Abstract
Background: Latinos with end-stage renal disease (ESRD) have worse mental and kidney composite health-related quality of life (HRQOL) scores compared to non-Latino ESRD patients. Latino ESRD patients uniquely report that social factors (e.g., lack of care coordination, food insecurity, and low health literacy) and mental health influence their HRQOL. We developed a culturally tailored peer navigator (PN) intervention to improve the HRQOL of Latinos on hemodialysis.
Objective: To determine the feasibility of the PN intervention.
Design: Single-arm prospective study. The PN provided individualized support with advance care planning, care coordination, and counseling about the importance of diet and mental health.
Setting and Participants: Latino with ESRD receiving scheduled outpatient thrice-weekly hemodialysis or reliant on emergency-only hemodialysis in Denver.
Main measures: Recruitment, retention rates, data completeness, intervention dose, patient- and staff-reported satisfaction with the intervention.
Results: Of 49 eligible patients, 40 (82%) agreed to participate. The majority of participants received scheduled outpatient hemodialysis (75%), 20 were women (50%), with a mean (standard deviation [SD]) age of 56 (13) years. No participants withdrew from the intervention. One participant died. The mean (SD) number of PN visits per participant was 7 (2) and the mean (SD) length of the visits was 97 minutes (49). The majority of visits took place at the hemodialysis facility (59%) and home (27%). The vast majority of participants reported that the PN improved their quality of life as a patient on hemodialysis (95%).
Conclusions: The PN intervention achieved feasibility goals and was well received by participants.
Keywords: health-related quality of life, hemodialysis, Latinos, patient navigators, renal failure, undocumented immigrants
Introduction
Latinos represent 17% of the United States end-stage renal disease (ESRD) population, yet, remain underrepresented in existing ESRD research.1 Compared to the general United States population, patients with ESRD have a lower life expectancy, lower health-related quality of life (HRQOL), and a symptom burden similar to patients with advanced cancer.2–9 Multiple factors (e.g., symptom burden, mental health) associated with ESRD can affect HRQOL. In Latinos, these concerns are compounded by cultural factors (i.e., behaviors and values), social factors (i.e., socioeconomic status, health literacy), and access to hemodialysis (i.e., undocumented immigrants rely on emergency-only hemodialysis).4,10,11–14
A peer navigator (PN) intervention that provides individualized support by addressing patient-identified barriers and facilitators to care within a dialysis center has the potential to improve HRQOL. A PN (i.e., patient navigator, community health worker, lay health worker, or promotora) is a culturally and linguistically congruent individual who helps patients achieve their health care goals by helping them overcome modifiable barriers and facilitating the interaction between the patient and the health care system. The objective of this study was to assess the feasibility and acceptability of a PN intervention for Latino patients with ESRD receiving scheduled or emergency-only hemodialysis.
Methods
Design
This is a prospective, single-arm study conducted from January 2016 to December 2017 to assess the feasibility of a large-scale randomized controlled trial (RCT). The Colorado Multi-institutional Review Board approved this study.
Setting and participants
Participants were recruited from January 2016 to May 2017 at an inpatient dialysis center at a safety-net hospital, and at an outpatient inner city dialysis center in Denver, Colorado. Eligible participants were English or Spanish-speaking Latinos with ESRD receiving scheduled thrice-weekly outpatient hemodialysis or emergency only hemodialysis (EOHD). EOHD patients are undocumented immigrants with ESRD who must meet critically illness criteria (e.g., high potassium; uremic symptoms; and/or severe shortness of breath) to receive hemodialysis, while admitted to hospital. Patients were excluded from the study if they were <18 years of age, not Latino, pregnant, incarcerated, or lacked decisional capacity.
PN intervention
A community advisory panel composed of patient and caregiver stakeholders provided guidance on the tailoring of the PN intervention, informed by our previous research on the HRQOL preferences and needs of Latino ESRD patients.10,13,14 The PN intervention focused on four domains: (1) advance care planning (ACP); (2) care coordination; (3) dietary support; and (4) mental health support (Appendix Table A1). We chose a maximum of five planned visits based on preliminary studies.15 The PN continued to be available to participants if they requested additional visits.
PN training
The PN, a Latina fluent in English and Spanish, had personal experience as a caregiver for her ESRD family member. The PN also had previous experience in the health-related field as a medical Spanish interpreter for a safety-net hospital for four years and training as a certified nurse assistant. The PN was trained in motivational interviewing and navigator fundamentals through the Colorado Patient Navigator Training Program.16
Outcome measures and data collection
The primary outcomes were feasibility and acceptability. To assess feasibility, we tracked recruitment and retention, intervention implementation, data collection, and intervention delivery (e.g., number of visits, visit duration, and visit content through detailed field notes). To measure patient acceptability, we used a modified version of the Patient Navigation Process and Outcomes Measure.15 To measure dialysis center staff acceptance, we conducted semistructured interviews.
Exploratory measures were collected at baseline and study completion. Measures included the following: (1) Kidney Dialysis Quality of Life Short Form (KDQOL-SF 36)17,18; (2) Modified Edmonton Symptom Assessment Scale (ESAS-r:Renal)19; (3) Patient Health Questionnaire-9 (PHQ-9); and (4) Generalized Anxiety Disorder-7 (GAD-7). To assess acceptability, L.C. conducted semistructured interviews with the PN and hemodialysis center staff. Interviews were audio recorded and transcribed.
Statistical analysis
Descriptive analyses were conducted using SAS Enterprise Guide 5.1 (SAS Institute, Inc., 2012). For continuous and normally distributed data, we calculated means with standard deviation (SD). Numeric counts with a percent were calculated for categorical variables. Our study was not powered to detect changes of exploratory measures, and we thus provide the results at baseline only. ATLAS.ti software (version 8.0.27.0) was used for thematic analysis of transcribed interviews.
Results
In total, 40 (30 scheduled hemodialysis and 10 EOHD) participants were enrolled. Participants had a mean (SD) age of 56 (13), a mean (SD) Charlson Comorbidity Index of 7.2 (2.7), 20 (50%) were female, and 28 (70%) were primarily Spanish-speaking (Table 1). Nearly one-third of participants had at least moderate depression (PHQ-9 ≥ 10) and/or moderate anxiety (GAD-7 ≥ 10). The ESAS-r: Renal showed that patients report a mean (SD) of 6 (3) symptoms, of which 4 (4) were moderate to severe.
Table 1.
Patient Characteristics
| Characteristic | All patients |
|---|---|
| N = 40 | |
| Age, mean (SD), years | 56 (13) |
| Male gender, n (%) | 20 (50) |
| Hispanic/white, n (%) | 40 (100) |
| Language, n (%) | |
| Spanish | 28 (70) |
| English | 12 (30) |
| Did not complete high school, n (%) | 25 (63) |
| Married/domestic partner, n (%) | 16 (40) |
| Employed, n (%) | 2 (5) |
| Income, n (%) | |
| Less than $15K | 33 (83) |
| $15–30K | 7 (17) |
| History of diabetes, n (%) | 30 (75) |
| History of CVD, n (%) | 7 (18) |
| Charlson comorbidity index score, mean standard deviation | 7.2 ± 2.7 |
| Laboratory values, mean (SD) | |
| Creatinine, mg/dL | 8.9 (3.7) |
| Serum albumin, g/dL | 3.7 (0.5) |
| Hemoglobin, g/dL | 10.4 (1.9) |
| Phosphorus, mg/dL | 4.8 (1.4) |
| KDQOL-36 SF, mean (SD) | |
| Burden of kidney disease | 33 (27) |
| Symptoms/problems | 68 (21) |
| SF-12 physical health composite | 33 (1) |
| SF-23 mental health composite | 45 (13) |
| PHQ-9, median (IQR) | 4 (1,10) |
| PHQ-9 ≥ 10, n (%) | 13 (30) |
| ESAS-r:Renal, mean (SD) | |
| Symptoms present | 6 (3) |
| Symptoms moderate/severe | 5 (4) |
| GAD-7, median (IQR) | 4 (1, 9) |
| GAD-7 ≥ 10, n (%) | 10 (25) |
SD, standard deviation; KDQOL-SF, Kidney Dialysis Quality of Life Short Form; ESAS-r:Renal Modified Edmonton Symptom Assessment Scale; PHQ-9, Patient Health Questionnaire-9; GAD-7, Generalized Anxiety Disorder-7; IQR, interquartile range; CVD, cardiovascular disease.
Feasibility
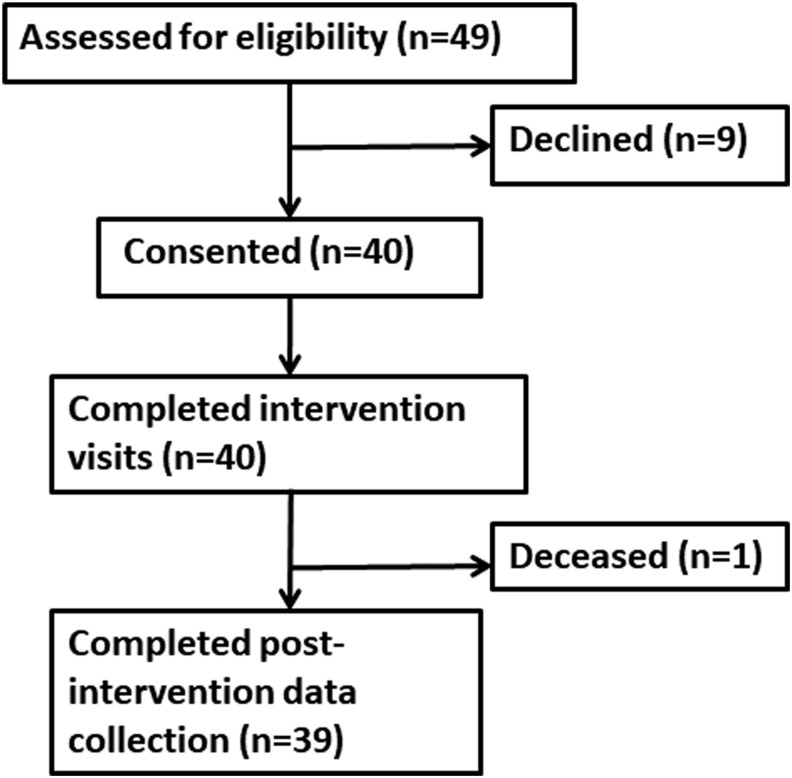
With respect to feasibility, 49 patients were approached and 40 (82%) agreed to participate. Of the 40 participants, none withdrew, and data collection was complete except for one participant who died (Fig. 1). Nearly all (95%) participants completed the five-visit protocol within 90 days. Overall, the mean (SD) number of visits was 7 (2), and the mean (SD) length of the visits was 97 (49) minutes. The majority of visits took place at the dialysis facility (59%) or the participant's home (27%) (Table 2).
FIG. 1.
Study flow diagram.
Table 2.
Intervention Feasibility
| All patients | |
|---|---|
| Outcome/measure | N = 40 |
| Retention, n % | |
| Completed peer navigator visits, n (%) | 40 (100) |
| Completed follow-up data collection, n (%) | 39 (98) |
| Implementation, n % | |
| First visit occurred within 14 days of enrollment, n (%) | 15 (38) |
| Patients completed all five visits within 90 days, n (%) | 38 (95) |
| Intervention dose | |
| Number of navigator visits, mean (SD) | 7 (2) |
| Length of navigator visits, minutes, mean (SD) | 97 (49) |
| Location of navigator visits | |
| Home, n (%) | 57 (27) |
| Dialysis center, n (%) | 126 (59) |
| Other, n (%) | 32 (14) |
Acceptability
The majority of participants felt that the PN improved their quality of life (95%), provided emotional support (100%), and helped them make important decisions about care (100%) (Table 3). When asked about the domains, the majority reported having discussed ACP (90%), diet (92%), mental health (95%), and having received social support with basic resources (e.g., food, housing, disability, and transportation paperwork) (95%). All dialysis center staff interviewed agreed that the intervention was well received by patients (Table 4). Staff also reported an increase in the number of patients listed for a kidney transplant and improvement of renal therapy adherence. The PN identified a major challenge in supporting depressed participants to seek mental health treatment due to a mix of cultural preferences and communication barriers.
Table 3.
Patient Acceptability, Patient Navigation Process Outcomes Measure
| Peer navigator intervention overall, n (%) | |
|---|---|
| The number of peer navigator visits was… | |
| About right | 26 (67) |
| Too many | 0 |
| Not enough | 13 (33%) |
| My peer navigator provides emotional support, yes | 39 (100) |
| Improved my quality of life, yes | 37 (95) |
| Improved the health care I received as a patient on dialysis, yes | 37 (95) |
| I would recommend the peer navigator intervention, yes | 39 (100) |
| Care coordination, n (%) | |
| My peer navigator… | |
| Provided resources/information that was new to me, yes | 37 (95) |
| Was helpful to my family, yes | 37 (95) |
| Figures out important issues in my health care, yes | 39 (100) |
| Helps me make important decisions about my health care, yes | 39 (100) |
| Since I started with the peer navigator intervention… | |
| I have tried to better understand my illness by asking questions of my clinicians, yes | 39 (100) |
| I have been involved with decisions or choices about my health care, yes | 37 (95) |
| Advance care planning, n (%) | |
| My navigator and I discussed advance care planning, yes | 35 (90) |
| Advance care planning can include things that are important to my culture, yes | 36 (92) |
| My navigator and I talked about hospice, yes | 31 (79) |
| I spoke with my family about the kind of care I would like to receive if I were very sick at the end of life, yes | 26 (67) |
| I spoke with my health care provider about the kind of care I would like to receive if I were very sick at the end of life, yes | 23 (59) |
| I have thought about what is most important to me and what makes my life worth living, yes | 39 (100) |
| Diet support, n (%) | |
| My navigator and I discussed how my kidney failure diet restrictions have impacted my diet, yes | 36 (92) |
| I can still make foods that are important to my traditions and culture, yes | 36 (92) |
| My navigator and I talked about how I have adjusted to the dietary changes since starting dialysis, yes | 39 (100) |
| I would recommend a navigator to talk to about the kidney diet, yes | 38 (97) |
| Mental health support, n (%) | |
| My navigator and I talked about my mental health, yes | 37 (95) |
| I would recommend a peer navigator to help with mental health symptoms, yes | 37 (95) |
| My navigator and I talked about the spiritual or religious aspects of my illness, yes | 36 (92) |
| I would recommend a navigator to help with coping and adjusting, yes | 38 (97) |
N = 39.
Table 4.
Illustrative Quotes from Acceptability Interviews
| Illustrative quotes | |
|---|---|
| Peer navigator | “I think that I was able to relate with patients culturally because patients saw me as part of their family. I also feel I was able to support them when they needed me, like going with them to social services and most important, I was able to gain their trusts because I demonstrated a genuine interest in them as individuals.” “Patients don't really have much to do during hemodialysis and I provided the social support that so many patients lack. Having someone to talk to about everything and anything is a huge things for most of the patients.” “Several patients count on family but they can't attend kidney transplant visits because of competing demands. Patients relied on my knowledge of the medical system and my interpretation skills gave them the reassurance that I would professionally interpret for them.” |
| Dialysis center staff | “The patients miss her since your study ended. They ask about her. I think it was nice to have a navigator come in and say, ‘How's your day been?’ because I think a lot of times we go and quickly say to patients, ‘this is your baseline, these are your labs, and here's what your fluid is doing’ and we forget that they are not numbers, they are human” “The patients looked forward to seeing her. To be honest, we're disappointed that the study is over.” “The patients miss her. She had rapport. She was a good advocate for our patients. We need to see how we can implement this patient navigator program now that your study is done because we need her.” “I think it really helped with our patient adherence, coming to hemodialysis treatments and kidney transplant appointments…the patients requested more time with the patient navigator, more than the five visits.” “We had a lot of transplants this year and I know that the patient navigator is the reason. She went to kidney transplant appointments with them, she had conversations with them and she made phone calls for them…just going with them that initial visit, it's so beneficial. The transplant part of it was huge. There's nobody that speaks Spanish that answers the phone for transplant clinic appointments. Many patients say that they call and no one calls back or they call back but they don't understand English and the transplant clerk doesn't speak Spanish. The patient navigator will be missed” “The patient navigator went to some patient's homes and actually went with them to buy groceries and stuff. We also had a patient that was struggling with alcohol and I know that the patient navigator advocated for him to get help and treatment.” “She spoke Spanish and knew their culture which helped because I don't understand the different foods and the different ways the family interacts at home or is involved in their care. She go into the home and we can't do that. She can tell us what types of foods are in the cupboards and what the kitchen looks like or if they have someone helping them with meals. She bridge the care they receive with what is going on at home.” “They share a lot more about their problems with the patient navigator than they ever would with us. She was seen as a friend and so they are more open with her. They tell her about the things that are stressful in their home and they would never tell us. She formed a bond with them.” “She gave us feedback like, ‘this person isn't getting their medication mail delivery or that person doesn't have their supplements’ and this is important because patients don't want to bother us and don't tell us these important things” “I've been doing this for years and it was just so helpful to have the patient navigator be another set of eyes for us, and to the patient…because we're always saying ‘you need to do this and this’ and the navigator didn't, because the navigator's role is so different than ours so the patients felt closer to the navigator.” “The people are lonely at home. Seeing the patient navigator gave them something to look forward to. She understands them and can speak their language” “We use the interpreter sometimes but that's different. They don't trust the interpreter and so we don't get the whole story. With the patient navigator, they tell her the whole story, because she's a person that cares and understands them. It makes a big difference.” “We were so fortunate to have the study here…there's so many people that need this so expanding this study would be really helpful.” |
Discussion
To our knowledge, this is the first prospective culturally tailored PN program focused on improving HRQOL for Latino ESRD patients. Our findings demonstrated its feasibility and acceptability.
The high referral, enrollment, and retention rate as well as acceptability of this study are strengths. In this pilot study, the PN introduced the study and credited this initial recruitment encounter with enhancing study retention because participants developed a trusting relationship that may have facilitated subsequent visits. We designed the PN intervention to include five navigator-initiated visits for each intervention participant; however, the mean (SD) number of visits was 7 (2) and one-third of participants reported that the number of visits was “not enough” indicating a desire for ongoing support. Participants felt that the PN provided emotional support, improved their lives, and/or the health care they received. Our findings are consistent with the emotional support reported in a systematic review of the experiences of cancer patients in navigation programs.20
One of the challenges faced by the PN was in supporting participants who faced depression and anxiety. Previous research demonstrated that patients with mental health issues did not want medications and did not want to see a psychiatrist or psychologist due to social stigma and their demanding hemodialysis schedule.10,13,14 In our study, the PN used motivational interviewing to connect participants to mental health services; however, participants were reluctant to follow-up with mental health care. An innovative approach that aligns with Latino ESRD participant preferences is Chairside Cognitive Behavioral Therapy (CCBT) delivered by a Licensed Clinical Social Worker during hemodialysis. In a small RCT of CCBT, English-speaking ESRD patients randomized to CCBT had a reduction in self-reported depression, greater improvement in HRQOL, and hemodialysis fluid adherence.21 These findings are promising; however, more research is needed on the use of CCBT for minority ESRD groups.
Navigator programs have been highlighted by the nephrology community as an important strategy to address inequities.22 Ethnic minorities are disproportionately burdened with both a high prevalence of ESRD and face inequities in various ESRD outcomes, including end-of life care.14,23 For example, compared to non-Latino Whites, Latino ESRD patients are less likely to report engagement in a conversation about ACP.23 When examining patterns of end-of life care, Latino ESRD patients with a hospital death are more likely to receive intensive procedures during their last hospitalization.24 In our study, the majority of participants reported having a conversation about ACP with their PN and their health care provider. Having a culturally congruent PN support, ACP has the potential to promote goal concordant care.
Our study has limitations, some of which are inherent to its design as a feasibility study. While this early pilot work was not powered to detect changes postintervention, we were able to demonstrate that the intervention could be successfully delivered. An additional limitation is that we had one highly invested PN who was culturally congruent with the study participants and in a single research setting. Future trials will be necessary to demonstrate fidelity in conducting the intervention and reproducibility in other hemodialysis centers,
In conclusion, we demonstrated that the PN intervention is feasible for Latinos on hemodialysis. A future multi-site RCT of the PN intervention among Latino groups could examine HRQOL, hemodialysis adherence, and kidney transplantation outcomes.
Acknowledgments
The work was supported by the Harold Amos Medical Faculty Development Award from the Robert Wood Johnson Foundation and grant 2015212 from the Doris Duke Charitable Foundation (University of Colorado School of Medicine Fund to Retain Clinical Scientists). The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the article; and decision to submit article for publication.
Appendix
Appendix Table A1. Framework for Peer Navigator Visit by Domain
| Social support | Mental health support | ||
|---|---|---|---|
| Advance care planning | Care coordination | Diet support | |
| • Discuss values and goals using motivation interviewing through empathy and reflective listening. • Review advance directive and hospice educational materials • Use motivational interviewing to help patient complete advance directives and/or have advance care planning conversations with family and clinicians. |
• Discuss concerns related to health, finances, housing, transportation, and family. • Provide support with connection to community resources, clinic appointments, language interpretation, and logistical issues. |
• Accommodate cultural dietary preferences with renal restriction. • Provide recipes that are culturally and linguistically congruent. • Activate patient to troubleshoot diet issues. |
• Explore patient methods for coping and adjustment to illness. • Use motivational interviewing, and help patient obtain mental health support. |
Author Disclosure Statement
No competing financial interests exist.
References
- 1.United States Renal Data System: Chapter 1: Incidence, prevalence, patient characteristics, and treatment modalities. (Table 1.2) Adjusted prevalence of dialysis, per million, and percentage distribution of diabetes and ethnicity among prevalent dialysis patients, by ESRD network , 2012. (Figure 1.6) Trends in (a) prevalent ESRD cases and (b) ESRD, per million/year, by Hispanic ethnicity, in the US population, 1996–2012. Annual data report 2014. 2014. http://usrds.org/2014/view/v2_01.aspx (Last accessed January21, 2015)
- 2. Davison SN, Jhangri GS: Impact of pain and symptom burden on the health-related quality of life of hemodialysis patients. J Pain Symptom Manage 2010;39:477–485 [DOI] [PubMed] [Google Scholar]
- 3. Davison SN, Jhangri GS, Johnson JA: Longitudinal validation of a modified Edmonton symptom assessment system (ESAS) in haemodialysis patients. Nephrol Dial Transplant 2006;21:3189–3195 [DOI] [PubMed] [Google Scholar]
- 4. Lopes AA, Bragg-Gresham JL, Satayathum S, et al. : Health-related quality of life and associated outcomes among hemodialysis patients of different ethnicities in the United States: The Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis 2003;41:605–615 [DOI] [PubMed] [Google Scholar]
- 5. Beddhu S, Bruns FJ, Saul M, et al. : A simple comorbidity scale predicts clinical outcomes and costs in dialysis patients. Am J Med 2000;108:609–613 [DOI] [PubMed] [Google Scholar]
- 6. United States Renal Data System: Chapter 5: Mortality. Table 5.1. Adjusted survival probabilities among ESRD patients, by months after initiation of treatment. 2014 Annual data report. 2014. http://usrds.org/2014/view/v2_05.aspx (Last accessed January30, 2015)
- 7. Landreneau K, Lee K, Landreneau MD: Quality of life in patients undergoing hemodialysis and renal transplantation—a meta-analytic review. Nephrol Nurs J 2010;37:37–44 [PubMed] [Google Scholar]
- 8. Weisbord SD, Fried LF, Arnold RM, et al. : Prevalence, severity, and importance of physical and emotional symptoms in chronic hemodialysis patients. J Am Soc Nephrol 2005;16:2487–2494 [DOI] [PubMed] [Google Scholar]
- 9. Chang VT, Hwang SS, Feuerman M: Validation of the Edmonton symptom assessment scale. Cancer 2000;88:2164–2171 [DOI] [PubMed] [Google Scholar]
- 10. Cervantes L, Zoucha J, Jones J, Fischer S: Experiences and values of Latinos with end-stage renal disease: A systematic review of qualitative studies. Nephrol Nurs J 2016;43:478–493 [PubMed] [Google Scholar]
- 11. Lora CM, Gordon EJ, Sharp LK, et al. : Progression of CKD in Hispanics: Potential roles of health literacy, acculturation, and social support. Am J Kidney Dis 2011;58:282–290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Porter AC, Vijil JC, Jr, Unruh M, et al. : Health-related quality of life in Hispanics with chronic kidney disease. Transl Res 2010;155:157–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cervantes L, Jones J, Linas S, Fischer S: Qualitative interviews exploring palliative care perspectives of Latinos on dialysis. Clin J Am Soc Nephrol 2017;12:788–798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cervantes L, Linas S, Keniston A, Fischer S: Latinos with chronic kidney failure treated by dialysis: Understanding their palliative care perspectives. Am J Kidney Dis 2016;67:344–347 [DOI] [PubMed] [Google Scholar]
- 15. Fischer SM, Cervantes L, Fink RM, Kutner JS: Apoyo con Carino: A pilot randomized controlled trial of a patient navigator intervention to improve palliative care outcomes for Latinos with serious illness. J Pain Symptom Manage 2015;49:657–665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Patient Navigator Training Collaborative: 2018. http://patientnavigatortraining.org/ (last accessed January25, 2019)
- 17. Ricardo AC, Hacker E, Lora CM, et al. : Validation of the Kidney Disease Quality of Life Short Form 36 (KDQOL-36) US Spanish and English versions in a cohort of Hispanics with chronic kidney disease. Ethn Dis 2013;23:202–209 [PMC free article] [PubMed] [Google Scholar]
- 18. Hays RD, Kallich JD, Mapes DL, et al. : Development of the kidney disease quality of life (KDQOL) instrument. Qual Life Res 1994;3:329–338 [DOI] [PubMed] [Google Scholar]
- 19. Davison SN, Jhangri GS, Johnson JA: Longitudinal validation of a modified Edmonton symptom assessment system (ESAS) in haemodialysis patients. Nephrol Dial Transplant 2006;21:3189–3195 [DOI] [PubMed] [Google Scholar]
- 20. Tan CH, Wilson S, McConigley R: Experiences of cancer patients in a patient navigation program: A qualitative systematic review. JBI Database System Rev Implement Rep 2015;13:136–167 [DOI] [PubMed] [Google Scholar]
- 21. Cukor D, Ver Halen N, Asher DR, et al. : Psychosocial intervention improves depression, quality of life, and fluid adherence in hemodialysis. J Am Soc Nephrol 2014;25:196–206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Narva AS, Norton JM, Boulware E: Education patients about CKD: The path to self-management and patient-centered care. Clin J Am Soc Nephrol 2016;11:694–703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kurella Tamura M, Goldstein MK, Perez-Stable EJ: Preferences for dialysis withdrawal and engagement in advance care planning within a diverse sample of dialysis patients. Nephrol Dial Transplant 2010;25:237–242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Eneanya ND, Hailpern SM, O'Hare AM, et al. : Trends in receipt of intensive procedures at the end of life among patients treated with maintenance dialysis. Am J Kidney Dis 2017;69:60–68 [DOI] [PMC free article] [PubMed] [Google Scholar]