Abstract
Background
Transitions between healthcare settings are vulnerable points for patients.
Aim
To identify key threats to safe patient transitions from hospital to primary care settings.
Design and setting
Three-round web-based Delphi consensus process among clinical and non-clinical staff from 39 primary care practices in North West London, England.
Method
Round 1 was a free-text idea-generating round. Rounds 2 and 3 were consensus-obtaining rating rounds. Practices were encouraged to complete the questionnaires at team meetings. Aggregate ratings of perceived level of importance for each threat were calculated (1–3: ‘not important’, 4–6: ‘somewhat important’, 7–9: ‘very important’). Percentage of votes cast for each patient or medication group were recorded; consensus was defined as ≥75%.
Results
A total of 39 practices completed round 1, 36/39 (92%) completed round 2, and 30/36 (83%) completed round 3. Round 1 identified nine threats encompassing problems involving communication, service organisation, medication provision, and patients who were most at risk. ‘Poor quality of handover instructions from secondary to primary care teams’ achieved the highest rating (mean rating at round 3 = 8.43) and a 100% consensus that it was a ‘very important’ threat. Older individuals (97%) and patients with complex medical problems taking >5 medications (80%) were voted the most vulnerable. Anticoagulants (77%) were considered to pose the greatest risk to patients.
Conclusion
This study identified specific threats to safe patient transitions from hospital to primary care, providing policymakers and healthcare providers with targets for quality improvement strategies. Further work would need to identify factors underpinning these threats so that interventions can be tailored to the relevant behavioural and environmental contexts in which these threats arise.
Keywords: communication, patient handover, patient discharge, transition of care
INTRODUCTION
Transition between healthcare settings are a recognised vulnerable time in a patient’s care, with estimates that between 19–23% of patients transitioning from hospital to primary care will experience an incident in the weeks following discharge.1 Incidents range from avoidable symptoms, for example poorly controlled pain, to additional emergency department visits, hospital readmissions, or even death.1–3
Growing demand for NHS inpatient beds has increased pressures on hospital teams to discharge patients sooner.4,5 Patients are consequently spending more of their recovery time in their own homes, vulnerable in the event of unanticipated clinical deteriorations. Often a patient’s first point of contact in the community is their GP, who is expected to initially manage any complications before deciding if and when to escalate problems to hospital specialists.6 GPs make such decisions based on information delivered to them by patients themselves or contained within their hospital discharge summary, a written narrative describing the patient’s hospital admission and plans for future management.
Discharge summaries, frequently the sole source of handover between hospital and primary care teams, are usually written by doctors qualified <2 years7,8 who move between teams, or even hospitals, as frequently as every 4 months,9 perpetuating unfamiliarity with systems and processes, and increasing risk of miscommunication, errors, and compromises in patient safety. Furthermore, the introduction of the European Working Time Directives in 2004 has resulted in changes to doctors’ shift patterns, with increased frequency of handovers and inevitable implications for continuity of care.10 Fragmentation of care perpetuated by the number of services available to patients today in community settings in England, such as urgent care centres, local pharmacies, or the NHS 111 helpline, also makes it difficult for GPs to follow developments in their patients’ clinical histories, limiting their ability to anticipate and mitigate any adverse events or changes in their clinical conditions while in the community.11,12 Such challenges in hospital and community settings make patients today even more vulnerable to harm during the critical transition between hospital and primary care.
Williams and colleagues examined safety issues related to patient transitions from hospital to primary care in England and Wales utilising incident reporting data from the National Reporting and Learning System (NRLS).13 Their study identified four key areas where deficits led to patient harm: errors in discharge communication, referrals to community care teams, medication provision, and availability of therapeutic adjuncts and care equipment, such as wound dressings or urinary catheters, on discharge.13 In 2017, the World Health Organization (WHO) included medication safety in transitions of care among its early priority actions in its medication-themed Global Patient Safety Challenge, acknowledging that mistakes are usually made because of flawed systems and processes rather than neglect by professionals.14 However, insights into threats to safe patient transitions remain broad and require greater definition before they can be targeted effectively by policymakers. Previous studies have relied on formalised channels, such as the NRLS,13,15 for insights into such threats. Although these data are valuable, they do not allow detailed capture of insights from frontline staff. There is evidence suggesting that professional attitudes, culture, and individuals’ behaviours play an important role in patient safety during transitions of care.16,17 In order for interventions to be more effective, they should target specific behavioural and environmental factors, and be based on theory and evidence as this is known to lead to more effective interventions.17–19 However, interventions to date have largely focused on improving coordination of care, communication, and information sharing between providers, with few demonstrating any application of behavioural theory, or considering organisational context or culture in their design.
How this fits in
| Transitions of care between healthcare settings are known vulnerable times for patients, when one in four people experience a safety incident in the weeks following their discharge from hospital. Existing research does not sufficiently detail the organisational and behavioural context related to the discharge process, or specific clinical groups at risk, therefore policymakers have not been able to effectively identify and address root causes of threats to safe patient transitions. A Delphi consensus process, engaging frontline primary care staff, has identified local safety priorities for patient transitions from hospital to primary care settings within a defined urban area. The detailed information generated by this Delphi study exposes the multifaceted threats to patient safety during this transition. Future work should further explore the environmental and behavioural contexts surrounding discharge to enable the design of effective interventions with successful long-term outcomes. |
This study aims to bridge some of these gaps by defining specific threats to patient safety during transitions from hospital to primary care, which can subsequently be explored from behavioural, social, and environmental perspectives, facilitating future evidence-based and theory-led intervention design. This study will examine the views of frontline primary care staff, both clinical and non-clinical, such as practice managers, administrative, and reception staff, on the largest threats to safe patient transitions from hospital to primary care. This study will also explore which patient groups are most vulnerable and medications that are thought to pose the greatest risk to patients during this transition to identify specific and tangible target groups that could benefit most from future interventions.
METHOD
A three-round Delphi consensus approach20 was undertaken to identify and prioritise key threats to safe patient transitions from hospital to primary care as perceived by primary care practices (PCPs) in North West (NW) London. The Delphi process is an iterative consensus technique whereby a panel of participants, typically field experts, are provided with anonymised feedback about choices made by their peers in previous rounds. Any bias from senior or dominant members is reduced by maintaining anonymity of participants’ responses, allowing outcomes to more accurately reflect the opinions of participants as a group. The WHO definition of ‘patient safety’ was used as it is: ‘ ... the absence of preventable harm to a patient [...] and reduction of risk of unnecessary harm associated with health care to an acceptable minimum’.21
Selection of expert panel
The expert panel in this study was formed of PCPs from NW London. All 367 practices, encompassed by eight clinical commissioning groups (CCGs), within the NW London Clinical Research Network (CRN) were eligible for inclusion. These practices serve a population of >2 million patients,22 a significant proportion of whom are from black, Asian, and minority ethnic (BAME) backgrounds, with the main disease burdens being chronic cardiorespiratory disease and cancer.23 Whole practices, as opposed to individual professionals, were included as units of analysis, encouraging incorporation of views from both clinical and non-clinical staff to provide a more holistic representation of existing threats.
Although all 367 eligible practices received an email inviting them to participate in the study, only 70 practices accepted the invitation and signed up to the study.
Literature review
A scoping literature review was conducted to elicit the main threats to patient safety during transitions from hospital to primary care described by existing research, and involved a search of PubMed using the following terms: ‘patient safety’ or ‘safety’; ‘transitions of care’ or ‘patient transitions’ or ‘patient discharge’; and ‘incident’ or ‘safety incident’. As this was a scoping review, no other limits were imposed. A list of the threats identified was compared with responses given by participants in round 1, ensuring all potential problems would be considered by participating practices in rounds 2 and 3 (see Supplementary Box 1 for a list of threats identified).
Delphi rounds
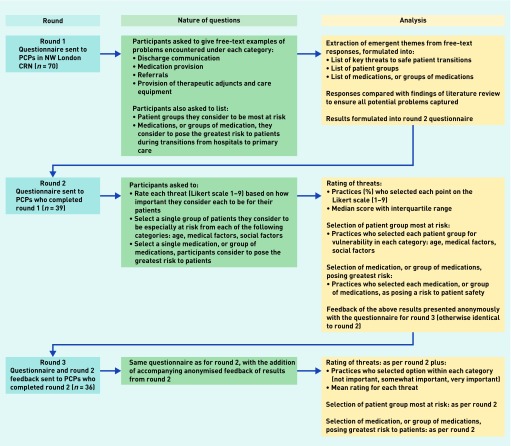
An outline of the study process is presented in Figure 1. Questionnaires were sent electronically using Qualtrics software (http://www.qualtrics.com). The online format enabled practices to determine answers at a time convenient for them, for example at a practice meeting, before nominated senior practice representatives, such as a practice partner, submitted responses for each round. This provided consistency in contributors from each participating practice. Practices were instructed to submit only one questionnaire per practice. They were also requested to complete the questionnaire during a practice meeting so that answers would reflect, as best as possible, the views of the multiple professionals working at the practice. Practices were given 3 weeks to submit answers for each round, with email reminders sent after 1 and 2 weeks. Subsequent questionnaires were only sent to practices who had submitted answers in preceding rounds. Each practice was considered as a single and equal unit for analytical purposes, therefore no weighting across practices was conducted.
Figure 1.
The Delphi process and study outline. CRN = clinical research network. NW = North West. PCP = primary care practices.
Round 1
Round 1 was sent to 70 practices in NW London and aimed to generate a list of threats to patient safety that PCPs and their patients had encountered during transitions from hospital to primary care that caused risk of, or actual, harm to patients. The questionnaire for round 1 was developed in consultation with experts in the fields of patient safety, implementation science, and primary care. It was based on the findings from the study by Williams and colleagues,13 which identified four key categories of threats from patient discharge using NHS NRLS data: errors in discharge communication, referrals to community care teams, medication provision, and availability of therapeutic adjuncts and care equipment.13 These four categories served as broad headings under which participants were prompted to describe, in free text, problems encountered during patients’ transitions from hospital to primary care. Practices were also asked which patient groups they considered the most vulnerable, and which medications they considered to pose the greatest risk to patients during this transition. Final versions of the questionnaire were piloted with GP trainees to ensure relevance and clarity of questions (see Supplementary Box 2 for details).
Round 1 analysis
Qualitative free-text responses were analysed using an inductive thematic analysis approach. The first author read through all of the responses and identified discrete threats to patient safety reported by GP practices. Similar threats were grouped together, and a theme label summarising the nature of these threats inductively generated, for example ‘poor quality handover instructions from secondary care teams’ and ‘problems sending and receiving discharge paperwork’, were grouped under the theme label ‘communication between primary and secondary care teams’. These were checked against the literature review to ensure all previously identified threats were covered by PCPs’ responses. The identified threats and thematic synthesis were then discussed and refined with the broader research team until consensus was reached on the final groupings and theme labels. Lists of the most vulnerable patient groups and the medications considered to pose the greatest risk were also compiled.
Round 2
Themes extracted from round 1 were presented as threats in the round 2 questionnaire accompanied by specific examples given by participants in round 1. Participants were asked to rate each threat according to how important they considered it to be on a Likert scale (1 = not important at all to 9 = extremely important). Participants were also asked to select a single group of patients they considered to be the most at risk and a single medication, or group of medications, they considered to pose the greatest risk from lists compiled following round 1.
Round 2 analysis
The ratings for each threat were categorised as ‘not important’ (1–3), ‘somewhat important’ (4–6), and ‘very important’ (7–9) (Figure 1). Percentages of votes cast in each of the three categories were calculated. Consensus was set at ≥75%. Percentage of votes cast for patient and medication groups considered most at risk was also calculated and, again, consensus was set at ≥75%.
Round 3
Round 3 questionnaires were sent to practices that completed round 2. The round 3 questionnaire included a summary of anonymised aggregate responses from round 2 including a median score for each threat. A median rating was presented in order to portray a fairer indication of how important the cohort considered the threat to be, as opposed to a mean score that would at this stage have been significantly influenced by a few outlying ratings. Patient or medication groups that did not receive any votes in round 2 were excluded from round 3 to facilitate consensus generation. Practices were again asked to rate each threat according to their level of importance. Participants were encouraged to review the anonymised responses of their peers before answering round 3. They were advised that if following their review they wished to change how they answered in round 3 they could do so.
Round 3 analysis
Responses to round 3 were analysed as per round 2. Additionally, the mean ratings for each threat were calculated alongside the percentage of votes cast in each category (‘not important’, ‘somewhat important’, ‘very important’) (Figure 1, enabling the ranking of threats in order of perceived importance).
RESULTS
Of the 70 practices that received the questionnaire, 39 (56%) responded in round 1, covering a patient population of >310 000. There was representation throughout the three rounds of the study from all CCGs within the NW London CRN.
Literature review
The scoping literature review (see Supplementary Box 1) identified 51 discrete problems, 47 of which could be grouped into the four key areas for improvement identified by Williams and colleagues13 on which the round 1 questionnaire was designed. The category ‘Referrals to community care teams’ was renamed ‘Referrals’ following the literature review to reflect identified threats relating to difficulties referring patients to broader healthcare services, enabling practices to raise such problems in their responses in round 1.
Delphi rounds
Round 1
Following thematic analysis of round 1 responses, the four categories under which responses were recorded were restructured into five themes: communication between primary and secondary care teams; collaboration between primary and secondary care teams; communication with patients, relatives, and carers; support for patients, relatives, and carers in the home environment; and medication safety. These five themes encompassed nine key threats to safe patient transitions from hospital to primary care (see Supplementary Box 3 for details of themes). Thematic exhaustiveness of responses was reached by the 13th participating practice, with the nine threats covering all those identified in the scoping literature review (see Supplementary Box 1). Additional threats described by practices that were not found in the scoping literature review included ‘Key handover instructions not being acted on by primary care’ and ‘Poor engagement with primary care services in patient discharge planning’. In addition to raising threats that PCPs felt put their patients at risk of harm, practices highlighted a number of inefficiencies that significantly impacted workloads of primary care teams and that contained an underlying behavioural dimension. For example, across all four categories in round 1, practices conveyed frustration at being asked, or expected, by hospital teams to execute actions for recently discharged patients that were either impossible for primary care teams to perform, owing to a lack of resources or access to certain services, or deemed considerably more challenging to organise from the community setting. Many practices expressed that the information received from hospital teams was insufficient to enable safe ongoing patient care in the community and described challenges in trying to contact hospital professionals for clarifications. There were also many examples of patients and their families having a poor understanding of their treatment and future management plans, requiring primary care teams to fill this gap and manage expectations. Poor communication with patients included instructions around medication regimens, which practices reported were frequently changed without adequate explanations given to patients and their carers.
Patient groups identified as most at risk of harm fell into three categories determined by age, medical, and social factors (Table 1). Medications considered by practices to pose the greatest risk following round 1 are listed in Table 1.
Table 1.
Consensus for patient groups considered most at risk and medication groups considered to pose the greatest risk to patients during transitions from hospital to primary care in rounds 2 and 3
| Category | Groups | Consensus round 2,% | Consensus round 3, % |
|---|---|---|---|
| Age | Children | 2.78 | — |
| People who are older and frail | 97.22 | — | |
|
| |||
| Medical factors | Cancer | 2.78 | 3.33 |
| Complex patients on >5 medications | 58.33 | 80.00 | |
| Diabetes, including those newly started on insulin | 0 | — | |
| Drug addiction or those with alcohol dependency | 0 | — | |
| Heart failure | 0 | — | |
| Immunosuppression | 0 | — | |
| Learning disabilities and cognitive disorders (including dementia) | 16.67 | 6.67 | |
| Orthopaedic | 0 | — | |
| Palliative care | 0 | — | |
| Patients on anticoagulants | 2.78 | 0 | |
| Patients requiring services such as physiotherapy following surgery | 0 | — | |
| Patients who are frequently admitted to hospital | 5.56 | 3.33 | |
| Patients who have had a recent change to their medication | 5.56 | 3.33 | |
| Chronic kidney disease | 0 | — | |
| Poor vision or hearing | 2.78 | 3.33 | |
| Pregnancy | 2.78 | 0 | |
| Psychiatric illness | 0 | — | |
| Stroke | 2.78 | 0 | |
|
| |||
| Social factors | Illiteracy | 5.56 | 3.33 |
| Low socioeconomic status | 0 | — | |
| Patients who are non-English speakers, ethnic minorities, and refugees | 33.33 | 43.33 | |
| Out-of-area discharges | 0 | — | |
| Patients being partly managed by private health services | 0 | — | |
| Patients who are new to the practice or unsure about the NHS health system | 0 | — | |
| Patients who live on boundaries of CCG catchment areas | 0 | — | |
| Patients with no fixed abode | 8.33 | 10.00 | |
| Patients with poor mobility | 0 | — | |
| Patients with poor understanding of their health conditions | 8.33 | 6.67 | |
| Patients who are socially isolated (including housebound) | 19.44 | 20.00 | |
| Vulnerable adults requiring social care support and safeguarding cases | 25.00 | 16.67 | |
|
| |||
| Medications or groups of medications | Antibiotics | 0 | — |
| Anticoagulants (including warfarin, clopidogrel, rivaroxaban and other NOACs, DOACs) | 44.44 | 76.67 | |
| Anti-epileptic medications | 2.78 | 0 | |
| Antihypertensive medications (including ACEi, ARB) | 5.56 | 0 | |
| Antipsychotics | 2.78 | 3.33 | |
| DMARDs | 8.33 | 3.33 | |
| Eye drops | 0 | — | |
| Hormone tablets initiated by sex reassignment clinics | 2.78 | 0 | |
| Hypoglycaemics and insulin | 0 | — | |
| Immunosuppressants | 2.78 | 0 | |
| Injectables | 5.56 | 3.33 | |
| Melatonin | 0 | — | |
| Pain medications (including opioids) | 11.11 | 3.33 | |
| Sedatives (including benzodiazepines) | 2.78 | 6.67 | |
| Statins | 0 | — | |
| Steroids (oral and topical) | 0 | — | |
| Unlicensed medications of various specialties | 11.11 | 3.33 | |
ACEi = angiotensin-converting enzyme inhibitor. ARB = angiotensin receptor blockers. CCG = clinical commissioning group. DMARDs = disease modifying anti-rheumatic drugs. DOACs = direct oral anticoagulant. NOACs = non-vitamin K antagonist oral anticoagulants.
Round 2
Thirty-six practices (92%) completed round 2, with results presented in Tables 1 and 2. Consensus (≥75% agreement) was reached that 8/9 threats were considered ‘very important’ (Table 2). All nine threats were included in round 3 to strengthen consensus at the level of individual Likert points and monitor consistency of responses.
Table 2.
Most important threats to safe patient transitions from hospital to primary care, ranked by mean rating and percentage consensus of threat being considered ‘very important’ following analysis of round 3, round 2 results also displayed
| Final rank | Mean rating at round 3 | Threat | Round 3 | Round 2 | ||||
|---|---|---|---|---|---|---|---|---|
| Practices rating problem ‘very important’,% | Median rating | IQR of median rating | Practices rating problem ‘very important’,% | Median rating | IQR of median rating | |||
| 1 | 8.43 | Poor quality of handover instructions from secondary to primary care | 100.00 | 8.5 | 1 | 97.22 | 9.0 | 1 |
| 2 | 8.43 | Patients discharged before arrangements for care in place at home or in the community | 93.33 | 9.0 | 1 | 88.89 | 9.0 | 2 |
| 3 | 8.40 | Unsafe provision or availability of medication following patient discharge | 93.33 | 9.0 | 1 | 86.11 | 9.0 | 1 |
| 4 | 8.23 | Unreasonable handover of workload from secondary to primary care | 93.33 | 8.5 | 1 | 91.67 | 9.0 | 1 |
| 5 | 8.17 | Problems in sending and receiving discharge paperwork | 93.33 | 8.0 | 1 | 91.67 | 9.0 | 1 |
| 6 | 7.83 | Key handover instructions not acted on by primary care | 86.67 | 8.0 | 2 | 83.33 | 8.0 | 2 |
| 7 | 7.80 | Poor information given to patients, relatives, or carers on discharge from hospital | 86.67 | 8.0 | 1 | 88.89 | 8.0 | 2 |
| 8 | 7.80 | Unsafe prescribing practices during a patient’s transition from hospital to home | 83.33 | 8.0 | 2 | 77.78 | 8.0 | 2 |
| 9 | 7.23 | Poor engagement with primary care services in patient discharge planning | 66.67 | 9.0 | 3 | 69.44 | 7.0 | 2 |
IQR = interquartile range.
A strong consensus (97%) was achieved that older and frail people were the most vulnerable group in terms of age, and therefore this question was excluded from round 3. In terms of medical and social factors, no consensus was reached after round 2 as to which groups within these categories were most at risk of harm, nor which medication group posed the greatest risk, therefore these questions were included in round 3 (Table 1).
Round 3
Thirty practices (83%) completed round 3. First, for the most important threats to safe patient transitions from hospital to primary care: the mean scores for the nine threats indicated that they were all considered ‘very important’, though only 8/9 reached consensus of ≥75% (Cronbach’s α 0.79). Consensus was still not achieved at the level of individual Likert points, therefore threats were ranked according to a combination of their mean scores and strength of consensus in the ‘very important’ category (Table 2).
All participating practices (100%) agreed that ‘Poor quality of handover instructions from secondary to primary care’ (mean rating at round 3 = 8.43) was a ‘very important’ threat to safe patient transitions from hospital to primary care settings. Subcategories of this threat alongside specific examples are presented in Box 1. Over 90% of participating practices agreed that a further four problems were also ‘very important’ threats to safe patient transitions. These problems were: ‘Patients discharged before arrangements for care in place at home or in the community’ (93%), ‘Unsafe provision or availability of medication following patient discharge’ (93%), ‘Unreasonable handover of workload from secondary to primary care’ (93%), and ‘Problems in sending and receiving discharge paperwork’ (93%). The only threat that practices did not achieve consensus regarding its level of importance was ‘Poor engagement with primary care services in patient discharge planning’ (67%). The remaining three problems achieved a consensus of >80% that they too were considered ‘very important’ threats to safe patient transitions.
Box 1.
Subcategories and specific examples of highest-ranking threat ‘Poor quality of handover instructions from secondary to primary care teams’
| Subcategory | Specific examples |
|---|---|
| Key information missing from discharge summaries received by primary care from discharging teams |
|
| Poor quality of written handover content in discharge summary sent by discharging teams to primary care |
|
| Lack of clear explanation and instructions for primary care regarding patients’ medications at discharge |
|
| Lack of clarity regarding patient requirements and instructions for therapeutic adjuncts and care equipment |
|
| Poor communication between primary and secondary care teams regarding follow-up arrangements and referrals |
|
Second, for the most vulnerable patients during transitions from hospital to primary care, in addition to older and frail people, consensus was reached (80%) that those with complex medical problems taking >5 medications were particularly at risk (Table 1). No consensus was achieved on which social factors put patients most at risk, though the group that received the most votes (43%) was people who were non-English speakers, ethnic minorities, and refugees.
Third, for medications posing the greatest risk to patients during transitions from hospital to primary care, consensus was reached after round 3 (77%) that anticoagulants, including warfarin, clopidogrel, rivaroxaban, and other non-vitamin K antagonist oral anticoagulants (NOACs) and direct oral anticoagulants (DOACs) were the group of medications that posed the greatest risk to patients transitioning from hospital to primary care (Table 1).
DISCUSSION
Summary
This study identified and prioritised the most important threats to safe patient transitions from hospital to primary care settings as perceived by frontline primary care staff within a defined urban area providing policymakers with tangible targets for future improvement strategies. Patients who are older and frail with complex medical problems taking >5 medications were identified as especially vulnerable during this transition, and anticoagulants were identified as the single medication group posing the greatest risk to patients.
This study exposed how the most important threats to safe transitions from hospitals to primary care are underpinned by behaviours of the healthcare professionals involved. All participating practices agreed that poor quality of handover instructions from secondary to primary care teams is a very important threat to safe patient transitions, citing many examples of how inadequate handover communication has put their patients in actual, or at risk of, harm. Though it can be seen that many of these examples depend on behaviours of individual healthcare professionals, it is currently unknown which specific professionals and behaviours underpin these threats. For example, sending incomplete discharge summaries, which are pivotal in enabling ongoing care following patient transitions from hospital,24–26 may be owing to doctors not completing all the required information in the relevant sections. However, it may also be because nursing and administrative staff hurriedly provide patients and GPs with draft versions when faced with pressures to vacate beds and discharge patients promptly, or limitations in patient management software, which automatically sends existing versions of discharge summaries to patients’ GPs following their departure from hospital, irrespective of completion status. Practices also criticised the quality of the written content of discharge summaries, explanations for which could include limited clinical experience of the junior doctors who write them7,8 and low prioritisation of the task by junior and senior doctors alike. Organisational and environmental factors may also contribute to poor-quality summaries; for example, regular workforce changes resulting in doctors’ lack of familiarity with local policies, or rotas with more frequent handovers threatening continuity of care.10 Such potential explanations are in part supported by Coit and colleagues who found that reducing junior doctors’ workloads significantly improved the quality and completeness of discharge summaries.27 This study’s findings have illustrated the multifaceted, complex nature of problems related to discharge communication, adding granularity to existing research13 by identifying which specific aspects of this broad problem PCPs feel threaten their patients’ safety. The findings also support the need to understand this threat from a behavioural perspective to enable the design and implementation of effective intervention strategies.
A very strong consensus (97%) was reached in round 2 that patients who are older and frail are especially at risk of harm during transitions from hospital to primary care, which is perhaps unsurprising given this cohort is well known to be vulnerable across all aspects of health care.28–32 Furthermore, the second highest-ranking threat to safe patient transitions identified in this study was patients being discharged before arrangements for care were in place at home or in the community. Such care arrangements are most likely to be required by an increasing ageing population, compounding their vulnerability further.33 This study also identified that patients with complex medical problems taking >5 medications were particularly at risk (80%). Incomplete medication reconciliation during patient transitions, recently found to be the top scoring medication-related problem in primary care in London,34 and polypharmacy are known risk factors for hospital readmission,35,36 and patients with higher numbers of comorbidities are known to have more medication discrepancies at discharge.37 Interventions that have shown most success in reducing readmission rates and healthcare utilisation costs have targeted such high-risk patients.38,39 The present findings therefore strengthen the case to focus efforts on these cohorts of patients, including prioritisation of social and community services, when planning transitional care improvement strategies.
Anticoagulants were the group of medications considered to pose the greatest risk to patient transitions from hospitals to primary care (consensus 77%). This is in line with previous studies that estimate that anticoagulants are one of the most common drug groups involved in emergency admissions related to adverse drug events in the US.35,37,40,41 Interventions, such as improving patient education, to optimise safety of patients being discharged on anticoagulants have been shown to significantly reduce hospital readmission rates for anticoagulant events,36 making these patients another worthwhile target for policymakers and intervention designers.
The threat ‘Poor engagement with primary care services in patient discharge planning’ failed to reach consensus regarding its level of importance for patient safety among participating practices. Despite its mean score (mean 7.23) placing it within the ‘very important’ category (67% consensus), practices’ views on this problem were relatively polarised. Although some practices were content with existing communication with hospital teams, others expressed that engagement with PCPs was virtually non-existent and endangered safe patient care. Practices also disagreed regarding desired levels of engagement. Some felt that written communication containing clear instructions for primary care teams was sufficient, whereas others sought invitations to hospital multidisciplinary team meetings, either in person or via teleconference. Further work should therefore determine the nature and level of engagement that primary care and hospital teams would find mutually beneficial before focusing efforts in areas where discrepancies exists.
Participants also did not reach consensus on which patients in the social factors category were the most vulnerable, though people who were non-English speakers, ethnic minorities, and refugees received the most votes (43%). This lack of consensus may partly reflect the ethnic and social diversity present within urban areas such as London.42 However, the high proportion of votes held by this cohort echoes the region’s relatively large BAME population,23 indicating that, at least in some areas, due consideration should be afforded to these patients when planning improvement strategies.
Strengths and limitations
This study has several strengths, including a sample size representing approximately 10% of practices in NW London, covering a population of over 310 000 patients, with a relatively low attrition rate (23%). Another strength was the multidisciplinary input to the responses. To the best of the authors’ knowledge, this is the first Delphi study to engage whole practices, involving both clinical and non-clinical staff, providing a holistic overview of challenges related to transitions from hospital to primary care.
The findings of this study must also be considered in the context of its limitations. Following feedback from subject matter experts and piloting of the round 1 questionnaire, a few examples for each category were included to facilitate practices’ understanding of the free-text questions. These examples of problems that put patients at risk during transitions of care from hospital to primary care settings were identified from the literature review. The authors acknowledge the potential for bias as practices’ responses may have been influenced by the examples provided. The data collected reflect responses from practices that agreed to participate in this study. As such the data may represent practices that are more engaged and motivated regarding patient safety compared with those practices that were invited to participate and did not respond. Furthermore, there is potential for additional response bias from the 44% non-response rate of those practices that did sign up to participate in the study. Although practices were instructed to discuss the questionnaire together as an interprofessional team, adherence to this was not investigated and the level of input from different professional groups to the questionnaire is unknown. It is possible that the hierarchical nature of healthcare teams may limit the input from non-clinical staff working in such environments. Given the working patterns and limited resources in primary care, the study was designed to enable practices to complete questionnaires at a time suitable for them, making it unfeasible for the study team to monitor the individual contributors to each round within practices.
The level of granularity and specificity achieved in this study was only possible through targeting a specific geographical area, which has limited the generalisability of the present findings beyond urban areas with similar population demographics and disease burdens, though questions on individual practice patient demographics were not included in order to decrease participant burden. Future studies should repeat this work in other regions to understand how population demographics may influence practice perceptions of threats to safe patient transitions and to improve policymakers’ understanding of national variation.
Comparison with existing literature
Despite ample research into transitions of care over the last decade,1,13,16,17,43,44 many interventions developed to improve handover between hospital and primary care have had variable results in practice.16,17 This study highlights the significance of ongoing problems in interprofessional communication, which, despite advances in technology, remain an important barrier to safe patient transitions. Interventions directly targeting healthcare providers’ behaviours surrounding patient transitions remain scarce despite increasing evidence that organisational culture and professional attitudes are key factors in improving patient safety.16,17 Additionally, many studies show limited evidence of how behavioural and environmental contexts in which developed interventions are expected to work have been considered in their design.18,19,45
Implications for research
Although this study has identified real and relevant threats to safe patient transitions from hospital to community settings, further work must explore why these threats arise, and include a secondary care perspective. A combination of ethnographic and one-to-one interview methodologies would provide an in-depth knowledge and understanding of the environmental, behavioural, and social contexts in which these threats arise. The knowledge obtained would enable the design of future interventions with the most appropriate behaviour change components and techniques for the relevant social and environmental contexts, producing the greatest impact on behaviours promoting safer transitions of care.
Acknowledgments
The authors would like to thank Stephen Campbell and Robbie Foy for their helpful comments on the study protocol and questionnaires.
Funding
This article is independent research funded by the National Institute for Health Research (NIHR) Imperial Biomedical Research Centre (grant number: 1215-20013) and the NIHR Imperial Patient Safety Translational Research Centre (grant number: PSTRC_2016_004). This study was also supported by the Primary Care team at the NIHR Clinical Research Network, North West London. The views expressed in this publication are those of the authors and not necessarily those of the NHS, NIHR, or Department of Health and Social Care.
Ethical approval
This study did not require approval from an NHS ethics committee. Approval was granted by the NHS Health Research Authority (reference number: 19/HRA/0079). One named practice representative provided informed consent to participate on behalf of each practice.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004;170(3):345–349. [PMC free article] [PubMed] [Google Scholar]
- 2.Cheah LP, Amott DH, Pollard J, Watters DA. Electronic medical handover: towards safer medical care. Med J Aust. 2005;183(7):369–372. doi: 10.5694/j.1326-5377.2005.tb07086.x. [DOI] [PubMed] [Google Scholar]
- 3.Simpson KR. Handling handoffs safely. MCN Am J Matern Child Nurs. 2005;30(2):152. doi: 10.1097/00005721-200503000-00030. [DOI] [PubMed] [Google Scholar]
- 4.Kostopoulou O, Delaney B. Confidential reporting of patient safety events in primary care: results from a multilevel classification of cognitive and system factors. Qual Saf Health Care. 2007;16(2):95–100. doi: 10.1136/qshc.2006.020909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clare J, Hofmeyer A. Discharge planning and continuity of care for aged people: indicators of satisfaction and implications for practice. Aust J Adv Nurs. 1998;16(1):7–13. [PubMed] [Google Scholar]
- 6.World Health Organization (WHO) Transitions of care: technical series on safer primary care. Geneva: WHO; 2016. https://apps.who.int/iris/bitstream/handle/10665/252272/9789241511599-eng.pdf;jsessionid=148122112375B910ECA2FB042508F2C0?sequence=1 (accessed 29 Nov 2019) [Google Scholar]
- 7.Abdel-Qader DH, Harper L, Cantrill JA, Tully MP. Pharmacists’ interventions in prescribing errors at hospital discharge. Drug Saf. 2010;33(11):1027–1044. doi: 10.2165/11538310-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Yemm R, Bhattacharya D, Wright D, Poland F. What constitutes a high quality discharge summary? A comparison between the views of secondary and primary care doctors. Int J Med Educ. 2014;5:125. doi: 10.5116/ijme.538b.3c2e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.UK Foundation Programme 2018. http://www.foundationprogramme.nhs.uk/content/foundation-training (accessed 29 Nov 2019)
- 10.Lambert TW, Smith F, Goldacre MJ. The impact of the European Working Time Directive 10 years on: views of the UK medical graduates of 2002 surveyed in 2013–2014. JRSM Open. 2016;7(3) doi: 10.1177/2054270416632703. 2054270416632703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baird B, Reeve H, Ross S, et al. Innovative models of general practice. 2018. https://www.kingsfund.org.uk/sites/default/files/2018-06/Innovative_models_GP_Kings_Fund_June_2018.pdf (accessed 29 Nov 2019)
- 12.MacKichan F, Brangan E, Wye L, et al. Why do patients seek primary medical care in emergency departments? An ethnographic exploration of access to general practice. BMJ Open. 2017;7(4):e013816. doi: 10.1136/bmjopen-2016-013816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams H, Edwards A, Hibbert P, et al. Harms from discharge to primary care: mixed methods analysis of incident reports. Br J Gen Pract. 2015. [DOI] [PMC free article] [PubMed]
- 14.Donaldson LJ, Kelley ET, Dhingra-Kumar N, et al. Medication without harm: WHO’s third global patient safety challenge. Lancet. 2017;389(10080):1680–1681. doi: 10.1016/S0140-6736(17)31047-4. [DOI] [PubMed] [Google Scholar]
- 15.Carson-Stevens A, Hibbert P, Williams H, et al. Characterising the nature of primary care patient safety incident reports in the England and Wales National Reporting and Learning System: a mixed-methods agenda-setting study for general practice. Health Serv Deliv Res. 2016;4(27) [PubMed] [Google Scholar]
- 16.Hesselink G, Schoonhoven L, Barach P, et al. Improving patient handovers from hospital to primary care. Ann Intern Med. 2012;157(6):417–428. doi: 10.7326/0003-4819-157-6-201209180-00006. [DOI] [PubMed] [Google Scholar]
- 17.Hesselink G, Zegers M, Vernooij-Dassen M, et al. Improving patient discharge and reducing hospital readmissions by using Intervention Mapping. BMC Health Serv Res. 2014;14(1):389. doi: 10.1186/1472-6963-14-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Bokhoven M, Kok G, Van der Weijden T. Designing a quality improvement intervention: a systematic approach. Qual Saf Health Care. 2003;12(3):215–220. doi: 10.1136/qhc.12.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baker R, Camosso-Stefinovic J, Gillies C, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2010;(3):CD005470. doi: 10.1002/14651858.CD005470.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311(7001):376. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization Patient safety. https://www.who.int/patientsafety/about/en/ (accessed 29 Nov 2019)
- 22.National Institute for Health Research About the CRN North West London. https://local.nihr.ac.uk/lcrn/north-west-london/about-us.htm (accessed 29 Nov 2019)
- 23.NHS North West London Collaboration of Clinical Commissioning Groups Healthier North West London. https://www.healthiernorthwestlondon.nhs.uk/about/about (accessed 29 Nov 2019)
- 24.van Walraven C, Rokosh E. What is necessary for high-quality discharge summaries? Am J Med Qual. 1999;14(4):160–169. doi: 10.1177/106286069901400403. [DOI] [PubMed] [Google Scholar]
- 25.Adams D, Bristol J, Poskitt K. Surgical discharge summaries: improving the record. Ann R Coll Surg Engl. 1993;75(2):96–99. [PMC free article] [PubMed] [Google Scholar]
- 26.Scottish Intercollegiate Guidelines Network . The immediate discharge document. Edinburgh: SIGN; 2003. [Google Scholar]
- 27.Coit MH, Katz JT, McMahon GT. The effect of workload reduction on the quality of residents’ discharge summaries. J Gen Intern Med. 2011;26(1):28–32. doi: 10.1007/s11606-010-1465-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee L, Heckman G, Molnar FJ. Frailty: identifying elderly patients at high risk of poor outcomes. Can Fam Physician. 2015;61(3):227–231. [PMC free article] [PubMed] [Google Scholar]
- 29.Bagshaw SM, Stelfox HT, McDermid RC, et al. Association between frailty and short- and long-term outcomes among critically ill patients: a multicentre prospective cohort study. CMAJ. 2014;186(2):E95–E102. doi: 10.1503/cmaj.130639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210(6):901–908. doi: 10.1016/j.jamcollsurg.2010.01.028. [DOI] [PubMed] [Google Scholar]
- 31.Martin FC, Brighton P. Frailty: different tools for different purposes? Age Ageing. 2008;37(2):129–131. doi: 10.1093/ageing/afn011. [DOI] [PubMed] [Google Scholar]
- 32.Shamliyan T, Talley KM, Ramakrishnan R, Kane RL. Association of frailty with survival: a systematic literature review. Ageing Res Rev. 2013;12(2):719–736. doi: 10.1016/j.arr.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 33.Humphries R, Thorlby R, Holder H, et al. Social care for older people: home truths. 2016 https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/Social_care_older_people_Kings_Fund_Sep_2016.pdf (accessed 29 Nov 2019) [Google Scholar]
- 34.Car LT, Papachristou N, Gallagher J, et al. Identification of priorities for improvement of medication safety in primary care: a PRIORITIZE study. BMC Fam Pract. 2016;17(1):160. doi: 10.1186/s12875-016-0552-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med. 2011;365(21):2002–2012. doi: 10.1056/NEJMsa1103053. [DOI] [PubMed] [Google Scholar]
- 36.Wilhelm SM, Petrovitch EA. Implementation of an inpatient anticoagulation teaching service: expanding the role of pharmacy students and residents in patient education. Am J Health Syst Pharm. 2011;68(21):2086–2093. doi: 10.2146/ajhp100658. [DOI] [PubMed] [Google Scholar]
- 37.Hafner JW, Jr, Belknap SM, Squillante MD, Bucheit KA. Adverse drug events in emergency department patients. Ann Emerg Med. 2002;39(3):258–267. doi: 10.1067/mem.2002.121401. [DOI] [PubMed] [Google Scholar]
- 38.Kwan JL, Lo L, Sampson M, Shojania KG. Medication reconciliation during transitions of care as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):397–403. doi: 10.7326/0003-4819-158-5-201303051-00006. [DOI] [PubMed] [Google Scholar]
- 39.Mueller SK, Sponsler KC, Kripalani S, Schnipper JL. Hospital-based medication reconciliation practices: a systematic review. Ann Intern Med. 2012;172(14):1057–1069. doi: 10.1001/archinternmed.2012.2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Budnitz DS, Pollock DA, Mendelsohn AB, et al. Emergency department visits for outpatient adverse drug events: demonstration for a national surveillance system. Ann Emerg Med. 2005;45(2):197–206. doi: 10.1016/j.annemergmed.2004.09.020. [DOI] [PubMed] [Google Scholar]
- 41.Shehab N, Sperling LS, Kegler SR, Budnitz DS. National estimates of emergency department visits for hemorrhage-related adverse events from clopidogrel plus aspirin and from warfarin. Arch Intern Med. 2010;170(21):1926–1933. doi: 10.1001/archinternmed.2010.407. [DOI] [PubMed] [Google Scholar]
- 42.Offivce for National Statistics. Regional ethnic diversity 2018. https://www.ethnicity-facts-figures.service.gov.uk/uk-population-by-ethnicity/national-and-regional-populations/regional-ethnic-diversity/latest#main-facts-and-figures (accessed 29 Nov 2019)
- 43.Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–323. doi: 10.1002/jhm.228. [DOI] [PubMed] [Google Scholar]
- 44.Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 45.Michie S, Van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]