Positive end-expiratory pressure (PEEP) is a cornerstone treatment for critically ill patients, with beneficial effects for acute respiratory distress syndrome (ARDS).
In ARDS, PEEP prevents alveolar collapse during expiration and counteracts increased surface tension due to surfactant impairment, alveolar over-deflation, and superimposed pressure. These mechanisms contribute to a reduction in intrapulmonary shunting. Furthermore, alveolar recruitment maintained through PEEP may translate into a higher end-expiratory lung volume (EELV), which often leads to better compliance of the respiratory system (CRS) and therefore a reduction in the driving pressure (DP), both of which are associated with higher survival rates [1]. Moreover, alveolar stability protects against intra-tidal recruitment/derecruitment (i.e., atelectrauma) [2] and imposed mechanical stresses and inflammation (i.e., biotrauma) [3], and it reduces ventilation heterogeneity [4].
Advantages of PEEP should be balanced against its potential disadvantages, namely, a reduction in cardiac output, an increase in pulmonary vascular resistance and alveolar dead space, and the risk of regional over-inflation [5].
Recommended PEEP titration
Current guidelines concerning moderate or severe ARDS recommend using higher rather than lower PEEP levels [6]. This recommendation is based on meta-analysis of individual patient data [7]. Furthermore, a subsequent ancillary analysis of LUNG SAFE reported that higher PEEP levels are associated with improved survival [8].
How do we set up PEEP
We present a PEEP titration strategy that relies heavily on physiological considerations, which is applied at our center. This opinion-based editorial is based on our interpretation of the evidence-based medical literature and on clinical experience, without presumptions of exhaustiveness or superiority to other strategies.
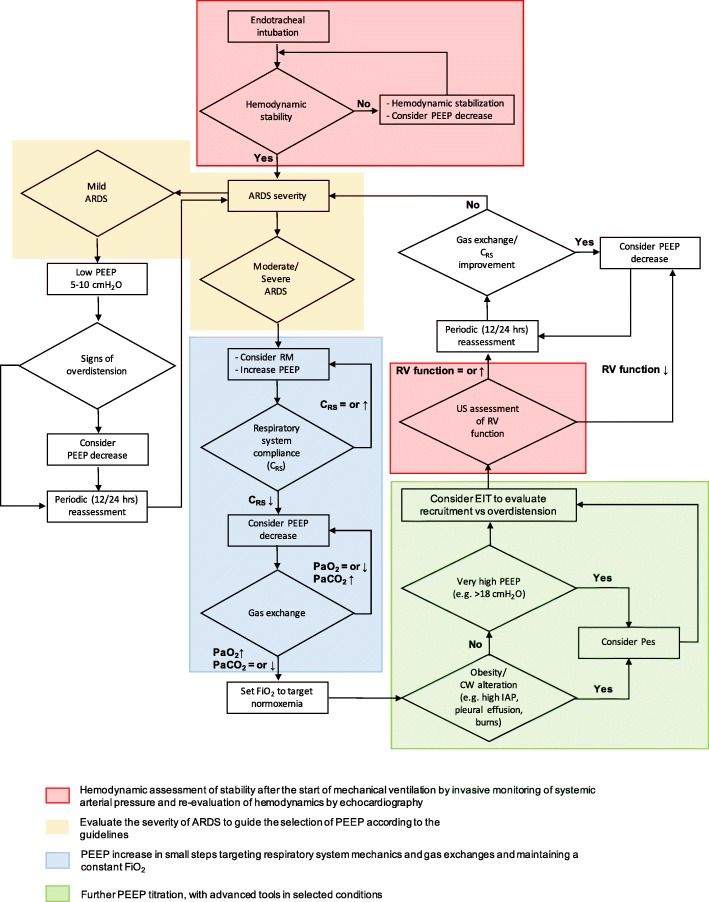
For moderate and severe ARDS, the guidelines [6] recommend higher PEEP levels without specifying absolute values or, more importantly, what methodology to apply. Therefore, for patients with moderate or severe ARDS, we typically aim to increase PEEP levels, if hemodynamic conditions allow it, through closely monitoring the individual response and focusing on two main targets: driving pressure and oxygenation (Fig. 1).
Fig. 1.
Evidence-based decision-making flow chart for patients with ARDS requiring treatment using PEEP, according to patient physiological readouts. The approach we use to set up PEEP is applied either to patients in a supine position or to those with moderate-to-severe ARDS and prone positioning. Each step lasts normally 10 to 30 min. The area in light blue indicates that FiO2 remains constant throughout the steps. After PEEP titration FiO2 can be decreased (or increased) to target normoxia. Pre-existing barotrauma and (according to some authors) elevated intracranial pressure should discourage from application of high PEEP. Abbreviations and symbols: ARDS, acute respiratory distress syndrome; CRS, compliance of the respiratory system; CW, chest wall; EIT, electrical impedance tomography; FiO2, inspiratory oxygen fraction; PEEP, positive end-expiratory pressure; Pes, esophageal pressure; RM, recruitment maneuver; RV, right ventricle; US, ultrasound; ↑, increase; ↓, decrease; =, equal
Driving pressure
CRS is proportional to the “baby lung” size [9]; therefore, as a good proxy of EELV (albeit possibly influenced by other factors, such as chest-wall compliance), CRS tends to increase with recruitment but decreases again once over-inflation begins. For this reason, changes in CRS are a key element for PEEP titration. At the same tidal volume (VT), any change in CRS will be reflected in the driving pressure (DP) [10], or if pressure control is used, VT increases for the same DP. We increase PEEP levels aiming to observe a decrease in DP at the same VT, likely indicating recruitment (not necessarily to a fully open lung). To facilitate this process, we could use a moderate recruitment maneuver (RM) (e.g., 40 cmH2O for 20 s) before increasing PEEP. An RM (rather than to correct hypoxemia) might work as a diagnostic tool (diagnostic RM) to explore the potential for lung recruitability, leading to an increase in PEEP levels in responders compared with non-responders. Simultaneously, if CRS decreases when PEEP is increased, indicating overdistension, we reduce either PEEP or VT (if feasible in terms of CO2 elimination and respiratory rate). For a safe plateau pressure (Pplat), one size (i.e., 30 cmH2O) does not fit all, and if overdistension is an issue, our safety threshold for Pplat is decreased.
Oxygenation
We always verify the response to gas exchange, primarily, an increase in PaO2 at a constant inspiratory FiO2, with constant or decreasing PaCO2. Although PaO2/FiO2 is a poor proxy for alveolar recruitment, patients who have responded to an increased PEEP with improved oxygenation have been reported to have a reduced risk of death [11]. As such, we prefer to uncouple the PEEP and FiO2 settings. Patients do not always show an improvement in oxygenation with higher PEEP levels. In this scenario, a strategy that mandates simultaneous increase of these parameters (e.g., PEEP/FiO2 tables) would recommend a further PEEP increase combined with FiO2. Finally, an increase in PaCO2 levels in relation to a PEEP increase should be an immediate alert for a risk of overdistension.
Of late, and more frequently, we are taking advantage of bedside electrical impedance tomography (EIT) to corroborate our PEEP titration procedure. We propose a 2-step strategy. First, we perform a diagnostic RM to evaluate the potential for lung recruitment. Second, we increase the PEEP level in small increments (e.g., 2 cmH2O) until it is sufficient to maintain EELV stability, according to the end-expiratory lung impedance signal. This approach leads to an improvement in arterial oxygenation and a reduction in the DP and provides regional information concerning the balance between alveolar overdistension and collapse [12].
We typically confine the measurement of esophageal pressure to selected clinical conditions (Fig. 1).
Controversies concerning the use of higher PEEP levels
The described approach might appear to be contradictory to the recent literature [13] reporting that patients receiving an RM followed by a decremental PEEP trial, according to CRS, have increased mortality rates. However, we consider that this study does not invalidate the concept of higher PEEP levels being associated with a lower DP, as it combined other procedures that might have contributed to the higher mortality, such as an aggressive RM of up to 60 cmH2O (reduced to 50 cmH2O after 50% enrollment) and lasting several minutes overall, which required important fluid expansion, neuromuscular blocking agents, and an additional RM performed after PEEP titration. Furthermore, the decision to set PEEP at 2 cmH2O above the best CRS likely led to regional overdistension of the non-dependent lung.
Future perspectives and conclusion
It is known that a high PEEP level does not fit all; therefore, innovative concepts such as the different responses of hypo- and hyper-inflammatory ARDS phenotypes to PEEP [14] and the use of population enrichment for inclusion in trials [15] are encouraging.
In the meantime, we set PEEP levels for patients with moderate or severe ARDS that aim for a moderate reasonable recruitment, given the challenges of full lung recruitment, according to incremental PEEP steps (possibly interspersed with short diagnostic RMs) and seek improvements in functional and physiologic readouts, such as CRS, gas exchange, and EIT.
Acknowledgements
We are grateful to Prof. Antonio Pesenti and Prof. Giacomo Grasselli for their invaluable suggestions in reviewing this manuscript.
Abbreviations
- ARDS
Acute respiratory distress syndrome
- CRS
Compliance of the respiratory system
- DP
Driving pressure
- EELV
End-expiratory lung volume
- EIT
Electrical impedance tomography
- FiO2
Inspiratory fraction of oxygen
- PaCO2
Arterial pressure of carbon dioxide
- PaO2
Arterial pressure of oxygen
- PEEP
Positive end-expiratory pressure
- Pplat
Plateau pressure
- RM
Recruitment maneuver
- VT
Tidal volume
Authors’ contributions
ER and GB conceived the study, reviewed the literature, wrote the manuscript, critically revised it, and read and approved the final manuscript.
Funding
The study was supported by Institutional funds.
Availability of data and materials
Not applicable
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
G.B. received lecturing fees from Draeger. E.R. declares that he has no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sahetya SK, Goligher EC, Brower RG. Fifty years of research in ARDS. Setting positive end-expiratory pressure in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(11):1429–1438. doi: 10.1164/rccm.201610-2035CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caironi P, Cressoni M, Chiumello D, Ranieri M, Quintel M, Russo SG, Cornejo R, Bugedo G, Carlesso E, Russo R, Caspani L, Gattinoni L. Lung opening and closing during ventilation of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2010;181(6):578–586. doi: 10.1164/rccm.200905-0787OC. [DOI] [PubMed] [Google Scholar]
- 3.Tremblay LN, Slutsky AS. Ventilator-induced injury: from barotrauma to biotrauma. Proc Assoc Am Physicians. 1998;110:482–488. [PubMed] [Google Scholar]
- 4.Cressoni M, Cadringher P, Chiurazzi C, et al. Lung inhomogeneity in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2014;189(2):149–158. doi: 10.1164/rccm.201308-1567OC. [DOI] [PubMed] [Google Scholar]
- 5.Luecke T, Pelosi P. Clinical review: positive end-expiratory pressure and cardiac output. Crit Care. 2005;9(6):607–621. doi: 10.1186/cc3877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fan E, Del Sorbo L, Goligher EC, et al. American Thoracic Society, European Society of Intensive Care Medicine, and Society of Critical Care Medicine. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(9):1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]
- 7.Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303(9):865–873. doi: 10.1001/jama.2010.218. [DOI] [PubMed] [Google Scholar]
- 8.Laffey JG, Bellani G, Pham T, et al. LUNG SAFE Investigators and the ESICM Trials Group. Potentially modifiable factors contributing to outcome from acute respiratory distress syndrome: the LUNG SAFE study. Intensive Care Med. 2016;42(12):1865–1876. doi: 10.1007/s00134-016-4571-5. [DOI] [PubMed] [Google Scholar]
- 9.Gattinoni L, Pesenti A. The concept of “baby lung”. Intens Care Med. 2005;31(6):776–784. doi: 10.1007/s00134-005-2627-z. [DOI] [PubMed] [Google Scholar]
- 10.Amato MB, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8):747–755. doi: 10.1056/NEJMsa1410639. [DOI] [PubMed] [Google Scholar]
- 11.Goligher EC, Kavanagh BP, Rubenfeld GD, et al. Oxygenation response to positive end-expiratory pressure predicts mortality in acute respiratory distress syndrome. A secondary analysis of the LOVS and ExPress trials. Am J Respir Crit Care Med. 2014;190(1):70–76. doi: 10.1164/rccm.201404-0688OC. [DOI] [PubMed] [Google Scholar]
- 12.Eronia N, Mauri T, Maffezzini E, et al. Bedside selection of positive end-expiratory pressure by electrical impedance tomography in hypoxemic patients: a feasibility study. Ann Intensive Care. 2017;7(1):76. doi: 10.1186/s13613-017-0299-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators. Cavalcanti AB, Suzumura ÉA, Laranjeira LN, et al. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318(14):1335–1345. doi: 10.1001/jama.2017.14171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Calfee CS, Delucchi K, Parsons PE, et al. NHLBI ARDS Network. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med. 2014;2(8):611–620. doi: 10.1016/S2213-2600(14)70097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shankar-Hari M, Rubenfeld GD. Population enrichment for critical care trials: phenotypes and differential outcomes. Curr Opin Crit Care. 2019;25(5):489–97. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable