SUMMARY
Health care disparities affecting the care of multiple disease groups are of growing concern internationally. Research guidelines, governmental institutions, and scientific journals have attempted to minimize disparities through policies regarding the collection and reporting of racial/ethnic data. One area where shortcomings remain is in gastroesophageal reflux disease (GERD). This systematic review, which adheres to the PRISMA statement, focuses on characterizing existing methodological weaknesses in research focusing on studies regarding the assessment, prevalence, treatment, and outcomes of GERD patients. Search terms included GERD and typical symptoms of GERD in ethnic groups or minorities. We reviewed 62 articles. The majority of studies did not report the race/ethnicity of all participants, and among those who did, very few followed accepted guidelines. While there were diverse participants, there was also diversity in the manner in which groups were labeled, making comparisons difficult. There appeared to be a disparity with respect to countries reporting race/ethnicity, with certain countries more likely to report this variable. Samples overwhelmingly consisted of the study country's majority population. The majority of studies justified the use of race/ethnicity as a study variable and investigated conceptually related factors such as socioeconomic status and environment. Yet, many studies wrote as if race/ethnicity reflected biological differences. Despite recommendations, it appears that GERD researchers around the world struggle with the appropriate and standard way to include, collect, report, and discuss race/ethnicity. Recommendations on ways to address these issues are included with the goal of preventing and identifying health care disparities.
Keywords: gastroesophageal reflux, health services research, outcomes research
INTRODUCTION
Health care disparities exist when quality of health care differs by racial or ethnic group.1 Disparities are well known across multiple disease groups and are of growing concern internationally.2,3 As an undue burden of health problems are disproportionately experienced by marginalized groups, including minority ethnic and racial groups, one of the best ways to close the gap on disparities is to systematically include diverse participants in research.2 Although race/ethnicity are recognized as social constructs, the collection of racial/ethnic data as a way to prevent and identify health disparities is emphasized for scientific and ethical reasons.3,4 Indeed, both the National Institutes of Health (NIH) and International Committee of Medical Journal Editors (ICMJE) have policies regarding the need for researchers to collect, report, and describe how they determined the racial/ethnic makeup of participants.5,6 Yet, reporting of race/ethnicity of study participants remains low and inconsistent around the world.7–9
Gastroesophageal reflux disease (GERD) is a particularly important area of research as it is a common and costly disease.10,11 Many individuals suffer from GERD; with epidemiological studies identifying it as a common condition throughout the world.11,12 In addition to its high prevalence, GERD is costly and is associated with impairment in quality of life and health complications.10,11,13,14 Given the aforementioned factors, identifying whether race/ethnicity are included and reported in GERD research is an important step toward identifying and preventing health disparities. Research in other chronic diseases show that race/ethnicity can impact the domains of assessment, prevalence, treatment, and outcomes and contribute to health disparities.15,16 We hypothesized that similar disparities may also occur in GERD and drive inequalities in disease burden. Thus, we sought to identify, analyze, and critique the current evidence in relation to GERD with consideration of the aforementioned domains. The goals are to determine how studies report race/ethnicity, identify disparities, and use our results to guide recommendations for future research. As some readers may not have a background in health care disparity research, Table 1 provides an overview of key concepts and recommendations.
Table 1.
Key concepts and recommendations to improve research in GERD among diverse populations
| • | Use appropriate standards for racial/ethnic collection and classification based on policy (e.g. NIH policies) including: allowing participants to self-report/identify their race/ethnicity, using two questions to first collect ethnicity then race, and reporting the identification of all participants including multiracial categories |
| • | Use identified standards when writing about race/ethnicity, particularly when discussing racial/ethnic differences (e.g. Kaplan and Bennett, NIH, ICMJE, and CSE policies) including: define how race/ethnicity was determined, justify the use of race/ethnicity as a study variable, follow guidance of appropriate and up-to-date terminology (ex: White instead of Caucasian or Native Hawaiian/Other Pacific Islander instead of Asian/Pacific Islander), and distinguish race/ethnicity as a risk marker rather than risk factor (i.e. race/ethnicity may point to risk factors like experiences of discrimination, social class, or genetics) |
| • | Collect a range of variables that are conceptually related to the social constructs of race/ethnicity (e.g. socioeconomic status, cultural health beliefs and practices, experiences of racism/discrimination) |
| • | Increase representation of diverse participants (e.g. use Community-based participatory research methods to structure study and recruitment, follow NIH and ICMJE policies of inclusion of diverse samples) |
| • | Increase health care disparity research in the field of GERD |
MATERIALS AND METHODS
Studies meeting the criteria listed below were included.
Inclusion criteria
GERD diagnosed using well-established criteria (e.g. Montreal classification, validated measure, physician diagnosis);
Montreal GERD definition: ‘the presence of troublesome heartburn and/or regurgitation’ of any severity on at least 1 day a week;12
Adults
Published any year
Controlled studies, randomized controlled trial, prospective, retrospective, and cross-sectional designs;
Peer-reviewed.
Exclusion criteria
Languages other than English;
Conference abstracts or short papers with incomplete data;
Case reports, case series, or qualitative research;
Reviews, opinion papers;
Animal studies.
SEARCH METHODOLOGY
Search strategy
A librarian (LO) developed the search strategies with other review authors (MC, LK2) and in April/May 2016 ran searches in: PubMed MEDLINE; Embase (embase.com); and Cochrane Central Register of Controlled Trials (CENTRAL) on the Wiley platform. All databases were searched back to their inception. A full list of strategies and terms used is provided (Appendix 1).
Data collection, extraction, and analysis
The systematic review used the PRISMA statement guidelines (http://www.prisma-statement.org) (Appendix 2) and the review protocol recommendations of Pai et al.17 During phase one, two independent reviewers [MC and LK1] screened the titles and abstracts. During phase two, the full text of articles were screened by two independent reviewers [MC and LK1]. Articles not meeting review criteria were excluded, with reasons documented. Relevant data (i.e. design, setting, manner of GERD diagnosis, etc.) were extracted from included articles. Throughout, disagreements were resolved through discussion. Each study was reviewed to determine whether the race/ethnicity of all participants was reported, if so, number of participants and associated descriptive terms were recorded.
Data synthesis
This review was guided by two frameworks: The Institute of Medicine's (IOM) 2002 report, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care and Kaplan and Bennett's 2003 special communication, Use of Race and Ethnicity in Biomedical Publication.18,19 We used the IOM’s definition of a health care disparity—when quality of health care differs by racial/ethnic group and is not due to access-related factors or clinical needs, preferences, and appropriateness of intervention.1 We used methods of investigation and analysis from Kaplan and Bennett's (2003) recommendations including (1) how studies collected, presented, analyzed, and rationalized reporting race/ethnicity, (2) whether factors beyond race/ethnicity were considered when differences were identified (socioeconomic status and health beliefs) and (3) whether authors distinguished race/ethnicity as a risk marker rather than a risk factor (race/ethnicity may reflect risk factors like access to care, environmental hazards or social class).19
Quality assessment
Two reviewers (MC, ES) divided and independently reviewed the full articles identified for inclusion to evaluate study quality. The quality appraisal of the studies was assessed using a scale developed a priori for the specific needs of this study (Appendix 3), based on recommendations from Sanderson et al.20 regarding key domains to assess in critical appraisal. We also consulted with a gastrointestinal health psychologist regarding the scale. We interpreted the quality in the following manner: if the mean quality score for the domain was between 0 and 30% on the rating scale it was considered low; 31–60% was considered moderate; and 61–100% was considered high.
RESULTS
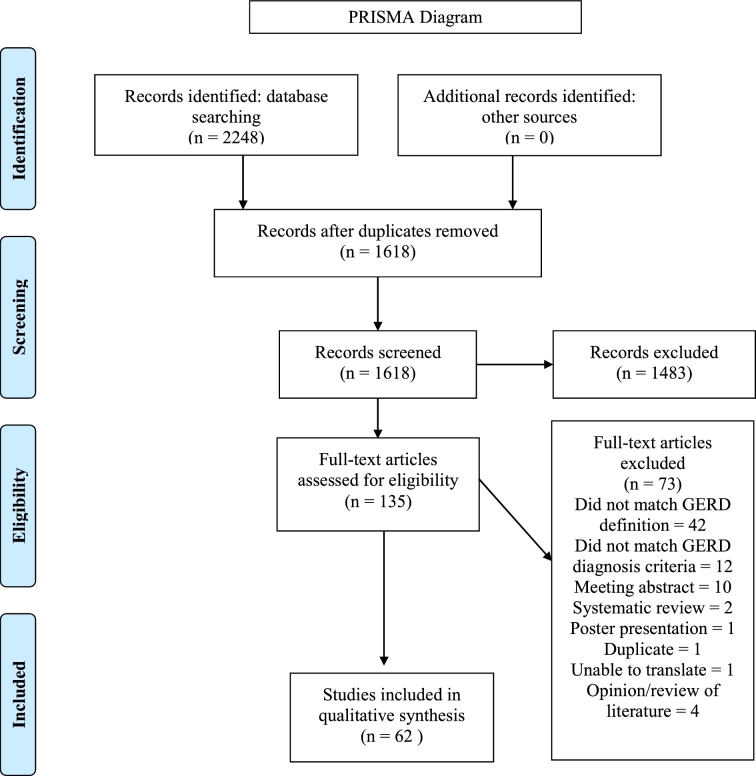
A total of 2248 articles were identified across all databases (PubMed: 790; Embase: 1360; CENTRAL: 98). After removing duplicates, titles and abstracts were screened for the remaining 1618 papers. 1,483 did not meet the inclusion criteria (see Appendix 2), leaving 135 included for full review, of which 62 met criteria.
Study characteristics
Most studies originated or had subjects in Asia (51%), followed by North America (26%), Europe (6%), Middle East (13%), Africa (3%), and South America (1%). Summary characteristics of the studies, categorized by domain, are presented in Table 2.
Table 2.
Summary characteristics of studies that met inclusion criteria
| Domain | Number of studies | Study location | Study design | Sample size |
|---|---|---|---|---|
| Assessment | 8 | Japan (3), China (2), United States of America (USA) (2), Singapore (1) | Cross-sectional (4), Cohort (4) | N = 10,501 |
| Prevalence | 31 | China (8), USA (7), Iran (4), India (2), Japan (2), Argentina (1), Israel (1), Korea (1), Singapore (1), Switzerland (1), Tunisia (1), Turkey (1), United Kingdom (UK) (1) | Cross-sectional (22), Cohort (8), Case-control (1) | N = 106,885 |
| Treatment | 14 | USA (4), Japan (4), Canada (1), China (1), Pakistan (1), Singapore (1), Taiwan (1), Multi-site: Ireland, South Africa, and the UK (1) | Cohort (6), Randomized Controlled Trial (7), Cross-sectional (1), | N = 3,620 |
| Biological outcomes | 5 | USA (2), India (1), Iran (1), Switzerland (1) | Cohort (3), Cross-sectional (2) | N = 2,484 |
| Psychosocial outcomes | 6 | China (2), Iran (1), Japan (1), USA, (1), Multi-site: Germany, Austria, and Switzerland (1) | Randomized placebo-controlled trial (1), Cross-sectional (3), Cohort (1), Longitudinal (1) | N = 22,977 |
GERD study outcomes
From the 62 unique studies that met initial criteria, we identified 25 (40%) studies that reported the ethnic and/or racial makeup of all participants. Study characteristics are presented in Tables 3–7.
Table 3.
Summary characteristics of the studies addressing domain 1: assessment
| Authors, year, country, quality score | Design, setting, recruitment | Participants (sample size, median/mean age and range, sex, GERD diagnosis) | Race/ethnicity how assigned | Justification of race/ethnicity examination of differences |
|---|---|---|---|---|
| Coyne et al. 23 USA Quality: 6 | Cohort; Convenience sample of GERD patients were recruited through seven clinical centers | 198, mean age 50.7, 68% female, patient's chart | White 83% | Did not provide justification for race/ethnicity as study variable |
| African American 11% | ||||
| Other 5% | ||||
| Not described | ||||
| Did not examine differences based on race/ethnicity: analysis and interpretation did consider conceptually relevant factors, did not control for SES | ||||
| Ho et al.24 Singapore Quality: 7 | Cross-Sectional; Fifty-five primary care physicians from various private practices consecutively screened and randomly recruited eligible patients | 209, mean age 41.3, range 19–70, 64% female, gastroenterologist's diagnosis | Chinese 90% | Provided justification for race/ethnicity as study variable |
| Malay 3.3% | ||||
| Indian 5.3 | ||||
| Other 1.4% | ||||
| Not described | ||||
| Did not examine differences based on race/ethnicity: analysis and interpretation did consider conceptually relevant factors, did not control for SES | ||||
| Spiegel et al. 25 USA Quality: 5 | Cross-sectional; Eleven clinical gastroenterology and primary care sites recruited patients who met the study eligibility criteria | 212, mean age 45, 76% female, pH probe or endoscopy or radionuclide milk study, or (ii) with response to acid suppressive medication or (iii) physician diagnosis of GERD | Caucasian 68.4% | Did not provide justification for race/ethnicity as study variable |
| Hispanic 19.3% | ||||
| Black 7.6% | ||||
| Other 3.3% | ||||
| Asian 1.4% | ||||
| Not described | ||||
| Did not examine differences based on race/ethnicity: analysis did consider conceptually relevant factors, did not control for SES | ||||
GERD, gastroesophageal reflux disease; SES, socioeconomic status.
Table 7.
Summary characteristics of the studies addressing domain 4: psychosocial outcomes
| Authors, year, country, quality score | Design, setting, recruitment | Participants (sample size, median/mean age and range, sex, GERD diagnosis) | Race/ethnicity How assigned | Justification of race/ethnicity Examination of differences |
|---|---|---|---|---|
| Damiano et al.40 USA Quality: 8 | Randomized controlled trial; recruitment not described | 223, mean age 43.49, 67.26% female, validated measure and endoscopy | Caucasian 77.58% African-American 12.56% Hispanic 7.62% Asian 0.9% Other 1.35% Not described | Did not provide justification for race/ethnicity as study variable Did not examine differences based on race/ethnicity: analysis and interpretation did not consider conceptually relevant factors, did not control for SES |
| Masoumi et al.46 Iran Quality: 8 | Cross-sectional; Subjects were selected by the cluster random sampling method based on socioeconomic status census data | 717, mean age 43.1, range 25–85, 60.4% female, validated measure | Qashqai 100% Coordinated with the Fards Nomadic Affairs org and used a guide to visit subjects in their tents | Provided justification for race/ethnicity as study variable Analysis and interpretation did consider conceptually relevant factors: analysis and interpretation did consider conceptually relevant factors, did not control for SES |
GERD, gastroesophageal reflux disease; SES, socioeconomic status.
Table 4.
Summary characteristics of the studies addressing domain 2: prevalence
| Authors, year, country, quality score | Design, setting, recruitment | Participants (sample size, median/mean age and range, sex, GERD diagnosis) | Race/ethnicity how assigned | Justification of race/ethnicity Examination of differences |
|---|---|---|---|---|
| Balasubramanian et al. 26 USA Quality: 7 | Cohort; Veterans Affairs Medical Center; Consecutive patients presenting for index upper endoscopy for GERD were prospectively enrolled | 1058, mean age 57.2, 8.6% female, validated measure and endoscopy | Caucasian 82.3% African American 8.1% Other 3.5% Not described | Provided justification for race/ethnicity as study variable Examined differences based on race/ethnicity: identified race as risk factor (not marker), did not consider conceptually relevant factors, did not control for SES |
| Bhatia et al. 27 India Quality: 2 | Cross-sectional; Convenience sample from 12 centers: study, academic centers, tertiary care corporate hospitals and community centers from both rural and urban areas | 3224, median age 38.4 48.3% female, nonvalidated questionnaire | Southern Indian 51.2% Northern Indian 48.8% State resided in | Provided justification for race/ethnicity as study variable Examined differences based on region but no significant findings |
| El-Serag et al. 28 USA Quality: 10 | Cross-sectional; Veterans Affairs Medical Center; Randomly selected from racially representative sample | 496, mean age 45, range: 18–75, 68% female, validated measure and endoscopy | Black 43% White 34% Hispanic 8% Asian 11% Native American 1% Other 3% Not described | Provided justification for race/ethnicity as study variable Examined differences based on race/ethnicity: identified race as risk factor (not marker), did consider conceptually relevant factors, did not control for SES |
| Friedenberg et al.29 USA Quality: 10 | Cohort; Urban hospital; Complex stratified sampling/random sample using zip codes/zone stratification | 379, mean age 43.2, 60.5% female, validated measure | Black American 100% ‘Self-described as a Black American’ | Provided justification for race/ethnicity as study variable Did not examine differences based on race/ethnicity: analysis and interpretation did consider conceptually relevant factors, did control for SES |
| Gerson et al.30 USA Quality: 9 | Cohort; Multiple sites; prospectively enrolled patients undergoing endoscopic evaluation for GERD | 751, mean age 55.4, 26% female, validated measure and endoscopy or 24-hour pH testing | Caucasian 75% Hispanic 12% African-American 6% Asian/Pacific Islander 5% Native American 2% Self-report | Provided justification for race/ethnicity as study variable Examined differences based on race/ethnicity: identified race as risk factor (not marker), did consider conceptually relevant factors, did control for SES |
| Islami et al.31 Iran Quality: 6 | Cross-sectional; Randomly selected urban inhabitants from Gonbad City by systematic clustering based on the household number | 50,001, mean age 52.1, 57.6% female, face-to-face interviews using structured questionnaires to collect data on GERD | Turkmen 74.43% Non-Turkmen 25.57% Self-report | Provided justification for race/ethnicity as study variable Examined differences based on race/ethnicity: identified ethnicity as a risk marker, did consider conceptually relevant factors, did control for SES |
| Lim et al. 32 Singapore Quality: 8 | Cohort; Race-stratified random sample of residents in a Singaporean town | 237, mean age 46, range 25–89, 51% female, validated measure | Chinese 45% Malay 29% Indian 25% Self-report | Provided justification for race/ethnicity as study variable Examined differences based on race/ethnicity: ran analysis to see if race was a risk factor, did consider conceptually relevant factors, did control for SES |
| Niu et al.33 China Quality: 10 | Cross-sectional; People who were residents of Zinjiang China who attended the First Affiliated Hospital of Xinjiang Medical University for a health examination were recruited | 1995, mean age 43.5, range 23–63, 28% female, validated measure and endoscopy, 24-hour PH testing, or PPI test | Uygur Chinese 54% Han Chinese 46% Not described | Provided justification for race/ethnicity as study variable Examined differences based on race/ethnicity: identified ethnicity as a risk marker, did consider conceptually relevant factors, did control for SES |
| Nouraie et al. 34 Iran Quality: 7 | Cross-sectional; Computer-generated random sample of the Tehran province was selected using the postcodes | 2,561, mean age 35.5, 57.7% female, direct interview using nonvalidated measure | Fars 55.8% Turk 32.3% Kurd 3.3% Lore 3.2% Guilak 3.4% Other (Arab, Balooch, Turkeman) 2.0% Self-report | Provided justification for race/ethnicity as study variable Examined differences based on race/ethnicity: identified ethnicity as a risk marker, did consider conceptually relevant factors, did not control for SES |
| Sperber et al.35 Israel Quality: 8 | Cross-sectional; Random selection of phone numbers | 981, mean age was 45, 55% female, validated measure | Israeli Jewish 100% Israeli Ministry of the Interior provided database containing a representative sample of the Israeli Jewish adult population | Provided justification for race/ethnicity as study variable Did not examine differences based on race/ethnicity: analysis and interpretation did consider conceptually relevant factors |
| Srinivasan et al. 36 USA Quality: 8 | Cross-sectional; Non-standardized method to sample patients in Philadelphia County | 410, mean age 44.2, 57.8% female, validated measure | White 54.2% Black 36.6% Native/Alaskan 2.5% Asian/Pacific 2% Other 4.9% Self-report | Provided justification for race/ethnicity as study variable Examined differences based on race/ethnicity: did consider conceptually relevant factors, did not control for SES |
| Wong et al.37 China Quality: 7 | Cross-sectional; Random telephone numbers were generated by computer | 2209, mean age 40.3, 58% female, validated measure | Ethnic Chinese 100% ‘Only numbers corresponding to ethnic Chinese were used’ | Provided justification for race/ethnicity as study variable Did not examine differences based on race/ethnicity: analysis and interpretation did consider conceptually relevant factors, did control for SES |
| Yang et al. 38 Korea Quality: 8 | Cross-sectional; Random sample of telephone numbers was drawn based on the population distribution within the eight provinces of South Korea | 1044, mean age not reported, 50.6% female, validated measure | South Korean 100% Self-report | Provided justification for race/ethnicity as study variable Did not examine differences based on race/ethnicity: analysis and interpretation did consider conceptually relevant factors, did control for SES |
| Yuen et al.39 USA Quality: 6 | Cross-sectional; attending local community centers or faith-based community activities or health fairs in specific ethnic sections of Philadelphia | 1172, mean age not reported, 67% female, self-report | African American 34% Caucasian 27% Hispanic 21% Asian 18% Self-report | Provided justification for race/ethnicity as study variable Examined differences based on race/ethnicity: identified ethnicity as a risk marker, did consider conceptually relevant factors, did control for SES |
GERD, gastroesophageal reflux disease; SES, socioeconomic status.
Table 5.
Summary characteristics of the studies addressing domain 3: treatment
| Authors, year, country, quality score | Design, setting, recruitment | Participants (sample size, median/mean age and range, sex, GERD diagnosis) | Race/ethnicity how assigned | Justification of race/ethnicity examination of differences |
|---|---|---|---|---|
| Damiano et al.40 USA Quality: 8 | Randomized controlled trial; recruitment not described | 223, mean age 43.49, 67.26% female, validated measure and endoscopy | Caucasian 77.58% African-American 12.56% Hispanic 7.62% Asian 0.9% Other 1.35% Not described | Did not provide justification for race/ethnicity as study variable Did not examine differences based on race/ethnicity: analysis and interpretation did not consider conceptually relevant factors, did not control for SES |
| Degl' Innocenti et al. 41 Canada Quality: 3 | Cohort; Patients were recruited in 13 gastroenterology practices and four general practices across Canada | 217, mean age 50, range: 20–82, 52.5% female, nonvalidated measure | Caucasian 88% Other 12% ‘Trained research assistants collected information concerning demographic data’ | Provided justification for race/ethnicity as study variable Examined differences based on race/ethnicity: did not consider conceptually relevant factors, did not control for SES |
| Fass et al.42 USA Quality: 4 | Randomized controlled trial; Patients were recruited at 52 US research sites, including office practices, research clinics, and academic hospitals | 282, mean age 49, 59.4% female, daily symptom diary | White 84% Black 10% Hispanic 5% Other 1% Not described | Provided justification for race/ethnicity as study variable Did not examine differences based on race/ethnicity: analysis and interpretation did not consider conceptually relevant factors, did not control for SES |
| Fock et al. 43 Singapore Quality: 6 | Randomized controlled trial; recruitment not described | 127, mean age 38.9, 48.8% female, symptom interview with physician | Chinese 79.5% Malay 7.1% Indian 11.8% Other 1.6% Not described | Provided justification for race/ethnicity as study variable Did not examine differences based on race/ethnicity: interpretation did consider conceptually relevant factors, did not control for SES |
| Karim et al.44 Pakistan Quality: 6 | Cross sectional study; Multicenter tertiary care hospitals; Randomly selected by computer generated charts | 1875, mean age 35.37, 46% female, validated measure | Punjabi 16% Sindhi 14.8% Pashto 12.1% Blauchi 5.1% Urdu 51.9% Self-report | Provided justification for race/ethnicity as study variable Examined differences based on race/ethnicity: identified ethnicity as risk factor (not marker), did consider conceptually relevant factors, did not control for SES |
| Morgan et al.21 USA Quality: 5 | Randomized controlled trial; Eight centers; recruitment not described | 83, mean age 38.7, 63% female, self-report | Self-identified ethnicity as Hispanic or Latino 100% Race self-defined as White 87% Black 6% American Indian 5% Other 2% ‘Self-identification of ethnicity and race according to the NIH standard was used’ | Provided justification for race/ethnicity as study variable Did not examine differences based on race/ethnicity: analysis and interpretation did consider conceptually relevant factors |
GERD, gastroesophageal reflux disease; SES, socioeconomic status.
Table 6.
Summary characteristics of the studies addressing domain 4: biological outcomes
| Authors, year, country, quality score | Design, setting, recruitment | Participants (sample size, median/mean age and range, sex, GERD diagnosis) | Race/ethnicity How assigned | Justification of race/ethnicity examination of differences |
|---|---|---|---|---|
| Gaddam et al.45 USA Quality: 9 | Cohort; Veterans Affairs Medical Center; Consecutive patients presenting to the gastrointestinal endoscopy unit for evaluation of GERD symptoms undergoing index endoscopy were prospectively enrolled. | 908, mean age 57.2, 7.1% female, validated measure and endoscopy | White 83.1% African American 13.9% Other 3% ‘noted at the time of enrollment’ | Did provide justification for race/ethnicity as study variable Examined differences based on race but no significant findings; ran analysis to see if race was a risk factor, did not control for SES |
GERD, gastroesophageal reflux disease; SES, socioeconomic status.
Domain 1 (Assessment): (n = 3)
Only one of the assessment studies provided justification for using race/ethnicity as a study variable and none examined racial/ethnic differences posthoc.
Domain 2 (Prevalence): (n = 14)
All of the prevalence studies provided justification for using race/ethnicity as a study variable. Among the nine that examined racial/ethnic differences and found significant results, four identified race/ethnicity as a risk marker rather than factor, eight considered conceptually relevant factors such as environmental exposures, social class, diet, and health beliefs when interpreting racial/ethnic differences, and eight controlled or adjusted for socioeconomic status during analysis.
Domain 3 (Treatment): (n = 6)
Five of the six treatment studies provided justification for using race/ethnicity as a study variable. Two studies examined racial/ethnic differences. Only one considered conceptually relevant factors, such as diet and health practices, neither adjusted for socioeconomic status, and one identified race as a risk factor, rather than marker.
Domain 4 (Biological Outcomes): (n = 1)
The one biological outcome study provided justification for using race/ethnicity as a study variable. Although the authors reported examining demographic factors as independent risk factors, they did not find significant differences based on race. This also indicates that they were identifying race as a potential risk factor, rather than risk marker.
Domain 5 (Psychosocial Outcomes): (n = 2)
Only one of the psychosocial outcome studies provided justification for using race/ethnicity as a study variable. While neither examined differences based on race/ethnicity, one study did consider conceptually relevant factors, such as tribal affiliation, diet and health practices, when interpreting results.
DISCUSSION
To our knowledge, this is the first systematic review to examine race/ethnicity in GERD with an effort to identify and prevent disparities in research. The findings demonstrate several trends. First, of the 62 considered, only 25 (40%) were eligible because they provided complete descriptions of their study populations. Thus, the majority of studies failed to follow NIH and ICMJE guidelines regarding the collection and reporting of race/ethnicity. Among those that did describe the race/ethnicity of participants, the wide range of descriptors makes comparisons and conclusions across studies difficult. Further, many of the studies used a category of ‘Other,’ limiting full knowledge of patient characteristics and a multiracial category was not mentioned in any study. On the other hand, the majority of studies reviewed in the final analysis did justify the use of race/ethnicity as a study variable and discussed relevant factors associated with race/ethnicity that could be used to help explain differences. Morgan et al.’s21 2010 clinical trial provides a good example of a study that addressed race/ethnicity methodologically. The authors justified the use of race/ethnicity as a study variable, utilized the NIH standard of self-identification of race/ethnicity, employed the US Census Bureau's definition for ethnicity, and considered the role of the conceptually relevant factor of diet. Second, the majority of studies that reported race/ethnicity took place in the USA, with none from Latin America, Africa, or Australia. Thus, there appears to be a disparity with respect to the countries reporting race/ethnicity; however, all international studies may not be published in the searched databases. Third, among the studies that reported the race/ethnicity of all participants, the populations often consisted overwhelmingly of the majority population of White in North America or Chinese in Asian studies. It is unclear if these majority-focused samples reflect a health care disparity, a difference in quality of care (who is included in research), or is a reflection of access to care and patient preference to not participate in research. Fourth, the majority of the studies met moderate quality on our quality appraisal scale that was focused on the overall methodological quality of papers including racial components.
The trends observed in this systematic review have been demonstrated in other studies. Kanakamedala and Haga's analysis of articles in high impact biomedical journals across three countries also found that the majority of articles did not report the race/ethnicity of participants and that the most represented racial group was White.8 Additionally, an international systematic review focused on racial/ethnic disparities also observed variability in the terms used to describe racial/ethnic groups.15
Limitations
While there are several meaningful findings, limitations of this systematic review should be noted. First, per Kaplan and Bennett,19 it is important to acknowledge the limitations of the data of the included studies. The studies utilized a range of methods to collect and categorize race/ethnicity and described the populations as though race/ethnicity were fixed and mutually exclusive. Additionally, it appeared that several studies were unable to compare racial/ethnic groups because the sample sizes of minority groups were too small. Second, only studies published in English were reviewed, which limits the studies included and may bias results. Third, publication bias may have limited the availability of studies as many with negative results are not published. Fourth, the authors’ knowledge of race/ethnicity outside the U.S. is limited but we used international recommendations and the papers’ terms to guide our work. Despite the limitations, this study is important as it helps to begin a conversation and fill in a gap in the research through systematically evaluating the international characterization of race/ethnicity in GERD.
Recommendations
GERD researchers should ensure that diverse participants are included and accurately described. This could help prevent health care disparities and ensure that evidence-based care can be translated to all patients. The following recommendations have the potential to inform future scientific endeavors as exemplified by the Kim, Tingen, and Woodruff's work on adoption of sex as a biological variable22 (Table 1).
Acknowledgments
Meredith Craven is supported by a National Institute of Diabetes and Digestive and Kidney Diseases Institutional Training Grant (T32DK101363). Dr Taft is a consultant and/or on the speakers bureau for Janssen and Abbvie. Dr Keefer is a consultant and/or on the speakers bureau for Janssen, Allergan, Pfizer, Abbvie, and MetaME Health. The authors are unaware of any competing interests.
Appendix 1
PubMed MEDLINE
(“Ethnic Groups”[Mesh] OR ‘Continental Population Groups’[mesh] OR ethnic*[tiab] OR racial[tiab] OR race[tiab] OR races[tiab] OR minorit*[tiab] OR black[tiab] OR blacks[tiab] OR hispanic[tiab] OR Hispanics[tiab] OR latin[tiab] OR Latino[tiab] OR Latina[tiab] OR asian[tiab] OR Asians[tiab] OR ‘African American’[tiab] OR ‘African Americans’[tiab] OR Africa[tiab] OR African[tiab] OR Indian[tiab] OR Indians[tiab] OR ‘Native American’[tiab] OR ‘Native Americans’[tiab] OR Jew[tiab] OR Jews[tiab] OR Jewish[tiab] OR Amish[tiab] OR Inuit[tiab] OR Inuits[tiab] OR Arab[tiab] OR Arabs[tiab] OR Arabic[tiab] OR Roma[tiab] OR Romany[tiab])
AND (“Gastroesophageal Reflux”[Mesh] OR ‘Acid Reflux’[tiab] OR ‘Gastro-Esophageal Reflux’[tiab] OR ‘Gastro Esophageal Reflux’[tiab] OR ‘Gastroesophageal Reflux’[tiab] OR GERD[tiab] OR ‘Esophageal Reflux’[tiab] OR ‘Gastro-oesophageal Reflux’[tiab] OR ‘Gastro oesophageal Reflux’[tiab] OR “acid reflux"[tiab] OR GORD[tiab] OR “heartburn"[MeSH Terms] OR “heartburn"[tiab] OR Pyrosis[tiab])
EMBASE
‘ethnic group'/exp OR 'ancestry group'/exp OR ‘Ethnic Group’: ti, ab OR ‘Continental Population Group’: ti, ab OR ethnic*: ti, ab OR racial: ti, ab OR race: ti, ab OR races: ti, ab OR minorit*: ti, ab OR black: ti, ab OR blacks: ti, ab OR hispanic: ti, ab OR Hispanics: ti, ab OR latin: ti, ab OR Latino: ti, ab OR Latina: ti, ab OR asian: ti, ab OR Asians: ti, ab OR ‘African American’: ti, ab OR ‘African Americans’: ti, ab OR Africa: ti, ab OR African: ti, ab OR Indian: ti, ab OR Indians: ti, ab OR ‘Native American’: ti, ab OR ‘Native Americans’: ti, ab OR Jew: ti, ab OR Jews: ti, ab OR Jewish: ti, ab OR Amish: ti, ab OR Inuit: ti, ab OR Inuits: ti, ab OR Arab: ti, ab OR Arabs: ti, ab OR Arabic: ti, ab OR Roma: ti, ab OR Romany: ti, ab
AND
‘gastroesophageal reflux'/exp OR 'heartburn'/exp OR ‘cardioesophageal reflux’: ti, ab OR ‘cardiooesophageal reflux’: ti, ab OR ‘esophageal reflux’: ti, ab OR ‘esophageal regurgitation’: ti, ab OR ‘esophagogastric reflux’: ti, ab OR ‘esophagus reflux’: ti, ab OR ‘gastric regurgitation’: ti, ab OR ‘gastro esophageal reflux’: ti, ab OR ‘gastro oesophageal reflux’: ti, ab OR ‘gastroesophageal reflex’: ti, ab OR ‘gastroesophageal reflux disease’: ti, ab OR ‘gastroesophageal regurgitation’: ti, ab OR ‘gastroesophagus reflux’: ti, ab OR ‘gastrooesophageal reflex’: ti, ab OR ‘gastrooesophageal reflux’: ti, ab OR ‘gastrooesophageal regurgitation’: ti, ab OR GERD: ti, ab OR GORD: ti, ab OR ‘oesophageal reflux’: ti, ab OR ‘oesophageal regurgitation’: ti, ab OR ‘oesophagogastric reflux’: ti, ab OR ‘oesophagus reflux’: ti, ab OR ‘Acid Reflux’: ti, ab OR ‘Gastro-Esophageal Reflux’: ti, ab OR ‘Gastro Esophageal Reflux’: ti, ab OR ‘Gastro-oesophageal Reflux’: ti, ab OR ‘Gastro oesophageal Reflux’: ti, ab OR ‘heartburn’: ti, ab OR Pyrosis: ti, ab
Limited to Articles, Articles in Press, Reviews (removed conference abstracts, editorials, letters, errata, surveys)
Cochrane CENTRAL Register of Controlled Trials
MeSH descriptor: [Ethnic Groups] explode all trees
MeSH descriptor: [Continental Population Groups] explode all trees
ethnic*: ab, ti, kw OR racial: ab, ti, kw OR race: ab, ti, kw OR races: ab, ti, kw OR minorit*: ab, ti, kw OR black: ab, ti, kw OR blacks: ab, ti, kw OR hispanic: ab, ti, kw OR Hispanics: ab, ti, kw OR latin: ab, ti, kw OR Latino: ab, ti, kw OR Latina: ab, ti, kw OR asian: ab, ti, kw OR Asians: ab, ti, kw OR ‘African American’: ab, ti, kw OR ‘African Americans’: ab, ti, kw OR Africa: ab, ti, kw OR African: ab, ti, kw OR Indian: ab, ti, kw OR Indians: ab, ti, kw OR ‘Native American’: ab, ti, kw OR ‘Native Americans’: ab, ti, kw OR Jew: ab, ti, kw OR Jews: ab, ti, kw OR Jewish: ab, ti, kw OR Amish: ab, ti, kw OR Inuit: ab, ti, kw OR Inuits: ab, ti, kw OR Arab: ab, ti, kw OR Arabs: ab, ti, kw OR Arabic: ab, ti, kw OR Roma: ab, ti, kw OR Romany: ab, ti, kw AND MeSH descriptor: [Gastroesophageal Reflux] explode all trees MeSH descriptor: [Heartburn] explode all trees
‘Acid Reflux’: ab, ti, kw OR ‘Gastro-Esophageal Reflux’: ab, ti, kw OR ‘Gastro Esophageal Reflux’: ab, ti, kw OR ‘Gastroesophageal Reflux’: ab, ti, kw OR GERD: ab, ti, kw OR ‘Esophageal Reflux’: ab, ti, kw OR ‘Gastro-oesophageal Reflux’: ab, ti, kw OR ‘Gastro oesophageal Reflux’: ab, ti, kw OR “acid reflux": ab, ti, kw OR GORD: ab, ti, kw OR “heartburn”: ab, ti, kw OR Pyrosis: ab, ti, kw
Appendix 2
From: Moher D, Liberati A, Tetzlaff J, Altman D G, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi:10.1371/journal.pmed1000097.
Appendix 3
| Design (max. 2 points) |
| Cross-sectional (1 point) |
| Cohort/Randomized Controlled Trial (2 points) |
| Recruitment (max. 3 points) |
| Convenience (0 points) |
| Consecutive (1 point) |
| Random (2 points) |
| Population-based or complete cover of patients in a large hospital(s) (3 points) |
| Selection of controls (max. 2 points) |
| Healthy controls (1 point) |
| Chronically ill controls/non-GERD controls (1 point) |
| Both (2 points) |
| GERD diagnosis (max. 2 point) |
| ICD or PPI use (0 points)* |
| Validated disease index questionnaire (1 points) |
| Gastroenterologist or chart confirmed (MD dx) with investigation support—endoscopically, ph probe, etc (2 point) |
| Measure of GERD activity (max. 2 points) |
| Nonvalidated disease index/non-specific disease measure (0 points) |
| Validated clinical index/questionnaire (1 point) |
| Endoscopy (2 points) |
| Sample size (max. 1 points) |
| Power calculation, justification of sample size or representative population based sample (1 point) |
| Definition of Race/Ethnicity (max. 2 points) |
| No racial breakdown (0 point) |
| Racial breakdown (1 point) |
| Race definition explained (i.e. self-report on a proper validated measure) (2 point) |
Notes
Specific author contributions: Search strategy development: Meredith R. Craven, Linda C. O’Dwyer, Tiffany H. Taft, Laurie Keefer; Data collection: Meredith R. Craven, Laurie Keefer, Emily Stern, Linda C. O’Dwyer; Interpretation of data: Meredith R. Craven, Laurie Keefer, Emily Stern; Drafting of manuscript: Meredith R. Craven, Linda C. O’Dwyer; Final approval of manuscript: Meredith R. Craven, Laurie Keefer, Emily Stern, Linda C. O’Dwyer, Tiffany H. Taft; : Critical revision for intellectual content: Laurie Keefer, Emily Stern, Tiffany H. Taft.L
References
- 1. Smedley B D, Stith A Y, Nelson A R. Unequal treatment: confronting racial and ethnic disparities in health care. In: Smedley B D, Stith A Y, Nelson A R (eds). Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington DC: 2002 by the National Academy of Sciences, 2003. [Google Scholar]
- 2. World Health Organization Health and freedom from discrimination. Human Rights Publication Series 2. 2001. [Google Scholar]
- 3. Centers for Disease Control and Prevention Atlanta, Ga CDC health disparities and inequalities report: United States 2013. In MMWR 2013; 62(Suppl 3): 2013. [Google Scholar]
- 4. Helms J E, Jernigan M, Mascher J. The meaning of race in psychology and how to change it: a methodological perspective. Am Psychol 2005; 60: 27. [DOI] [PubMed] [Google Scholar]
- 5. Health NIo NIH Policy on Reporting Race and Ethnicity Data: Subjects in Clinical Research (NOT-OD-01-053). http://grants.nih.gov.turing.library.northwestern.edu/grants/guide/notice-files/not-od-01-053.html [Accessed August 14, 2017] 2001.
- 6. ICMJE Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals. http://www.icmje.org/icmje-recommendations.pdf [Accessed August 14, 2017] 2016. [PubMed]
- 7. Geller S E, Koch A, Pellettieri B, Carnes M. Inclusion, analysis, and reporting of sex and race/ethnicity in clinical trials: have we made progress? J Womens Health 2011; 20: 315–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kanakamedala P, Haga S B. Characterization of clinical study populations by race and ethnicity in biomedical literature. Ethn Dis 2012; 22: 96–101. [PMC free article] [PubMed] [Google Scholar]
- 9. Corbie-Smith G, St George D M, Moody-Ayers S, Ransohoff D F. Adequacy of reporting race/ethnicity in clinical trials in areas of health disparities. J Clin Epidemiol 2003; 56: 416–20. [DOI] [PubMed] [Google Scholar]
- 10. Camilleri M, Dubois D, Coulie B et al. Prevalence and socioeconomic impact of upper gastrointestinal disorders in the United States: results of the US Upper Gastrointestinal Study. Clin Gastroenterol Hepatol 2005; 3: 543–52. [DOI] [PubMed] [Google Scholar]
- 11. Eusebi L H, Ratnakumaran R, Yuan Y et al. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut 2017, doi: 10.1136/gutjnl-2016-313589. [DOI] [PubMed] [Google Scholar]
- 12. Vakil N, van Zanten S V, Kahrilas P, Dent J, Jones R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 2006; 101: 1900–20; quiz 1943. [DOI] [PubMed] [Google Scholar]
- 13. Lacy B E, Weiser K, Chertoff J et al. The diagnosis of gastroesophageal reflux disease. Am J Med 2010; 123 (7): 583–92. [DOI] [PubMed] [Google Scholar]
- 14. Kahrilas P J. GERD pathogenesis, pathophysiology, and clinical manifestations. Cleve Clin J Med 2003; 70(Suppl 5): S4–19. [DOI] [PubMed] [Google Scholar]
- 15. Des Jarlais D C, Bramson H A, Wong C, et al. Racial/ethnic disparities in HIV infection among people who inject drugs: an international systematic review and meta-analysis. Addiction 2012; 107: 2087–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. May F P, Almario C V, Ponce N, Spiegel B M. Racial minorities are more likely than whites to report lack of provider recommendation for colon cancer screening. Am J Gastroenterol 2015; 110: 1388–94. [DOI] [PubMed] [Google Scholar]
- 17. Pai M, McCulloch M, Gorman J D, et al. Systematic reviews and meta-analyses: an illustrated, step-by-step guide. Natl Med J India 2004; 17: 86–95. [PubMed] [Google Scholar]
- 18. Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc 2002; 94: 666–8. [PMC free article] [PubMed] [Google Scholar]
- 19. Kaplan J B, Bennett T. Use of race and ethnicity in biomedical publication. JAMA 2003; 289: 2709–16. [DOI] [PubMed] [Google Scholar]
- 20. Sanderson S, Tatt I D, Higgins J. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol 2007; 36: 666–76. [DOI] [PubMed] [Google Scholar]
- 21. Morgan D, Pandolfino J, Katz P O, Goldstein J L, Barker P N, Illueca M. Clinical trial: gastric acid suppression in Hispanic adults with symptomatic gastro-oesophageal reflux disease—comparator study of esomeprazole, lansoprazole, and pantoprazole. Aliment Pharmacol Ther 2010; 32: 200–8. [DOI] [PubMed] [Google Scholar]
- 22. Kim A M, Tingen C M, Woodruff T K. Sex bias in trials and treatment must end. Nature 2010; 465: 688. [DOI] [PubMed] [Google Scholar]
- 23. Coyne K S, Wiklund I, Schmier J, Halling K, Degl' Innocenti A, Revicki D. Development and validation of a disease-specific treatment satisfaction questionnaire for gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2003; 18: 907–15. [DOI] [PubMed] [Google Scholar]
- 24. Ho K Y, Gwee K A, Khor J L, Selamat D S, Yeoh K G. Validation of a graded response questionnaire for the diagnosis of gastroesophageal reflux disease in an Asian primary care population. J Clin Gastroenterol 2008; 42: 680–6. [DOI] [PubMed] [Google Scholar]
- 25. Spiegel B M, Roberts L, Mody R et al. The development and validation of a nocturnal gastro-oesophageal reflux disease symptom severity and impact questionnaire for adults. Aliment Pharmacol Ther 2010; 32: 591–602. [DOI] [PubMed] [Google Scholar]
- 26. Balasubramanian G, Singh M, Gupta N et al. Prevalence and predictors of columnar lined esophagus in gastroesophageal reflux disease (GERD) patients undergoing upper endoscopy. Am J Gastroenterol 2012; 107: 1655–61. [DOI] [PubMed] [Google Scholar]
- 27. Bhatia S J, Reddy D N, Ghoshal U C et al. Epidemiology and symptom profile of gastroesophageal reflux in the Indian population: report of the Indian Society of Gastroenterology Task Force. Indian J Gastroenterol 2011; 30: 118–27. [DOI] [PubMed] [Google Scholar]
- 28. El-Serag H B, Petersen N J, Carter J et al. Gastroesophageal reflux among different racial groups in the United States. Gastroenterology 2004; 126: 1692–9. [DOI] [PubMed] [Google Scholar]
- 29. Friedenberg F K, Makipour K, Palit A, Shah S, Vanar V, Richter J E. Population-based assessment of heartburn in urban Black Americans. Dis Esophagus 2013; 26: 561–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gerson L B, Ullah N, Fass R, Green C, Shetler K, Singh G. Does body mass index differ between patients with Barrett's oesophagus and patients with chronic gastro-oesophageal reflux disease? Aliment Pharmacol Ther 2007; 25: 1079–86. [DOI] [PubMed] [Google Scholar]
- 31. Islami F, Nasseri-Moghaddam S, Pourshams A et al. Determinants of gastroesophageal reflux disease, including hookah smoking and opium use- a cross-sectional analysis of 50,000 individuals. PLoS One 2014; 9: e89256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lim S L, Goh W T, Lee J M, Ng T P, Ho K Y. Changing prevalence of gastroesophageal reflux with changing time: longitudinal study in an Asian population. J Gastroenterol Hepatol 2005; 20: 995–1001. [DOI] [PubMed] [Google Scholar]
- 33. Niu C Y, Zhou Y L, Yan R et al. Incidence of gastroesophageal reflux disease in Uygur and Han Chinese adults in Urumqi. World J Gastroenterol 2012; 18: 7333–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nouraie M, Radmard A R, Zaer-Rezaii H, Razjouyan H, Nasseri-Moghaddam S, Malekzadeh R. Hygiene could affect GERD prevalence independently: a population-based study in Tehran. Am J Gastroenterol 2007; 102: 1353–60. [DOI] [PubMed] [Google Scholar]
- 35. Sperber A D, Halpern Z, Shvartzman P, et al. Prevalence of GERD symptoms in a representative Israeli adult population. J Clin Gastroenterol 2007; 41: 457–61. [DOI] [PubMed] [Google Scholar]
- 36. Srinivasan R, Tutuian R, Schoenfeld P et al. Profile of GERD in the adult population of a northeast urban community. J Clin Gastroenterol 2004; 38: 651–7. [DOI] [PubMed] [Google Scholar]
- 37. Wong W, Lai K, Lam K et al. Prevalence, clinical spectrum and health care utilization of gastro-oesophageal reflux disease in a Chinese population: a population-based study. Aliment Pharmacol Ther 2003; 18: 595–604. [DOI] [PubMed] [Google Scholar]
- 38. Yang S Y, Lee O Y, Bak Y T et al. Prevalence of gastroesophageal reflux disease symptoms and uninvestigated dyspepsia in Korea: a population-based study. Dig Dis Sci 2008; 53: 188–93. [DOI] [PubMed] [Google Scholar]
- 39. Yuen E, Romney M, Toner R W et al. Prevalence, knowledge and care patterns for gastro-oesophageal reflux disease in United States minority populations. Aliment Pharmacol Ther 2010; 32: 645–54. [DOI] [PubMed] [Google Scholar]
- 40. Damiano A, Siddique R, Xu X, Johanson J, Sloan S. Reductions in symptom distress reported by patients with moderately severe, nonerosive gastroesophageal reflux disease treated with rabeprazole. Dig Dis Sci 2003; 48: 657–62. [DOI] [PubMed] [Google Scholar]
- 41. Degl' Innocenti A, Guyatt G H, Wiklund I et al. The influence of demographic factors and health-related quality of life on treatment satisfaction in patients with gastroesophageal reflux disease treated with esomeprazole. Health Qual Life Outcomes 2005; 3: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Fass R, Sontag S J, Traxler B, Sostek M. Treatment of patients with persistent heartburn symptoms: a double-blind, randomized trial. Clin Gastroenterol Hepatol2006; 4: 50–6. [DOI] [PubMed] [Google Scholar]
- 43. Fock K M, Teo E K, Ang T L, Chua T S, Ng T M, Tan Y L. Rabeprazole vs esomeprazole in non-erosive gastro-esophageal reflux disease: a randomized, double-blind study in urban Asia. World J Gastroenterol 2005; 11: 3091–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Karim S, Jafri W, Faryal A et al. Regular post dinner walk; can be a useful lifestyle modification for gastroesophageal reflux. J Pak Med Assoc 2011; 61: 526–30. [PubMed] [Google Scholar]
- 45. Gaddam S, Maddur H, Wani S et al. Risk factors for nocturnal reflux in a large GERD cohort. J Clin Gastroenterol 2011; 45: 764–8. [DOI] [PubMed] [Google Scholar]
- 46. Masoumi S J, Khademolhosseini F, Mehrabani D et al. Correlation of quality of life with gastroesophageal reflux disease amongst Qashqai nomads in Iran. Arch Iran Med 2012; 15: 747–50. [PubMed] [Google Scholar]