Abstract
Background: Growing evidence demonstrates the benefits of early, integrated palliative care (PC) for patients with advanced cancer and their caregivers. Yet, data are lacking on the communication patterns within this model of care.
Objective: The goals of this study were to describe the content of patient–clinician discussions among patients receiving PC and to compare differences in discussion content between oncologists and PC clinicians.
Design: We conducted a qualitative observational analysis.
Setting/Subjects: We included patients with incurable lung and esophageal cancer enrolled in a randomized trial of early, integrated PC versus usual oncology care. We analyzed 68 audio-recorded clinic visits (34 oncologist visits; 34 PC clinician visits) immediately after patients' (N = 19) first and second cancer progressions. We examined themes of clinician communication, comparing the content and frequency of discussions between oncologists and PC clinicians.
Results: Although both oncology and PC clinicians discussed symptom management, medical understanding, and treatment decision making with patients at nearly all postprogression visits, PC clinicians tended to assess patient understanding of the treatment process and prognosis more often than oncologists. PC clinicians addressed patient coping, caregiver experiences and needs, and advance care planning more frequently than oncologists.
Conclusion: PC clinicians play a distinct, complementary role to oncologists in providing care for patients with advanced cancer and their caregivers. PC clinicians tend to assess and elaborate on patient understanding of prognosis and treatment and emphasize effective coping, caregiver needs, and advance care planning. These results illuminate the communication elements by which early, integrated PC may improve patient and caregiver outcomes.
Keywords: advanced cancer, communication, neoplasms, palliative care, quality of life
Background
Over the past decade, early involvement of specialty-trained palliative care (PC) clinicians in the outpatient oncology care setting has increasingly been recognized as an essential element of comprehensive care for patients with advanced cancer and those with high symptom burden.1 A number of randomized trials have shown that early PC significantly improves quality of life, symptom burden, mood, illness understanding, and quality of care at the end of life for patients with advanced cancer.2–5 Family and friends (“caregivers”) also benefit from early PC, with improvements in depression, stress burden, and social functioning.6–8 Based on this evidence, the American Society of Clinical Oncology published a provisional clinical opinion9 that was later updated in 201710 calling for the standardization of early integration of PC into the medical management of all patients with advanced cancer. Despite this increased acceptance, the specific elements of early PC are unclear,11,12 prompting calls to clarify the salient components of PC provided by clinicians.
Objective
To elucidate the essential elements of PC that may lead to improved outcomes, we conducted an in-depth qualitative analysis of audio-recorded visits from a randomized trial of early, integrated PC versus standard oncology care in patients with advanced cancer. The goals of this study were to describe the content of patient–clinician discussions among patients receiving early, integrated PC and compare differences in discussion content between oncology and PC clinicians.
Setting/Subjects
This analysis is based on a larger randomized clinical trial in which we examined the efficacy of early PC integrated with oncology care versus usual oncology care alone in improving patient-reported outcomes and end-of-life care (Clinicaltrials.gov identifier: NCT01401907). To be eligible for the trial, patients needed to be at least 18 years, diagnosed with incurable lung or noncolorectal gastrointestinal cancer in the past eight weeks, and have a stable performance status. We previously reported detailed information regarding patient eligibility, recruitment, and enrollment.13 Caregivers present at clinic visits were consented to participate though patients did not need to identify a caregiver to enroll in the study. Patients randomly assigned to the intervention group met with a specialty-trained PC physician or advance practice nurse within four weeks of enrollment and at least monthly thereafter until death. Although the content of the PC intervention visits was based on national guidelines,14 clinicians could tailor discussions to the specific care needs of patients and their caregivers. Upon providing informed consent, we requested permission from patients to audio record their oncology and PC clinic visits. The Dana Farber/Harvard Cancer Center IRB approved the study protocol.
Design and Methods
We selected 21 consecutive patients from the intervention group to include in this qualitative study. Between April 2014 and June 2016, we audio recorded two outpatient clinic visits with medical oncology and two outpatient clinic visits with PC immediately after patients' first and second cancer progressions (i.e., up to eight recordings per patient). This sample size was sufficient for our intended qualitative analyses, which allowed us to achieve informational redundancy.15 We intentionally chose to record post-progression visits because these encounters were likely to include salient discussions about cancer treatment, patient understanding of illness and prognosis, and decision making. Seven oncologists and ten PC clinicians (physicians and advance practice nurses) were included in the analyzed clinic visits. Using TranscribeMe.com, we obtained verbatim transcriptions of each audio recording.
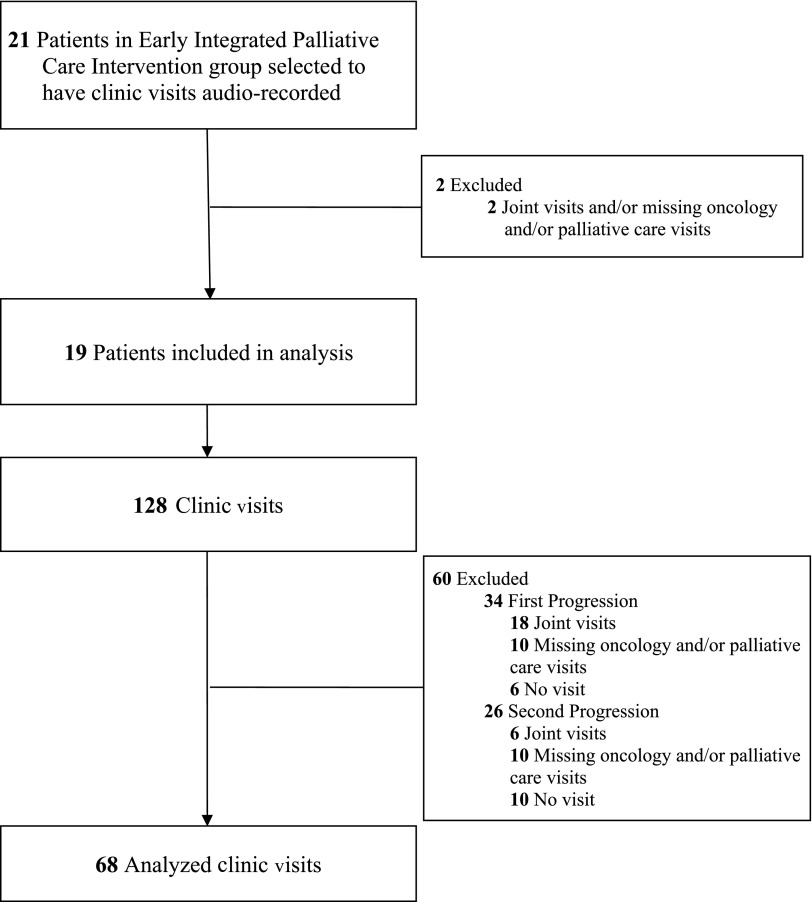
To identify and compare the unique content of conversations between each type of clinician with the patients and caregiver(s), we selected audio recordings in which the oncology and PC visits occurred separately. We were unable to analyze audio recordings in which both the oncologist and PC clinician jointly saw the patient or when a corresponding visit between oncology and PC was missing. For example, two patients did not have evaluable data for this study because they only had joint visits with clinicians post-progression or were missing either an oncology or PC visit for each of their audio-recorded visits. Most of the 19 patients with evaluable visits had two to six visits (M = 3.78 [SD = 1.67], Mode = 2) available for this analysis (N = 68 clinic visits total). Figure 1 illustrates the audio recordings included in this study.
FIG. 1.
Clinic visit audio-recording scheme.
We developed the initial coding scheme through an iterative review process using our team's prior qualitative study of the early PC intervention and expert feedback as well as audio-recorded PC visits and clinician documentation of discussions from the current trial.16 The prior qualitative coding scheme included seven key elements of PC visits including (1) relationship and rapport building, (2) addressing symptoms, (3) addressing coping, (4) establishing illness understanding, (5) discussing cancer treatments, (6) end-of-life planning, and (7) engaging family members. The primary reviewer refined this initial coding scheme by reviewing a subset of ten audio recordings from this study and adjusting the scheme based on the content of PC discussions among clinicians, patients, and caregivers during oncology and PC clinic visits. The final coding scheme (Supplementary Table S1; Supplementary Data are available online at www.liebertpub.com/jpm) included eight broad first-level codes, each comprising more detailed second- and third-level codes. Two experts including an oncologist and a clinical psychologist who specialize in PC research reviewed and confirmed the coding scheme before coding. The research team made additional minor edits to clarify specific codes throughout the coding process. Once confirmed, this coding scheme was applied to all 68 transcripts. For this analysis, we focused on the codes relevant to post-progression visits and chose not to report on two first-level codes related to initial PC visits, including “explaining the role of palliative care” and “rapport building.”
We conducted a summative content analysis. The primary reviewer coded all transcripts based on the final coding scheme. We trained a second independent reviewer (A.H.) with expertise in qualitative methods and advanced cancer populations in the coding scheme. This second reviewer independently coded a subset of transcripts (n = 7) and then met with the primary reviewer to discuss and compare the results. This comparison served to confirm that the primary reviewer was consistently applying the coding scheme to all transcripts and to ensure the trustworthiness of the coding. To assess inter-rater reliability between the two reviewers' coding, we calculated a Kappa coefficient, which ranged from 0.72 to 0.81 across transcripts, representing substantial to high reliability.17 The reviewers discussed any differences between their coding and resolved discrepancies, making adjustments and clarifications to the coding scheme. We performed all qualitative analyses using NVivo software, Version 11.
To describe and compare the topics that oncologists and PC clinicians addressed with patients and their families after cancer progression, we calculated the frequency of each first-level code across all clinic visits. We initially focused on the six first-level codes and compared the number of clinic visits in which each code was discussed (“yes/no”) by oncology and PC clinicians. Based on these comparisons, we conducted follow-up comparisons between second- and third-level codes and supplemented these comparisons with illustrative PC quotations. Finally, we calculated the mean time (range) of the patient–clinician discussions.
Results
The demographic characteristics of the 19 patients included in this analysis are reported in Table 1. The sample was predominantly female, white, and married, with a mean age of 67.11 (SD = 11.83) years. Cancer diagnoses included nonsmall-cell lung cancer (63.2%, n = 12), small-cell lung cancer (21.1%, n = 4), and esophageal cancer (15.8%, n = 3).
Table 1.
Sample Demographics
| Patient characteristics | Early, integrated palliative care patients (n = 19) |
|---|---|
| Age, mean (SD) | 67.11 (11.83) |
| Gender, n (%) | |
| Female | 11 (58) |
| Male | 8 (42) |
| Race, n (%) | |
| White | 17 (90) |
| American Indian or Alaskan Native | 2 (11) |
| Ethnicity, n (%) | |
| White, non-Hispanic | 18 (95) |
| Not reported | 1 (5) |
| Relationship status, n (%) | |
| Married or living with someone as if married | 12 (63) |
| Loss of partner/widowed | 3 (16) |
| Divorced/separated | 3 (16) |
| Single | 1 (5) |
| Highest educational level or n (%) | |
| 11th grade or less | 1 (5) |
| High school graduate or GED | 8 (42) |
| 2 years of college or associate degree | 5 (26) |
| College graduate | 3 (16) |
| Master's degree or higher | 2 (11) |
| Annual household income, n (%) | |
| <$25k | 4 (21) |
| $25–50k | 5 (26) |
| $50–100k | 2 (11) |
| $100–150k | 6 (32) |
| >$150k | 1 (5) |
| Not reported | 1 (5) |
| Cancer type, n (%) | |
| Nonsmall-cell lung | 12 (63) |
| Small-cell lung | 4 (21) |
| Esophageal | 3 (16) |
| Days between diagnosis of incurable disease and study enrollment, mean (SD) | 30.63 (15.38) |
The length of clinic visits with patients and caregivers was similar between oncology and PC. The mean time for oncology visits was 24 minutes (SD = 9 minutes, range = 7–40 minutes), whereas PC visits lasted 28 minutes on average (SD = 10 minutes, range = 8–48 minutes).
Comparison of major topics
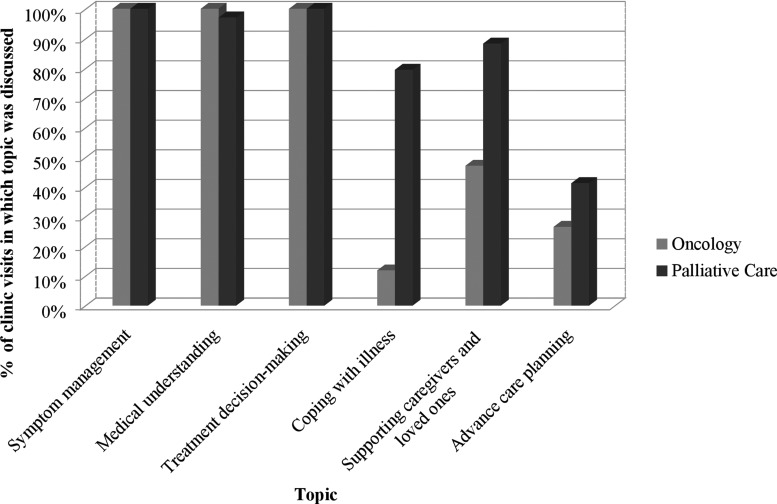
The Supplementary Table S1 illustrates the number of visits (stratified by clinician type) in which the oncologists and PC clinicians discussed specific topics. Table 2 provides representative quotations meant to illustrate several topics and elements within the coding scheme. Figure 2 shows the frequency of the major topics by clinician type. Across nearly all clinic visits, all clinicians discussed three of the six major topics, including symptom management, medical understanding, and treatment decision making. The clinicians less frequently and consistently addressed the three remaining topics during visits (i.e., coping with illness, supporting caregivers and loved ones, and advance care planning).
Table 2.
Representative Quotations of Topics and Elements
| Topic and element | Quotation | Purpose and effect of palliative care clinician's statement |
|---|---|---|
| Medical understanding | ||
| Assess patients' and caregivers' understanding and expectations of treatment process | “Tell me a little bit about what brought you—I've read in the notes, but I'd love to hear what brought you into the ER.” | Asked a patient to describe his understanding of what precipitated a recent emergency department visit and review the patient's recent hospitalization. |
| “What were the results? What's your understanding of the results of those CT scans?” | Asked the same patient as above to describe his interpretation of recent scan results, which prompted a lengthy dialogue about the patient's declining health and his concerns about the future, and the palliative care clinician sensitively responded to his worries while also helping him make decisions about treatment and symptom management. | |
| Assess patients' and caregivers' understanding of prognosis | “When someone shares with you that they think that [you will not make] it to the holidays, what was your guys' understanding of that comment?” | Asked immediately after an oncology visit in which a patient learned that he had a prognosis of only a few months, this question prompted the patient to reflect on the seriousness of his worsening health and reveal his internal conflict over the possibility of death. |
| Treatment decision making | ||
| Clarify patient experience | “I can imagine things have been hard. Can you share with me what you're thinking right now?” | Asked a patient to share his thoughts to understand the patient's experience and encourage open discussion. |
| Validating patients' values and concerns | “When you're feeling well, what's important to you? How do you want to spend your time because that helps guide me, so I'm making sure that we've got our eye on the prize about helping you live the way you want to live?” | Asked a patient to describe her values and priorities to focus care on the specific needs of the patient. |
| Coping with illness | ||
| Using social support | “You're kind of a pragmatist—you kind of see what needs to be done and you march forward. I'm just wondering when you're feeling worried or sad or anxious or not certain about what the path is, do you have folks that you can turn to?” | Asked if the patient had enough social support to help her cope emotionally after noticing that the patient was juggling major treatment decisions, multiple ongoing symptoms, and a hectic family life. |
FIG. 2.
Frequency of six major topics by clinician type.
For each topic, we present the number and percentage of visits in which each topic was discussed out of the total of 68 visits. To compare frequency of discussions by clinician type, we also report the number and percentage of visits in which clinicians discussed certain topics out of the 34 oncology and 34 PC visits.
Symptom management
All visits (100.0%, n = 68/68) included the assessment of symptoms and almost all (95.6%, n = 65/68) included the treatment of symptoms. Clinicians most often assessed the following symptoms: dyspnea/cough (79.4%, n = 54/68), appetite (66.2%, n = 45/68), pain (64.7%, n = 44/68), gastrointestinal/genitourinary symptoms (63.3%, n = 43/68), and fatigue (55.9%, n = 38/68). With respect to treatment of symptoms, the frequency of discussions varied somewhat by clinician type. Specifically, PC clinicians more frequently addressed pain (64.7%, n = 22/34 vs. 52.9%, n = 18/34), gastrointestinal/genitourinary symptoms (64.7%, n = 22/34 vs. 32.4%, n = 11/34), and fatigue (47.1%, n = 16/34 vs. 23.5%, n = 8/34), whereas the oncologists were more likely to address nausea/vomiting (29.4%, n = 10/34 vs. 17.6%, n = 6/34). All clinicians had approximately equal number of visits that addressed the treatment of dyspnea/cough (PC = 29.4%, n = 10/34 vs. oncology = 32.4%, n = 11/34).
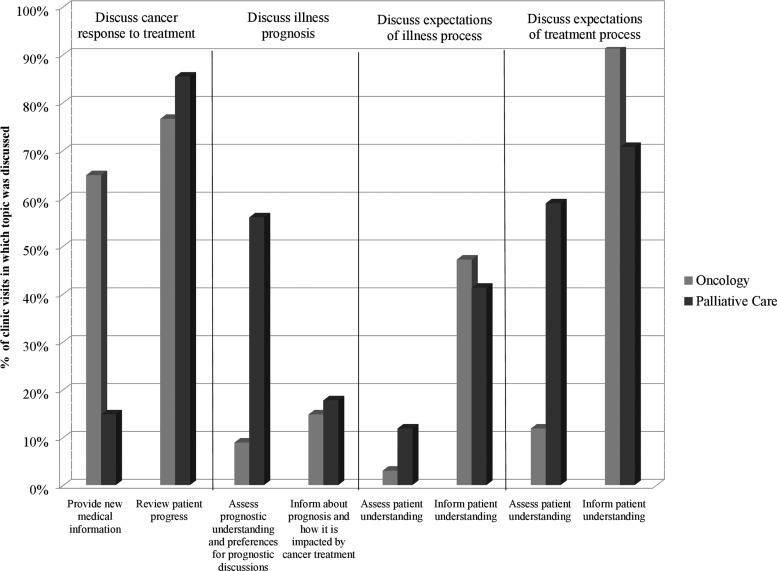
Medical understanding
Clinicians and patients discussed medical understanding at every oncology visit (100.0%, n = 34/34) and almost all PC visits (97.1%, n = 33/34). Figure 3 illustrates the frequency by which clinicians addressed each element within this topic. Regardless of clinician type, most visits included discussions concerning the cancer's response to treatment (88.3%, n = 60/68) and patients' and caregivers' expectations and understanding of the treatment process (85.3%, n = 58/68). Clinicians less frequently discussed topics including patients' and caregivers' expectations and understanding of the illness process (50.0%, n = 34/68) and illness prognosis (33.8%, n = 23/68).
FIG. 3.
Frequency of medical understanding topic elements by clinician type.
The oncologists and PC clinicians differed in discussing specific medical understanding topics. For example, although oncologists frequently informed patients of new medical information (64.7%, n = 22/34), PC clinicians rarely addressed this topic across visits (14.7%, n = 5/34). In addition, oncologists (91.2%, n = 31/34) informed patients and caregivers of the treatment process more frequently than PC clinicians (70.6%, n = 24/34). In contrast, PC clinicians more frequently assessed patients' and caregivers' understanding and expectations of the treatment process (58.8%, n = 20/34 vs. 11.8%, n = 4/34) and their understanding of prognosis (44.1%, n = 15/34 vs. 8.8%, n = 3/34) compared to oncologists.
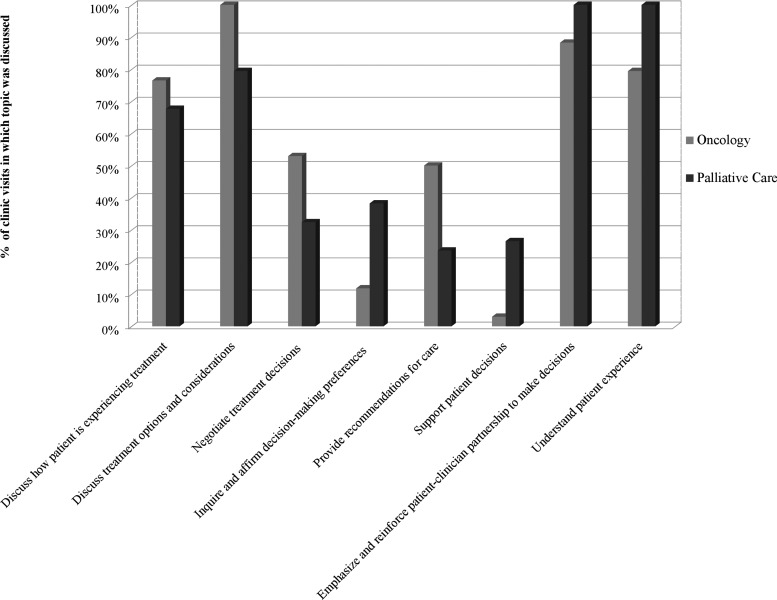
Treatment decision making
All clinicians discussed treatment decision making during each visit (100.0%, n = 68/68). Because this topic included numerous components, we performed a subanalysis of the frequency of specific elements within this topic (Fig. 4). Both oncologists (76.5%, n = 26/34) and PC clinicians (67.6%, n = 23/34) regularly discussed how the patient was experiencing treatment. Oncologists discussed treatment options and considerations at every visit (n = 100.0%, n = 34/34) by addressing patients' specific treatment concerns (100.0%, n = 34/34), discussing clinical trials (55.9%, n = 19/34) and treatment efficacy (44.1%, n = 15/34), and helping patients understand how treatment would impact their quality of life (64.7%, n = 22/34). In addition, oncologists provided treatment recommendations more often than PC clinicians (50.0%, n = 17/34 vs. 23.5%, n = 8/34). Although PC clinicians discussed treatment options and considerations less consistently across visits, they related treatment decisions to patients' attitudes, values, and life goals more frequently than oncologists (50.0%, n = 17/34 vs. 5.9%, n = 2/34).
FIG. 4.
Treatment decision-making topic elements by clinician type.
In discussions about treatment decision making, PC clinicians consistently emphasized the supportive role of their relationship with patients and caregivers (100.0%, n = 34/34) and focused on understanding how patients' experiences influence their treatment decisions (100.0%, n = 34/34). While oncologists were also engaged in these aspects of supporting patient decision making, PC clinicians engaged more frequently in validating patients' values and concerns (100.0%, n = 34/34 vs. 41.2%, n = 14/34), discussing patients' lives outside the context of their illness (88.3%, n = 30/34 vs. 52.9%, n = 18/34); building trust (82.4%, n = 28/34 vs. 61.8%, n = 21/34); and reinforcing the partnership between patients, caregivers, and clinicians (61.8%, n = 21/34 vs. 14.7%, n = 5/34).
Coping with illness
Although PC clinicians frequently discussed patient and caregiver coping with the illness (79.4%, n = 27/34), oncologists rarely addressed this topic (11.8%, n = 4/34). Specifically, PC clinicians talked about a variety of coping strategies such as behavioral approaches (38.2%, n = 13/34) (e.g., activity pacing, maintaining a normal life outside of illness, and relaxation techniques), ways to accept living with illness (32.4%, n = 11/34) (e.g., defining what is in one's control and maintaining hope), and use of social support (41.2%, n = 14/34) (e.g., emotional support, finding and using social support, and instrumental [tangible] support).
Supporting caregivers and loved ones
Caregivers were present at 88.2% (n = 60/68) of the clinic visits, attending both the oncology and PC visits. When caregivers were present at a clinic visit, clinicians were likely to support them (68.3%, n = 41/60), although clinicians at times also discussed caregivers who were not present (16.2%, n = 11/68). Regardless of whether the caregiver attended the visit, PC clinicians were more likely to support caregivers than oncologists. Specifically, compared with oncologists, PC clinicians more frequently addressed the relationship between the patient and caregiver (73.5%, n = 25/34 vs. 23.5%, n = 8/34), such as discussing changes in the patient–caregiver relationship (35.3%, n = 12/34 vs. 8.8%, n = 3/34), as well as made efforts to understand the caregiver's experience (47.1%, n = 16/34 vs. 14.7%, 5/34) and validate the caregiver's values and concerns (38.2%, n = 13/34 vs. 11.8%, n = 4/34). One second-level code, “discuss relationship between patient and loved one,” and two nested third-level codes were infrequently discussed but retained as codes for comparison.
Advance care planning
Of the major topics, clinicians addressed advance care planning with the least frequency, although these discussions occurred more often during PC visits than during oncology visits (41.2%, n = 14/34 vs. 23.5%, n = 9/34). PC and oncology clinicians, respectively, discussed code status (32.4%, n = 11/34 vs. 8.8%, n = 3/34), health care proxy (29.4%, n = 10/34 vs. 2.9%, n = 1/34), hospice (26.5%, n = 9/34 vs. 23.5%, n = 8/34), and home care (8.8%, n = 3/34 vs. 5.9%, n = 2/34).
Discussion
This analysis is the first to provide insights regarding the ways in which early, integrated PC and oncology care provides comprehensive management of patients with advanced cancer and their caregivers.18 Within this comanagement model of care, PC and oncology clinicians shared responsibilities and often engaged in complementary discussions regarding a comprehensive breadth of topics with patients and caregivers.
Overall, PC clinicians supplemented oncology care, discussing similar content areas such as symptom management, medical understanding, and treatment decision making while also emphasizing discussions regarding patients' coping with illness, caregivers' experiences, and advance care planning. PC clinicians complemented patients' discussions with oncologists in three overarching ways: (1) building supportive partnerships with patients and caregivers; (2) clarifying patients' understanding of their health, prognosis, and treatment; and (3) providing concrete coping skills to help patients and caregivers manage the illness. We discuss each of these points in the paragraphs hereunder. Notably, although clinicians varied in their frequency of discussing certain topics, no topic was solely addressed by one type of clinician. This finding underscores that, whereas a patient's specific needs (e.g., cancer- and treatment-related symptoms) may trigger a PC consultation in clinical practice,19–21 the care patients receive is neither one-dimensional nor compartmentalized.
-
(1)
PC clinicians focused on developing supportive, personal relationships with patients and caregivers demonstrated by their frequent discussions that included the codes “emphasizing and reinforcing their partnership with patients and caregivers” and “understanding the patient experience.” PC clinicians regularly validated patient concerns, asking about their lives outside of their cancer experience, building trust, and reinforcing their ongoing partnership with the patient and caregiver(s). These conversations were often interwoven in larger discussions regarding symptoms, treatment, and decision making, which often strengthened the bond between patients, caregivers, and clinicians.
-
(2)
In following up on patients' discussions with oncologists, PC clinicians assessed patients' and caregivers' comprehension and interpretation of treatment information and prognosis. Such assessment is key to enhancing medical understanding, encouraging patients and caregivers to review, evaluate, and interpret information while discussing their perceptions with the clinician. At times when patients or caregivers express confusion or concerns, the PC clinicians serve as an extra layer of support directly addressing those misperceptions or apprehensions. In a prior qualitative study with PC clinicians, Back and colleagues observed that PC clinicians view themselves as “interpreters” between oncologists and patients in helping to clarify understanding of illness and prognosis as well as treatment information.22
-
(3)
A distinctive feature of the PC intervention included the provision of tangible constructive coping skills. Clinicians sought to empower patients in actively managing their illness by addressing range of coping strategies tailored to patients' specific needs.23
This qualitative analysis suggests that the early, integrated PC model is simultaneously reflective, intimate, and practical. That is, by developing strong relationships in which patients and caregivers feel comfortable to share deeply personal and emotionally laden concerns after a cancer progression, PC clinicians were then able to broach more challenging discussions about advance care planning and the end of life as clinically indicated. The low frequency of these discussions in the current study may be due to the focus on outpatient visits after first and second cancer progressions. In the parent study, only 14.2% of PC clinicians discussed advance care planning with patients by 24 weeks after study enrollment.13 Nonetheless, as patients and caregivers faced critical questions about the future and the end of life, PC clinicians provided reassurance by reinforcing the team approach to supporting the family throughout the entire course of illness.
Several limitations of the study warrant consideration. We conducted the parent trial at a single large academic hospital with a largely white sample in which PC is already integrated into oncology clinics and likely more culturally embedded than at other cancer care settings. Also, rather than adjusting our initial coding scheme based on the current qualitative data, we may have identified additional topics particularly relevant for the oncologists' discussions if we had not started with an a priori coding scheme. Since a qualitative analysis of audio-recorded visits throughout the full course of care was not feasible, we analyzed a substantial number of clinic visits after first and second cancer progressions.
Conclusion
PC clinicians provide complementary and additive care to oncologists by deepening patients' and caregivers' understanding of their illness and prognosis, supporting treatment decisions, reinforcing adaptive coping skills, and planning for the end of life. As the first qualitative comparison to summarize the care provided during early, integrated PC, this study provides insight into the mechanisms by which this model of care improves patient outcomes. Follow-up longitudinal studies are needed to ascertain more fully how PC's clinical discussions impact patient quality of life and end-of-life care outcomes.
Supplementary Material
Author Disclosure Statement
J.S.T. and J.A.G. have received research funding for a separate study from Pfizer. Kamdar has a consulting and advisory role in addition to stock/ownership in Amorsa Therapeutics. All other authors have no competing financial interests.
NIH/NCI: K24 CA181253 (J.S.T.); NIH/NINR: R01 NR012735 (J.S.T.).
References
- 1. National Quality Forum: A National Framework and Preferred Practices for Palliative and Hospice Care Quality. 2006
- 2. Bakitas M, Lyons KD, Hegel MT, et al. : Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer. JAMA 2009;302:741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Temel JS, Greer JA, Muzikansky A, et al. : Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med 2010;363:733–742 [DOI] [PubMed] [Google Scholar]
- 4. Siouta N, Van Beek K, van der Eerden ME, et al. : Integrated palliative care in Europe: A qualitative systematic literature review of empirically-tested models in cancer and chronic disease. BMC Palliat Care 2016;15:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zimmermann C, Swami N, Krzyzanowska M, et al. : Early palliative care for patients with advanced cancer: A cluster-randomised controlled trial. Lancet 2014;383:1721–1730 [DOI] [PubMed] [Google Scholar]
- 6. Dionne-Odom JN, Azuero A, Lyons KD, et al. : Benefits of early versus delayed palliative care to informal family caregivers of patients with advanced cancer: Outcomes from the ENABLE III randomized controlled trial. J Clin Oncol 2015;33:1446–1452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. El-Jawahri A, LeBlanc T, VanDusen H, et al. : Effect of inpatient palliative care on quality of life 2 weeks after hematopoietic stem cell transplantation. JAMA 2016;316:2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. El-Jawahri A, Jackson VA, Greer JA, et al. : Early integrated palliative care to improve family caregivers (FC) outcomes for patients with gastrointestinal and lung cancer. J Clin Oncol 2006;34(suppl; abstr 10131) [Google Scholar]
- 9. Smith TJ, Temin S, Alesi ER, et al. : American Society of Clinical Oncology provisional clinical opinion: The integration of palliative care into standard oncology care. J Clin Oncol 2012;30:880–887 [DOI] [PubMed] [Google Scholar]
- 10. Ferrell BR, Temel JS, Temin S, et al. : Integration of palliative care into standard oncology care: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 2017;35:96–112 [DOI] [PubMed] [Google Scholar]
- 11. Zimmermann C, Riechelmann R, Krzyzanowska M, et al. : Effectiveness of specialized palliative care. JAMA 2008;299:1698. [DOI] [PubMed] [Google Scholar]
- 12. Kavalieratos D, Corbelli J, Zhang D, et al. : Association between palliative care and patient and caregiver outcomes. JAMA 2016;316:2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Temel JS, Greer JA, El-Jawahri A, et al. : Effects of early integrated palliative care in patients with lung and GI cancer: A randomized clinical trial. J Clin Oncol 2017;35:834–841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. National Consensus Project for Quality Palliative Care: Clinical Practice Guidelines for Quality Palliative Care, Third Edition. Pittsburgh, 2013. www.nationalconsensusproject.org/NCP_Clinical_Practice_Guidelines_3rd_Edition.pdf (Last accessed February6, 2018)
- 15. Sandelowski M: Sample size in qualitative research. Res Nurs Health 1995;18:179–183 [DOI] [PubMed] [Google Scholar]
- 16. Yoong J, Park ER, Greer JA, et al. : Early palliative care in advanced lung cancer. JAMA Intern Med 2013;173:283. [DOI] [PubMed] [Google Scholar]
- 17. Sim J, Wright CC: The kappa statistic in reliability studies: Use, interpretation, and sample size requirements. Phys Ther 2005;85:257–268 [PubMed] [Google Scholar]
- 18. Kelley AS, Meier DE: Palliative care—A shifting paradigm. N Engl J Med 2010;363:781–782 [DOI] [PubMed] [Google Scholar]
- 19. Hui D, Meng Y-C, Bruera S, et al. : Referral criteria for outpatient palliative cancer care: A systematic review. Oncologist 2016;21:895–901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wentlandt K, Krzyzanowska MK, Swami N, et al. : Referral practices of oncologists to specialized palliative care. J Clin Oncol 2012;30:4380–4386 [DOI] [PubMed] [Google Scholar]
- 21. Kwon JH, Hui D, Chisholm G, et al. : Clinical characteristics of cancer patients referred early to supportive and palliative care. J Palliat Med 2013;16:148–155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Back AL, Park ER, Greer JA, et al. : Clinician roles in early integrated palliative care for patients with advanced cancer: A qualitative study. J Palliat Med 2014;17:1244–1248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Greer JA, El-Jawahri A, Pirl WF, et al. : Randomized trial of early integrated palliative and oncology care. J Clin Oncol 2016;34(suppl 26S; abstr 104) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.