Abstract
Background
Implants made of various types of material can be used for the internal fixation of fractures. Carbon fiber reinforced polyetheretherketone (CFR-PEEK) is a radiolucent material that may have advantageous handling properties compared with titanium implants.
Methods
Seventy-six patients with proximal humerus fractures requiring surgery were randomized to receive a fixed-angle plate made out of either titanium or CFR-PEEK. To measure the functional outcome, the DASH score (Disabilities of Arm, Shoulder, and Hand; primary endpoint), the Simple Shoulder Test (SST), and the Oxford Shoulder Score (OSS) were determined in 63 patients at 6 weeks, 12 weeks, and 6 months after surgery, accompanied at each time point by radiological evaluation.
Results
Both groups displayed improvement in DASH scores 6 months after surgery (CFR-PEEK: 27.5 ± 20.5; titanium: 28.5 ± 17.9; p = 0.82). Sensitivity analysis with multiple imputations confirmed this result (27.4 ± 19.2 versus 28.5 ± 16.6). The OSS and SST scores were likewise improved in both groups. All patients displayed full bony consolidation 12 weeks after surgery. In no case was material failure, secondary dislocation, or screw perforation seen. No difference was seen in the maintenance of postoperative reposition between the CFR-PEEK group and the titanium group.
Conclusion
The internal fixation of proximal humerus fractures with either CFR-PEEK or titanium led to clinical improvement 6 months after surgery. No clinical or radiological difference in outcomes was seen between the two groups. Because of the study design, however, the equivalence of the two interventions was not conclusively demonstrated; a non-inferiority study would have been needed for this purpose.
Fractures of the proximal humerus are common in humans, accounting for 4–5% of all fractures and approximately 10% of fractures in patients over 65 years of age (1– 3). Studies have shown an increasing incidence of this fracture, primarily explained by the increased risk of osteoporosis in the ageing population (4).
Treatment decision making is based on fracture morphology and on patient-specific characteristics such as age, comorbidities, level of physical activity, and adherence.
A broad spectrum of treatments are available for proximal humerus fractures. Breaks with no or only minor displacement can usually be treated conservatively with short-term sling immobilization (5).
Surgical treatment options include internal fixation with fixed-angle (locking) and non-fixed-angle (non-locking) plates, screws, K-wires, intramedullary nails, and total joint replacement. Open reduction and stabilization with locking plates is frequently the treatment of choice for displaced or comminuted fractures of the proximal humerus (6, 7). This strategy aims to achieve anatomic reconstruction and retention of the humeral head.
Plates with different material properties are used for this procedure. Plates made of steel, titanium or, more recently, carbon fiber reinforced polyetheretherketone (CFR-PEEK) are most commonly used. In biomechanical studies, fixation with CFR-PEEK plates allowed for more minimal movements at the fracture site than fixation with titanium plates, with equal or even superior stability of the connection between screws and plate (8– 10). In addition, CRF-PEEK is a radiolucent material, offering the advantage of easier intraoperative and postoperative radiographic assessment of the fracture situation (11). The aim of our study was to compare the functional and radiographic outcomes in patients with proximal humerus fracture treated with internal fixation using locking plates made of CRF-PEEK or titanium. The primary endpoint was the Disabilities of Arm, Shoulder and Hand (DASH) score at 6 months after surgery.
Methods
Study design and study population
In this randomized controlled trial, proximal humerus fractures in 76 patients were managed using plates made of either titanium or CFR-PEEK. The outcome parameters included:
Age
Sex
Body mass index (BMI)
Risk classification according to the American Society of Anesthesiologists (ASA)
Fracture type
Comorbidities
Patients were followed up at 6 weeks, 12 weeks, and 6 months after surgery. The primary endpoint was the DASH score (0–100) at 6 months after surgery. The secondary endpoints included:
Simple Shoulder Test (SST; 0–100%)
Oxford Shoulder Score (OSS; 12–60 points)
Maintenance of reduction outcome (head–shaft angle) (12, 13)
Statistical analysis was performed using the t-test, repeated-measures analysis of variance (rANOVA), Fisher’s exact test, and the chi-square test. The level of significance was set at p<0.05. A detailed description of the methods used is provided in the eMethods. The study procedure with follow-up time points is detailed in eTable 1.
eTable 1. Study procedure with follow-up time points.
| Before surgery | At surgery | After surgery | 1 week | 3 weeks | 5 weeks | 6 weeks | 12 weeks | 6 months | |
| Informed consent | x | ||||||||
| Demographic data | x | ||||||||
| Randomization | x | ||||||||
| Rehabilitation | Immobilization with Gilchrist bandage |
Assisted/active up to 60° flexion/ abduction, 0° external rotation / extension |
Assisted/active up to 90° flexion/ abduction, 20° external rotation/ extension |
Full range of motion permitted |
Full loading permitted (>15 kg) |
||||
| Radiography | x | x | x | ||||||
| DASH test | x | x | x | ||||||
| Simple Shoulder Test | x | x | x | ||||||
| Oxford Shoulder Score | x | x | x | ||||||
| Complications | x | x | x | x | x | x | x | x |
Implants
The CFR-PEEK plate (PEEK Power Humeral Fracture Plate; Arthrex, Naples, Florida, USA) is made of polyetheretherketone (14) reinforced with carbon fibers (55–60%). The plate is anatomically preshaped and designed to allow placement of polyaxial locking screws and fixation of stay sutures at the plate. It is radiolucent and designed for use with 3.5 mm and 4.0 mm titanium screws in the shaft and head of the humerus, respectively (figure 1). The CFR-PEEK–titanium interface eliminates the risk of cold welding between screws and plate. Cold welding is a phenomenon whereby two metal components of identical composition adhere strongly even at room temperature (15). Georgiadis et al. found that when they attempted removal of titanium locking plates from the femur, 17% of the screws were cold welded to the plate (16). In the case of the humerus, three screws (locking or conventional) are used to fix the plate to the shaft and seven screws (locking) at the head.
Figure 1.
A 1– 4: A 56-year-old patient with a left proximal humerus fracture, treated with a CFR-PEEK plate. AP and scapular Y radiographs before and 6 weeks after surgery. B 1– 4: A 63-year-old patient with a left proximal humerus fracture, treated with a titanium plate. AP and scapular Y radiographs before and 6 weeks after surgery.
CFR-PEEK, carbon fiber-reinforced polyetheretherketone; AP, anteroposterior
In the comparison group, a titanium locking plate (Proximal Humerus Internal Locking System—PHILOS; Depuy Synthes, West Chester, Pennsylvania, USA) was used. The plate is anatomically preshaped and also designed to allow placement of locking 3.5 mm titanium screws at the humeral shaft and head as well as fixation to the rotator cuff using stay sutures. Three screws (locking or conventional) can be placed at the humeral shaft and nine screws (locking) at the humeral head (figure 1). In contrast to the CFR-PEEK plate described above, this system does not allow for polyaxial screw placement. Ockert et al. found no advantages or disadvantages associated with the use of plates designed for polyaxial screw insertion in patients with proximal humerus fractures (17).
Results
Altogether, 76 patients (60 women, 16 men) were included in this study. The mean age was 60.7 ± 12.7 years. Thirty-seven (49%) patients were randomized to receive a CRF-PEEK plate and 39 (51%) to receive a titanium plate. There were no significant differences between the two groups with respect to age, BMI, involvement of dominant shoulder, or comorbidity profile (table 1). However, the groups differed significantly with respect to fracture type. The duration of inpatient care after surgery was 4.8 ± 0.4 days in the CFR-PEEK group and 4.9 ± 0.3 days in the titanium group (p = 0.81).
Table 1. Baseline characteristics in the two groups*1.
| Variable | CRF-PEEK | Titanium | p*2 | |
| Number of randomized patients (n) | 37 | 39 | – | |
| Number of patients followed up (n) | 32 | 31 | – | |
| Age (years, mean ± SD) | 61.8 ± 12.4 | 60.9 ± 12.4 | 0.77 | |
| Gender (n) / (%) | Women | 26 (81.3 %) | 24 (77.4 %) | 0.71 |
| Men | 6 (18.8 %) | 7 (22.6 %) | ||
| Neer fracture type (two to four parts) (n) / (%) |
Two-part | 6 (16.2 %) | 5 (23.0 %) | 0.02 |
| Three-part | 22 (64.9 %) | 13 (38.5 %) | ||
| Four-part | 4 (18.9 %) | 13 (38.5 %) | ||
| Dominant side affected (n) / (%) |
Yes | 15 (46.9 %) | 14 (45.2 %) | 0.89 |
| No | 17 (53.1 %) | 17 (54.8 %) | ||
| BMI (kg/m², mean ± SD) | 26.4 ± 5.7 | 26.2 ± 4.7 | 0.91 | |
| Comorbidities – ASA classification (I–VI) (n) / (%) |
I | 2 (6.3 %) | 3 (9.7 %) | 0.87 |
| II | 28 (87.5 %) | 26 (83.9 %) | ||
| III | 2 (6.3 %) | 2 (6.5 %) | ||
*1 The analysis population includes all patients for whom data from at least one follow-up time point are available; *2The t-test (age, BMI), Fisher’s exact test (comorbidities), and the chi-squared test (sex, fracture type, ASA classification) were used to test for differences in patient distribution.
ASA classification, Risk classification of the American Society of Anesthesiologists; BMI, body mass index; CRF-PEEK, carbon fiber reinforced polyetheretherketone; SD, standard deviation
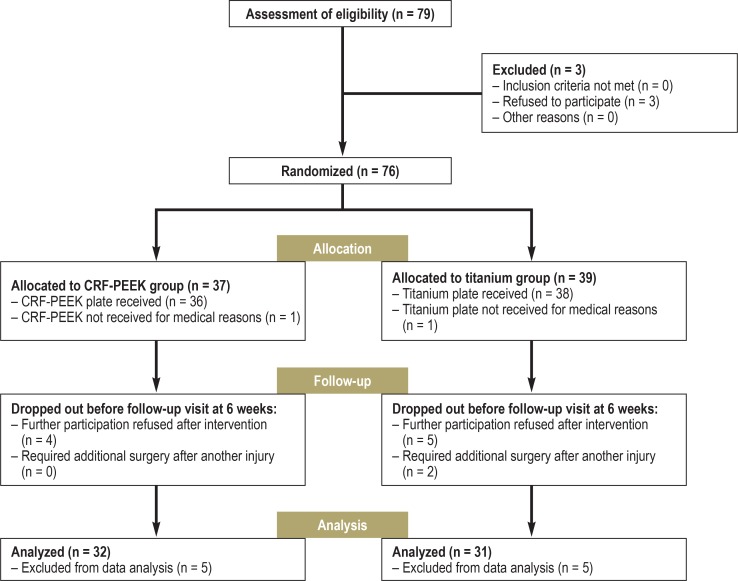
In two patients, a head-split fracture occurred intraoperatively. Two further patients had to undergo surgery a second time because they suffered a new injury after the initial operation. Nine patients withdrew from the study postoperatively without giving a reason. Consequently, 13 patients were not available for postoperative follow-up (figure 2). The analysis of the functional outcomes is based on the remaining group of 63 patients (CFR-PEEK n = 32, titanium n = 31). Surgeon 1 treated 15 patients with a CFR-PEEK plate and 25 patients with a titanium plate. Seventeen CFR-PEEK plates and 6 titanium plates were implanted by surgeon 2.
Figure 2.
CRF-PEEK group versus titanium group: Inclusion and exclusion criteria, randomized allocation to the groups, follow-up and analysis of the two groups
The radiographs obtained 6 weeks after surgery were available for analysis from all patients. Radiographic follow-up at 12 weeks after surgery was performed in 11 cases by community-based specialists; because of the lack of standardization of the radiographs, it was not possible to measure the head–shaft angle. Over the further course of the study, no adverse events, such as infection, displacement, screw perforation, and non-union, were observed.
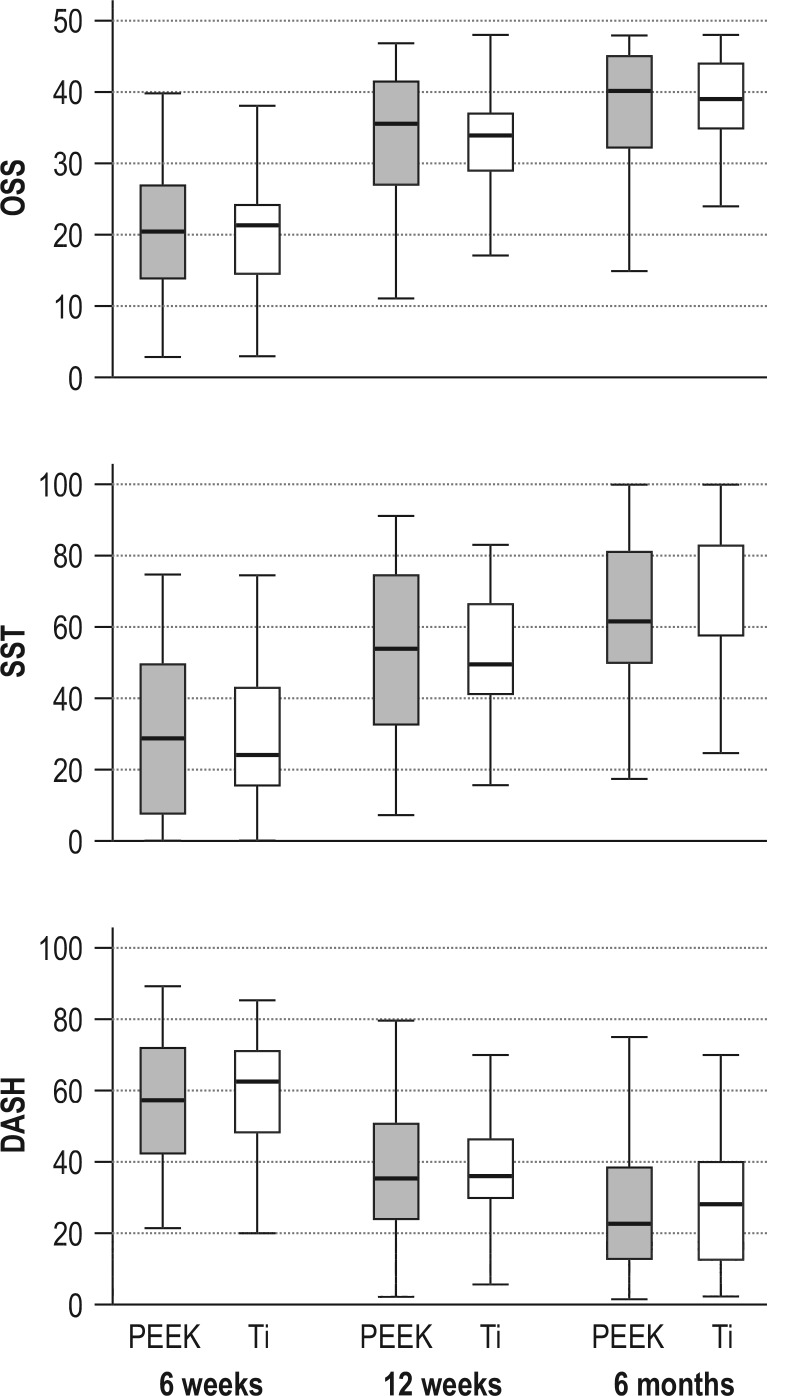
Functional outcome
Six months after surgery, no significant differences were found between the DASH scores of the CFR-PEEK group and the titanium group (27.5 ± 20.5 vs 28.5 ± 17.9; p = 0.82). Sensitivity analysis with multiple imputations confirmed the results of the primary analysis (mean 27.4 ± 19.2 vs 28.5 ± 16.6; p = 0.81). Figure 3 depicts the OSS, SST, and DASH scores of the two groups at all follow-up time points as a box-plot diagram. Improvements in functional outcome were achieved in both groups over the postoperative course (etable 2).
Figure 3.
Functional outcomes of the CFR-PEEK group and the titanium group at 6 weeks, 12 weeks, and 6 months after surgery, measured using (A) the DASH score (0 best score, 100 poorest score), (B) the Simple Shoulder Test (SST; 0 poorest score, 100 best score), and (C) the Oxford Shoulder Score (OSS; 0 = poorest score, 48 = best score). Error bars represent one standard deviation.
Ti, titanium.
eTable 2. Functional outcome.
| Questionnaire | Time point after surgery | PEEK | Titanium | ||
| Mean ± SD | Median (min–max) | Mean ± SD | Median (min–max) | ||
| OSS | 6 weeks | 20.3 ± 9.8 | 20.5 (3.0–40.0) | 20.4 ± 8.5 | 21.5 (3.0–39.0) |
| 12 weeks | 33.8 ± 10.0 | 35.5 (11.0–47.0) | 33.3 ± 6.5 | 34.0 (17.0–48.0) | |
| 6 months | 37.7 ± 8.8 | 40 (15.0–48.0) | 38.6 ± 6.8 | 39.0 (19.0–48.0) | |
| SST | 6 weeks | 30.0 ± 20.8 | 29.2 (0.0–75.0) | 29.4 ± 18.9 | 25.0 (0.0–75.0) |
| 12 weeks | 54.9 ± 24.8 | 54.2 (8.3–91.7) | 51.5 ± 16.5 | 50.0 (16.7–83.3) | |
| 6 months | 62.5 ± 22.3 | 61.8 (18.2–100) | 65.0 ± 20.1 | 58.3 (16.7–100.0) | |
| DASH | 6 weeks | 56.5 ± 19.3 | 56.9 (20.7–88.9) | 59.8 ± 15.6 | 62.5 (19.8–85.3) |
| 12 weeks | 38.4 ± 21.4 | 35.1 (1.7–79.3) | 37.7 ± 16.2 | 35.8 (5.2–73.3) | |
| 6 months | 27.5 ± 20.5 | 22.4 (1.0–81.5) | 28.5 ± 17.9 | 27.6 (1.7–69.8) | |
DASH, Disabilities of Arm, Shoulder and Hand; OSS, Oxford Shoulder Score; PEEK, polyetheretherketone; SD, standard deviation; SST, Simple Shoulder Test
Radiographic outcome
Both in the CFR-PEEK group and in the titanium group, all patients (n = 63) had achieved complete bony consolidation of the fractures by 12 weeks after surgery. No material failure, secondary displacement, or screw perforation was observed. In the CFR-PEEK group, the mean head–shaft angle was 142.46 ± 6.39° immediately after surgery, 142.13 ± 6.38° at 6 weeks after surgery, and 142.53 ± 6.45° at 12 weeks after surgery. The mean head–shaft angles in the titanium group were 139.97 ± 7.70°, 139.82 ± 7.70°, and 138.81 ± 8.21°, respectively. Thus, significant loss of reduction was observed neither in the CFR-PEEK group nor in the titanium group over the postoperative course (table 2).
Table 2. Humerus head–shaft angle at 2–4 days, 6 weeks, and 12 weeks after surgery.
| 2–4 days after surgery | 6 weeks after surgery | 12 weeks after surgery | p* | |
| CFR-PEEK (°) | 142.46 ± 6.39 (n = 32) |
142.13 ± 6.38 (n =3 2) |
142.53 ± 6.45 (n = 28) |
0.065 |
| Titanium (°) | 139.97 ± 7.70 (n = 30) |
139.82 ± 7.70 (n = 30) |
138.81 ± 8.21 (n = 23) |
0.073 |
* Repeated-measures analysis of variance for assessment of differences among the first, second, and third radiographic follow-up examinations.
CFR-PEEK, Carbon fiber reinforced polyetheretherketone
Discussion
In both study groups (CFR-PEEK and titanium), bony consolidation of the treated fractures was confirmed in all patients at 12 weeks after surgery. The functional outcomes 6 months after surgery had improved compared with 6 weeks after surgery. No significant difference was noted between the CFR-PEEK group and the titanium group.
To date, no consensus about the best strategy for the management of proximal humerus fractures has been reached in the literature. In the absence of prospective controlled trials, the superiority of surgical treatment over conservative treatment remains unproven. Comparative studies have not found significant differences between surgical and non-surgical treatment with respect to the outcome parameters, but have shown higher complication rates after surgical procedures (18– 21).
In this study, product-related adverse events were observed neither in the CFR-PEEK group nor in the titanium group during the 3-month follow-up period. The high complication rate described after plating for proximal humerus fractures is directly related to the initial surgical procedure (22, 23). Complications such as primary screw perforation, plate malpositioning, or loss of reduction due to the lack of medial support can be prevented by optimizing the surgical technique. In a multicenter trial, intraoperative screw perforation was observed in 14% of patients after locked plating of proximal humerus fractures (23).
Due to the radiolucent material of the CFR-PEEK plate, it is possible to visualize all the screws used in two-view radiographs without superimposition of the plate on the fracture site. In addition, the polyaxial locking self-tapping screws allow for correct screw placement in the parts of the humeral head with high bone mineral density. Inadequate primary stability and lack of medial support may result in loss of reduction with subsequent varus angulation and in screw cutout with destruction of the glenoid (24– 26). Numerous biomechanical and clinical studies have demonstrated the importance of reconstructing the medial support (27– 30).
Another potential cause of loss of reduction is the high stiffness of the locking plate, which may result in failure of the construct at the screw–bone interface, especially in patients with osteoporosis. Lill et al. studied the initial stiffness of a variety of implants designed for the treatment of proximal humerus fractures (31). They found that implants with lower stiffness and more elastic properties appeared to lessen the peak stresses at the bone–implant interface, which would make them particularly suitable for fracture fixation in osteoporotic bone. Consequently, the CFR-PEEK plate, with elasticity similar to that of human bone, could prevent screw cutout and loss of reduction with subsequent varus angulation, because it is less stiff than conventional titanium plates. In the study by Lill et al., no significant loss of reduction was observed 12 weeks after CFR-PEEK plate fixation of proximal humerus fractures. Schliemann et al. found a lower rate of secondary varus displacement after treatment of proximal humerus fractures with CFR-PEEK plates than in an independent group treated with titanium implants (32). One explanation could be that the high elasticity of the PEEK plate compared with the titanium plate helps to prevent failure of the construct at the screw–bone interface.
According to the most recent literature, both CFR-PEEK plate systems and titanium plate systems achieve good to excellent mid- and long-term clinical results (33– 35). Ockert et al. reported good to outstanding functional long-term outcomes in patients with proximal humerus fracture treated with a locking titanium plate (34). Hirschmann et al. described similar favorable subjective and objective clinical outcomes and a similar complication rate (17%, including pain and stiffness) in patients treated with a conventional titanium locking plate after a median 5 years of follow-up (33).
Rotini et al., in a large study of 160 proximal humerus fractures treated with CFR-PEEK plates (Diphos H), observed no improvement in clinical or functional outcome after 2 years and a low complication rate (9%; complications included a humeral head necrosis and a case with lack of bone healing) compared with the outcomes published in the literature. They highlight as advantages of CFR-PEEK plates the improved intraoperative fluoroscopic visibility of the fracture fragments and the absence of screw-to-plate cold fusion, making plate removal easier than with titanium plates (35).
Our study found similar results with respect to clinical and radiographic outcomes after treatment with CFR-PEEK and titanium plates, despite the difference regarding fracture classification, with a larger number of four-part fractures in the titanium group. For each of the clinical scores, significant improvements were noted between the follow-ups at 6 weeks and 12 weeks and again between 12 weeks and 6 months after surgery. This can be attributed to the reduction in the importance of immobilization as part of the standardized postoperative follow-up care and the subsequent increasing emphasis on active physiotherapeutic treatment.
One of the limitations of our study was the comparatively short follow-up. It cannot be ruled out that some patients developed complications later. Furthermore, comparability of the PEEK group and the titanium group was limited by the fact that randomization of the patients resulted in an unequal distribution of fracture types between the two study groups.
Because the conventional radiographs obtained immediately after surgery and at 6 and 12 weeks after the procedure were interpreted, neither investigators nor patients could be blinded during the follow-up period. The study design did not allow for conclusions on the equivalence of the two interventions. That would have required a non-inferiority study design.
Supplementary Material
eMETHODS
Study design and study population
This randomized controlled trial was registered at the German Registry of Clinical Studies in Freiburg (DRKS00011376, https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00011376), and the protocol was approved by the ethics committee of the University of Tübingen (347/2016MP1). All patients included in this study gave their consent. The randomization list was created before the start of the study, using the “Randbetween” function in MS Excel. The corresponding results (PEEK/titanium) were placed in consecutively numbered envelopes. These were opened by the operating surgeon immediately before the surgical procedure.
Between October 2016 and June 2018, 76 patients treated for proximal humerus fractures at the BG Hospital Tübingen were included in the study and randomized to the titanium group or the CFR-PEEK group by means of a randomization list. There was no blinding of the patients, surgeons, or investigators. The exclusion criteria were bilateral or previous humerus fractures, head-split fractures, rotator cuff arthropathy, neural or vascular injury, thrombophilia, severe heart or lung disease, and alcohol or drug abuse.
Endpoints and follow-up examinations
Preoperatively, demographic data of all patients were documented, including age, gender, body mass index (BMI), risk classification of the American Society of Anesthesiologists (ASA), fracture type, and comorbidities.
Patients were followed up at 6 weeks, 12 weeks, and 6 months after surgery. The primary endpoint was the Disabilities of Arm, Shoulder and Hand (DASH) score (0–100) obtained at 6 months after surgery. Secondary endpoints included:
The scores were obtained in collaboration with a doctoral candidate who had been trained by the principal investigator. For any queries, one of the clinical investigators was consulted. The radiographs were interpreted by two experienced, specialists in orthopedic and trauma surgery independently, based on two-view (anteroposterior and scapular Y) radiographs. To this end, the angle between the tangent to the joint plane and the axis of the humeral shaft was determined (12, 13). For further analysis, the means of the measurements of the two investigators were calculated.
Surgical technique and follow-up care
All surgical procedures were performed using an anterolateral approach (Mackenzie) with the patient under general anesthesia and in beach-chair position. Single-dose perioperative antibiotic prophylaxis with cefuroxime was also administered. The greater and lesser tubercles of the humerus were looped using non-absorbable stay sutures (Fibre Wire 2.0; Arthrex, Naples, Florida, USA), followed by reduction of the fracture by pulling the sutures and/or with the help of K-wires. The respective plate was placed 5 to 8 mm distal to the greater tubercle and directly lateral to the bicipital groove and then fixed using a cortical screw and two 3.5 mm locking screws at the shaft and 3.5 mm locking titanium screws or 4.0 mm locking CRF-PEEK screws at the humeral head.
The surgical technique always included fixation of the stay sutures to the dedicated plate holes. Allogeneic or autogenous cancellous bone grafting was not performed. Intraoperative fluoroscopy was used to assess reduction of fracture fragments and correct placement of implants. Two experienced surgeons specialized in orthopedic and trauma surgery performed all surgical procedures during the study.
After surgery, all patients received a Gilchrist bandage for 7 to 10 days. Pendulum exercises performed with the bandage in place were allowed during this period of immobilization. Subsequently, the range of motion was extended to assisted/active movements up to 60° flexion/abduction and 0° external rotation/extension over a period of 2 weeks. Thereafter, the range of motion was further extended to assisted/active movements up to 90° flexion/abduction and 20° external rotation/extension for another 2-week period. Finally, at 5 weeks after surgery, the full range of motion was permitted. In addition, the patients were instructed not to expose the operated arm to loads of more than 15 kg for a period of 6 weeks after surgery (etable 1).
Statistical analysis
Sample size planning was based on an assumed mean difference between the DASH scores of 5 points with a range of ± 18 points. Based on a desired power of 80%, a sample size of n = 30 patients per group (30 CFR-PEEK and 30 titanium) was calculated. For planning, the independent two sample t-test was used.
The analysis was performed using the SPSS statistical software package (version 24). All obtained data were documented descriptively. Continuous variables were reported as means ± standard deviation. For dichotomous/categorical variables, frequencies and percentage shares, respectively, were reported. For the comparison of baseline characteristics, a two-sided significance level was used.
The independent two sample t-test was used to analyze potential differences between the two groups with respect to the primary endpoint. The postoperative head–shaft angle measurements were evaluated using repeated-measures analysis of variance. Potential preoperative differences between the two groups were calculated using the independent samples t-test (age, BMI), Fisher‘s exact test (comorbidities) or the chi-squared test (sex, fracture type, ASA classification). Values of p<0.05 were regarded as significant.
All patients for whom data from at least one follow-up time point were available were included in the analysis (figure 2). Missing data were not replaced. As a sensitivity analysis with respect to the primary endpoint (DASH), the independent two sample t-test was used with the method of multiple imputations (n = 100), based on all randomized patients.
Simple Shoulder Test (SST; 0–100%)
Oxford Shoulder Score (OSS; 12–60 points)
Maintenance of reduction outcome (head–shaft angle).
Key Messages.
No significant difference between a CFR-PEEK plate and a titanium plate was found at the primary endpoint (DASH score after 6 months).
Internal fixation of a proximal humerus fracture using a CFR-PEEK plate achieved clinical and radiographic outcomes comparable with those using a conventional titanium locking plate.
Both fixation of a proximal humerus fracture using a CFR-PEEK plate and fixation using a titanium plate were associated with significant improvement of the clinical outcomes within 12 weeks after surgery.
The study was not designed to demonstrate the equivalence of the two interventions.
Acknowledgments
Translated from the original German by Ralf Thoene, MD.
Footnotes
Conflict of interest
Dr. Ziegler, Prof. Stöckle, Dr. Gühring, and Dr. Stuby received study support (third party funding) from Arthex.
Mr. Maier declares that no conflict of interest exists.
Data sharing
The authors are willing to share the data with other researchers for scientific purposes. Interested parties should contact Markus Gühring.
Financial support
This study was financially supported by Arthrex.
References
- 1.Passaretti D, Candela V, Sessa P, Gumina S. Epidemiology of proximal humeral fractures: a detailed survey of 711 patients in a metropolitan area. J Shoulder Elbow Surg. 2017;26:2117–2124. doi: 10.1016/j.jse.2017.05.029. [DOI] [PubMed] [Google Scholar]
- 2.Bell JE, Leung BC, Spratt KF, et al. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am. 2011;93:121–131. doi: 10.2106/JBJS.I.01505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baron JA, Karagas M, Barrett J, et al. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7:612–618. doi: 10.1097/00001648-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87–92. doi: 10.1097/01.blo.0000194672.79634.78. [DOI] [PubMed] [Google Scholar]
- 5.Burkhart KJ, Dietz SO, Bastian L, Thelen U, Hoffmann R, Müller LP. The treatment of proximal humeral fracture in adults. Dtsch Arztebl Int. 2013;110:591–597. doi: 10.3238/arztebl.2013.0591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tepass A, Blumenstock G, Weise K, Rolauffs B, Bahrs C. Current strategies for the treatment of proximal humeral fractures: an analysis of a survey carried out at 348 hospitals in Germany, Austria, and Switzerland. J Shoulder Elbow Surg. 2013;22:e8–e14. doi: 10.1016/j.jse.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften. S1 Leitlinie: Oberarmkopffraktur. AWMF-Nr 012-023 18.10.2017 [Google Scholar]
- 8.Schliemann B, Seifert R, Theisen C, et al. PEEK versus titanium locking plates for proximal humerus fracture fixation: a comparative biomechanical study in two- and three-part fractures. Arch Orthop Trauma Surg. 2017;137:63–71. doi: 10.1007/s00402-016-2620-8. [DOI] [PubMed] [Google Scholar]
- 9.Katthagen JC, Schwarze M, Warnhoff M, Voigt C, Hurschler C, Lill H. Influence of plate material and screw design on stiffness and ultimate load of locked plating in osteoporotic proximal humeral fractures. Injury. 2016;47:617–624. doi: 10.1016/j.injury.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Hak DJ, Fader R, Baldini T, Chadayammuri VBS. Locking screw-plate interface stability in carbon-fibre reinforced polyetheretherketone proximal humerus plates. Int Orthop. 2017;41:1735–1739. doi: 10.1007/s00264-017-3562-7. [DOI] [PubMed] [Google Scholar]
- 11.Padolino A, Porcellini G, Guollo B, et al. Comparison of CFR-PEEK and conventional titanium locking plates for proximal humeral fractures: a retrospective controlled study of patient outcomes. Musculoskelet Surg. 2018;102:49–56. doi: 10.1007/s12306-018-0562-8. [DOI] [PubMed] [Google Scholar]
- 12.Hertel R, Knothe U, Ballmer FT. Geometry of the proximal humerus and implications for prosthetic design. J Shoulder Elbow Surg. 2002;11:331–338. doi: 10.1067/mse.2002.124429. [DOI] [PubMed] [Google Scholar]
- 13.Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical treatment of three and four-part proximal humeral fractures. J Bone Joint Surg Am. 2009;91:1689–1697. doi: 10.2106/JBJS.H.00133. [DOI] [PubMed] [Google Scholar]
- 14.Katthagen JC, Ellwein A, Lutz O, Voigt C, Lill H. Outcomes of proximal humeral fracture fixation with locked CFR-PEEK plating. Eur J Orthop Surg Traumatol. 2017;27:351–358. doi: 10.1007/s00590-016-1891-7. [DOI] [PubMed] [Google Scholar]
- 15.Müller M, Mückley, T, Hofmann GO. Kosten und Komplikationen der Materialentfernung. Trauma Berufskrankh. 2007;9(3) [Google Scholar]
- 16.Georgiadis GM, Gove NK, Smith AD, Rodway IP. Removal of the less invasive stabilization system. J Orthop Trauma. 2004;18:562–564. doi: 10.1097/00005131-200409000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Ockert B, Braunstein V, Kirchhoff C, et al. Monoaxial versus polyaxial screw insertion in angular stable plate fixation of proximal humeral fractures: radiographic analysis of a prospective randomized study. J Trauma. 2010;69:1545–1551. doi: 10.1097/TA.0b013e3181c9b8a7. [DOI] [PubMed] [Google Scholar]
- 18.Fjalestad T, Hole MO. Displaced proximal humeral fractures: operative versus non-operative treatment—a 2-year extension of a randomized controlled trial. Eur J Orthop Surg Traumatol. 2014;24:1067–1073. doi: 10.1007/s00590-013-1403-y. [DOI] [PubMed] [Google Scholar]
- 19.Fjalestad T, Hole MO, Hovden IA, Blucher J, Stromsoe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma. 2012;26:98–106. doi: 10.1097/BOT.0b013e31821c2e15. [DOI] [PubMed] [Google Scholar]
- 20.Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011;20:747–755. doi: 10.1016/j.jse.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 21.Sanders RJ, Thissen LG, Teepen JC, van Kampen A, Jaarsma RL, Locking plate versus nonsurgical treatment for proximal humeral fractures: better midterm outcome with nonsurgical treatment J Shoulder Elbow Surg. 2011;20:1118–1124. doi: 10.1016/j.jse.2011.01.025. [DOI] [PubMed] [Google Scholar]
- 22.Schliemann B, Siemoneit J, Theisen C, Kosters C, Weimann A, Raschke MJ. Complex fractures of the proximal humerus in the elderly—outcome and complications after locking plate fixation. Musculoskelet Surg. 2012;96(1):3–11. doi: 10.1007/s12306-012-0181-8. [DOI] [PubMed] [Google Scholar]
- 23.Südkamp N, Bayer J, Hepp P, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate Results of a prospective, multicenter, observational study. J Bone Joint Surg Am. 2009;91:1320–1328. doi: 10.2106/JBJS.H.00006. [DOI] [PubMed] [Google Scholar]
- 24.Brunner F, Sommer C, Bahrs C, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma. 2009;23:163–172. doi: 10.1097/BOT.0b013e3181920e5b. [DOI] [PubMed] [Google Scholar]
- 25.Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2013;22:542–549. doi: 10.1016/j.jse.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 26.Sproul RC, Iyengar JJ, Devcic Z, Feeley BT. A systematic review of locking plate fixation of proximal humerus fractures. Injury. 2011;42:408–413. doi: 10.1016/j.injury.2010.11.058. [DOI] [PubMed] [Google Scholar]
- 27.Erdogan M, Desteli EE, Imren Y, Uzturk A, Kilic M, Sezgin H. The effect of inferomedial screw on postoperative shoulder function and mechanical alignment in proximal humerus fractures. Eur J Orthop Surg Traumatol. 2014;24:1055–1059. doi: 10.1007/s00590-013-1391-y. [DOI] [PubMed] [Google Scholar]
- 28.Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG. The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma. 2007;21:185–191. doi: 10.1097/BOT.0b013e3180333094. [DOI] [PubMed] [Google Scholar]
- 29.Ponce BA, Thompson KJ, Raghava P, et al. The role of medial comminution and calcar restoration in varus collapse of proximal humeral fractures treated with locking plates. J Bone Joint Surg Am. 2013;95 doi: 10.2106/JBJS.K.00202. e113 (1- 7). [DOI] [PubMed] [Google Scholar]
- 30.Zhang L, Zheng J, Wang W, et al. The clinical benefit of medial support screws in locking plating of proximal humerus fractures: a prospective randomized study. Int Orthop. 2011;35:1655–1661. doi: 10.1007/s00264-011-1227-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lill H, Hepp P, Korner J, et al. Proximal humeral fractures: how stiff should an implant be? A comparative mechanical study with new implants in human specimens. Arch Orthop Trauma Surg. 2003;123:74–81. doi: 10.1007/s00402-002-0465-9. [DOI] [PubMed] [Google Scholar]
- 32.Schliemann B, Hartensuer R, Koch T, et al. Treatment of proximal humerus fractures with a CFR-PEEK plate: 2-year results of a prospective study and comparison to fixation with a conventional locking plate. J Shoulder Elbow Surg. 2015;24:1282–1288. doi: 10.1016/j.jse.2014.12.028. [DOI] [PubMed] [Google Scholar]
- 33.Hirschmann MT, Fallegger B, Amsler F, Regazzoni P, Gross T. Clinical longer-term results after internal fixation of proximal humerus fractures with a locking compression plate (PHILOS) J Orthop Trauma. 2011;25:286–293. doi: 10.1097/BOT.0b013e3181f2b20e. [DOI] [PubMed] [Google Scholar]
- 34.Ockert B, Siebenburger G, Kettler M, Braunstein V, Mutschler W. Long-term functional outcomes (median 10 years) after locked plating for displaced fractures of the proximal humerus. J Shoulder Elbow Surg. 2014;23:1223–1231. doi: 10.1016/j.jse.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 35.Rotini R, Cavaciocchi M, Fabbri D, et al. Proximal humeral fracture fixation: multicenter study with carbon fiber peek plate. Musculoskelet Surg. 2015;99(1):1–8. doi: 10.1007/s12306-015-0371-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMETHODS
Study design and study population
This randomized controlled trial was registered at the German Registry of Clinical Studies in Freiburg (DRKS00011376, https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00011376), and the protocol was approved by the ethics committee of the University of Tübingen (347/2016MP1). All patients included in this study gave their consent. The randomization list was created before the start of the study, using the “Randbetween” function in MS Excel. The corresponding results (PEEK/titanium) were placed in consecutively numbered envelopes. These were opened by the operating surgeon immediately before the surgical procedure.
Between October 2016 and June 2018, 76 patients treated for proximal humerus fractures at the BG Hospital Tübingen were included in the study and randomized to the titanium group or the CFR-PEEK group by means of a randomization list. There was no blinding of the patients, surgeons, or investigators. The exclusion criteria were bilateral or previous humerus fractures, head-split fractures, rotator cuff arthropathy, neural or vascular injury, thrombophilia, severe heart or lung disease, and alcohol or drug abuse.
Endpoints and follow-up examinations
Preoperatively, demographic data of all patients were documented, including age, gender, body mass index (BMI), risk classification of the American Society of Anesthesiologists (ASA), fracture type, and comorbidities.
Patients were followed up at 6 weeks, 12 weeks, and 6 months after surgery. The primary endpoint was the Disabilities of Arm, Shoulder and Hand (DASH) score (0–100) obtained at 6 months after surgery. Secondary endpoints included:
The scores were obtained in collaboration with a doctoral candidate who had been trained by the principal investigator. For any queries, one of the clinical investigators was consulted. The radiographs were interpreted by two experienced, specialists in orthopedic and trauma surgery independently, based on two-view (anteroposterior and scapular Y) radiographs. To this end, the angle between the tangent to the joint plane and the axis of the humeral shaft was determined (12, 13). For further analysis, the means of the measurements of the two investigators were calculated.
Surgical technique and follow-up care
All surgical procedures were performed using an anterolateral approach (Mackenzie) with the patient under general anesthesia and in beach-chair position. Single-dose perioperative antibiotic prophylaxis with cefuroxime was also administered. The greater and lesser tubercles of the humerus were looped using non-absorbable stay sutures (Fibre Wire 2.0; Arthrex, Naples, Florida, USA), followed by reduction of the fracture by pulling the sutures and/or with the help of K-wires. The respective plate was placed 5 to 8 mm distal to the greater tubercle and directly lateral to the bicipital groove and then fixed using a cortical screw and two 3.5 mm locking screws at the shaft and 3.5 mm locking titanium screws or 4.0 mm locking CRF-PEEK screws at the humeral head.
The surgical technique always included fixation of the stay sutures to the dedicated plate holes. Allogeneic or autogenous cancellous bone grafting was not performed. Intraoperative fluoroscopy was used to assess reduction of fracture fragments and correct placement of implants. Two experienced surgeons specialized in orthopedic and trauma surgery performed all surgical procedures during the study.
After surgery, all patients received a Gilchrist bandage for 7 to 10 days. Pendulum exercises performed with the bandage in place were allowed during this period of immobilization. Subsequently, the range of motion was extended to assisted/active movements up to 60° flexion/abduction and 0° external rotation/extension over a period of 2 weeks. Thereafter, the range of motion was further extended to assisted/active movements up to 90° flexion/abduction and 20° external rotation/extension for another 2-week period. Finally, at 5 weeks after surgery, the full range of motion was permitted. In addition, the patients were instructed not to expose the operated arm to loads of more than 15 kg for a period of 6 weeks after surgery (etable 1).
Statistical analysis
Sample size planning was based on an assumed mean difference between the DASH scores of 5 points with a range of ± 18 points. Based on a desired power of 80%, a sample size of n = 30 patients per group (30 CFR-PEEK and 30 titanium) was calculated. For planning, the independent two sample t-test was used.
The analysis was performed using the SPSS statistical software package (version 24). All obtained data were documented descriptively. Continuous variables were reported as means ± standard deviation. For dichotomous/categorical variables, frequencies and percentage shares, respectively, were reported. For the comparison of baseline characteristics, a two-sided significance level was used.
The independent two sample t-test was used to analyze potential differences between the two groups with respect to the primary endpoint. The postoperative head–shaft angle measurements were evaluated using repeated-measures analysis of variance. Potential preoperative differences between the two groups were calculated using the independent samples t-test (age, BMI), Fisher‘s exact test (comorbidities) or the chi-squared test (sex, fracture type, ASA classification). Values of p<0.05 were regarded as significant.
All patients for whom data from at least one follow-up time point were available were included in the analysis (figure 2). Missing data were not replaced. As a sensitivity analysis with respect to the primary endpoint (DASH), the independent two sample t-test was used with the method of multiple imputations (n = 100), based on all randomized patients.
Simple Shoulder Test (SST; 0–100%)
Oxford Shoulder Score (OSS; 12–60 points)
Maintenance of reduction outcome (head–shaft angle).