Abstract
Background: Problem-based learning (PBL) is an inquiry-based learning strategy which is learner centered and facilitates group discussion and critical thinking. Case-based learning (CBL), which is a more guided approach of PBL, enables students to learn within the context of patients and formulate their knowledge around patients' scenarios. Midweek (MW) activity is an important educational activity in the internal medicine residency program (IMRP). CBL has shown many benefits in postgraduate education. The aim of our study was to describe the implementation of a teaching resident's management of acute medical conditions encountered during their call utilizing the CBL format and to evaluate resident satisfaction with the new teaching style. Methods: This study describes the implementation of CBL in residents' education at the IMRP. CBL was introduced in five of the 10 acute medical sessions taught in the noon activity. A mixed-method study was employed using both a structured questionnaire and a focus group to compare the two methods to evaluate the residents' satisfaction and perception of knowledge acquisition. Results: The focus group discussion showed that sessions conducted in CBL format were more engaging, interactive, and resulted in better knowledge acquisition through sharing and peer-to-peer teaching than the traditional lecture format. Thirty-nine out of 83 (47%) residents ranging from PGY2 to PGY4 responded to the survey. Overall satisfaction with CBL was good. Sixty-four percent preferred it over the lecture format; 87% found that they did improve their knowledge; 84% agreed that they were excellent and more interactive. Seventy-nine percent stated that they would like to have this type of teaching in the MW activity sessions. Conclusion: Based on the present study, we conclude that incorporation of CBL resulted in more engagement, interaction, peer-to-peer education, and overall residents' satisfaction. The key elements for a successful implementation of this format are both instructors' and residents' orientation and careful selection of the case scenarios (problems) that trigger the learning process. Incorporation of various teaching strategies in residents' education is mandatory to enhance learning and create excellent educational experiences.
Keywords: case-based learning, problem-based learning, teaching strategies, Accreditation Council of Graduate Medical Education, Accreditation Council of Graduate Medical Education- International
Background
The midweek (MW) activity is an important educational activity in IMRP, an accredited residency program at Hamad Medical Corporation, a large tertiary hospital in Qatar. The MW activity is conducted in the middle of every week at noon and consists of a series of one-hour sessions that focus on enhancing laboratory and radiological interpretation skills and management of acute medical conditions commonly encountered during the on-call service. It is run by a group of faculty using the traditional lecture-based teaching (TLBT) format. Attendees range from 30 to 35 residents per activity.
The revolution in information technology and the ease of information delivery make the traditional lecture format outdated. TLBT varies according to individual experience; therefore, the quality of teaching is not standardized and becomes questionable. Large lecture courses often do not contribute to fostering students' scientific curiosity, analytic thinking, and reasoning, which are key skills for future scientists.1
Problem solvers possess an organized and flexible knowledge base and master the skills to apply this knowledge for problem solving.2 Problem-based learning (PBL) is well-suited to helping students become active learners because it situates learning in real-world problems and makes students responsible for their learning.3 In PBL, students use triggers from a problem case or scenario to define their own learning objectives. PBL uses appropriate problems to increase knowledge and understanding.4 Case-based learning (CBL) is a form of PBL and is considered an inquiry-based learning method where case scenarios are carefully constructed to stimulate discussion. There have been several studies on the value of CBL in medical curricula showing where it has been widely used in both undergraduate and postgraduate medical training.5 CBL imparts relevance to medical and related curricula, is shown to tie theory to practice, and induces deeper learning; it is certain to become part of every medical and health profession's curriculum.6 A study in teaching residents the concepts of reproductive endocrinology and infertility through interactive case-based learning showed that CBL can be successfully integrated into a residency curriculum, and significantly improves knowledge and confidence of critical concepts in the subject.7
There are few studies that describe the implementation of CBL in medical and nursing curricula in Qatar and the gulf region with promising benefits. For instance, flipping the classroom from a teacher-centered to a learner-centered approach in a developing needs analysis training module using the CBL format has been shown to encourage participants' higher-order learning and foster engagement, exploration, evaluation, and reflection.8 Another regional study performed among medical students who received PBL found that this format helped them understand the underlying mechanism of problems and contributed to their communication skills better than if it had been lectured in the conventional way, ultimately giving them more confidence to speak up and explain their ideas.9 Besides satisfaction, among nursing students taught in the CBL nursing program, performance was better in the total critical thinking scores and all critical thinking subscales than for the didactic program participants.10
Thus, as part of the educational redesign phase, several curriculum reform initiatives were adopted to support the transformation of the IMRP into the Accredited Council for Graduate Medical Education-International (ACGME-I) program. The aim of this study was to incorporate a CBL curriculum during the regular MW activity to teach the medical residents management of acute medical conditions encountered during their calls using cases and to explore residents' perceptions of CBL on their learning. Understanding the impact of CBL on the perceived knowledge and learning behavior of postgraduate trainees will help us design appropriate teaching encounters for residency training.
Methods
Setting and participants
The study involved all 83 internal medicine residents (PGY2 to PGY4) at the internal medicine department at Hamad Medical Corporation, a large tertiary hospital that provides postgraduate education, who attended the 10 MW activity sessions over the duration of three blocks. The study excluded the newly joined PGY1 as they had not enough exposure to the MW activity. Ten sessions of the MW activity are usually dedicated to teaching acute medical conditions commonly encountered during the residents' on-call service. MW activities are moderated by a group of faculty from different specialties. Some examples of topics discussed are management of electrolyte disturbances, diabetic and hypertensive emergencies, etc. Each session lasts for one hour and is attended by a group of 20–30 IM residents in the traditional lecture format at noon.
The CBL format was implemented in five out of the 10 acute medicine session slots of the MW activity. Instructors who volunteered to run the selected sessions received a half-hour orientation about the CBL format from the study author's. They were educated about knowledge delivery through case scenarios and discussions and to act as facilitators rather than as teachers. The seating arrangement of the conference room was changed and attendees were divided into small groups around tables to facilitate collaboration and teamwork. The chosen topics were five of the acute cases: two sessions on management of electrolyte imbalance (one on sodium and one on potassium); one on management of glucose emergencies; one on management of asthma exacerbation; and one on management of calcium disorders. Each session started with an interactive introduction about the topic. Each group was then given different case scenarios which were to be analyzed and discussed within the group. Residents were provided with questions at the end of each case scenario that helped them analyze the case and come up with a management plan. The instructor acted as a facilitator and moved among the groups, checking on their progress, supervising their discussions, and providing guidance as needed. At the end, all the groups engaged in discussion of the answers to the questions asked.
Evaluation methods
The measure of improvement was reflected through employment of a mixed research method using a structured questionnaire and focus group discussions. Data collection was confidential and descriptive statistics expressed as sums and percentages of all variables across all participants were computed.
Residents' satisfaction survey
To better understand the residents' acceptance and satisfaction of the new CBL system, they were encouraged to complete a web-based questionnaire using the Survey Monkey program. This 28-item questionnaire included one question on residents' training level and 27 items on residents' perception of the MW activity in general and specifically on the sessions delivered in the CBL format. The first part of the survey focused on the current format and included questions about the residents' attendance and their ratings on the quality, content, topic selection, choice of instructors, and measures for improvement. The second part of the questionnaire inquired about the residents' perception of the CBL format, whether it had enhanced learning. Both five-point Likert scale (1 = strongly disagree, 5 = strongly agree) and open-ended questions were included to enable the residents to demonstrate their level of agreement and provide more detailed information (Appendix A). The questionnaire was piloted on a group of residents. Questions and data findings from the pilot study were analyzed through a plenary discussion to decide if changes to the questionnaire were necessary. The survey was completed anonymously and was kept online for eight weeks; three reminders were sent. Prior to emailing the survey, we sought ethical approval from the Medical Research Center Institutional Review Board, which approved the study exemption.
Focus group discussions
We conducted two focus group discussions to solicit residents' opinions regarding the MW activity in general and the CBL format. To produce valid results, two one-hour focus groups were conducted in the medical education classrooms by the study investigators: one included eight participants and the other included 10. Their participation was strictly voluntary and opinions were kept confidential. A list of five questions was developed to aid the discussion. The questions were of a short exploration type; they were open-ended and began with “Why” and “How” and targeted the concept of CBL. During the discussions, the participants were encouraged to express their opinions about the current MW activity format and the new CBL format sessions. Notes were documented and full sentences were converted to bulleted phrases.
Results
Results of the focus group discussions
More than 85% of the residents rated the MW activity as a valuable activity in the residency program, the main reason being the topic selection, which was very relevant to their practice. They recommended more sessions to develop and improve procedural skills. According to the residents, attendance was difficult because of time constraints. Residents stated that the MW activity runs at the end of the day and coincides with the nurses' endorsement time and as a result, they receive many interruptions and pages forcing them to leave the activity midway. Most of the residents were happy with the selection of the speakers with very few reservations; most of the residents favored junior faculty such as fellows rather than senior faculty to moderate the sessions as their lecture format was more interactive and interesting. The residents also felt that senior speakers from other specialties deliver very specialized information that is not required at their level. They rated the learning environment as ideal and recommended adding snacks in the conference room.
When they were interviewed about the CBL format that had been incorporated in some of the acute medicine sessions, they found that these sessions were more engaging, interactive and resulted in better knowledge acquisition through sharing among each other and peer-to-peer teaching than the traditional lecture format. They found it suitable only with the sessions where investigations and management were the focus of the activity as it enhanced their perceived knowledge and clinical reasoning skills. Each session conducted in CBL format provided different case scenarios representing multiple presentations of the same disease through which residents were able to develop reasoning skills and provide the proper management accordingly. For instance, residents were able to identify the various presentations of electrolyte disturbances with different etiologies and hence could provide different approaches to managing them. This was reflected in their practical application of those approaches during on-call duty. Thus, they concluded that CBL is very helpful when immediate management is needed as it enhanced their clinical reasoning and their memory. On the other hand, residents found didactic lectures more suitable for certain topics such as medical ethics and discussion of end-of-life care, where passage of massive information is required and clear decisions can be made easily.
Results of the residents' survey
Thirty-nine out of 83 (47%) residents ranging from PGY2 to PGY4 responded to the survey. There was equal representation according to the PGY (postgraduate year) level: PGY2 (31%), PGY3 (33%), and PGY4 (36%). Of these, 74% admitted attending the activity (often and very often). The main reasons for lack of attendance of the activity were postings outside the hospital (62%) and busy schedule (23%).
Most of the residents (97%) rated the MW activity as a valuable activity, as most of the topics were comprised of the management of problems commonly encountered during routine day-to-day patient care. The quality of the MW activity was graded as good by 86% and this depended mainly on presenters, who mostly were perfect for the chosen topic, as agreed by 77% respondents. Regarding the contents and topics of the MW activity, 87% found that they did improve their knowledge. Eighty-six percent of the residents commented that discussion should be more interactive and practical instead of presentations with overloaded PowerPoint slides.
In open-ended questions, residents commented on the main elements that need to be changed (Figure 1). Their main concern was the lack of interaction; almost half of the residents (42%) recommended more interactive sessions.
Figure 1.
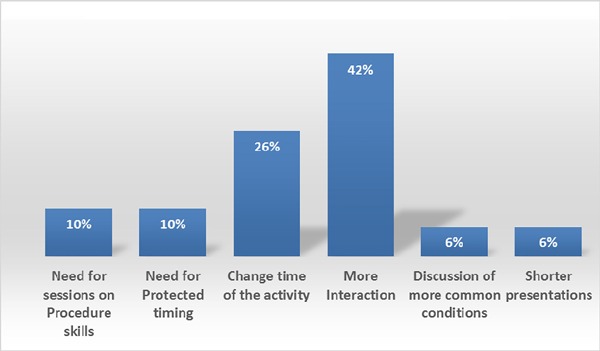
Residents' recommendations for change.
The rest of the survey targeted the sessions which were delivered in CBL format. The overall satisfaction with the new CBL format was good. Seventy-four percent of the residents attended these sessions. Of those, 64% preferred it over the lecture format; 87% found that they did improve their knowledge and applicability in everyday practice; 84% agreed that the new format was excellent and more interactive. Moreover, it enabled them to apply concepts to practical settings and learn from each other. It also resulted in creating new ideas, creating a sense of community (Figure 2). Eighty percent recommended that this type of teaching be implemented in the MW activity sessions.
Figure 2.
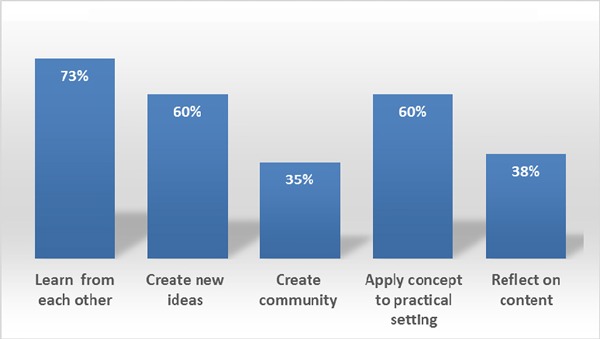
Residents' perception of the new CBL format.
Discussion
This study demonstrated residents' preference for CBL in management of commonly encountered conditions during their calls. Residents specified that they were able to apply the practical knowledge they gained during the CBL sessions in providing direct care to ill patients during their on-call duties. They indicated that they did not have to look for resources as they were easily able to recall lines of management taught in the CBL sessions. This has been shown in studies where CBL has become a popular method in teacher education and in instructional design and technology. In one study, case-based conferences received higher Likert ratings on residents' perception in topic understanding when compared with traditional lecture-based conferences and were thus described as a dynamic approach to identifying strengths and weaknesses in a resident's curriculum as well as a means for more focused and real-time improvements.11 Our study demonstrated this popularity among residents as described in the following sections.
Knowledge acquisition, applicability, and reflective learning
Our study results showed that CBL is an effective tool in learning. Postgraduate education occurs within hospital settings and knowledge is best created around patients. By presenting complex case histories of near-real patients as the pretext for learning, CBL encourages students to formulate an integrated, multidisciplinary knowledge-based approach. This agrees with already published data, including a systematic review on the effectiveness of CBL in health education.5 As a part of our detailed assessment, we noted that residents actually preferred CBL over traditional teaching methods. The residents were motivated by the new format as it allowed them to engage in problem solving, critical thinking, and analysis of complex issues. They relied on constructing their own knowledge rather than passively perceiving knowledge from their instructors. They noted that “Discussion should be more interactive and practical instead of presentations with overloaded PowerPoint slides.” This was further reflected in their comments and recommendations for change as the main concern of the majority of residents was to have more interactive sessions rather than being overloaded with passive knowledge transfer through traditional lectures with overloaded slides, emphasizing the residents' preference for the CBL format over the TBL format.
Ali et al., showed that CBL enhances students' clinical skills, and that the role of the facilitator switches from being relatively passive in PBL to playing a more active role in guiding students through clinical or diagnostic reasoning with CBL.12
Besides being a more enjoyable modality,13 a recent study demonstrated an increase in residents' engagement and scores as well.14 By allowing residents to reflect on their reasoning, CBL provides a safe learning environment. The literature shows that it engages learners in higher-order thinking processes such as analysis and synthesis.15–16 In an interactive case-based curriculum that teaches concepts of reproductive endocrinology and infertility, there was a significant improvement in residents' knowledge of and confidence in understanding the subject's critical concepts.7 Moreover, residents became more involved and proactive in their learning process and consequently more eager to test their competence when following a case-based strategy.17 Discussions around case scenarios created cognitive interactions and confidence in formulating clinical reasoning skills that enabled the residents to provide immediate care to their patients during calls:
“We were able to manage our patients without any difficulty during our calls.”
“Case scenarios provided were very helpful and augmented real case scenarios.”
This has also been shown in a study teaching anatomy to medical students where data confirms that case-based resources are a useful adjunct to anatomy teaching when used as a focal point for small group discussions where students made multiple requests that additional cases be made available for their study.18
Teamwork and collaboration
In CBL, students work in collaborative groups to identify what they need to learn in order to solve problems, engage in self-directed learning, apply their new knowledge to problems, and reflect on what they learn and the effectiveness of the strategies employed.15 Our study confirmed the residents' satisfaction and motivation with the collaborative work and group discussions. Besides motivation, collaborative learning potentially promotes deep learning, in which students engage in high-quality social interaction, such as discussing contradictory information.19 Collaborative learning also provides an opportunity for critical discourse and immediate, directed feedback to the students, both as individuals and as a group.20 Therefore, CBL has the benefit of both nurturing trainees' motivation and domain knowledge.21 This has been shown in a recent study that fostered medical trainees' collaborative learning skills as a lifelong learning endeavor with the support of real-world clinical cases.12 The interaction among our residents created a peer-to-peer teaching environment that was perceived as a sense of community. Interaction between residents at different training levels was perceived as useful in developing confidence in communication skills in a collaborative setting.22 Research on collaborative learning concludes that it contributes to cognitive learning as well as social and emotional development.23–24 In our study, residents were motivated to work as a team towards problem solving. In dermatology medical education, CBL was well-received by students, and participants commented that the format made a huge difference leading to more group interactions and questions.25
While residents favor the new format over the traditional lecture-based style in managing acute medical conditions, they stated that some topics cannot be conducted using this format. Ethics and discussion of end-of-life care are better taught in the lecture-based format. Traditional approaches were favored for short-term retention of course content that did not require any elaboration. Lectures were found to be effective in covering large chunks of the material quickly, can be easily adapted to fit the needs and interests of a particular audience and can be used for promoting basic knowledge of the subject material.26
Study limitations
The study has some limitations. One is that it was implemented on a small number of activities concerned with management of acute medical conditions. Most importantly, this study measured trainees' perception of the new format. While this is of significant importance as it is expected to be reflected in their attendance and commitment, a more objective measure that assesses a higher level on the Kirkpatrick hierarchy would reflect a better impact on trainees learning. Future studies should describe its implementation on all postgraduate activities using a more objective measure that evaluates knowledge acquisition and perhaps its impact on patient outcome.
Conclusions
At our institution, the MW activity is currently conducted in a traditional lecture-based format at noon. Our study emphasizes that in spite of the efforts and the time spent in implementation of the new format, utilizing CBL in postgraduate education improves residents' overall perception of knowledge acquisition, applicability and reflection, in addition to sense of teamwork and collaboration. We recommend incorporation of the CBL format in postgraduate education to improve residents' learning experience. Factors that enable successful implementation of this format include instructor and resident orientation and careful selection of the case scenarios (problems) that trigger the learning process. Residents require protected time for these activities to enhance learning during their residency period.
Conflict of interest
The authors report no conflicts of interest. The authors are responsible for the content and writing of this article.
Funding
The research is supported by the Medical Research Center at Hamad Medical Corporation.
Appendix A: Midweek activity residents' satisfaction survey
MW: Midweek
1. Resident Level: PGY2 PGY3 PGY4
2. Do you attend the midweek activity regularly?
Very Often Often Sometimes Rarely Never
○ ○ ○ ○ ○
3. Comment on Question 2

4. Do you rate it as a valuable educational activity?
Strongly agree Agree Neutral Disagree Strongly disagree
○ ○ ○ ○ ○
5. Comment on Question 4

6. Is the quality of the MW lectures satisfactory?
Strongly agree Agree Neutral Disagree Strongly disagree
○ ○ ○ ○ ○
7. Comment on Question 6

8. Is the quality of instructors satisfactory?
Strongly agree Agree Neutral Disagree Strongly disagree
○ ○ ○ ○ ○
9. Comment on Question 8

10. Contents and topics of the midweek activity improved my knowledge:
Strongly agree Agree Neutral Disagree Strongly disagree
○ ○ ○ ○ ○
11. Comment on Question 10

12. The midweek activity presentations were useful.
Strongly agree Agree Neutral Disagree Strongly disagree
○ ○ ○ ○ ○
13. Comment on Question 12

14. Elements of the course that I found very helpful:

15. Elements of the sessions that I would like to change (and how you would change them):

16. Have you attended the last acute medicine sessions of the MW activity?
All Some None
17. Have you attended MW activity in the Case Based learning format (case scenario group Discussion)?
Yes No
18. Comment on Question 17

19. Would you prefer it over the lecture style of teaching?
Strongly agree Agree Neutral Disagree Strongly disagree
○ ○ ○ ○ ○
20. Comment on Question 19

21. Discussions in Case based format provided opportunities to (select all that apply)
▪ Learn from each other
▪ Create community
▪ Reflect on content
▪ Create new ideas
▪ Apply concepts to practical settings
22. Comment on Question 21

23. The new format of teaching (CBL) is more engaging when compared to the traditional format:
Strongly agree Agree Neutral Disagree Strongly disagree
24. The new format of teaching (CBL) provides more knowledge when compared to the traditional format:
Strongly agree Agree Neutral Disagree Strongly disagree
25. The new format of teaching (CBL) provides more interaction when compared to the traditional format:
Strongly agree Agree Neutral Disagree Strongly disagree
26. Comment on Questions 23–25

27. Would you like to have this type of teaching in the Midweek activity sessions?
Strongly agree Agree Neutral Disagree Strongly disagree
28. Comment on Question 27

References
- 1.Handelsman J, Ebert-May D, Beichner R, Bruns P, Chang A, DeHaan R et al. Scientific teaching. Science. 2004;304(5670):521–522. doi: 10.1126/science.1096022. [DOI] [PubMed] [Google Scholar]
- 2. Chi MTH, Glaser R, Rees E. Expertise in problem solving. In: Sternberg RS, ed. Advances in the Psychology of Human Intelligence. Hillsdale, NJ: Erlbaum; 1982:1–75.
- 3.Hmelo-Silver CE. Problem-based learning: what and how do students learn? Educ Psychol Rev. 2004;16(3):235–266. [Google Scholar]
- 4.Barbour RS. Making sense of focus groups. Med Educ. 2005;39(7):742–750. doi: 10.1111/j.1365-2929.2005.02200.x. [DOI] [PubMed] [Google Scholar]
- 5.Thistlethwaite JE, Davies D, Ekeocha S, Kidd JM, MacDougall C, Matthews P et al. The effectiveness of case-based learning in health professional education: A BEME systematic review: BEME Guide 23. Med Teach. 2012;34(6):e421–e444. doi: 10.3109/0142159X.2012.680939. [DOI] [PubMed] [Google Scholar]
- 6.McLean SF. Case-based learning and its application in medical and health-care fields: a review of worldwide literature. J Med Educ Curricular Dev. 2016:3. doi: 10.4137/JMECD.S20377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldman KN, Tiegs AW, Uquillas K, Nachtigall M, Fino ME, Winkel AF et al. Interactive case-based learning improves resident knowledge and confidence in reproductive endocrinology and infertility. Gynecol Endocrinol. 2017;33(6):496–499. doi: 10.1080/09513590.2017.1290075. [DOI] [PubMed] [Google Scholar]
- 8. Berger G. Needs assessment lessons learned in Qatar: a flipped classroom approach. MedEdPublish. 2019;8(1) [DOI] [PMC free article] [PubMed]
- 9.Hagi SK, Al-Shawwa LA. Evaluation of second and fourth year undergraduate medical students' perception and acceptance of the problem-based learning process. Saudi Med J. 2011;32(10):1060–1065. [PubMed] [Google Scholar]
- 10.Majeed F. Effectiveness of case-based teaching of physiology for nursing students. J Taibah Univ Med Sci. 2014;9(4):289–292. [Google Scholar]
- 11.Barnwell JC, Halvorson JJ, Teasdall RD, Carroll EA. Finding value in surgical didactics: longitudinal resident feedback from case-based and traditional lectures in an orthopaedic residency. J Surg Educ. 2017;74(1):61–67. doi: 10.1016/j.jsurg.2016.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Ali M, Han SC, Bilal HSM, Lee S, Kang MJY, Kang BH et al. iCBLS: an interactive case-based learning system for medical education. Int J Med Inform. 2018;109:55–69. doi: 10.1016/j.ijmedinf.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 13.Garvey MT, O'Sullivan M, Blake M. Multidisciplinary case-based learning for undergraduate students. Eur J Dent Educ. 2000;4(4):165–168. doi: 10.1034/j.1600-0579.2000.040404.x. [DOI] [PubMed] [Google Scholar]
- 14.Mokadam NA, Dardas TF, Hermsen JL, Pal JD, Mulligan MS, Jacobs LM et al. Flipping the classroom: case-based learning, accountability, assessment, and feedback leads to a favorable change in culture. J Thorac Cardiovasc Surg. 2017;153(4):987–996. doi: 10.1016/j.jtcvs.2016.10.101. [DOI] [PubMed] [Google Scholar]
- 15.Savery JR. Overview of problem-based learning: definitions and distinctions. Interdiscip J Problem Based Learn. 2006;1(1) [Google Scholar]
- 16.Tawfik AA. Essential readings in problem-based learning: exploring and extending the legacy of Howard S. Barrows. Interdiscip J Problem Based Learn. 2015;9(2):10. [Google Scholar]
- 17.Rodriguez-Muñoz D, Alonso-Salinas G, Franco-Diez E, Moreno J, Matía-Francés R, Hernández-Madrid A et al. Training in management of arrhythmias for medical residents: a case-based learning strategy. Int J Med Educ. 2016;7:322–323. doi: 10.5116/ijme.57c2.a738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holland JC, Pawlikowska T. Undergraduate medical students' usage and perceptions of anatomical case-based learning: comparison of facilitated small group discussions and elearning resources. Anat Sci Educ. 2019;12(3):245–256. doi: 10.1002/ase.1824. [DOI] [PubMed] [Google Scholar]
- 19.Visschers-Pleijers AJSF, Dolmans DHJM, De Leng BA, Wolfhagen IHAP, Van Der Vleuten CPM. Analysis of verbal interactions in tutorial groups: a process study. Med Educ. 2006;40(2):129–137. doi: 10.1111/j.1365-2929.2005.02368.x. [DOI] [PubMed] [Google Scholar]
- 20.Bowe CM, Voss J, Thomas Aretz H. Case method teaching: an effective approach to integrate the basic and clinical sciences in the preclinical medical curriculum. Med Teach. 2009;31(9):834–841. doi: 10.1080/01421590902922904. [DOI] [PubMed] [Google Scholar]
- 21.De Hei MSA, Strijbos JW, Sjoer E, Admiraal W. Collaborative learning in higher education: lecturers' practices and beliefs. Res Pap Educ. 2015;30(2):232–247. [Google Scholar]
- 22.Edmunds S, Brown G. Effective small group learning: AMEE Guide 48. Med Teach. 2010;32(9):715–726. doi: 10.3109/0142159X.2010.505454. [DOI] [PubMed] [Google Scholar]
- 23.Järvelä S, Volet S, Järvenoja H. Research on motivation in collaborative learning: moving beyond the cognitive-situative divide and combining individual and social processes. Educ Psychol. 2010;45(1):15–27. [Google Scholar]
- 24.Flynn AE, Klein JD. The influence of discussion groups in a case-based learning environment. Educ Technol Res Dev. 2001;49(3):71–86. [Google Scholar]
- 25.Liu A, Zhou LL, Lam A, Dahlke E. Case-based learning in dermatology. J Cutan Med Surg. 2018;22(3):273–279. doi: 10.1177/1203475417752368. [DOI] [PubMed] [Google Scholar]
- 26.Omelicheva MY, Avdeyeva O. Teaching with lecture or debate? Testing the effectiveness of traditional versus active learning methods of instruction. PS Political Sci Politics. 2008;41(3):603–607. [Google Scholar]


