Abstract
Objective
As technology continues to improve, it plays an increasingly vital role in the practice of medicine. This study aimed to assess the feasibility of the implementation of virtual reality (VR) in a rheumatology clinic as a platform to administer guided meditation and biofeedback as a means of reducing chronic pain.
Methods
Twenty participants were recruited from a rheumatology clinic. These participants included adults with physician‐diagnosed autoimmune disorders who were on a stable regimen of medication and had a score of at least 5 on the pain Visual Analog Scale (VAS) for a minimum of 4 days during the prior 30 days. VAS, part of most composite outcome measurements in rheumatology, is an instrument used to assess pain that consists of a straight line with the endpoints ranging from “no pain at all” and “pain as bad as it could be.” Patients were randomized into two groups that differed in the order in which they experienced the two VR modules. One module consisted of a guided meditation (GM) environment, whereas the other module consisted of a respiratory biofeedback (BFD) environment. Data on pain and anxiety levels were gathered before, during, and after the two modules.
Results
The three most common diagnoses among participants were rheumatoid arthiritis (RA), lupus, and fibromyalgia. There was a significant reduction in VAS scores after BFD and GM (P values = 0.01 and 0.04, respectively). There was a significant reduction in Facial Anxiety Scale after the GM compared with the BFD (P values = 0.02 and 0.08, respectively).
Conclusion
This novel study demonstrated that VR could be a feasible solution for the management of pain and anxiety in rheumatology patients. Further trials with varying treatment exposures and durations are required to solidify the viability of VR as a treatment option in rheumatology clinics.
Introduction
Patients with chronic autoimmune conditions such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), spondyloarthropathy, and vasculitis often suffer from chronic and debilitating pain. RA is a systemic inflammatory disease of unknown etiology. It is characterized by chronic, symmetric polyarthritis and erosive synovitis 1. SLE is a multi‐organ systemic autoimmune disease that is characterized by chronic inflammation with clinical and serological heterogeneity 2.
Physical and psychological stress have been postulated to be a possible component involved in the development of autoimmune diseases 3, and multiple studies have demonstrated that stress worsens disease activity in patients with RA, SLE, spondyloarthropathy, and vasculitis 4, 5, 6, 7, 8. Often patients suffering from chronic pain due to these conditions are prescribed highly addictive opioids for pain management. Because of the nature of opioids, patients are continually prescribed higher doses of medication due to a buildup of tolerance, which can eventually lead to addiction and in certain cases death 9. In February 2018, The International Association for the Study of Pain (IASP) recognized that longer‐term use, tolerance, dependence, and other neuroadaptations of opioids compromise both efficacy and safety 10.
An analysis of national Medicare data from 2014 revealed that 41% of older patients with RA were regular users of opioids 11. Chronic pain co‐occurring with addiction has been linked to anxiety, depression, financial problems, functional disability, cognitive disturbances, sleep disturbances, family, and social problems 12. The current opioid crisis in the United States 13 has highlighted the importance of alternative strategies for pain management 14.
An alternative option for pain management may lie within the field of virtual reality (VR). VR has emerged as a promising and evidence‐based treatment modality for musculoskeletal pain 15. A clinical trial comparing VR with the effects of opioids used functional magnetic resonance imaging (fMRI) to assess brain activities related to thermal pain stimulation revealed that opioids and VR both significantly reduced pain‐related brain activity in the insula and thalamus 16. By stimulating the visual cortex while engaging other senses, VR modulates the user's processing of nociceptive stimuli 17. A review of VR literature found that VR interventions appeared to alter how the brain processes pain and produces analgesia 18.
Meditation is a practice where an individual uses different techniques, including mindfulness, to cultivate a mentally clear and emotionally stable sense of being. The term “meditation” is now commonly used to refer to several different techniques including contemplation, concentration, use of nature sounds such as the ocean, guided meditation, meditative movement exercises such as yoga and tai chi, qigong, breathing exercises, and mantra 19. These techniques work to influence the senses, mind, intellect, and emotions 19. Systematic reviews have found that mindfulness meditation has an effect on psychological aspects on living with chronic pain and is associated with improving depression and quality of life 20. Recently there have been developments in VR technology, creating new platforms for the distribution and implementation of meditation modules. There is reasonable evidence suggesting that VR is a viable way to practice mindfulness meditation 21.
Biofeedback interventions have been shown to diminish stress‐related symptoms in patients with RA 22. Biofeedback is a process that enables patients to control otherwise autonomic processes by providing visual and/or auditory cues whenever a physiological target has been met 22. Biofeedback is a self‐regulation technique through which patients learn how to control nonconscious body processes, such as heart rate and respiration rate. This technique requires specialized equipment to convert physiological signals into meaningful visual and auditory cues. Biofeedback allows patients to acknowledge the processes inside their bodies and use the feedback to adjust their physiology in a desired direction 23. For example, if one were using a temperature biofeedback device, a patient would place his or her hand onto a device and attempt to control breathing and heart rate to increase the skin temperature. When the skin temperature increases (thus representing an increase in parasympathetic activation), they may hear a high‐pitched tone. Technology involving the use of visual biofeedback has been shown to improve quality of life, pain level, and physical function in patients with RA and SLE 24, 25.
VR represents an important advance in biofeedback technologies by providing immersive and realistic multisensory experiences that can help alleviate symptomology by allowing patients to learn stress reduction and pain management skills 26. Previously, VR has been studied in a range of disease states, including obesity 27, 28, 29, anxiety disorders 30, 31, 32, acute pain management 26, 33, 34, 35, 36, oncology 37, and neurorehabilitation 38, 39. Concurrent improvements in software and hardware design, as well as associated cost reductions, have made VR promising for more widespread accessibility in health care 40. These recent advances in VR technology thus offer a compelling opportunity to both address biopsychosocial distress and reduce chronic pain 17. For instance, Cedars‐Sinai medical center in Los Angeles, California, has conducted VR studies in which they assessed the eligibility, usability, and acceptability of VR for pain symptoms in a diverse cohort of patients among an urban community medical center 41.
In this study, we recruited 20 patients with active, physician‐diagnosed rheumatic diseases such as RA, SLE, ankylosing spondylitis, psoriatic arthritis, myositis, and vasculitis. Secondary fibromyalgia was prevalent in a small group of patients. Patients with active pain symptoms indicated by the study investigators were offered the opportunity to undergo biofeedback training using a portable VR unit in the clinic. The primary aim of this study was to evaluate the feasibility of a VR‐based biofeedback intervention for outpatients within a rheumatology clinic. Secondly, we aimed to explore whether VR‐based biofeedback and guided meditation could help decrease chronic pain and anxiety in a short period of time. Finally, we aimed to qualitatively observe the experience of a VR intervention from the perspective of the patients.
Methods
Participants
Participants (n = 20) were recruited from Attune Health, a private practice rheumatology clinic in Los Angeles, California. Inclusion criteria included adult patients with physician‐diagnosed chronic autoimmune disorders who were on a stable medication regimen. Additionally, all participants had a score of at least 5 on the Visual Analog Scale (VAS) for a minimum of 4 days within the prior 30 days 42. The VAS is an instrument used to assess pain that consists of a straight line with the endpoints ranging from “no pain at all” and “pain as bad as it could be” 43. Physicians approached adult patients to ask if they would be interested in taking part in a study in which they could experience and provide feedback on VR. We excluded patients (n = 3) with symptoms of active nausea or vomiting, history of current chronic vertigo or dizziness that might have made them susceptible to motion sickness, and those who were unable to use the VR headset for any reason. Patients with epilepsy were excluded because of an estimated 0.025% risk of inducing seizures 26.
VR hardware and software
We used Samsung Gear VR goggles with a Samsung Galaxy S7 mobile phone to deliver a 3D environment. The sound was transmitted through Nubwo N2 headphones, which were also equipped with a microphone used for breath tracking. The equipment was provided for study use by AppliedVR.
We selected two VR environments for participants based on AppliedVR's EaseVR chronic pain platform. One module consisted of a guided meditation (GM) environment, whereas the other module consisted of a respiratory biofeedback (BFD) environment. Both modules contained immersive experiences with 360° views of similar nature environments. The BFD contained a virtual guide who instructed participants to breathe along with an oscillating pacer at six breaths per minute. Exhales were visualized by outward‐moving blue particles, which increased in size as the participant's respiratory rate more closely synchronized with the rate of the pacer. Guided audio prompts acknowledged effort while including reminders for slow and controlled breathing periodically. These audio prompts adjusted when participants had increased or decreased respiratory rates. Figure 1 shows an example of the environment.
Figure 1.

Two‐dimensional still from the biofeedback environment. In this scene, purple rings move radially inward and outward to represent inhalation and exhalation, respectively.
The GM placed participants in the same natural enlivened environment. Participants were led in a meditation by a virtual guide who asked them to shift their focus onto different parts of the body while maintaining awareness of breath control without any audio or visual feedback. Breathing data were collected but neither interacted with nor affected the experience. Similarly, neither a pacer nor breathing particles were presented. The frequency of guided instruction and the duration of the session was fixed, regardless of data.
The two VR modules, GM and BFD, occurred right after one another. Participants were randomly assigned to either receive GM first followed by BFD or BFD first followed by GM. Both modules lasted around 10‐15 minutes each, which totaled around 30 minutes of VR. Figure 2 demonstrates how participants were randomized using a random number generator in a 1:1 ratio to either the BFD first or the GM first groups. Both groups received only one 30‐minute VR session that consisted of the BFD and GM modules that were administered back to back.
Figure 2.
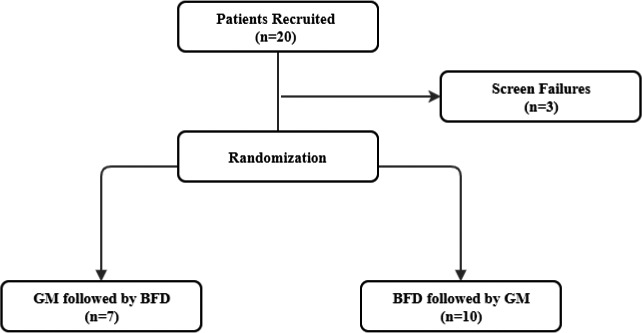
Patient randomization schema. Abbreviation: GM, guided meditation; BFD, biofeedback.
Pre‐VR assessments
Prior to beginning the VR session, participants filled out three questionnaires from the Patient‐Reported Outcomes Measurement Information System (PROMIS): Emotional Distress/Anxiety (Short Form 8a v.1.0), Emotional Distress/Anger (Short Form 5a v.1.1), and the Global Health Scale (v.1.2). PROMIS surveys were administered prior to patients’ receiving VR therapy, allowing for the quantification of both their global health and emotional distress. Within these questionnaires, patients were tasked with responding to the questions and statements posed with a number from 1 to 5, with higher numbers generally corresponding to better health. The global health survey inquired about patients’ overall health, quality of life, and mental health. With regard to emotional distress, patients were asked to specify their anger and anxiety levels using a scale identical to the one utilized in the global health questionnaire. Participants then individually completed semistructured face‐to‐face interviews with a trained research assistant regarding prior conceptions of VR, disease history, pain history, and past treatments. It has been found that patients with musculoskeletal disease are able to accurately recall and rate the severity of pain for a period of three months 44. During this interview, a VAS from 0 to 10 was administered to assess pain, followed by the five‐level Facial Anxiety Scale (FAS) to assess anxiety.
Post‐VR assessments
Questions about general impressions were asked between the two VR sessions. Participants were also asked to recall what their pain and anxiety levels were during the session using the VAS and FAS before continuing on to the second VR environment. After the second VR environment, participants were once again asked to record current pain and anxiety levels using the VAS and FAS as well as to recall pain and anxiety levels during the second VR experience. After the final session, we continued an extensive semistructured interview to evaluate patient opinions on the equipment used, comparisons between sessions, and perceived benefits and harms. We also asked for patient feedback on potential avenues of improvement for the VR experiences. Medical charts were reviewed for age, sex, ethnicity, race, diagnoses, disease activity status, and treatment history.
Analysis
Qualitative analysis
We carefully analyzed transcripts of the qualitative patient interviews conducted before, after, and during their respective VR experiences. This analysis was observational and was conducted by an independent coder reading through each transcript. Any common sentiments were recorded, and we kept particular track of prior attempted interventions for pain management, including both pharmacological and behavioral techniques. We also paid particular attention to the reported effect of pain on mood, comments on the comfort level of the device, and which intervention each participant preferred more.
Quantitative analysis
Analyses were conducted in R software and Microsoft Excel. All relevant assumptions, including sphericity, were examined and corrected prior to further analyses. Data were then analyzed using 2‐way, 1‐way repeated measure ANOVAs with three levels (baseline, after GM, and after BFD) to examine FAS and VAS scores, respectively. Any significant findings were then examined using post hoc pairwise t tests. We also completed pairwise t tests to determine if there was a difference in reduction in pain or anxiety based on which intervention, GM or BFD, was administered first.
Results
Demographics
The average age of participants was 52.65 (Standard Deviation [SD] = 16.1) years old. The study population was predominantly Caucasian female, with 88.24% (n = 15) of the participants identifying as female and 76.47% (n = 14) of the participants identifying as Caucasian. The most common diagnosis among participants was RA at 64.71% (n = 11), followed by SLE and fibromyalgia at 23.53% (n = 4) and 17.65% (n = 3), respectively. Average PROMIS scores for physical health and mental health were 10.94 (SD = 2.61, T‐Score [T] = 37.4, Standard Error [SE] = 4.10) and 12.41 (SD = 3.30, T = 43.50, SE = 3.60), respectively. Average PROMIS scores for anger were 12 (SD = 3.34, T = 52.7, SE = 3.20) and average PROMIS scores for anxiety were 18.29 (SD = 4.86, T = 75.4, SE = 2.70). These PROMIS scores indicate that our patient sample had higher anxiety scores than the normal population. See Table 1 for demographic information.
Table 1.
Demographics
| GM Followed by BFD | BFD Followed by GM | |||
|---|---|---|---|---|
| (n = 7) | (n = 10) | |||
| Mean | SD | Mean | SD | |
| Age | 53.71 | 15.94 | 51.9 | 17.87 |
| n | (%) | n | (%) | |
| Sex | ||||
| Female | 6 | 85.71% | 9 | 90.00% |
| Male | 1 | 14.26% | 1 | 10.00% |
| Race | ||||
| White | 6 | 85.71% | 8 | 80.00% |
| Black | 0 | 0.00% | 2 | 20.00% |
| Asian | 1 | 14.29% | 0 | 0.00% |
| Ethnicity | ||||
| Non‐Hispanic | 6 | 85.71% | 9 | 90.00% |
| Hispanic | 1 | 14.29% | 1 | 10.00% |
| Medication a | ||||
| Anticonvulsant drug | 2 | 16.67% | 0 | 0.00% |
| Biologic | 1 | 8.33% | 1 | 6.67% |
| DMARD | 3 | 25.00% | 6 | 46.67% |
| Marijuana | 1 | 8.33% | 1 | 6.67% |
| Opioid | 2 | 16.67% | 2 | 13.33% |
| Over the counter | 1 | 8.33% | 1 | 6.67% |
| Steroid | 1 | 8.33% | 2 | 13.33% |
| NSAID | 1 | 8.33% | 1 | 6.67% |
| Other | 0 | 0.00% | 1 | 6.67% |
Abbreviation: BFD, biofeedback; DMARD, disease‐modifying antirheumatic drug; GM, guided meditation; NSAID, nonsteroidal anti‐inflammatory drug.
There is a greater number of medications than the number of participants as some individuals were on multiple medications.
Qualitative analysis: acceptance and utility of VR intervention
The actual VR device seemed to be well tolerated by participants, as 100% of participants in the study reported that they would participate in a similar study again. All participants also reported that they use, or have used, oral medications for pain management but are currently seeking other options for various reasons, including chemical dependence, unpalatable side effects, or failure to increase long‐term pain symptoms. VR was not necessarily a new concept for most participants, as 88.24% (n = 15) reported that they had heard of VR prior to engaging in the study. The majority of participants reported positive responses to at least one of the VR interventions, with 64.71% (n = 11) spontaneously mentioning, without being prompted, increased relaxation and/or calmness during their respective interviews. These positive responses were often dramatic, with one participant saying in regard to BFD that, “I was able to relax my body. I was able to lower the pain levels by breathing, almost like wiping it away.” Another participant, in reference to GM, reported, “When [the guide] was talking about my back… I released my breath [and] it's like everything just melted [away].”
Qualitative analysis: barriers to VR use
Most participants reported that they visually enjoyed the experience, as reported in Table 2. Within the BFD Followed by GM Group, 60.00% of individuals reported enjoying the visuals, while 42.86% of the GM followed by BFD reported enjoying the experience. Finally, only one participant reported the device to be uncomfortable, whereas 44% mentioned that the device felt heavy and/or bulky toward the end of the session. As participants wore the device for two consecutive VR sessions, this finding may not be relevant, as most people may complete one individual session at a time.
Table 2.
VR experience and acceptability
| Acceptability of VR | ||||
|---|---|---|---|---|
| GM Followed by BFD | BFD Followed by GM | |||
| (n = 7) | (n = 10) | |||
| n | (%) | n | (%) | |
| Familiar with VR prior to study | ||||
| Yes | 6 | 85.71% | 1 | 10.00% |
| No | 1 | 14.29% | 9 | 90.00% |
| Comfort of headset | ||||
| Comfortable | 2 | 28.57% | 4 | 40.00% |
| Slight discomfort | 4 | 57.15% | 6 | 60.00% |
| No response | 1 | 14.29% | 0 | 0.00% |
| Liked visuals | ||||
| Yes | 3 | 42.86% | 6 | 60.00% |
| Would prefer more realistic | 3 | 42.86% | 3 | 30.00% |
| No response | 1 | 14.29% | 1 | 10.00% |
| Reported relaxation | ||||
| Yes | 5 | 71.43% | 6 | 60.00% |
| No | 2 | 28.57% | 4 | 40.00% |
VAS: Pain
First, we conducted Mauchly tests on the pain scores at baseline, after Tree (GM), and after Body Scan to determine whether the sphericity assumption was met, W = 0.93, χ2(2) = 1.12, P = 0.57. Then, we conducted a 1‐way ANOVA with repeated measures to examine the effect of all interventions on VAS scores (F (2, 32) = 3.96, P = 0.03, P < 0.05; see Table 4). There was a significant difference between VAS scores at baseline, after BFD, and after GM at the 95% confidence level. Then, we conducted a post hoc analysis using pairwise t tests to determine which interventions most decreased VAS scores (see Table 3). We found a reduction in VAS scores after BFD, with a mean reduction of 1.07, t = 2.83, Cohen's d = 0.50, P = 0.01, P < 0.05. We also found a reduction in VAS scores after GM, with a mean reduction of 1.09, t = 2.29, Cohen's d = 0.52, P = 0.04, P < 0.05. These results suggest that both BFD and GM may decrease pain acutely after a VR environment.
Table 4.
ANOVA table for VAS scores (top) and FAS scores (bottom)
| ANOVA (VAS) | |||||
|---|---|---|---|---|---|
| Sources | SS | df | MS | F | P value |
| Subjects | 178.80 | 16 | 11.18 | 6.71 | 0.000 |
| Groups | 13.21 | 2 | 6.60 | 3.96 | 0.029 |
| Error | 53.32 | 32 | 1.67 | ||
| Total | 245.33 | 50 | |||
| ANOVA (FAS) | |||||
|---|---|---|---|---|---|
| Sources | SS | df | MS | F | P value |
| Subjects | 9.75 | 16 | 0.61 | 2.16 | 0.03 |
| Groups | 2.98 | 1.32 | 2.25 | 5.29 | 0.024 |
| Error | 9.02 | 21.19 | 0.43 | ||
| Total | 21.75 | 38.51 | |||
Abbreviation: FAS, Facial Anxiety Scale; MS, mean square; SS, sum of squares; VAS, Visual Analog Scale.
Table 3.
Descriptive table of post hoc pairwise t tests for pain scores (represented by VAS; top four rows) and anxiety scores (represented by FAS; bottom four rows)
| Condition | Preintervention Score | Postintervention Score | M Difference | t Test | P Value | 95% CI LL | 95% CI UL | Cohen's d |
|---|---|---|---|---|---|---|---|---|
| VAS | ||||||||
| Baseline X BFD* | 5.47 | 4.40 | 1.07 | 2.83 | 0.01 | 0.27 | 1.87 | 0.50 |
| Baseline X GM* | 5.47 | 4.38 | 1.09 | 2.29 | 0.04 | 0.08 | 2.10 | 0.52 |
| BFD X GM | 4.40 | 4.38 | 0.02 | 0.04 | 0.97 | −0.97 | 1.01 | 0 |
| FAS | ||||||||
| Baseline X BFD | 1.82 | 1.47 | 0.35 | 1.85 | 0.08 | −0.05 | 0.76 | 0.54 |
| Baseline X GM* | 1.82 | 1.23 | 0.59 | 2.58 | 0.02 | 0.11 | 1.07 | 0.91 |
| BFD X GM* | 1.47 | 1.23 | 0.24 | 2.22 | 0.04 | 0.01 | 0.46 | 0.41 |
Abbreviation: BFD, biofeedback; GM, guided meditation; FAS, Facial Anxiety Scale; LL, lower limit; UL, upper limit; VAS, Visual Analog Scale.
P < 0.05.
FAS: Anxiety
We conducted Mauchly tests on anxiety scores at baseline, after BFD, and after GM and found that the sphericity assumption was not met, W = 0.49, χ2(2) = 10.71, P < 0.05. Then, we used the Greenhouse‐Geisser correction (ε = 0.66) and conducted a 1‐way ANOVA with repeated measures to examine the effect of GM and BFD on baseline FAS scores (F (1.32, 21.19) = 5.27, P < 0.05, see Table 4). There was a significant difference between FAS scores at baseline, after BFD, and after GM at the 95% confidence level. Then, we conducted a post hoc analysis using pairwise t tests to determine which intervention most decreased FAS scores (see Table 3). We found that the greatest reduction in anxiety scores were recorded after the GM intervention, with a mean reduction of 0.59, t = 2.28, Cohen's d = 0.91, P < 0.05. We also found that there was a significant difference between GM and BFD, with a mean reduction of 0.24, t = 2.22, Cohen's d = 0.41, P = 0.04, P < 0.05. These results suggest that GM, but not BFD, may decrease anxiety acutely in a VR environment.
Order of intervention
We conducted pairwise t tests to determine which order of intervention, GM or BFD first, decreased FAS and VAS scores (see Table 5). We found that there was no significant reduction in VAS scores regardless of the order of intervention, with GM followed by BFD (t = 1.96, P = 0.097) or BFD followed by GM (t = 1.81, P = 0.1032). We found that there was no significant reduction in FAS scores regardless of the order of intervention; however, GM followed by BFD (t = 2.34, P = 0.582) was closer to being significant compared with BFD followed by GM (t = 0.89, P = 0.397).
Table 5.
Descriptive table of paired t tests for pain scores and anxiety scores by order of intervention
| Condition | Preintervention Score | Postintervention Score | t Test | P Value | 95% CI LL | 95% CI UL |
|---|---|---|---|---|---|---|
| VAS | ||||||
| Guided Meditation First | ||||||
| Baseline X after both VR sessions | 5.14 | 3.83 | 1.96 | 0.0971 | −0.351 | 3.2081 |
| Biofeedback First | ||||||
| Baseline X after both VR sessions | 5.7 | 4.58 | 1.81 | 0.1032 | −0.2649 | 2.4049 |
| FAS | ||||||
| Guided Meditation First | ||||||
| Baseline X after both VR sessions | 1.71 | 1 | 2.34 | 0.0582 | −0.0341 | 1.4626 |
| Biofeedback First | ||||||
| Baseline X after both VR sessions | 1.9 | 1.65 | 0.89 | 0.3974 | −0.3865 | 0.8865 |
Abbreviation: CI, confidence interval; FAS, Facial Anxiety Scale; LL, lower limit; UL, upper limit; VAS, Visual Analog Scale; VR, virtual reality.
Discussion
VR is an emerging technology for which researchers are finding novel uses in a variety of different disorders. VR has shown promise in traumatic brain injury rehabilitation for both cognitive and gait‐related difficulties 45, 46, 47. VR has shown to be useful in psychiatric settings, especially for those with anxiety‐related disorders 48, such as social anxiety disorder. It has also show to be effective for posttraumatic stress disorder 49. Over the past decade, VR has also been associated with an improvement in acute pain symptoms 26, 35, 50, 51, 52. To the best of our knowledge, no studies to this date have examined the feasibility or effectiveness of VR in an outpatient rheumatology setting. The purpose of this study was to examine the feasibility of a novel VR intervention within an outpatient rheumatology setting.
Our qualitative interview determined that the majority of participants reported a positive—if not profound—experience. These results are consistent with the VR studies done for musculoskeletal pain management 15. Possible modalities for this reduction in pain may be due to a reduction in pain‐related brain activity in the insula and thalamus, ie, how the brain processes pain and produces analgesia 18. Technology involving the use of visual biofeedback has been shown to improve quality of life, pain level, and physical function in patients with RA and SLE 26, 27. Additionally, all participants reported that they would participate in a similar study again if given the opportunity. In terms of the VR experience, we found that the VR device itself was mostly comfortable, which is integral for any intervention involving a population of individuals suffering from chronic diseases. However, many participants (44%) noted that they would prefer a less heavy or bulky device in the future. A small but notable subset of participants (n = 6) remarked that they would have preferred more “realistic” VR environments, although it is unclear whether that change would provide clinical benefit. Overall, the findings in our study suggest that VR interventions are feasible to use in outpatient rheumatology clinics and are well tolerated and often enjoyable for participants.
It is important to note that this is a pilot study with a small sample size (n = 17) and therefore is underpowered to make definite conclusions about efficacy. These results suggest possible benefits from the intervention, though there is a need for a higher‐powered study to solidify findings. Our patients were administered two separate treatment conditions, GM and BFD, and we found that pain was significantly reduced immediately following both conditions with moderate effect sizes, and we did not find a significant difference between those two conditions. Other studies and reviews have found similar trends in immediate reduction of acute and chronic pain post‐VR experience 53, 54, 55, 56.
Anxiety was significantly reduced immediately following an immersive GM environment with a large effect size. However, anxiety wasn't reduced after respiratory BFD. This was inconsistent with results from previous studies 24 and may be a result of the small sample size.
Taken together, these findings suggest that virtual reality may be an efficacious intervention for acute pain relief and anxiety reduction. Specifically, our study suggests that acute pain relief occurs after immersive respiratory biofeedback and, to a lesser extent, immersive GM. On the other hand, our study demonstrated acute anxiety reduction only after GM and not after respiratory BFD. The order of intervention did not have a significant effect on pain or anxiety.
There are a number of limitations in this study. First, interpretation of the results using within‐subject methods can be flawed, as it creates more room for the placebo effect than in a randomized controlled trial. Secondly, as this is only a feasibility study, the sample size is too small to generalize our findings to a larger clinical population. Finally, we elected to use a participant group that is more representative of a real‐life clinic setting than a laboratory. As such, participants had multiple diagnoses, ages, backgrounds, and treatment trials.
Future research should look to replicate these findings with a larger sample size, ideally in a randomized controlled trial. A significant portion of patients in rheumatology clinics suffer from chronic pain so future studies need to demonstrate sustained benefit in this patient population. Hence, longer trials with varying dose exposures to VR therapy would be helpful in determining the optimal length, intertreatment gaps, and duration of treatment in rheumatology patients. Another next step would involve alternative types of biofeedback, including heart rate variability biofeedback, temperature biofeedback, or electromyogram biofeedback. Lastly, future researchers could use more thorough pain and anxiety scales to tease out which dimensions most benefit from these novel experiences.
Conclusion
This is the first study to investigate the tolerability and acceptance of VR by patients in a general Rheumatology clinic. The patients had a mix of conditions seen in typical rheumatology clinics, including RA, SLE, osteoarthritis, and fibromyalgia. In this study, rheumatology patients tolerated the VR‐based BFD and GM and experienced a short‐term reduction in pain and anxiety. Our results demonstrate that VR could be a feasible nonpharmacological solution for the management of pain and anxiety in rheumatology patients. Further trials that are larger, of greater duration, and with varying treatment exposures are required to solidify the use of VR as a viable treatment option in the rheumatology clinic. As the technology and user experience of VR‐based interventions improves, VR technology has the potential to greatly reduce the pain and suffering of rheumatology patients.
Author Contributions
All listed authors have contributed sufficiently to this project to take public responsibibility for the content, including participation in the concept, design, analysis, writing, and/or revision of the manuscript. As primary investigator, Dr. Venuturupalli takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Venuturupalli, Vicari.
Acquisition of data
Chu, Vicari, Kumar.
Analysis and interpretation of data
Fortune, Spielberg.
Drafting the manuscript
Venuturupalli, Fortune, Chu, Kumar, Vicari, Spielberg.
Revising the manuscrupt
Venuturupalli, Fortune, Chu, Kumar, Vicari, Spielberg.
Acknowledgments
Completion of this manuscript would not be possible without the efforts of the following individuals. We would like to acknowledge Brennan Spiegel, MD and Brendan Birckhead, MD for contributing to the concept of the manuscript and the scientific method, as well as James Mirocha, MS for providing feedback on the statistics. We would also like to recognize Nikhil Davuluri, BS and Sarosh Motivala, PhD for reviewing the manuscript and providing valuable edits. Finally, we would like to thank Applied VR for supplying our team with equipment.
The research reported in this publication was supported by Attune Health. Dr. Venuturupalli is the director of this institution. No other disclosures relevant to this article were reported.
REFERENCES
- 1. De Carvalho MR, Tebexreni AS, Salles CA, Barros Neto T, Natour J. Oxygen uptake during walking in patients with rheumatoid arthritis–a controlled study. J Rheumatol 2004;31:655–62. [PubMed] [Google Scholar]
- 2. Yu C, Gershwin ME, Chang C. Diagnostic criteria for systemic lupus erythematosus: a critical review. J Autoimmun 2014;48–49:10–3. [DOI] [PubMed] [Google Scholar]
- 3. Stojanovich L, Marisavljevich D. Stress as a trigger of autoimmune disease. Autoimmun Rev 2008;7:209–13. [DOI] [PubMed] [Google Scholar]
- 4. Crosby LJ. Stress factors, emotional stress and rheumatoid arthritis disease activity. J Adv Nurs 1988;13:452–61. [DOI] [PubMed] [Google Scholar]
- 5. Wallace DJ. The role of stress and trauma in rheumatoid arthritis and systemic lupus erythematosus. Semin Arthritis Rheum 1987;16:153–7. [DOI] [PubMed] [Google Scholar]
- 6. Zochling J, Bohl‐Bühler MH, Baraliakos X, Feldtkeller E, Braun J. Infection and work stress are potential triggers of ankylosing spondylitis. Clin Rheumatol 2006;25:660–6. [DOI] [PubMed] [Google Scholar]
- 7. Koutantji M, Pearce S, Harrold E. Psychological aspects of vasculitis. Rheumatology (Oxford) 2000;39:1173–9. [DOI] [PubMed] [Google Scholar]
- 8. Paulozzi LJ, Jones CM, Mack KA, Rudd RA. Vital signs: overdoses of prescription opioid pain relievers: United States, 1999–2008. MMWR Morb Mortal Wkly Rep 2011;60:1487–92. [PubMed] [Google Scholar]
- 9. Coe MA, Nuzzo PA, Lofwall MR, Walsh SL. Effects of short‐term oxycodone maintenance on experimental pain responses in physically dependent opioid abusers. J Pain 2017;18:825–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. International Association for the Study of Pain . IASP Statement on Opioids. February 2018. URL: https://www.iasp-pain.org/Advocacy/Content.aspx?ItemNumber=7194.
- 11. Curtis JR, Xie F, Smith C, Saag KG, Chen L, Beukelman T, et al. Changing trends in opioid use among patients with rheumatoid arthritis in the United States. Arthritis Rheumatol 2017;69:1733–40. [DOI] [PubMed] [Google Scholar]
- 12. Salsitz EA. Chronic pain, chronic opioid addiction: a complex nexus. J Med Toxicol 2016;12:54–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mahan KT. The opioid crisis. J Foot Ankle Surg 2017;56:1–2. [DOI] [PubMed] [Google Scholar]
- 14. Kuo YF, Raji MA, Chen NW, Hasan H, Goodwin JS. Trends in opioid prescriptions among Part D Medicare recipients from 2007 to 2012. Am J Med 2016;129:221.e21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lin HT, Li YI, Hu WP, Huang CC, Du YC. A scoping review of the efficacy of virtual reality and exergaming on patients of musculoskeletal system disorder. J Clin Med 2019;8:E791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hoffman HG, Richards TL, Van Oostrom T, Coda BA, Jensen MP, Blough DK, et al. The analgesic effects of opioids and immersive virtual reality distraction: evidence from subjective and functional brain imaging assessments. Anesth Analg 2007;105:1776–83. [DOI] [PubMed] [Google Scholar]
- 17. Li A, Montaño Z, Chen VJ, Gold JI. Virtual reality and pain management: current trends and future directions. Pain Manag 2011;1:147–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gold JI, Belmont KA, Thomas DA. The neurobiology of virtual reality pain attenuation. Cyberpsychol Behav 2007;10:536–44. [DOI] [PubMed] [Google Scholar]
- 19. Sharma H. Meditation: process and effects. Ayu 2015;36:233–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ball EF, Nur Shafina Muhammad Sharizan E, Franklin G, Rogozińska E. Does mindfulness meditation improve chronic pain? A systematic review. Curr Opin Obstet Gynecol 2017;29:359–66. [DOI] [PubMed] [Google Scholar]
- 21. Navarro‐Haro MV, López‐Del‐Hoyo Y, Campos D, Linehan MM, Hoffman HG, García‐Palacios A, et al. Meditation experts try Virtual Reality Mindfulness: a pilot study evaluation of the feasibility and acceptability of virtual reality to facilitate mindfulness practice in people attending a mindfulness conference. PLoS One 2017;12:e0187777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dissanayake RK, Bertouch JV. Psychosocial interventions as adjunct therapy for patients with rheumatoid arthritis: a systematic review. Int J Rheum Dis 2010;13:324–34. [DOI] [PubMed] [Google Scholar]
- 23. Frank DL, Khorshid L, Kiffer JF, Moravec CS, McKee MG. Biofeedback in medicine: who, when, why and how? [Review Article]. Ment Health Fam Med 2010;7:85–91. [PMC free article] [PubMed] [Google Scholar]
- 24. El Miedany Y, El Gaafary M, Palmer D. Assessment of the utility of visual feedback in the treatment of early rheumatoid arthritis patients: a pilot study. Rheumatol Int 2012;32:3061–8. [DOI] [PubMed] [Google Scholar]
- 25. Greco CM, Rudy TE, Manzi S. Effects of a stress‐reduction program on psychological function, pain, and physical function of systemic lupus erythematosus patients: a randomized controlled trial. Arthritis Rheum 2004;51:625–34. [DOI] [PubMed] [Google Scholar]
- 26. Malloy KM, Milling LS. The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clin Psychol Rev 2010;30:1011–8. [DOI] [PubMed] [Google Scholar]
- 27. Manzoni GM, Cesa GL, Bacchetta M, Castelnuovo G, Conti S, Gaggioli A, et al. Virtual reality‐enhanced cognitive‐behavioral therapy for morbid obesity: a randomized controlled study with 1 year follow‐up. Cyberpsychol Behav Soc Netw 2016;19:134–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cesa GL, Manzoni GM, Bacchetta M, Castelnuovo G, Conti S, Gaggioli A, et al. Virtual reality for enhancing the cognitive behavioral treatment of obesity with binge eating disorder: randomized controlled study with one‐year follow‐up. J Med Internet Res 2013;15:e113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Riva G. The key to unlocking the virtual body: virtual reality in the treatment of obesity and eating disorders. J Diabetes Sci Technol 2011;5:283–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. McCann RA, Armstrong CM, Skopp NA, Edwards‐Stewart A, Smolenski DJ, June JD, et al. Virtual reality exposure therapy for the treatment of anxiety disorders: an evaluation of research quality. J Anxiety Disord 2014;28:625–31. [DOI] [PubMed] [Google Scholar]
- 31. Malbos E, Boyer L, Lancon C. Virtual reality in the treatment of mental disorders. Presse Med 2013;42:1442–52. In French. [DOI] [PubMed] [Google Scholar]
- 32. Rothbaum BO, Garcia‐Palacios A, Rothbaum AO. Tratamiento de los trastornos de ansiedad con terapia de exposición a realidad virtual. Rev Psiquiatr Salud Ment 2012;5:67–70. [DOI] [PubMed] [Google Scholar]
- 33. JahaniShoorab N, Ebrahimzadeh Zagami S, Nahvi A, Mazluom SR, Golmakani N, Talebi M, et al. The effect of virtual reality on pain in primiparity women during episiotomy repair: a randomize clinical trial. Iran J Med Sci 2015;40:219–24. [PMC free article] [PubMed] [Google Scholar]
- 34. Hua Y, Qiu R, Yao WY, Zhang Q, Chen XL. The effect of virtual reality distraction on pain relief during dressing changes in children with chronic wounds on lower limbs. Pain Manag Nurs 2015;16:685–91. [DOI] [PubMed] [Google Scholar]
- 35. Morris LD, Louw QA, Grimmer‐Somers K. The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: a systematic review. Clin J Pain 2009;25:815–26. [DOI] [PubMed] [Google Scholar]
- 36. Su WC, Yeh SC, Lee SH, Huang HC. A virtual reality lower‐back pain rehabilitation approach: system design and user acceptance analysis In: UAHCI 2015: Universal Access in Human‐Computer Interaction. Access to Learning, Health and Well‐Being. Vol. 9177 Cham, Switzerland: Springer; 2015. p. 374–82. [Google Scholar]
- 37. Chirico A, Lucidi F, De Laurentiis M, Milanese C, Napoli A, Giordano A. Virtual reality in health system: beyond entertainment. A mini‐review on the efficacy of VR during cancer treatment. J Cell Physiol 2016;231:275–87. [DOI] [PubMed] [Google Scholar]
- 38. Ogourtsova T, Souza Silva W, Archambault PS, Lamontagne A. Virtual reality treatment and assessments for post‐stroke unilateral spatial neglect: a systematic literature review. Neuropsychol Rehabil 2017;27:409–54. [DOI] [PubMed] [Google Scholar]
- 39. Pedroli E, Serino S, Cipresso P, Pallavicini F, Riva G. Assessment and rehabilitation of neglect using virtual reality: a systematic review. Front Behav Neurosci 2015;9:226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gaba DM. The future vision of simulation in health care. Qual Saf Health Care 2004;13 Suppl 1:i2–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Cedars Sinai . Cedars‐Sinai study finds virtual reality therapy helps decrease pain in hospitalized patients. March 2017. URL: https://www.cedars-sinai.edu/About-Us/News/News-Releases-2017/Cedars-Sinai-Study-Finds-Virtual-Reality-Therapy-Helps-Decrease-Pain-in-Hospitalized-Patients.aspx.
- 42. Lataoui S, Belghali S, Zeglaoui H, Bouajina E, Ben Saad H. Sub‐maximal aerobic capacity and quality of life of patients with rheumatoid arthritis. Rev Mal Respir 2017;34:74–85. In French. [DOI] [PubMed] [Google Scholar]
- 43. Haefeli M, Elfering A. Pain assessment. Eur Spine J 2006;15 Suppl 1:S17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Brauer C, Thomsen JF, Loft IP, Mikkelsen S. Can we reply on retrospective pain assessments? [Peer-Reviewed Article]. Am J Epidemiol 2003;157:552–7. [DOI] [PubMed] [Google Scholar]
- 45. Aida J, Chau B, Dunn J. Immersive virtual reality in traumatic brain injury rehabilitation: a literature review. NeuroRehabilitation 2018;42:441–48. [DOI] [PubMed] [Google Scholar]
- 46. Shin H, Kim K. Virtual reality for cognitive rehabilitation after brain injury: a systematic review. J Phys Ther Sci 2015;27:2999–3002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Dahdah MN, Bennett M, Prajapati P, Parsons TD, Sullivan E, Driver S. Application of virtual environments in a multi‐disciplinary day neurorehabilitation program to improve executive functioning using the Stroop task. NeuroRehabilitation 2017;41:721–34. [DOI] [PubMed] [Google Scholar]
- 48. Maples‐Keller JL, Bunnell BE, Kim SJ, Rothbaum BO. The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv Rev Psychiatry 2017;25:103–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Carl E, Stein AT, Levihn‐Coon A, Pogue JR, Rothbaum B, Emmelkamp P, et al. Virtual reality exposure therapy for anxiety and related disorders: a meta‐analysis of randomized controlled trials. J Anxiety Disord 2019;61:27–36. [DOI] [PubMed] [Google Scholar]
- 50. Ramachandran VS, Seckel EL. Using mirror visual feedback and virtual reality to treat fibromyalgia. Med Hypotheses 2010;75:495–6. [DOI] [PubMed] [Google Scholar]
- 51. Pourmand A, Davis S, Marchak A, Whiteside T, Sikka N. Virtual reality as a clinical tool for pain management. Curr Pain Headache Rep 2018;22:53. [DOI] [PubMed] [Google Scholar]
- 52. Wiederhold BK, Gao K, Sulea C, Wiederhold MD. Virtual reality as a distraction technique in chronic pain patients. Cyberpsychol Behav Soc Netw 2014;17:346–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mallari B, Spaeth EK, Goh H, Boyd BS. Virtual reality as an analgesic for acute and chronic pain in adults: a systematic review and meta‐analysis. J Pain Res 2019;12:2053–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ahmadpour N, Randall H, Choksi H, Gao A, Vaughan C, Poronnik P. Virtual reality interventions for acute and chronic pain management. Int J Biochem Cell Biol 2019;114:105568. [DOI] [PubMed] [Google Scholar]
- 55. Jones T, Moore T, Choo J. The impact of virtual reality on chronic pain. PLoS One 2016;11:e0167523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Tashjian VC, Mosadeghi S, Howard AR, Lopez M, Dupuy T, Reid M, et al. Virtual reality for management of pain in hospitalized patients: results of a controlled trial. JMIR Ment Health 2017;4:e9. [DOI] [PMC free article] [PubMed] [Google Scholar]


