Abstract
Background
Stress has been known to increase craving in individuals with Alcohol Use Disorders (AUD) and predict future alcohol relapse risk, but whether stress on a particular day affects craving on that day to impact prospective alcohol intake in the real world, particularly during early treatment and recovery, has not been studied thus far.
Method
The first study included 85 AUD individuals who reported their daily stress, craving, and alcohol intake in the first two weeks of early treatment. A second validation study included 28 AUD patients monitored daily during eight weeks of outpatient 12-Step based behavioral counseling treatment for AUD. Data were collected from telephone-based daily diaries for 903 days in Study 1 and 1488 in Study 2. Multilevel latent models tested if daily and person-averaged craving mediated the link between stressful events and next day drinking during treatment.
Results
In both Study 1 and 2, exposure to a stressful event on a particular day predicted increased craving on that day (p’s≤.002); and such increases in craving predicted the likelihood of drinking the next day (p’s≤.014) and the drinking amount (p’s<=008). Individuals who experienced more stressful events reported higher craving (p’s≤.012), and higher cravers reported greater next day drinking (p’s<.001).
Conclusions
The results across two studies with separate samples are the first to establish that craving directly mediates the association between stress and next day alcohol intake in individuals with AUD. Findings suggest a need for novel treatment approaches to address stress-induced craving to improve alcohol use outcomes.
Keywords: Stress, Craving, Drinking, Alcohol Use Disorder, Treatment, Daily Diary
1. Introduction
Twenty-nine percent of adults in the United States meet criteria for Alcohol Use Disorder (AUD), one of the most disabling conditions worldwide, at some point during their lifetime (Grant et al., 2015; Rehm et al., 2009). AUD treatment is fraught with high dropout in early engagement, treatment failure, and high relapse risk (Hunt et al., 1971; Sinha, 2011; Stark, 1992), factors that contribute to high levels of alcohol-related morbidity and mortality (GBD Collaboration, 2018). The typical objective of treatment for AUD is that the patient will abstain, restore, or establish healthy drinking behaviors; however, patients are confronted with a multitude of obstacles, including interpersonal and situational stressors, that prevent them from reaching these goals or even initiating treatment in the first place. Thus, identifying potential therapeutic targets may help reduce the impact that stressors have on drinking behaviors and potentially increase the likelihood that patients will succeed.
Stress is a key component in many modern theories of the development and maintenance of addiction (Koob and Volkow, 2016; Sinha, 2001). Stress broadly refers to a process that involves perceiving, interpreting, responding, and adapting to a potentially harmful, threatening, or challenging event (Lazarus and Folkman, 1984). Stressful events result in emotional reactions (e.g., fear, anxiety, anger, sadness) and physiological/endocrinological reactions to allow the individual to mobilize resources to effectively manage the stress event. Stressful life events, such as trauma or early-life adverse events, make individuals more prone to developing an alcohol or substance use disorder. In turn, heavy, chronic use of substances, such as alcohol or drugs, results in adaptations to the stress response system that prevent the individual from responding appropriately. While stress has been associated with alcohol use, heavy social drinkers and those with AUD are more prone to stress-related alcohol intake than light drinkers (Adinoff et al., 2005; Blaine et al., 2018; Brown et al., 1995; Noone et al., 1999). Such findings suggest that higher levels of alcohol and drug intake may impact emotion and motivational processes by closely tying environmental precipitants, such as stress, to alcohol and drug intake and relapse (Amlung and Mackillop, 2014; Fox et al., 2007; Sinha et al., 2011a). Basic science studies that have modeled acute stress provocation in the laboratory have shown stress-induced reinstatement of alcohol and drug seeking in dependent animals (Lê et al., 2000; Mantsch et al., 2016; Sinha et al., 2011b). In humans, acute stress provocation using the personalized stress imagery procedure increased alcohol and drug craving in the laboratory (Fox et al., 2008; Sinha, 2007, 2001; Sinha et al., 2009, 2003; Sinha and Li, 2007), and at significantly higher levels than healthy social drinkers (Sinha et al., 2011a, 2009). Furthermore, reactivity to stress provocation predicted future relapse after treatment (Higley et al., 2011; Sinha et al., 2011b, 2006). Acute stress-induced alcohol and drug craving also increased intake in the laboratory (Blaine et al., 2018; McKee et al., 2011); however, it is not known if craving is a key process that links stressful experiences and future drinking in the real-world, especially during early treatment.
Significant previous research employing daily diary (DD) methods and ecological momentary assessment (EMA) has investigated triggers for alcohol use in social drinkers and clinical samples of AUD as well as in other substance use disorders (Serre et al., 2015; Shiffman et al., 2002; Wray et al., 2014). However, direct assessments of whether stress increases alcohol and drug craving and if craving mediates future use have been rare. For example, Preston and colleagues have shown that exposure to both stress and opioid and cocaine-related cues increases craving in an additive and synergistic manner using momentary sampling methods with multiple randomly assessed measurements per day (i.e., random prompts; Bertz et al., 2018; Kowalczyk et al., 2015; Preston et al., 2018; Preston et al., 2018a); however, stressful events by themselves were not sufficient to reliably predict opioid or cocaine use (Furnari et al., 2015; Preston and Epstein, 2011). Craving is a reliable predictor of substance use in both non-treatment seeking and treatment-seeking samples (see Serre et al., 2015 for review), including among adults in outpatient substance treatment (Moore et al., 2014) and heavy-drinking adults and adolescents on naltrexone for alcohol use (Miranda et al., 2018, 2014; Tidey et al., 2008). The extant research studies have therefore separately tested if stress increases alcohol or drug intake and if craving increases alcohol or drug use, but not if daily stress is associated with daily craving and if stress related craving predicts future intake, particularly in individuals with AUD.
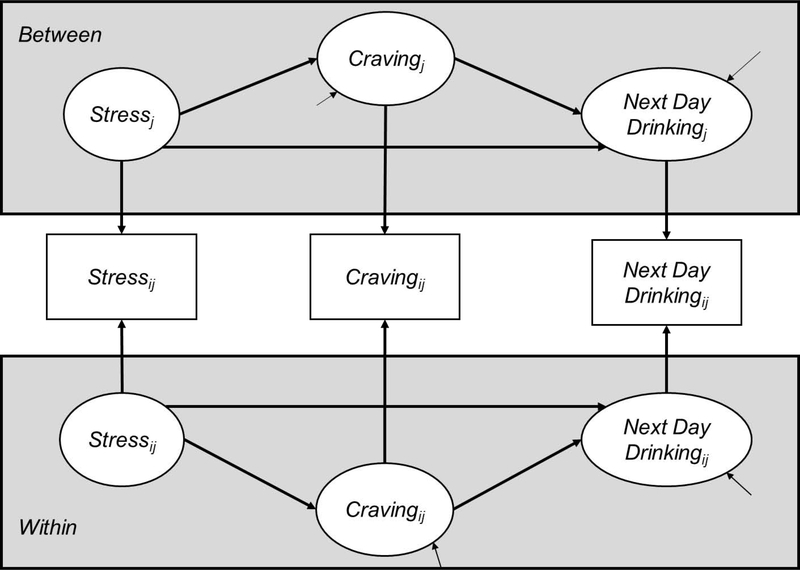
The goal of the current studies was to extend laboratory findings of stress-related craving and its association to future relapse to the real world. Based on the laboratory findings described above, we hypothesized that daily stressful experiences would lead to increased craving, and that craving, acting as a mediator, would prospectively predict alcohol intake the following day (see Figure 1). This hypothesis was tested in samples from two separate studies of treatment engaged individuals with AUD. We disaggregated within- and between-person variability in stress versus no stressful events and craving to isolate the day-to-day fluctuations in stress and craving (within-person) from each person’s average tendency to experience stressors and crave alcohol (between-person). We used the daily single day assessment approach (DD) rather than EMA as our goal was to assess daily stressors, daily craving and prospective next-day alcohol use, rather than identify specific predictors of drinking on a specific day which is best tested using an EMA approach (Serre et al., 2015; Shiffman et al., 2008; Wray et al., 2014). The focus of this paper and the hypotheses were based on investigating day- and next-day level processes of stress and craving on day-by-day drinking while individuals are engaged in outpatient treatment.
Figure 1.
Conceptual diagram for testing hypothesized effects using Multilevel Structural Equation Models. Specifically, we examined the mediating effect of craving between stress events and next day drinking in the day-to-day fluctuations (within-person) and the averaged differences across individuals (between-person) in both studies.
2. Material and Methods
2.1. Participants
Participants in both studies had to meet the following criteria to participate in the study: male or female individuals between the ages of 18 and 65, meet current DSM criteria for Alcohol Dependence/AUD (DSM-IV-TR for Study 1; DSM-5 for Study 2) and entering outpatient treatment, able to sign informed consent, and read English and complete study evaluations. Exclusion criteria included: a diagnosis of abuse or dependence for any other psychoactive substance except cannabis, nicotine, and caffeine; current use of psychoactive drugs; any psychotic disorder or psychiatric disorder requiring specific attention (e.g., Bipolar I or II Disorder, active suicidal intent and plan); significant underlying medical conditions that would interfere or be of potential harm during the study (e.g., history of myocardial infarction, cardiovascular disease, cancer). Additional exclusion for Study 1 was hypotension as indicated by a sitting blood pressure below 90/60 mmHg because of the potential side effects of prazosin, an anti-hypertensive, of lowering blood pressure for these individuals. In the first study, 85 participants were included in the analyses during the first two weeks of their participation; a second validation sample of 28 AUD individuals were assessed daily over a longer 8-week outpatient behavioral treatment period (Table 1 for demographics).
Table 1.
Sample Demographics and Clinical Characteristics at Intake.
| Study 1 | Study 2 | ||
|---|---|---|---|
| Sample in Each Study (N) | 85 | 28 | |
| Gender – no. of females | 31 (36.5%) | 11 (39.3%) | |
| Race | |||
| Caucasian | 41 (48.2%) | 9 (32.1%) | |
| African American | 43 (50.6%) | 18 (64.3%) | |
| Other | 1 (1.2%) | 1 (3.6%) | |
| Age | 40.36 ± 11.05 | 36.93 ± 11.27 | |
| Years of Education | 13.59 ± 2.11 | 13.25 ± 2.14 | |
| No. of regular smokers | 50 (58.8%) | 17 (60.7%) | |
| Psychiatric Diagnoses | 17 (20.2%) | 4 (14.4%) | |
| Major Depressive Disorder | 4 (4.7%) | 1 (3.6%) | |
| Anxiety Disorders | 2 (2.3%) | 3 (10.7%) | |
| PTSD | 8 (9.4%) | 1 (3.6%) | |
| Years of alcohol use | 16.25 ± 9.99 | 13.02 ± 10.91 | |
| Days of alcohol used (past 30) | 20.20 ± 8.49 | 17.76 ± 8.84 | |
| Ave Drinks/Day | 7.12 ± 4.79 | 5.56 ± 3.11 | |
| AUDIT Score | 21.14 ± 6.89 | 18.96 ± 6.23 |
Note: Psychiatric diagnoses were determined using the DSM-IV-TR criteria in Study 1 and DSM-5 criteria in Study 2.
2.2. Procedures
For both studies, treatment-seeking participants with AUD were recruited from the community through advertising on the web, newspapers and via flyers posted in the Greater New Haven area. For both studies, all participants provided written informed consent and the research was approved by the Yale University Human Investigation Committee. Trained research assistants completed a phone screen with participants to determine preliminary eligibility. Participants were then invited to the Center where they received a complete description of the study, provided their written informed consent, and completed an in-person screening. During these appointments, participants completed a series of baseline assessments and provided urine samples to verify recent alcohol and drug use history.
On the first day of study initiation in both studies, participants completed an orientation to the DD assessments. For participants in Study 1, 50 participants (58.8%) completed their daily diaries via a telephone interactive voice response system. The remaining 35 participants (41.2%) completed their assessments via a smartphone app (MetricWire, Inc) because of a change in the protocol. Participant responses in Study 2 were collected entirely through the app. Measurements were collected during an evening survey that was triggered at 8 pm every night that participants could complete within six hours before going to bed. For Study 2, participants also completed a morning survey at 8 am where participants reported their alcohol use for the previous day, which was used to estimate drinking if the participants missed the previous day’s evening survey. Compliance was monitored throughout the study. Participants were paid $2 per day for responding to surveys and received an additional $10 bonus for completing all surveys that week.
2.3. Self-Report Measurements
Sociodemographic Information. Demographic data, medical history, and family psychiatric history were assessed via interviews and self-reports.
Structured Clinical Interview for DSM-IV/DSM-5 was used to obtain Alcohol Dependence and AUD, respectively, and other diagnoses (First et al., 2015; First and Gibbon, 2004).
The Timeline Followback (TLFB; Sobell and Sobell, 1992) was used as a secondary source for daily data on alcohol use at each weekly face-to-face appointment.
2.4. Daily Diary Monitoring
Study 1. Participants completed a daily survey that assessed if a stress event occurred that day, their current alcohol craving, and the amount of alcohol consumed that day. In this way, data on stressors experienced and alcohol craving on each day as well as alcohol intake per day was assessed, providing day-by-day data on predictor variables and drinking outcome. Participants were asked to respond yes or no to three questions designed to measure stressful events that day (“Did you have or nearly have an argument or disagreement with anyone?”, “Did anything else happen at home, work, or school that you felt was stressful?”, “Did anything else happen to you that most people would consider stressful?”) derived from the Daily Inventory of Stress Events (Almeida et al., 2002). Recent work has demonstrated that asking participants to recall stressful events at the day level yields similar results as asking participants to report stressful events as they occur (Preston et al., 2018b). The three items were combined into a single index that indicated if a stressful event occurred that day (“1”) or not (“0”). Tiffany and Wray (2012) describe craving as an expression of desire or wanting for alcohol or drugs. Questions that target this desire or want, tend to perform as well as questions that directly ask about craving. Thus, we opted for the average of two items was used to create an index of craving, “Right now, I could really use a drink” and “Right now, the idea of a drink is appealing,” to capture aspects of desire and want. Participants indicated their agreement to these items on a 5-point Likert scale (0=“Definitely False” and 4=“Definitely True”). When reporting drinking behavior, participants were provided with a description of standard drinks (i.e., 12 oz. of beer, 5 oz. of wine, 1.5 oz. of liquor) and asked how many glasses of beer, wine, and mixed drinks they consumed on that day. Information about their alcohol consumption that day was supplemented by TLFB if a participant missed an evening survey in Study 1 (6.8% of drinking days). The quantity of each type of drink was summed for each day to create an index of total drinks consumed per day.
Study 2. The second study used the same procedure to measure alcohol consumption, but the assessment of stressful events and craving differed slightly. As before, the TLFB was used to estimate drinking on days missing alcohol consumption reports (15.5% of days). To assess stressors that occurred that day, participants completed a more extensive version of the daily stress assessment based on work from previous EMA studies (Armeli et al., 2015). Participants were asked, “Which of the following events made you feel stressed today?” to which they could check a box of twelve possible events (e.g., “Work/Education,” “Home/Family,” “Finances,” among others). Responses were dichotomized to indicate if any stressful events occurred that day (“1”) or not (“0”) in order to make the results comparable between studies. Craving was measured by asking participants about their current desire to drink (“Right now I could really use a drink”) on a Visual Analog Scale (VAS) ranging from 1 representing “Strongly disagree” up to 100, anchored at “Strongly agree.” We opted for a single question to reduce participant burden since the two items described in Study 1 were strongly correlated (r=.77).
2.4.1. Treatment Description of Studies 1 and 2
The first study focused on early treatment engagement in the first two weeks of treatment in a medication trial of Prazosin versus Placebo that required a 2-week titration before reaching full dose (Study 1). All participants in Study 1 also received one hour per week of 12-step facilitation behavioral treatment as an adjunctive therapy. Study 2 served to provide a separate validation sample and test the hypothesis over an 8-week period using the same behavioral treatment as Study 1 but without the medication. The behavioral treatment consisted weekly one hour meetings with a therapist that provided 12-step facilitation (Nowinski et al., 1992) and was standard of care provided and was not compared to any other treatment. Thus, the focus of the present study was to assess the day-to-day effects of changes in stress and craving on drinking on each day as they naturally occur in the real world setting of outpatient treatment over and above any effect of standard treatment. Participants could attend self-help groups (e.g., Alcoholics Anonymous) but could not attend any other formal treatment. As stress and cravings commonly occur while AUD patients are in outpatient treatment and 12-Step Counseling, how stress and craving may impact drinking during treatment remains a significant question.
2.5. Data Analytic Plan
Since the data in Study 1 was focused on the first two weeks of a 12-week medication trial before participants reached the full-dose of the study medication, we chose to assess stress, craving and drinking during the titration phase. As expected, medication condition (Prazosin vs. Placebo) did not significantly affect alcohol use during this period (p>.20) In Study 2, responses collected throughout the entirety of the eight-week behavioral counseling protocol were included in the analyses. To control for any effect of medication condition, we included it as a covariate in the analysis for Study 1. In both studies, we also covaried for the effect of study day or time during treatment on stressful events, craving, and drinking, because it is possible that the behavioral treatment participants received could exert increasing effects as participants attended more sessions. We also controlled for age, gender, psychiatric diagnoses of depression and anxiety, and cigarette smoking status in both studies. We used Multilevel Structural Equation Modeling (MSEM) with Bayesian estimation and fixed slope in Mplus 8.0 to test the prospective mediating effect of craving right now on the association between that day stress and prospective next day drinking and drinks consumed. MSEM allows for isolating variations in drinking that are due to a person being exposed to more stress or having greater craving relative to their peers (between-person) from deviations in the person’s own average level of stress or craving (within-person; Figure 1).
Results Verification Analyses: As craving assessed in the evening may also be influenced by drinking earlier in the day, we conducted secondary analyses to further test the stability and strength of the prospective associations by also testing the model using drinking behavior on the same day as the stress and craving reports, and their effects on next-day drinking controlling for the previous day’s drinking behavior (see Supplementary Appendix).
3. Results
Participants’ characteristics and baseline drinking prior to treatment entry for Study 1 and 2 are summarized in Table 1. Consistent with previous patient treatment based daily diary research, adherence to daily reporting during the target data collection phase while in treatment to all possible assessments was 73.0% in Study 1 and 77.5% in Study 2 (Litt et al., 1998). In Study 1, participants completed a total of 903 daily logs of which 42.1% were drinking days (M=4.49, SD=4.15 days, range: 0–14 days). The average number of drinks consumed on drinking days were 4.96±6.94. Stressful events occurred on 35.2% assessed days, and the average daily craving was 1.59±1.25 on the 5-point scale. In Study 2, participants completed approximately 1488 daily logs of which 29.9% were drinking days (M=15.93, SD=16.12 days, range: 0–50). On drinking days, participants drank approximately 4.17±2.84 drinks on average (1–14.32). Stressful events occurred on 43.2% of the days recorded, and the average craving on the VAS scale was 31.19±30.80. The Supplemental Appendix includes additional descriptive results. All results described in the following sections included all the covariates, and inclusion of these covariates did not change the pattern of results.
3.1. Craving Mediation of Stress and Next-Day drinking at the Between-Person Level
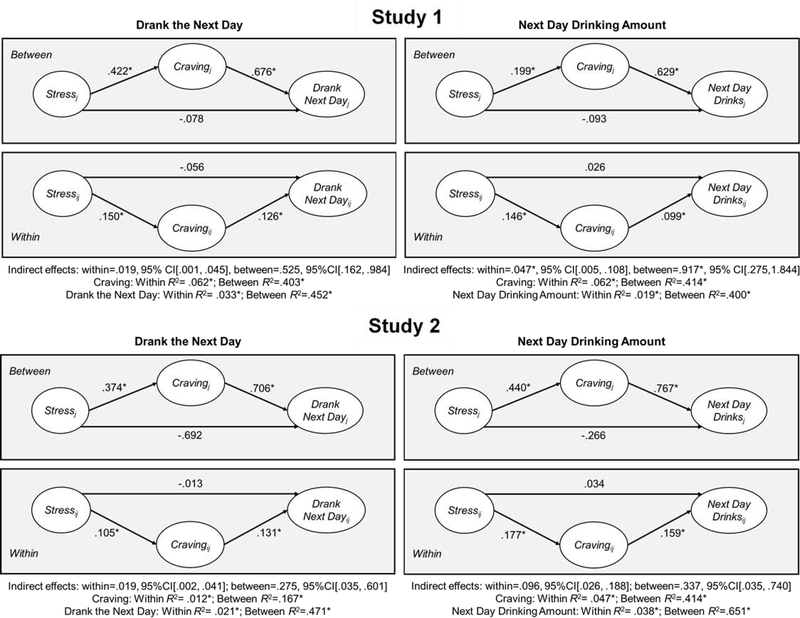
A similar pattern of findings played out at the between-person level in both Study 1 (Table 2) and Study 2 (Table 3). Specifically, individuals in Study 1 who experienced more stress on average reported significantly higher overall craving (abetween:R2=.403-.414, p’s<.001; b=.484-.502, p’s<.001). A one-unit increase in craving on the five-point craving scale increases the probability of drinking by .883 on average (bbetween:R2=. 452, p<.001; b=1.089, p<.001) and the number of drinks by 1.83 on average (bbetween:R2=.367, p<.001; b=1.796, p<.001; Figure 4). The indirect effect of stress on drinking mediated via craving (defined as the product of the abetween and bbetween paths) was significant (indirectbetween:b=2.541–3.963, p’s<.001) but the direct effect of stress on drinking was not (cwithin & c’within p’s>.08).
Table 2.
Results from the Study 1 mediation multilevel structural equation model predicting the likelihood of next day drinking day and number of drinks consumed.
| Drank Next Day | Next Day Drinking Amount | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Parameter | Est. | Posterior S.D. | p | 95% C.I. | Est. | Posterior S.D. | p | 95% C.I. | |||
| Lower | Upper | Lower | Upper | ||||||||
| Within | |||||||||||
| awithin: Stress → Craving | .129 | .042 | .002 | .048 | .208 | .126 | .043 | .002 | .041 | .210 | |
| bwithin: Craving → Drinking | .148 | .068 | .014 | .018 | .283 | .373 | .151 | .008 | .069 | .675 | |
| cwithin: Stress → Drinking | −.056 | .079 | .252 | −.215 | .090 | .084 | .197 | .338 | −.283 | .475 | |
| c’within: Stress → Drinking | −.039 | .075 | .301 | −.182 | .108 | .086 | .186 | .326 | −.282 | .455 | |
| Between | |||||||||||
| abetween: Stress → Craving | .484 | .163 | .001 | .167 | .822 | .502 | .168 | .001 | .159 | .918 | |
| bbetween: Craving → Drinking | 1.089 | .224 | <.001 | .634 | 1.552 | 1.825 | .473 | <.001 | .859 | 2.706 | |
| cbetween: Stress → Drinking | −.133 | .305 | .322 | .728 | .507 | −.313 | .609 | .307 | −1.544 | .836 | |
| c’between: Stress → Drinking | .442 | .300 | .068 | −.122 | 1.065 | −.300 | .530 | .181 | −1.355 | .741 | |
| Indirect (a x b) | |||||||||||
| indirect within | .019 | .011 | .016 | .001 | .045 | .047 | .026 | .010 | .005 | .108 | |
| indirect between | .525 | .206 | <.001 | .162 | .984 | 917 | .402 | .001 | .275 | 1.844 | |
Note: Est. = estimate, S.D. = standard deviation, C.I.= credibility interval, p = Bayesian one-tailed p-value, or the proportion of the posterior distribution that overlaps zero (for positive estimates=proportion below zero, for negative estimates=proportion above zero). Analyses controlled for gender, age, medication condition, day in the study, smoking status, and psychiatric diagnoses. The drinking day outcome is a binary variable (0=non-drinking day, 1=drinking day), thus probit link was used for the outcome variable. The Bayesian credibility interval encompasses the lower 2.5% and 97.5% in the posterior distribution.
Table 3.
Results from the Study 2 mediation multilevel structural equation model predicting the likelihood of next day drinking day and number of drinks consumed.
| Drank Next Day | Next Day Drinking Amount | ||||||||||
| Parameter | Est. | Posterior S.D. | p | 95% C.I. | Est. | Posterior S.D. | p | 95% C.I. | |||
| Lower | Upper | Lower | Upper | ||||||||
| Within | |||||||||||
| awithin: Stress → Craving | 3.589 | 1.042 | <.001 | 1.542 | 5.605 | 3.728 | 1.092 | .001 | 1.594 | 5.858 | |
| bwithin: Craving → Drinking | .005 | .002 | .011 | .001 | .010 | .026 | .008 | .001 | .010 | .041 | |
| cwithin: Stress → Drinking | .012 | .105 | .457 | −.191 | .219 | .117 | .294 | .346 | −.466 | .691 | |
| c’within: Stress → Drinking | .035 | .106 | .373 | −.169 | .247 | −.091 | .288 | .358 | −.610 | .500 | |
| Between | |||||||||||
| abetween: Stress → Craving | 6.175 | 2.699 | .010 | .997 | 11.771 | 5.821 | 2.650 | .012 | .741 | 11.198 | |
| bbetween: Craving → Drinking | .045 | .012 | <.001 | .022 | .070 | .058 | .015 | <.001 | .028 | .087 | |
| cbetween: Stress → Drinking | −.232 | .151 | .057 | −.541 | .062 | −.258 | .180 | .072 | −.622 | .095 | |
| c’between: Stress → Drinking | .045 | .171 | .397 | −.286 | .396 | −.262 | .186 | .071 | −.630 | .089 | |
| Indirect (a x b) | |||||||||||
| indirect within | .019 | .010 | .011 | .002 | .041 | .096 | .042 | .001 | .026 | .188 | |
| indirect between | .275 | .144 | .010 | .035 | .601 | .337 | .179 | .013 | .035 | .740 | |
Note: Est. = estimate, S.D. = standard deviation, C.I.= credibility interval, p = Bayesian onet-ailed p-value, or the proportion of the posterior distribution that overlaps zero (for positive estimates=proportion below zero, for negative estimates=proportion above zero). Analyses controlled for gender, age, medication condition, day in the study, smoking status, and psychiatric diagnoses. The drinking day outcome is a binary variable (0=non-drinking day, 1=drinking day), thus probit link was used for the outcome variable. The Bayesian credibility interval encompasses the lower 2.5% and 97.5% in the posterior distribution.
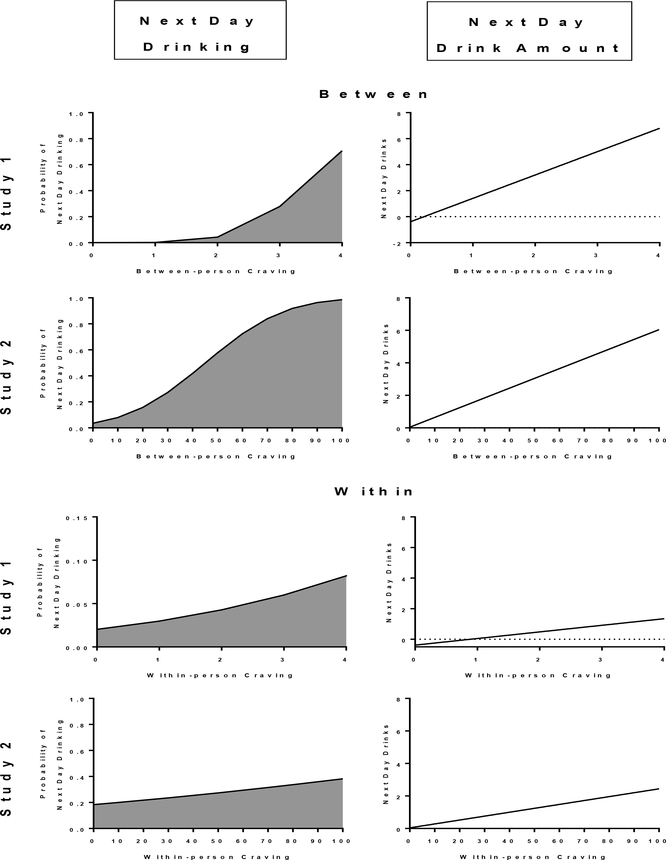
Figure 4.
Effects of craving on alcohol intake at the within- and between-person levels in both studies when between-person level variables are at their average and on a stress day. The gray areas indicate the increased probability of a drinking day as craving increases in Study 1 (within-person: p’s<.001, between-person: p’s<.001) and in Study 2 (within-person: p’s<.001, between-person: p’s≤.001). In Study 1, each point is plotted at 1-point intervals of the craving measure; in Study 2, each point is plotted at 10-point intervals.
Individuals in Study 2 who experienced more stress on average also reported higher same day craving (abetween:R2=.117-.167, p<.001;b=23.240–23.409 p=.010; Table 3). A ten-point increase in average craving on the VAS scale corresponded with a .4 increase in the probability of drinking (bbetween:R2=.471, p<.001; b=.040, p<.001), and an increase of about .60 drinks on average for every ten-unit increase in craving as compared to their peers who craved less (bbetween:R2=.568, p<.001; b=.060, p<.001). Higher levels of stress did not have direct effects on the average probability of drinking the next day or average alcohol intake (cwithin & c’within p’s>.05). However, overall stress had an indirect effect on averaged next day alcohol intake via its effect on craving (indirectbetween:b=.919–1.518, p’s<.001).
3.2. Craving Mediation of Stress and Next Day Drinking at the Within-Person Level
In Study 1, at the within-person level, experiencing a stressor earlier in the day predicted a .27 increase in craving that night (R2=.012-.062,p’s<.001; awithin:b=.126-.129-,p=.002; Figure 3). An increase in an individual’s craving relative to their average was associated with a greater probability of the following day being a drinking day(R2=.033,p<.001; bwithin:b=.148,p=.014) and an increase of .43 drinks consumed from their own average levels (R2=.019,p<.001; bwithin:b=.373,p=.008; Figure 4). Although stress did not have a direct effect on the following day’s drinking behavior (cwithin & c’within p’s>.08), the indirect effect via craving was significant at the within-person level (indirectwithin:b=.019-.047,p’s<.001).
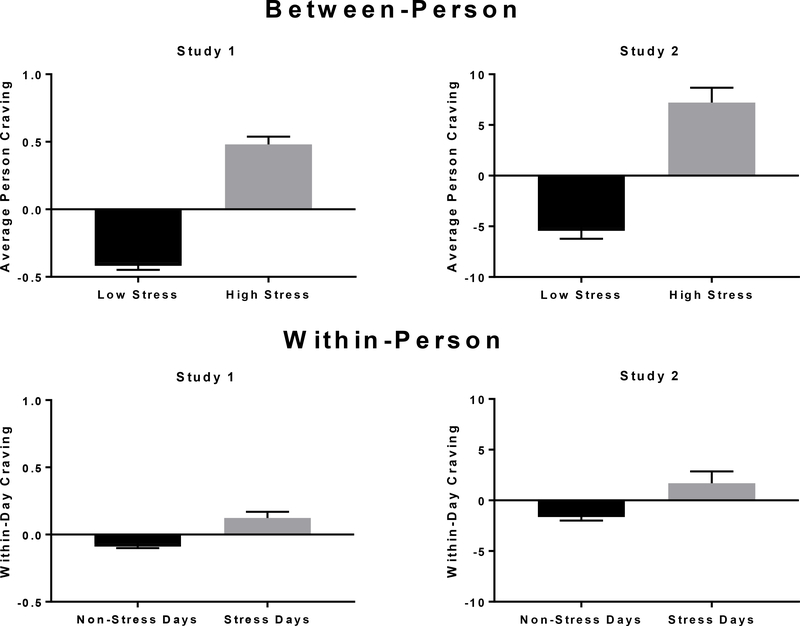
Figure 3.
The within- and between-person effects of stress on craving. Each point is plotted using the person-centered (within-person) and grand-mean centered (between-person) craving variables. Error bars ± SE. Within-Person effects are for days when stress occurrence consistently increased craving for that day (within-person; p’s<.001). Between-person effects indicate individuals that were higher in stress relative to their peers reported higher craving on average (between-person; p’s≤.010).
The same results were obtained in the validation sample in Study 2 (Table 3; Figure 2). Stressful events that day predicted about an 1-point increase in craving relative to the participants’ own average levels (awithin:R2=.012-.047,p’s<.001; b=1.042–1.092–8.302,p<.001). Higher within-person craving, in turn, predicted the next day’s alcohol consumption, including an increased likelihood that the next day would be a drinking day (bwithin: R2=.021,p<.001; b=.005,p=.011) and an increased deviation of .58 drinks for every 10-unit increase in craving (bwithin:R2=.038, p<.001; b=.058, p<.001). As in Study 1, stress did not have direct effects on the following day’s drinking in Study 2 (cwithin & c’within p’s>.26), but it did have an indirect effect via craving (indirectwithin b=.019-.096,p’s<.001).
Figure 2.
The between and within-person results for the multilevel structural equation models in both studies assessing the mediating effect of craving on the relationship between stress and drinking outcomes. Depicted are the standardized coefficients for each path. R2 refers to the explained variance proportion in an underlying continuous latent response variable. *indicates significant results.
3.3. Secondary Analyses to Verify Stability of the Results
We also assessed if the prospective mediation model remained significant after accounting for the impact of same-day drinking on same-day craving and next-day drinking. Same-day drinking increased craving that day and was significantly associated with the following day drinking behavior. However, the prospective models remained robust in both studies and indicated that including same-day drinking did not reduce the effect of the stress-craving relationship on next day drinking (see Tables S1–S4 in Supplemental Results).
4. Discussion
Both clinical lore and laboratory research suggests that stress is associated with alcohol intake during treatment and with relapse risk after treatment. However, there has been limited research directly testing mediators of this association and the role that craving plays in the link between stress and alcohol intake during daily life in AUD. This study is the first to directly measure the mediating effect of craving on the link between daily stress exposure and prospective assessment of next-day drinking in two studies with separate samples of outpatient treatment engaged adults with AUD. Findings indicate that participants’ abstinence and their reductions in drinking were jeopardized by stress-related craving. On days that individuals experienced a stressor, they reported greater alcohol craving that night. Craving, in turn, predicted an increased likelihood of drinking and greater amount of alcohol consumed on the following day. Furthermore, the finding of stress-related craving mediating next-day alcohol use was replicated in two separate treatment-seeking samples and remained significant even when accounting for same day drinking. The consistency of the findings across two separate studies and samples speaks to the stability and validity of the results.
A strength of this study and other intensive repeated-measure designs is the ability to model within-person state-based changes separately from between-person individual differences. At the within-person or day-by-day level, we found that the presence or absence of stress per day covaried with changes in craving levels for that day, which in turn predicted higher likelihood of drinking and higher alcohol amounts consumed for the following day. At the between-person or individual level, associations between stress, craving, and drinking were also similar, in that individuals exposed to more stressors were at risk for higher craving than their peers. In turn, individuals with high craving profiles were generally more likely to drink and consumed greater average number of drinks than low craving peers.
It should be noted that a large proportion of the variance in craving and drinking were accounted for by between-person differences (see Supplemental Appendix). The remaining variance at the within-person level was smaller by comparison. In addition, our results showed that the magnitude of the effect was much larger across individuals, or at the between-level albeit with more variation, than at the daily or within-level in both studies. It may be that small deviations in the within-person motivational state that are sustained over the day are adequate to affect drinking behavior. However, craving can fluctuate over time and individuals vary extensively in their reports (Shiffman, 2000). By separately modeling the between- and within-person components, we could not only identify who is more at-risk for drinking while in treatment, but also when they would be most at risk. An additional strength of this study was the time-locked nature of the mediation tested in these analyses. Although stress and craving were measured simultaneously, others have found that end-of-day stress reports were comparable to stressful events reported at the moment that the event occurred (Preston et al., 2018b). Furthermore, how the participants were asked to respond (i.e., stressful events earlier in the day, craving right now) lend confidence to the temporal sequencing of the predictor and mediator. More importantly, considering a prospective future outcome of next-day drinking also supports temporal sequential testing of the effects of stress and craving on the next-day drinking outcome assessed daily across 14 days in Study 1 and daily over an 8-week period in Study 2.
Other investigations of stress, craving, and drug use (i.e., cocaine, heroin) have found that craving increases in the presence of stress, independent of drug cues (Jobes et al., 2011; 2018); in contrast, the relationship between stress and substance use has been less reliable (Furnari et al., 2015; Preston et al., 2018a). These previous results are consistent with our present findings in treatment engaged AUD individuals. We did not find that stressful events had a direct effect on alcohol use; rather, the effect of stress on next day alcohol intake was fully mediated via its effect on alcohol craving. Early mediation models were required to have a significant direct path between the predictor and dependent variable (Baron and Kenny, 1986), but researchers have made the case that this is not a necessary condition for testing indirect effects (Zhao et al., 2010). When our findings are taken together with previous research, stress influences substance use when it directly increases the urge to use. This is consistent with previous work from Furnari and colleagues (2015) that found stress occurrence alone was an inconsistent predictor of opioid or cocaine use; however, they also found that severity of the stressor mattered. That is, the more stressful an event was, the more strongly the event predicted cocaine use. Therefore, it could be that certain types of stressful events (i.e., interpersonal stressors) that are more severe might have a direct impact on drinking. Another study from the same laboratory found that stress-related feelings was related to increased craving (Preston et al., 2018). These collective results suggest that response to event is important and the inability mount an effective response to a stressful event, and a lack of a sense of effective coping, may make addicted individuals more vulnerable to craving and drug use. Consistent with this, laboratory evidence suggests that stress may specifically act on alcohol and drug use primarily via craving. It is entirely possible that more severe stressors or stressors that elicit stronger reactions might exert their impact via increased craving or motivation to drink. Trauma-related symptoms predicted coping-related alcohol use in a group of individuals with co-morbid AUD and Post-Traumatic Stress Disorder (Kaysen et al., 2007; Simpson et al., 2014). Failing to consider the critical role of craving, or motivation to use, in the stress-substance use link would likely provide an underestimate of the impact that stress has on alcohol use and potential relapse in early treatment.
Although there are several FDA approved medications and evidence-based behavioral counseling approaches to AUD treatment, their effects are modest (Garbutt, 2009; Litten et al., 2015) and relapse during and after treatment are common (Hunt et al., 1971; Shim et al., 2017; Sinha, 2011). Craving, encompassing the psychological urge and intent to use and the associated physiological arousal (Sinha, 2013), is a cardinal symptom in DSM-5 for each of the substance use disorders (SUD) including alcohol (American Psychiatric Association, 2013). It has also been the focus of pharmacologic and behavioral treatments for SUD and AUD, but craving associated with stress is rarely addressed in SUD and AUD treatment, and there are no specific empirically validated pharmacologic or behavioral treatments for AUD to date that specifically targets the stress-induced craving state. Naltrexone, by far the most studied pharmacological intervention for AUD, targets craving but it is unclear if it reduces stress-induced craving. There is preliminary evidence that pharmacological interventions that target the adrenergic system may reduce craving evoked by both alcohol/drugs and stress (Fox and Sinha, 2014; Fox et al., 2012; Lê et al., 2011). Cognitive behavioral treatments separately address craving and negative affect in selective modules, but neither module directly addresses the stress-induced craving state, which may encompass physiologic, emotional, cognitive, and behavioral aspects of stress-related alcohol and drug motivation to potentially impact risk of intake (Bergquist et al., 2010; Chaplin et al., 2010; Sinha, 2013). As evidenced by the current study, stressful events are common for most individuals in early recovery. Current findings support the notion that novel treatment development to specifically target craving and high risk of drinking on stressful days during treatment could be of benefit in decreasing stress-related craving and its potential for adversely jeopardizing alcohol treatment and recovery.
The current findings should be considered within the context of its limitations. Our findings may only generalize to treatment-seeking individuals with AUD and replication of current results would be needed in non-treatment seeking AUD or binge/heavy alcohol users. It should also be noted that the results were somewhat stronger in Study 1 as compared to Study 2. This is likely in part due to the larger sample size included in Study 1 as far more power is achieved by adding participants than number of assessments in intensive longitudinal designs (Bolger and Laurenceau, 2013). We also focused on daily evening reports of craving. However, craving not only fluctuates during the day, but also commonly occurs in the context of alcohol- and drug-related cues. Despite this, findings from other groups have found that craving can be sustained for as long as four hours before drug intake (Fatseas et al., 2015). This suggests that the effects of craving may be more sustained unless an intervention is introduced. The fact that craving continued to exert an impact on next-day drinking behavior over and above same-day drinking suggests that craving still wields powerful effects beyond any possible within day variation of when it might be at its peak, at least for individuals receiving outpatient treatment for AUD. Future investigations that use EMA approaches with random prompts and participant-initiated surveys would be necessary to address the relative impact of within day variation of stressors, alcohol cues, and their combination on alcohol craving and future drinking. It is important to note that we assessed all daily stressors and not specifically traumatic events, which tend to be more infrequent occurrences. Notably, current findings suggest that stressors do not have to be traumatic in nature to increase craving and influence day-to-day drinking outcomes. Specific assessment of the influence of traumatic occurrences on day-to-day craving and drinking in the real world would be an important future research goal. Another important area for future research would be to assess if gender moderates the associations between the variables of interest. Studies with a larger sample could explore how treatment-seeking men and women might differ in their stress-evoked craving and alcohol use.
5. Conclusions
Despite these caveats, the current research is the first to establish that stress has its pernicious impact on drinking during treatment by its positive association with increasing craving, that in turn, increases the risk of next day alcohol intake in AUD individuals’ initiation of treatment and early recovery across two separate samples. These findings validate previous laboratory studies that show acute personalized stress provocation increases craving and such increases in stress-induced craving prospectively predict relapse (Sinha et al., 2011a, 2006). Furthermore, the findings underscore the importance of targeting craving specific to stressful experiences during AUD treatment. Since there are limited treatments that directly target stress-evoked craving, development, and testing of novel interventions that specifically address the stress-induced craving state may serve to enhance alcohol use treatment outcomes.
Supplementary Material
Highlights.
Stress is a significant risk factor for alcohol relapse, and although laboratory studies show stress increases craving and predicts future relapse, whether this occurs in the real world during early outpatient treatment is not known.
Here we report on two separate studies where participants completed phone-based daily diary surveys of stress events, craving, and alcohol consumption for each day during treatment.
Multilevel latent models were used to disaggregate within-person from between-person differences.
In two separate study samples, craving mediated the association between stress and next-day drinking behavior.
Acknowledgments
The authors wholeheartedly thank Drs. Verica Milivojevic, Sara Blaine, and Nia Fogelman, as well as Ms. Rachel Hart and the staff of the Yale Stress Center for their assistance with this project.
Role of Funding Source
This work was supported by grants from the National Institutes of Health (NIH) [grant numbers: R01-AA013892, R01-AA020504, and T32-DA007238].
Footnotes
Author Disclosures
Conflicts of Interest
Dr. Sinha is on the Scientific Advisory Board of Embera Neurotherapeutics. Drs. Wemm, Hermes, and Tennen and Ms. Chloe Larkin report no competing interests. There are no conflicts of interest related to findings and data presented in this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adinoff B, Krebaum SR, Chandler PA, Ye W, Brown MB, Williams MJ, 2005. Dissection of Hypothalamic-Pituitary-Adrenal Axis Pathology in 1-Month-Abstinent Alcohol-Dependent Men, Part 1: Adrenocortical and Pituitary Glucocorticoid Responsiveness. Alcohol. Clin. Exp. Res 29, 517–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida DM, Wethington E, Kessler RC, 2002. The Daily Inventory of Stressful Events. Assessment 9, 41–55. 10.1177/1073191102091006 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and Statistical Manual of Mental Disorders, 5th ed American Psychiatric Publishing, Inc; US, Arlington, VA: 10.1176/appi.books.9780890425596.744053 [DOI] [Google Scholar]
- Amlung M, Mackillop J, 2014. Understanding the effects of stress and alcohol cues on motivation for alcohol via behavioral economics. Alcohol. Clin. Exp. Res 38, 1780–1789. 10.1111/acer.12423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armeli S, Tennen H, Affleck G, Kranzler HR, 2015. Does affect mediate the association between daily events and alcohol use? J. Stud. Alcohol 61, 862–871. 10.15288/jsa.2000.61.862 [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA, 1986. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol 51, 1173–1182. 10.1037/0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- Bergquist KL, Fox HC, Sinha R, 2010. Self-reports of interoceptive responses during stress and drug cue-related experiences in cocaine- and alcohol-dependent individuals. Exp. Clin. Psychopharmacol 18, 229–237. 10.1037/a0019451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertz JW, Epstein DH, Preston KL, 2018. Combining ecological momentary assessment with objective, ambulatory measures of behavior and physiology in substance-use research. Addict. Behav 83, 5–17. 10.1016/j.addbeh.2017.11.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaine SK, Nautiyal N, Hart R, Guarnaccia JB, Sinha R, 2018. Craving, cortisol and behavioral alcohol motivation responses to stress and alcohol cue contexts and discrete cues in binge and non-binge drinkers. Addict. Biol 10.1111/adb.12665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolger N, Laurenceau J, 2013. Intensive longitudinal methods: An introduction to diary and experience sampling research. Guilford Press; US, New York. [Google Scholar]
- Brown SA, Vik PW, Patterson TL, Grant I, Schuckit MA, 1995. Stress, Vulnerability and Adult Alcohol Relapse. J. Stud. Alcohol 56, 538–545. [DOI] [PubMed] [Google Scholar]
- Chaplin TM, Hong K, Fox HC, Siedlarz KM, Bergquist KL, 2010. Behavioral arousal in response to stress and drug cue in alcohol and cocaine addicted individuals versus healthy controls. Hum. Psychopharmacol. Clin. Exp 25, 368–376. 10.1002/hup [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatseas M, Serre F, Alexandre JM, Debrabant R, Auriacombe M, Swendsen J, 2015. Craving and substance use among patients with alcohol, tobacco, cannabis or heroin addiction: A comparison of substance- and person-specific cues. Addiction 110, 1035–1042. 10.1111/add.12882 [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, 2004. The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II). Compr. Handb. Psychol. Assess 134–143. 10.1002/9780471726753 [DOI] [Google Scholar]
- First MB, Williams J, Karg R, Spitzer R, 2015. Structured Clinical Interview for DSM-5—Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV). American Psychiatric Publishing, Arlington, VA. [Google Scholar]
- Fox H, Sinha R, 2014. The role of guanfacine as a therapeutic agent to address stress-related pathophysiology in cocaine-dependent individuals. Adv. Pharmacol 69, 218–265. 10.1016/B978-0-12-420118-7.00006-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox HC, Anderson GM, Tuit K, Hansen J, Kimmerling A, Siedlarz KM, Morgan PT, Sinha R, 2012. Prazosin Effects on Stress- and Cue-Induced Craving and Stress Response in Alcohol-Dependent Individuals: Preliminary Findings. Alcohol. Clin. Exp. Res 36, 351–360. 10.1111/j.1530-0277.2011.01628.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox HC, Bergquist KL, Hong KI, Sinha R, 2007. Stress-induced and alcohol cue-induced craving in recently abstinent alcohol-dependent individuals. Alcohol. Clin. Exp. Res 31, 395–403. 10.1111/j.1530-0277.2006.00320.x [DOI] [PubMed] [Google Scholar]
- Fox HC, Hong KIA, Siedlarz K, Sinha R, 2008. Enhanced sensitivity to stress and drug/alcohol craving in abstinent cocaine-dependent individuals compared to social drinkers. Neuropsychopharmacology 33, 796–805. 10.1038/sj.npp.1301470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furnari M, Epstein DH, Phillips KA, Jobes ML, Kowalczyk WJ, Vahabzadeh M, Lin J-LL, Preston KL, 2015. Some of the people, some of the time: field evidence for associations and dissociations between stress and drug use. Psychopharmacology (Berl). 232, 3529–3537. 10.1007/s00213-015-3998-7 [DOI] [PubMed] [Google Scholar]
- Garbutt JC, 2009. The state of pharmacotherapy for the treatment of alcohol dependence. J. Subst. Abuse Treat 36, S15–23; quiz S24–25. [PubMed] [Google Scholar]
- GBD Collaboration, 2018. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 6736, 1–21. 10.1016/S0140-6736(18)31310-2 [DOI] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Patricia Chou S, Jung J, Zhang H, Pickering RP, June Ruan W, Smith SM, Huang B, Hasin DS, 2015. Epidemiology of DSM-5 alcohol use disorder results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry 72, 757–766. 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higley AE, Crane NA, Spadoni AD, Quello SB, Goodell V, Mason BJ, 2011. Craving in response to stress induction in a human laboratory paradigm predicts treatment outcome in alcohol-dependent individuals. Psychopharmacology (Berl). 218, 121–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt WA, Barnett LW, Branch LG, 1971. Relapse Rates in Addiction Programs. J. Clin. Psychol 27, 455–456. 10.1016/j.cnur.2013.05.005 [DOI] [PubMed] [Google Scholar]
- Jobes ML, Ghitza UE, Epstein DH, Phillips KA, Heishman SJ, Preston KL, 2011. Clonidine blocks stress-induced craving in cocaine users. Psychopharmacology (Berl). 218, 83–88. 10.1007/s00213-011-2230-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, Dillworth TM, Simpson T, Waldrop A, Larimer ME, Resick PA, 2007. Domestic violence and alcohol use: Trauma-related symptoms and motives for drinking. Addict. Behav 32, 1272–1283. 10.1016/J.ADDBEH.2006.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, Volkow ND, 2016. Neurobiology of addiction: a neurocircuitry analysis. The Lancet Psychiatry 3, 760–773. 10.1016/S2215-0366(16)00104-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalczyk WJ, Phillips KA, Jobes ML, Kennedy AP, Ghitza UE, Agage DA, Schmittner JP, Epstein DH, Preston KL, 2015. Clonidine maintenance prolongs opioid abstinence and decouples stress from craving in daily life: A randomized controlled trial with ecological momentary assessment. Am. J. Psychiatry 172, 760–767. 10.1176/appi.ajp.2014.14081014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R, Folkman S, 1984. Stress, appraisal, and coping. Spring Pub. Co., New York. [Google Scholar]
- Lê AD, Funk D, Juzytsch W, Coen K, Navarre BM, Cifani C, Shaham Y, 2011. Effect of prazosin and guanfacine on stress-induced reinstatement of alcohol and food seeking in rats. Psychopharmacology (Berl). 218, 89–99. 10.1007/s00213-011-2178-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lê AD, Harding S, Juzytsch W, Watchus J, Shalev U, Shaham Y, Le A, Harding S, Juzytsch W, Watchus J, 2000. The role of corticotrophin-releasing factor in stress-induced relapse to alcohol-seeking behavior in rats. Psychopharmacology (Berl). 150, 317–24. [DOI] [PubMed] [Google Scholar]
- Litt MD, Cooney NL, Morse P, 1998. Ecological momentary assessment (EMA) with treated alcoholics: Methodological problems and potential solutions. Heal. Psychol 17, 48–52. 10.1037/0278-6133.17.1.48 [DOI] [PubMed] [Google Scholar]
- Litten RZ, Ryan ML, Falk DE, Reilly M, Fertig JB, Koob GF, 2015. Heterogeneity of Alcohol Use Disorder: Understanding Mechanisms to Advance Personalized Treatment. Alcohol. Clin. Exp. Res 39, 579–584. 10.1111/acer.12669 [DOI] [PubMed] [Google Scholar]
- Mantsch JR, Baker DA, Funk D, Lê AD, Shaham Y, 2016. Stress-Induced Reinstatement of Drug Seeking: 20 Years of Progress. Neuropsychopharmacology 41, 335–356. 10.1038/npp.2015.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee SA, Sinha R, Weinberger AH, Sofuoglu M, Harrison EL, Lavery M, Wanzer J, 2011. Stress decreases the ability to resist smoking and potentiates smoking intensity and reward. J. Psychopharmacol 25, 490–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda R, Ray L, Blanchard A, Reynolds EK, Monti PM, Chun T, Justus A, Swift RM, Tidey J, Gwaltney CJ, Ramirez J, 2014. Effects of naltrexone on adolescent alcohol cue reactivity and sensitivity: An initial randomized trial. Addict. Biol 19, 941–954. 10.1111/adb.12050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda R, Treloar Padovano H, Gray JC, Wemm SE, Blanchard A, 2018. Real-time assessment of alcohol craving and naltrexone treatment responsiveness in a randomized clinical trial. Addict. Behav 83, 72–78. 10.1016/j.addbeh.2018.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore TM, Seavey A, Ritter K, McNulty JK, Gordon KC, Stuart GL, 2014. Ecological momentary assessment of the effects of craving and affect on risk for relapse during substance abuse treatment. Psychol. Addict. Behav 28, 619–624. 10.1037/a0034127 [DOI] [PubMed] [Google Scholar]
- Noone M, Dua J, Markham R, 1999. Stress, cognitive factors, and coping resources as predictors of relapse in alcoholics. Addict. Behav 24, 687–693. 10.1016/S0306-4603(98)00087-2 [DOI] [PubMed] [Google Scholar]
- Nowinski J, Baker S, Carroll K, 1992. Twelve step facilitation therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. Proj. MATCH Monogr. Ser. 1 [Google Scholar]
- Preston KL, Epstein DH, 2011. Stress in the daily lives of cocaine and heroin users: Relationship to mood, craving, relapse triggers, and cocaine use. Psychopharmacology (Berl). 218, 29–37. 10.1007/s00213-011-2183-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston KL, Kowalczyk WJ, Phillips KA, Jobes ML, Vahabzadeh M, Lin JL, Mezghanni M, Epstein DH, 2018. Exacerbated craving in the presence of stress and drug cues in drug-dependent patients. Neuropsychopharmacology 43, 859–867. 10.1038/npp.2017.275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston KL, Kowalczyk WJ, Phillips KA, Jobes ML, Vahabzadeh M, Lin JL, Mezghanni M, Epstein DH, 2018a. Before and after: craving, mood, and background stress in the hours surrounding drug use and stressful events in patients with opioid-use disorder. Psychopharmacology (Berl). 235, 2713–2723. 10.1007/s00213-018-4966-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston KL, Schroeder JR, Kowalczyk WJ, Phillips KA, Jobes ML, Dwyer M, Vahabzadeh M, Lin JL, Mezghanni M, Epstein DH, 2018b. End-of-day reports of daily hassles and stress in men and women with opioid-use disorder: Relationship to momentary reports of opioid and cocaine use and stress. Drug Alcohol Depend. 193, 21–28. 10.1016/j.drugalcdep.2018.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J, 2009. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 373, 2223–2233. 10.1016/S0140-6736(09)60746-7 [DOI] [PubMed] [Google Scholar]
- Serre F, Fatseas M, Swendsen J, Auriacombe M, 2015. Ecological momentary assessment in the investigation of craving and substance use in daily life: A systematic review. Drug Alcohol Depend. 10.1016/j.drugalcdep.2014.12.024 [DOI] [PubMed] [Google Scholar]
- Shiffman S, 2000. Comments on craving. Addiction 95, 171–175. 10.1046/j.1360-0443.95.8s2.6.x [DOI] [PubMed] [Google Scholar]
- Shiffman S, Gwaltney CJ, Balabanis MH, Liu KS, Paty JA, Kassel JD, Hickcox M, Gnys M, 2002. Immediate antecedents of cigarette smoking: An analysis from ecological momentary assessment. J. Abnorm. Psychol 111, 531–545. 10.1037/0021-843X.111.4.531 [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR, 2008. Ecological Momentary Assessment. Annu. Rev. Clin. Psychol 4, 1–32. 10.1146/annurev.clinpsy.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- Shim RS, Compton MT, Zhang S, Roberts K, Rust G, Druss BG, 2017. Predictors of Mental Health Treatment Seeking and Engagement in a Community Mental Health Center. Community Ment. Health J 53, 510–514. 10.1007/s10597-016-0062-y [DOI] [PubMed] [Google Scholar]
- Simpson TL, Stappenbeck CA, Luterek JA, Lehavot K, Kaysen DL, 2014. Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. J. Abnorm. Psychol 123, 237–247. 10.1037/a0035193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, 2013. The clinical neurobiology of drug craving. Curr. Opin. Neurobiol 10.1016/j.conb.2013.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, 2011. New findings on biological factors predicting addiction relapse vulnerability. Curr. Psychiatry Rep 13, 398–405. 10.1007/s11920-011-0224-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, 2007. The role of stress in addiction relapse. Curr. Psychiatry Rep. 9, 388–395. [DOI] [PubMed] [Google Scholar]
- Sinha R, 2001. How does stress increase risk of drug abuse and relapse? Psychopharmacology (Berl). 158, 343–59. 10.1007/s002130100917 [DOI] [PubMed] [Google Scholar]
- Sinha R, Fox HC, Hong KA, Bergquist K, Bhagwagar Z, Siedlarz KM, 2009. Enhanced negative emotion and alcohol craving, and altered physiological responses following stress and cue exposure in alcohol dependent individuals. Neuropsychopharmacology 34, 1198–208. 10.1038/npp.2008.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Fox HC, Hong KIA, Hansen J, Tuit K, Kreek MJ, 2011a. Effects of adrenal sensitivity, stress- and cue-induced craving,and anxiety on subsequent alcohol relapse and treatment outcomes. Arch. Gen. Psychiatry 68, 942–952. 10.1001/archgenpsychiatry.2011.49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Garcia M, Paliwal P, Kreek MJ, Rounsaville BJ, 2006. Stress-induced cocaine craving and hypothalamic-pituitary-adrenal responses are predictive of cocaine relapse outcomes. Arch. Gen. Psychiatry 63, 324–331. 10.1001/archpsyc.63.3.324 [DOI] [PubMed] [Google Scholar]
- Sinha R, Li CS, 2007. Imaging stress- and cue-induced drug and alcohol craving: association with relapse and clinical implications. Drug Alcohol Rev. 26, 25–31. 10.1080/09595230601036960 [DOI] [PubMed] [Google Scholar]
- Sinha R, Shaham Y, Heilig M, 2011b. Translational and reverse translational research on the role of stress in drug craving and relapse. Psychopharmacology (Berl). 218, 69–82. 10.1007/s00213-011-2263-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Talih M, Malison R, Cooney N, Anderson GM, Kreek MJ, 2003. Hypothalamic-pituitary-adrenal axis and sympatho-adreno-medullary responses during stress-induced and drug cue-induced cocaine craving states. Psychopharmacology (Berl). 170, 62–72. 10.1007/s00213-003-1525-8 [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, 1992. Timeline Follow-Back, in: Measuring Alcohol Consumption. Humana Press, Totowa, NJ, pp. 41–72. 10.1007/978-1-4612-0357-5_3 [DOI] [Google Scholar]
- Stark MJ, 1992. Dropping out of substance abuse treatment: A clinically oriented review. Clin. Psychol. Rev 12, 93–116. 10.1016/0272-7358(92)90092-M [DOI] [Google Scholar]
- Tidey JW, Monti PM, Rohsenow DJ, Gwaltney CJ, Miranda R, McGeary JE, MacKillop J, Swift RM, Abrams DB, Shiffman S, Paty JA, 2008. Moderators of naltrexone’s effects on drinking, urge, and alcohol effects in non-treatment-seeking heavy drinkers in the natural environment. Alcohol. Clin. Exp. Res 32, 58–66. 10.1111/j.1530-0277.2007.00545.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiffany ST, Wray JM, 2012. The clinical significance of drug craving. Ann. N. Y. Acad. Sci 10.1111/j.1749-6632.2011.06298.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray TB, Merrill JE, Monti PM, 2014. Using Ecological Momentary Assessment (EMA) to Assess Situation-Level Predictors of Alcohol Use and Alcohol-Related Consequences. Alcohol Res. 36, 19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X, Lynch JG, Chen Q, 2010. Reconsidering Baron and Kenny: Myths and truths about mediation analysis. J. Consum. Res 37, 197–206. 10.1086/651257 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.