Abstract
Introduction: While smoking remains one of the leading causes of death in Mexico, uptake of evidence-based cessation therapy remains low. Widespread use of mobile devices and internet in Mexico has created new avenues for providing access to cessation treatment.
Methods: We assessed the feasibility and acceptability of “Vive Sin Tabaco… ¡Decídete!” (English: Live without Tobacco…. Decide!), a web-based, informed decision-making tool designed to help Mexican smokers develop a quit plan and take advantage of cessation resources. We invited 164 smokers in two primary care clinics. Measures included physical, situational, and psychological nicotine dependence, interest in using pharmacotherapy and counseling, smoking status at 3 months, and satisfaction with the program.
Results: Most participants were light smokers and reported low-to-moderate nicotine dependence. Immediately after using ¡Vive Sin Tabaco… ¡Decídete!, the majority were interested in quitting, set a quit date, and reported interest in using pharmacotherapy and cessation counseling. Follow-up rate at 3 months was 81.5%; seven-day point prevalence abstinence was 19.1% using intention-to-treat analysis.
Conclusion: Integration of e-Health tools in primary healthcare settings has the potential to improve knowledge about cessation treatments among smokers and integrate smoking cessation into routine of care.
Keywords: e-health, telemedicine, m-health, technology, behavioral health
Introduction
Globally, one billion people will die from tobacco-related illnesses this century if trends in tobacco use remain unchecked. According to a 2017 World Health Organization report, the global smoking rates have decreased faster in High Income Countries compared to Low- and Middle-Income Countries (LMICs), where the smoking rates have remained, for the most part, undeterred in the last decade.1 To have an impact on reducing the prevalence of smoking in LMICs, new strategies are needed to engage smokers with effective cessation programs. Electronic health (e-Health) tools have the potential for reaching large numbers of smokers and helping them quit.2 There is a critical need to evaluate the potential of e-Health interventions in LMICs like Mexico.
Similar to smokers elsewhere,3 ∼72% of smokers in Mexico are interested in quitting.4 In Mexico, cessation treatment is partially covered through different public systems, including The Secretariat of Health's Seguro Popular (English: Popular Insurance), which offers brief advice and smoking cessation group counseling,5 the Instituto Mexicano del Seguro Social (IMSS) (English: Mexican Social Security Institute), and the Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado (ISSSTE) (English: Institute for Social Security and Services for State Workers), which offer counseling and pharmacotherapy treatment.6,7 Smoking cessation counseling is primarily delivered through referral to group counseling sessions in specialized centers.8 Unfortunately, healthcare providers often fail to initiate cessation treatment with smokers, even where these resources are available. Pharmacotherapy and cessation counseling use remain low in Mexico at 3.5% and 5.9%, respectively.4
Overcoming the burden of tobacco demands affordable, time-saving, easy to access, and effective technology-based solutions to address health problems in the healthcare system.9,10 The integration of an e-Health tool for smoking cessation in the Mexican healthcare system has the potential to address this serious public health problem and increase the reach and utilization of cessation interventions while also reducing the burden on healthcare professionals.11
e-Health tools can be used to provide patients with the ability to make informed decisions about treatment alternatives. There is strong evidence that informed decision-making interventions can improve patients' knowledge, enhance their ability to solve conflicts, and bring clarity regarding treatment options.12 To our knowledge, four studies have analyzed the effect of informed decision-making tools on smoking cessation,13–15 with one of these tools being delivered on a mobile platform. In this study of 128 mostly uninsured individuals (46.7% Spanish-speaking Latinos) in 3 safety-net clinics in the United States (U.S.), use of the tool was associated with a significant increase in uptake of smoking cessation pharmacotherapy and quit-line counseling.15
Despite the potential of e-Health tools to improve access to smoking cessation resources, it has not yet been used in Mexico.16,17 The purpose of this study was to assess the feasibility and acceptability of a web-based smoking cessation tool designed to inform Mexican smokers about the importance of quitting, promote smoking cessation, and guide smokers through their development of a quit plan.
Methods
Subjects and Setting
This study was conducted in two primary healthcare clinics (Centro Médico Familiar Ignacio Chavez and Tlalpan) in the south of Mexico City, between February and July 2015. These centers provide healthcare services to federal workers as part of the Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado (ISSSTE). Both centers provide smoking cessation services (smoking cessation group counseling and pharmacotherapy treatment) at no cost and have wireless internet capable of supporting web-based tools.
A research assistant recruited participants from the waiting room. Eligible participants were 18 years old or over, identified themselves as current smokers (all levels of smoking), and had telephone service. All subjects gave their informed verbal consent before participation in the study. Study procedures were approved by the Human Subjects Committee of the Instituto Nacional de Salud Pública (English: National Institute of Public Health) CI: 1197, No. 1471.
Intervention
Vive Sin Tabaco… ¡Decídete! (English: Live without Tobacco…. Decide!) was adapted from an existing web-based, informed decision-making tool for smoking cessation developed in English and Spanish for use among Latinos in the U.S.15 Vive Sin Tabaco… ¡Decídete! was designed to be displayed on an internet connected tablet computer with any internet browser. It uses an open source relational database management system based on Structured Query Language (MySQL) and Hypertext Preprocessor (PHP) language. A panel of healthcare professionals and researchers in Mexico adapted the content of Vive Sin Tabaco… ¡Decídete! to reflect the smoking behaviors and sociocultural characteristics of Mexican smokers.
Vive Sin Tabaco… ¡Decídete! was designed to help participants tailor their quit plan and identify “how,” “when,” and “where” they want to quit smoking. The software queried participants about their sociodemographic information, smoking patterns, smoking dependence, and attitudes related to smoking. The program guided smokers through specific decisions related to smoking, including use of pharmacotherapy (nicotine replacement therapy, bupropion, or varenicline) and counseling. The software contained a combination of video and audio featuring a professional actor guiding them through the program, as well as a testimonial from a former smoker.
The e-Health tool was placed in the main corridor of a waiting room for 4 weeks in each healthcare center so that it was private from public access but also accessible to all visitors of the healthcare centers. The tool was connected to a wireless printer that printed two forms for each participant, including one for the patient's healthcare provider with a summary of the patient's smoking behaviors, the patients desired strategies for quitting, and suggestion for how the provider could help the smoker quit. A second printout provided participants with their own reported reasons for quitting, level of interest in quitting, pharmacotherapy and behavioral treatment preferences, levels of physical and psychological tobacco dependence, and personalized recommendations for behavioral changes to consider before quitting smoking. The printout also prompted the participant to discuss their smoking cessation plan with their healthcare provider. The use of the Vive Sin Tabaco… ¡Decídete! tool took ∼15–20 min per participant to complete.
Participants expressing an interest in cessation counseling were invited to attend an information meeting about a smoking cessation group therapy within the center. Pharmacotherapy was provided to smokers at the discretion of their healthcare provider.
Measures
Baseline data were collected through the Vive Sin Tabaco… ¡Decídete! tool and included sociodemographic variables such as age, gender, education level, marital status, and type of health insurance and smoking characteristics, including number of cigarettes smoked per day, motivation to stop smoking, physical, situational, and psychological dependence on smoking,18,19 number of previous quit attempts, previous use of smoking cessation pharmacotherapy or counseling, and previous receipt of cessation advice from a healthcare provider. Treatment preferences (pharmacotherapy and group counseling) were collected through the tablet as part of the decision-making process.
Research staff conducted follow-up assessments through telephone call three months after the utilization of the e-Health tool. During this call, acceptability of the tool, uptake of cessation services, and cessation outcomes were collected. Acceptability measures included satisfaction questions such as “Did the use of the Vive Sin Tabaco… ¡Decídete! tool prepare you to quit smoking?” and “Would you recommend this smoking cessation tool to a friend?” Participants reported on their attendance at cessation counseling sessions. Participants were asked about their current number of cigarettes smoked per day and their 7-day point-prevalence abstinence. A qualitative interview was conducted at follow-up to assess participants' perceptions of the weaknesses and strengths of the Vive Sin Tabaco… ¡Decídete! tool.
Analysis
Simple frequencies and percentages were calculated for categorical variables, including the number and percentage of smokers who used and completed the tool and those who had quit at 3-month follow-up assessment. For continuous variables, means and standard deviations were obtained. A paired-sample t test was used to compare the pre- and postintervention mean number of cigarettes per day among continuing smokers. Statistical significance was based on a two-sided α ≤ 0.05. All analyses were performed using SPSS 22.20
Results
Of 164 participants who consented to participate, 2 were ineligible (1 due to age and 1 due to their smoking status) (Fig. 1). Participants' age at baseline ranged from 18 to 87 years (M = 49.9; SD = 15.13); 52.5% were women, 47.5% were married, and 68.5% had at least a high school education. While the majority of participants were light smokers (smoked ten or fewer cigarettes per day), smoking dependence varied depending on the scale used.18,19,21 According to the Fagerstrom test, 48.1% had no or low nicotine dependence (scores between zero and two). Psychological dependence on smoking was rated as low or mild among 62.1% of participants,19 whereas 86.4% were rated as moderate to high on situational smoking dependence18 (Table 1).
Fig. 1.
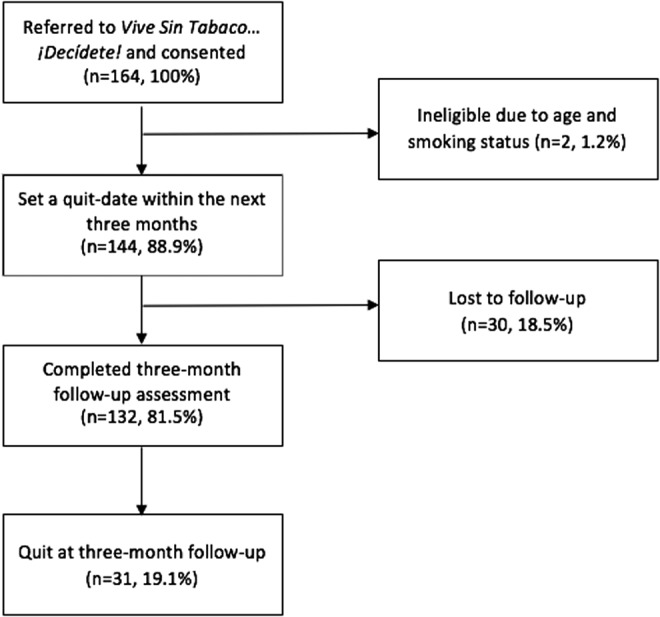
Web-based e-health smoking cessation intervention flow in primary healthcare clinics.
Table 1.
Sociodemographic Characteristics of the Sample at Baseline
| PARTICIPANT CHARACTERISTICS (N = 162) | TOTAL |
|---|---|
| Age at study enrollment, mean (SD) | 49.9 (15.0) |
| Women, n (%) | 85 (52.5) |
| Level of education, n (%) | |
| Less than high school graduate | 49 (31.4) |
| High school graduate or GED | 35 (22.4) |
| Some post high school education or technical school | 35 (22.4) |
| College graduate or more | 37 (23.7) |
| Marital status, n (%) | |
| Married | 77 (47.5) |
| Single | 37 (22.8) |
| Separated/divorced | 26 (16.0) |
| Widowed | 8 (4.9) |
| Cohabitating | 14 (8.6) |
| Amount of tobacco use at baseline | |
| Nondaily | 26 (16.0) |
| Daily, 1–10 cpd | 97 (59.9) |
| Daily, 11–20 cpd | 35 (21.6) |
| Daily, 21 or more cpd | 4 (2.5) |
| FTND—Fagerstrom Test for Nicotine Dependence21 | |
| No dependence (0) | 30 (18.5) |
| Low dependence (1–2) | 48 (29.6) |
| Moderate dependence (3–5) | 52 (32.1) |
| High dependence (6–8) | 30 (18.5) |
| Very high dependence (9–10) | 2 (1.2) |
| TAPS—Test to Assess the Psychological Dependence on Smoking19 | |
| Low dependence (8–13) | 100 (62.1) |
| Moderate dependence (14–19) | 59 (36.6) |
| High dependence (20–24) | 2 (1.2) |
| ISSS—Issa Situational Scale Score18 | |
| Low dependence (0–1) | 22 (13.6) |
| Moderate dependence (2–3) | 81 (50.0) |
| High dependence (4) | 59 (36.4) |
GED, general educational development test.
Before the use of Vive Sin Tabaco… ¡Decídete!, 63.0% of the 162 participants reported having made at least one quit attempt in the prior year; 35.8% had received advice to quit smoking from a healthcare provider during the 12 months before the intervention. Previous use of any kind of smoking cessation pharmacotherapy among the participants in their lifetime was 17.3%, and only 9.9% of participants had used professional counseling for smoking cessation (Table 2).
Table 2.
Utilization of Pharmacotherapy, Counseling, Setting a Quit Date, and Discussion with Provider Prior and Immediately After the Intervention and 3-Month Follow-Up
| PARTICIPANT CHARACTERISTICS (N = 162) | PRIOR TO INTERVENTION (N = 162) | INTEREST IMMEDIATELY AFTER INTERVENTION (N = 162) | 3-MONTH FOLLOW-UP (N = 132) |
|---|---|---|---|
| Pharmacotherapy, n (%) | 28 (17.3) | 135 (83.3)a | No data |
| Counseling, n (%) | 16 (9.9) | 151 (93.2) | 26 (19.7) |
| Quitting, n (%) | 102 (63.0)b | 144 (88.9)c | 31 (19.1)d |
| Discussion with provider, n (%) | 58 (35.8) | 156 (96.3)e | No data |
At least a 4 on a 0–10 scale of interest in using pharmacotherapy.
At least one previous quit attempt in the last 12 months.
Setting a quit date which is within the following 3 months.
Intention-to-treat analysis for self-reported 7-day point prevalence abstinence.
At least a 4 on a 0–10 scale of interest in quitting.
After using Vive Sin Tabaco… ¡Decídete!, 156 participants (96.3%) reported interest in quitting, and 144 (88.9%) set a quit date within the following 3 months. Most participants were interested in using pharmacotherapy (83.3%) and counseling (93.2%).
At 3 months, follow-up was completed on 132 (81.5%) of participants. Of these respondents, 26 (19.7%) reported that they had participated in smoking cessation group counseling. Of those who did not attend counseling sessions, 44.5% reported not doing so because of the incompatibility with their schedule. A total of 126 (95.4%) reported that they would recommend Vive Sin Tabaco… ¡Decídete! to a friend, and 97 (73.5%) thought that using the tool prepared them to make the decision to quit smoking. For those who thought that the tool did not prepare them to quit smoking, some reasons reported included: competing mental health issues, lack of information from the tool, and not enough clarity from the videos.
Open-ended comments from participants (Table 3) indicated that the program appeared to motivate smokers to quit, helped them identify a quit date, and gave them new information about cessation resources. Smokers also appeared to appreciate the innovative nature of the program. Limitations included difficulties with Wi-Fi connections and problems fitting follow-up counseling sessions into their schedules.
Table 3.
Weaknesses and Strengths of Vive Sin Tabaco… ¡Decídete!, the Web-Based e-Health Smoking Cessation Tool
| STRENGTHS | WEAKNESSES |
|---|---|
| Motivation to quit smoking “It [the mobile tool] got me to think and say ‘Now I'll make it’. I know that I need help and that's why I'm here…” Male, 64 years old “It [the mobile tool] motivated me. How wouldn't it? ‘Life without tobacco’… Of course I'd like that.” Male, 63 years old “I wasn't even thinking about quitting. I was at the clinic for my husband's medical appointment when I saw the kiosk… Yes, I wanted to use it.” Female, 57 years old |
Weak integration to accessible smoking cessation resources “He [referring to her husband] came to join the [group counseling] program but lost hope because the group had already been created and he had to wait until a new one was formed. He said ‘Now that I was ready… I wish I didn't have to wait’.” Woman, 30 years old “The group [group counseling] takes place very far away from my home. I couldn't attend…” Male, 51 years old “For my budget… It was good to hear about the different medications, but some of them are out of my budget.” Male, 51 years old “…It turned out that the sessions [group counseling] were on Tuesdays and that's when my daughter has to go to the psychologist. It didn't fit into my schedule… That's why I didn't even start the program.” Woman, 58 years old “…I'm sure that [the group counseling program] would help but the schedule didn't work for me. I'm working at that time.” Man, 63 years old |
| Helps to select a quit date “I decided to quit smoking on May 10th [Mother's Day]. I wanted something special…” Male, 64 years old | |
| Is innovative “I saw it [the mobile tool] and it caught my attention. I wanted to quit smoking right away” Female, 19 years old | |
| Is personalized “It [the mobile tool] was personalized… I was taken into consideration… Other people don't smoke for the same reasons I do. The medication someone else needs might not be the one I need” Female, 63 years old | |
| Educates about smoking cessation resources “Knowing about the medications and therapies was very helpful. I wanted to hear everything about it” Male, 63 years old “Hearing the testimony [from the former smoker] and about the medications available helped me a lot” Female, 35 years old “The testimony [from the former smoker] and the videos talking about the medication were very helpful” Male, 68 years old |
Depends on Wi-Fi connection “I couldn't watch all the videos, something was wrong with the Wi-Fi connection. I wish I could have seen all the videos…” Male, 63 years old |
The 7-day point prevalence abstinence at 3 months, using intention-to-treat analysis (assuming nonrespondents did not quit) was 19.1% (31 of 162) (per protocol 7-day point prevalence abstinence was 23.5%). Among continuing smokers, the average number of cigarettes per day decreased from 9.6 (SD 6.6) at baseline to 6.5 (SD 4.7) at 3-month follow-up (p < 0.001).
Discussion and Conclusion
This study tested a low-cost, scalable smoking cessation decision-support e-Health tool designed for smokers in Mexico. Our findings showed that the Vive Sin Tabaco… ¡Decídete! tool was feasible and acceptable for use by Mexican smokers presenting at a primary healthcare center. All eligible participants completed the intervention; participants reported high levels of satisfaction, and most would recommend it to a friend. Our study showed that it was feasible to integrate this tool into the clinical workflow of the healthcare center. We found that ∼2 out of 10 smokers using the tool quit smoking, similar to 2 comparable studies conducted in the U.S., one with Latino smokers and one with socioeconomically disadvantaged smokers.13,14
Substantial international debate about the potential of e-Health to make major impacts in improving the health in LMICs has been taking place. A recent report concluded that e-Health can have a major impact on quality and access to healthcare in LMICs.22 Our study appears to corroborate this report. In two primary healthcare centers, use of Vive Sin Tabaco… ¡Decídete! linked smokers with evidence-based cessation services offered through the Mexican healthcare system.
An e-Health intervention for smoking cessation in Mexico can only be effective if it is properly deployed to reach smokers in need of evidence-based services. In Mexico, the most logical setting for e-Health deployment is the primary healthcare system. Primary healthcare systems follow established guidelines for the identification and treatment of smokers.8 However, implementation of these cessation guidelines have been limited due to the lack of time during routine care, inadequate training of personnel, and by competing patient needs.19 e-Health tools have the potential to overcome these barriers and increase the integration of smoking cessation in primary healthcare centers.12 These tools can provide an innovative, credible, and trustworthy source of information and reduce barriers to quitting.23 Consistent with previous studies, we found that a high proportion of participants are interested in quitting. After using Vive Sin Tabaco… ¡Decídete!, the vast majority was interested in using pharmacotherapy and counseling. While the percentage of participants using counseling at follow-up was low, it is important to note that the percentage of participants who had used smoking cessation counseling in their lifetime was even lower before using Vive Sin Tabaco… ¡Decídete!
The present study has several limitations. First, the study design did not include a comparison group, which would have allowed us to assess efficacy. However, the aims of the study were to assess the feasibility and acceptability of the intervention before randomization. Second, participants were self-identified smokers who agreed to participate in a research study, which excludes some low intensity smokers as they do not consider themselves smokers.24 The study did, however, include smokers at all stages of readiness to quit, many of whom have been excluded in previous studies. Third, biomarkers were not used to verify smoking status, making it possible that actual quitting rates were lower. Fourth, even though different pharmacological and psychotherapy treatment options were explained in the tool, the number of options available to most patients was limited to the ones currently available in the clinic. Finally, this study was conducted at two clinics with wireless internet capacity; many healthcare clinics in Mexico still lack high speed internet connections, especially in rural areas.
Future studies should consider testing Vive Sin Tabaco… ¡Decídete! as part of a randomized controlled trial with a larger number of participants to assess the efficacy of this e-Health smoking cessation platform. As almost half of the participants, who did not attend group counseling cessation sessions, reported not doing so due to incompatibility with their schedules, future studies should link Vive Sin Tabaco… ¡Decídete! to other counseling resources that can be adapted to the time constraints of participants such as telephone quit lines or text-message interventions.25–27 These programs could be tailored to smoking behaviors and characteristic information provided by participants using the tool.
The Vive Sin Tabaco… ¡Decídete! smoking cessation tool appears to be feasible to deploy in a primary healthcare clinic. The tool can provide critical information to the healthcare provider and appears to be acceptable to patients. e-Health smoking cessation tools such as Vive Sin Tabaco… ¡Decídete! have the potential to address concerns cited by healthcare providers regarding their lack of time for addressing smoking cessation and have the potential to link patients to evidence based cessation services—services currently covered by the Mexican healthcare system.
Acknowledgments
Work was supported by grant SALUD-2013-01-201533 from Consejo Nacional de Ciencia y Tecnología (CONACYT) (English: National Council of Science and Technology). The authors acknowledge the research team from the Instituto Nacional de Salud Pública (María Guadalupe Flores Escartín and Moisés Ortiz), software developers (Davor Peic and Carlos Mayoral Romero), video and logo designers (Marco Polo Ramírez, René Navarro, and Chan Shigematsu), video place support (Francina Bolaños, MD; and José Alfredo Santibañez, MD), data base management and analysis (Miguel Ángel Reyes, MPH; and Javier Pruñonosa, MD, MSc), qualitative analyst (Anabel Rojas, MPH), the team from ISSSTE (Margarita Blanco, Blanca de la Rosa, Héctor Morales, and Lydia Cecilia López), the directors and chairs of the healthcare clinics (Luis Alberto Blanco, Martha Medina, Felipe Ruíz, and Angélica Marina García), the research team from the University of Kansas Medical Center (Kendra Cruz, MPH; Mariana Ramírez, LMSW; and Mitzi Ramírez, BS), and the research team from the Universidad Nacional Autónoma de México (César Pliego Rosas).
Disclosure Statement
No competing financial interests exist.
References
- 1. World Health Organization. WHO Report on the global tobacco epidemic, 2017: Monitoring tobacco use and prevention policies. Geneva: World Health Organization, 2017 [Google Scholar]
- 2. Civljak M, Sheikh A, Stead LF, Car J. Internet-based interventions for smoking cessation. Cochrane Database Syst Rev 2010;9:CD007078. [DOI] [PubMed] [Google Scholar]
- 3. Velicer W, Fava JL, Prochaska JO, Abrams DB, Emmons KM, Pierce JP. Distribution of smokers by stage in three representative samples. Prev Med 1995;24:401–411 [DOI] [PubMed] [Google Scholar]
- 4. Pan American HealthOrganization, Instituto Nacional de SaludPublica. Global adult tobacco survey. Mexico 2015 [In Spanish]. Cuernavaca, Mexico: INSP/PAHO, 2017 [Google Scholar]
- 5. National Commission for Social Protection in Health-Popular Insurance. Universal catalog of health services 2012 [In Spanish]. Mexico City: Federal Government of Mexico, 2012 [Google Scholar]
- 6. Mexican Social Security Institute, Direction of Medical Benefits Medical CareUnit. Basic drugs list [In Spanish]. Juarez, Mexico: Mexican Social Security Institute, 2015 [Google Scholar]
- 7. Institute for Social Security and Services for State Workers. Health services [In Spanish]. 2015. Available at: http://sgm.issste.gob.mx/medica/# (last accessed April20, 2018).
- 8. The Secretariat of Health. Prevention, diagnosis and treatment of tobacco consumption and second-hand smoke in the first level of care [In Spanish]. Mexico City: The Secretariat of Health, 2009 [Google Scholar]
- 9. Kreps GL, Neuhauser L. New directions in eHealth communication: Opportunities and challenges. Patient Educ Couns 2010;78:329–336 [DOI] [PubMed] [Google Scholar]
- 10. Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev 2010;32:56–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ponciano-Rodríguez G. The urgent need to change the current medical approach on tobacco cessation in Latin America. Salud Pública Méx 2010;52(Suppl 2):S336–S372 [DOI] [PubMed] [Google Scholar]
- 12. Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Thomson R, Trevena L. Decision aids for people facing health treatment or screening decisions. Cochrane Database Sys Rev 2014;4:CD001431. [DOI] [PubMed] [Google Scholar]
- 13. Brunette MF, Ferron JC, McHugo GJ, Davis KE, Devitt TS, Wilkness SM, Drake RE. An electronic decision support system to motivate people with severe mental illnesses to quit smoking. Psychiatr Serv 2011;62:360–366 [DOI] [PubMed] [Google Scholar]
- 14. Brunette MF Gunn W, Alvarez H.Finn PC, Geiger P, Ferron JC, McHugo GJ. A pre-post pilot study of a brief, web-based intervention to engage disadvantaged smokers into cessation treatment. Addict Sci Clin Pract 2015;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cupertino AP, Richter K, Cox LS, Garrett S, Ramirez R. Mujica F, Ellerbeck EF. Feasibility of a Spanish/English computerized decision aid to facilitate smoking cessation efforts in underserved communities. J Health Care Poor Underserved 2010;21:504–517 [DOI] [PubMed] [Google Scholar]
- 16. Cabrera Mendoza NI, Castro Enriquez PP, Demeneghi Marini VP, et al. . mSalUV: A new mobile messaging system for diabetes control in Mexico. Rev Panam Salud Pública 2014;35:371–377 [PubMed] [Google Scholar]
- 17. Andrews L, et al. . Consumer acceptance of an SMS-assisted smoking cessation intervention: A multicountry study. Health Mark Q 2013;30:47–62 [DOI] [PubMed] [Google Scholar]
- 18. Issa JS. A new nicotine dependence score and a new scale assessing patient comfort during smoking cessation treatment. J Bras Pneumol 2012;38:761–765 [DOI] [PubMed] [Google Scholar]
- 19. Ponciano-Rodríguez G, et al. . Development and evaluation of a new self-rating Test to Assess the Psychological Dependence on Smoking (TAPDS). J Addic Med Therap 2015;3:1016 [Google Scholar]
- 20. IBM Corp. Released 2013. IBM SPSS Statistics for Windows. Version 22.0, Released 2013. Armonk, NY: IBM Corp, 2013. [Google Scholar]
- 21. Fagerstrom KO. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addict Behav 1978;3:235–241 [DOI] [PubMed] [Google Scholar]
- 22. Chetley A, et al. . Improving health, connecting people: The role of ICTs in the health sector of developing countries: A framework paper. Washington, D.C.: World Bank, 2016. infoDev Working Paper No. 7 [Google Scholar]
- 23. Willemsen MC, et al. . Helping smokers to decide on the use of efficacious smoking cessation methods: A randomized controlled trial of a decision aid. Addiction 2006;101:441–449 [DOI] [PubMed] [Google Scholar]
- 24. Guillory J, Lisha N, Lee YO, Ling PM. Phantom smoking among young adult bar patrons. Tob Control 2017;26:153–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Whittaker R, McRobbie H, Bullen C, Borland R, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation (Review). Cochrane Database Sys Rev 2012;11:CD006611. [DOI] [PubMed] [Google Scholar]
- 26. Wetter DW, et al. . Reaching and treating Spanish-speaking smokers through the National Cancer Institute's Cancer Information Service. A randomized controlled trial. Cancer 2007;109(2 Suppl):406–413 [DOI] [PubMed] [Google Scholar]
- 27. Ybarra ML, Holtrop JS, Prescott TL, Strong D. Process evaluation of a mHealth program: Lessons learned from Stop My Smoking USA, a text messaging-based smoking cessation program for young adults. Pat Educ Couns 2014;97:239–243 [DOI] [PMC free article] [PubMed] [Google Scholar]


