong F., Zhou Y., Zhao X., Sheng L., Wang L. Maternal exposure to nanosized titanium dioxide suppresses embryonic development in mice. Int. J. Nanomed. 2017;12:6197–6204. doi: 10.2147/IJN.S143598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ascar M.S., Bulut Z.B., Ateş A., Nami B., Koçak N., Yıldız B. Titanium dioxide nanoparticles induce cytotoxicity and reduce mitotic index in human amniotic fluid-derived cells. Hum. Exp. Toxicol. 2015;34:74–82. doi: 10.1177/0960327114530742. [DOI] [PubMed] [Google Scholar]
- 37.Nowack B., Bucheli T.D. Occurrence behavior and effects of nanoparticles in the environment. Environ. Pollut. 2007;150:5–22. doi: 10.1016/j.envpol.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 38.Nigro M., Bernardeschi M., Costagliola D., Della Torre C., Frenzilli G., Guidi P., Lucchesi P., Mottola F., Santonastaso M., Scarcelli V., et al. n-TiO2 and CdCl2 co-exposure to titanium dioxide nanoparticles and cadmium: Genomic, DNA and chromosomal damage evaluation in the marine fish European sea bass (Dicentrarchus labrax) Aquat. Toxicol. 2015;168:72–77. doi: 10.1016/j.aquatox.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 39.Della Torre C., Buonocore F., Frenzilli G., Corsolini S., Brunelli A., Guidi P., Kocan A., Mariottini M., Mottola F., Nigro M., et al. Influence of titanium dioxide nanoparticles on 2,3,7,8-tetrachlorodibenzo-p-dioxin bioconcentration and toxicity in the marine fish European sea bass (Dicentrarchus labrax) Environ. Pollut. 2015;196:185–193. doi: 10.1016/j.envpol.2014.09.020. [DOI] [PubMed] [Google Scholar]
- 40.Canesi L., Frenzilli G., Balbi T., Bernardeschi M., Ciacci C., Corsolini S., Della Torre C., Fabbri R., Faleri C., Focardi S., et al. Interactive effects of n-TiO2 and 2,3,7,8-TCDD on the marine bivalve Mytilus galloprovincialis. Aquat. Toxicol. 2014;153:53–65. doi: 10.1016/j.aquatox.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 41.Hussain S., Joo J., Kang J., Kim B., Braun G.B., She Z.G., Kim D., Mann A.P., Mölder T., Teesalu T., et al. Antibiotic-loaded nanoparticles targeted to the site of infection enhance antibacterial efficacy. Nat. Biomed. Eng. 2018;2:95–103. doi: 10.1038/s41551-017-0187-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen Y.H., Li T.J., Tsai B.Y., Chen L.K., Lai Y.H., Li M.J., Tsai C.Y., Tsai P.J., Shieh D.B. Vancomycin-loaded nanoparticles enhance sporicidal and antibacterial efficacy for clostridium difficile Infection. Front Microbiol. 2019;10:1141. doi: 10.3389/fmicb.2019.01141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spížek J., Řezanka T. Lincosamides: Chemical structure, biosynthesis, mechanism of action, resistance, and applications. Biochem. Pharm. 2017;133:20–28. doi: 10.1016/j.bcp.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 44.Haahr T., Ersbøll A.S., Karlsen M.A., Svare J., Sneider K., Hee L., Weile L.K., Ziobrowska-Bech A., Østergaard C., Jensen J.S., et al. Treatment of bacterial vaginosis in pregnancy in order to reduce the risk of spontaneous preterm delivery - a clinical recommendation. Acta Obs. Gynecol. Scand. 2016;95:850–860. doi: 10.1111/aogs.12933. [DOI] [PubMed] [Google Scholar]
- 45.Lamont R.F., Nhan-Chang C.L., Sobel J.D., Workowski K., Conde-Agudelo A., Romero R. Treatment of abnormal vaginal flora in early pregnancy with clindamycin for the prevention of spontaneous preterm birth: A systematic review and metaanalysis. Am. J. Obs. Gynecol. 2011;205:177–190. doi: 10.1016/j.ajog.2011.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Saquib Q., Al-Khedhairy A.A., Siddiqui M.A., Abou-Tarboush F.M., Azam A., Musarrat J. Titanium dioxide nanoparticles induced cytotoxicity, oxidative stress and DNA damage in human amnion epithelial (WISH) cells. Toxicol. In vitro. 2012;26:351–361. doi: 10.1016/j.tiv.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 47.Rocco L., Peluso C., Stingo V. Micronucleus test and comet assay for the evaluation of zebrafish genomic damage induced by erythromycin and lincomycin. Environ. Toxicol. 2012;27:598–604. doi: 10.1002/tox.20685. [DOI] [PubMed] [Google Scholar]
- 48.Strober W. Trypan blue exclusion test of cell viability. Curr. Protoc. Immunol. 2001;21:A.3B.1-A.3B.2.. doi: 10.1002/0471142735. [DOI] [PubMed] [Google Scholar]
- 49.Frenzilli G., Nigro M., Lyons B.P. The comet assay for the evaluation of genotoxic impact in aquatic environments. Mutat. Res. Rev. 2009;681:80–89. doi: 10.1016/j.mrrev.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 50.Gyori B.M., Venkatachalam G., Thiagarajan P.S., Hsu D., Clement M.V. OpenComet: An automated tool for comet assay image analysis. Redox Biol. 2014;2:457–465. doi: 10.1016/j.redox.2013.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Meintières S., Nesslany F., Pallardy M., Marzin D. Detection of ghost cells in the standard alkaline comet assay is not a good measure of apoptosis. Environ. Mol. Mutagen. 2003;41:260–269. doi: 10.1002/em.10156. [DOI] [PubMed] [Google Scholar]
- 52.Singh N.P. A simple method for accurate estimation of apoptotic cells. Exp. Cell Res. 2000;256:328–337. doi: 10.1006/excr.2000.4810. [DOI] [PubMed] [Google Scholar]
- 53.Cantafora E., Sean Giorgi F., Frenzilli G., Scarcelli V., Busceti C.L., Nigro M., Bernardeschi M., Fornai F. Region-specific DNA alterations in focally induced seizures. J. Neural. Transm. 2014;121:1399–1403. doi: 10.1007/s00702-014-1211-5. [DOI] [PubMed] [Google Scholar]
- 54.Rocco L., Valentino I.V., Scapigliati G., Stingo V. RAPD-PCR analysis for molecular characterization and genotoxic studies of a new marine fish cell line derived from Dicentrarchus labrax. Cytotechnology. 2014;66:383–393. doi: 10.1007/s10616-013-9586-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jugan M.L., Barillet S., Simon-Deckers A., Herlin-Boime N., Sauvaigo S., Douki T., Carriere M. Titanium dioxide nanoparticles exhibit genotoxicity and impair DNA repair activity in A549 cells. Nanotoxicology. 2012;6:501–513. doi: 10.3109/17435390.2011.587903. [DOI] [PubMed] [Google Scholar]
- 56.Valdiglesias V., Costa C., Sharma V., Kilic G., Pásaro E., Teixeira J.P., Dhawan A., Laffon B. Comparative study on effects of two different types of titanium dioxide nanoparticles on human neuronal cells. Food Chem. Toxicol. 2013;57:352–361. doi: 10.1016/j.fct.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 57.Hu R., Zheng L., Zhang T., Gao G., Cui Y., Cheng Z., Cheng J., Hong M., Tang M., Hong F. Molecular mechanism of hippocampal apoptosis of mice following exposure to titanium dioxide nanoparticles. J. Hazard Mater. 2011;191:32–40. doi: 10.1016/j.jhazmat.2011.04.027. [DOI] [PubMed] [Google Scholar]
- 58.Petković J., Žegura B., Stevanović M. DNA damage and alteration in expression of DNA damage responsive genes induced by TiO2 nanoparticles in human hepatoma HepG2 cells. Nanotoxicology. 2011;5:341–353. doi: 10.3109/17435390.2010.507316. [DOI] [PubMed] [Google Scholar]
- 59.Baranowska-Wójcik E., Szwajgier D., Oleszczuk P., Winiarska-Mieczan A. Effects of titanium dioxide nanoparticles exposure on human health—A review. Biol. Trace Elem. Res. 2019 doi: 10.1007/s12011-019-01706-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wick P., Malek A., Manser P., Meili D., Maeder-Althaus X., Diener L., Diener P.A., Zisch A., Krug H.F., Mandach U.V. Barrier capacity of human placenta for nanosized materials. Environ. Health Perspect. 2010;118:432–436. doi: 10.1289/ehp.0901200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Takeda K., Suzuki K.I., Ishihara A., Kubo-Irie M., Fujimoto R., Tabata M., Oshio S., Nihei Y., Ihara T., Sugamata M. Nanoparticles transferred from pregnant mice to their offspring can damage the genital and cranial nerve systems. J. Health Sci. 2009;55:95–102. doi: 10.1248/jhs.55.95. [DOI] [Google Scholar]
- 62.Hussain S., Boland S., Baeza-Squiban A., Hamel R., Thomassen L.C., Martens J.A., Billon-Galland M.A., Fleury-Feith J., Moisan F., Pairon J.C., et al. Oxidative stress and proinflammatory effects of carbon black and titanium dioxide nanoparticles: Role of particle surface area and internalized amount. Toxicology. 2009;260:142–149. doi: 10.1016/j.tox.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 63.Hussain S., Thomassen L.C.J., Ferecatu I., Borot M.C., Andreau K., Martens J.A., Fleury J., Baeza-Squiban A., Marano F., Boland S. Carbon black and titanium dioxide nanoparticles elicit distinct apoptotic pathways in bronchial epithelial cells. Part. Fiber Toxicol. 2010;7:10. doi: 10.1186/1743-8977-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sadhukha T., Wiedmann T.S., Panyama J. Enhancing therapeutic efficacy through designed aggregation of nanoparticles. Biomaterials. 2014;35:7860–7869. doi: 10.1016/j.biomaterials.2014.05.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Boland S., Hussain S., Baeza-Squiban A. Carbon black and titanium dioxide nanoparticles Induce distinct molecular mechanisms of toxicity. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2014;6:641–652. doi: 10.1002/wnan.1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dalton S., Janes P.A., Jones N.G., Nicholson J.A., Hallam K.R., Allen G.C. Photocatalytic oxidation of NOx gases using TiO2: A surface spectroscopic approach. Environ. Pollut. 2002;120:415–422. doi: 10.1016/S0269-7491(02)00107-0. [DOI] [PubMed] [Google Scholar]
- 67.Donaldson K., Stone V. Current hypotheses on the mechanisms of toxicity of ultrafine particles. Ann. Ist. Super. Sanità. 2003;39:405–410. [PubMed] [Google Scholar]
- 68.Nel A., Xia T., Madler L., Li N. Toxic potential of materials at the nanolevel. Science. 2006;311:622–627. doi: 10.1126/science.1114397. [DOI] [PubMed] [Google Scholar]
- 69.Shukla R.K., Sharma V., Pandey A.K., Singh S., Sultana S., Dhawan A. ROS-mediated genotoxicity induced by titanium dioxide nanoparticles in human epidermal cells. Toxicol. In vitro. 2011;25:231–241. doi: 10.1016/j.tiv.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 70.Kazimirova A., Baranokova M., Staruchova M., Drlickova M., Volkovova K., Dusinska M. Titanium dioxide nanoparticles tested for genotoxicity with the comet and micronucleus assays in vitro, ex vivo and in vivo. Mutat. Res. 2019;843:57–65. doi: 10.1016/j.mrgentox.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 71.Stoccoro A., Di Bucchianico S., Coppedè F., Ponti J., Uboldi C., Blosi M., Delpivo C., Ortelli S., Costa A.L., Migliore L. Multiple endpoints to evaluate pristine and remediated titanium dioxide nanoparticles genotoxicity in lung epithelial A549 cells. Toxicol. Lett. 2017;276:48–61. doi: 10.1016/j.toxlet.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 72.Patel S., Patel P., Bakshi Sonal R. Titanium dioxide nanoparticles: An in vitro study of DNA binding, chromosome aberration assay, and comet assay. Cytotechnology. 2017;69:245–263. doi: 10.1007/s10616-016-0054-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Reeves J.F., Davies S.J., Dodd N.J.F., Jha A.N. Hydroxyl radicals (•OH) are associated with titanium dioxide (TiO 2) nanoparticle-induced cytotoxicity and oxidative DNA damage in fish cells. Mutat. Res. 2008;640:113–122. doi: 10.1016/j.mrfmmm.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 74.Challier J.C., Panigel M., Meyer E. Uptake of colloidal 198Au by fetal liver in rat, after direct intrafetal administration. Int. J. Nucl. Med. Biol. 1973;1:103–106. [PubMed] [Google Scholar]
- 75.Bosman S.J., Nieto S.P., Patton W.C., Jacobson J.D., Corselli J.U., Chan P.J. Development of mammalian embryos exposed to mixed-size nanoparticles. Clin. Exp. Obs. Gynecol. 2005;32:222–224. [PubMed] [Google Scholar]
- 76.Enescu D., Cerqueira M.A., Fucinos P., Pastrana L.M. Recent advances and challenges on applications of nanotechnology in foodpackaging. A literature review. Food Chem. Toxicol. 2019;134:110814. doi: 10.1016/j.fct.2019.110814. [DOI] [PubMed] [Google Scholar]