Abstract
Background
The prevalence of dental caries and its effect on the oral-health-related quality of life (OHRQoL) of children with special needs (CSNs) have not been established in South Africa.
Aim
The study aimed to assess how caregivers of CSNs who attended Down Syndrome Association outreach sites in Johannesburg, South Africa, perceived the contribution of OHRQoL to the quality of life of these children.
Setting
The study was conducted at Down Syndrome Association (DSA) outreach sites in Johannesburg. These sites cater for children with several types of disabilities including cerebral palsy, hydrocephalus, autism, epilepsy and developmental delays. The association schedules and facilitates support group meetings for the caregivers of children with Down syndrome and other disabilities. These meetings are held at the outreach sites that are located at different district hospitals and community health centres in Johannesburg and are co-facilitated by the association’s outreach coordinator together with a team of physiotherapists, occupational therapists and speech therapists.
Methods
This cross-sectional study was composed of a convenient sample of 150 caregiver and child pairs from five outreach sites during January – June 2015. The short-form Parent-Caregiver Perception Questionnaire (P-CPQ) was used. The caries status of the children was assessed using the decayed, missing and filled teeth (dmft/DMFT) indices (whereby dmft or DMFT stands for decayed missing filled teeth in primary dentition [dmft] and in permanent dentition [DMFT]) based on World Health Organization guidelines.
Results
The mean age of the caregivers was 39.52 years (standard deviation [SD] 9.26) and 8.72 years (SD 6.07) for the children. The mean P-CPQ score was 12.88 (SD 12.14). All the caregivers stated that dental caries had a negative impact on the OHRQoL of the CSNs. However, 60% of caregivers stated that an oral condition had no impact on the child’s overall well-being. The majority (56.7%) of the caregivers rated their children’s overall oral health status as average and only 12% reported the oral health status to be poor. There was a high prevalence of untreated caries among the CSNs regardless of the type of disability.
Conclusion
All the caregivers stated that dental caries had a negative impact on the OHRQoL of the CSNs. However, they appeared to have contradictory perceptions of the oral health needs or status of their children.
Keywords: Oral-health-related quality of life, Dental caries status, Caregiver perception, Children with special needs, Oral health
Introduction
Over a billion people (15% of the world’s population) are estimated to live with some form of disability and this percentage is on the increase (WHO 2014). In South Africa, about 7.5% of the population is regarded as having disabilities with the lowest prevalence (5%) reported in Gauteng province (STATSSA 2014). Studies show that the prevalence of disabilities is higher among women (8.3%) than men (6.5%). About 2.1 million children in South Africa (11.2% of the total child population) are categorised as children with disabilities that is children with special needs (CSNs). Of the total child population with special needs, 28% is in the 0–4-year-old group and 10% is in the 5–9-year-old group (STATSSA 2014).
Children with special needs are the neglected segment of the population in terms of access to services like education and health. However, there is no up-to-date data in South Africa about their general health status and the use of health services (UNICEF 2012). Current data show that attendance at early childhood development centres or schools among children aged 5–6 years with disabilities is lower than for those without disabilities (STATSSA 2014) and children with disabilities have poor access to oral health care services.
Limitations such as motor, sensory and intellectual disabilities lead to CSNs having difficulties in maintaining oral health and communicating their oral health needs. As a result, they depend on their caregivers for general care including oral hygiene (Oredugba & Akindayomi 2008). Studies have reported that caregivers of CSNs also face an increased burden because of the demands of taking care of their children. In some instances, the huge burden related to the general health concerns of these children often results in the neglect of their oral health as this is not regarded as a priority (Lewis et al. 2015).
Oral-health-related quality of life (OHRQoL) is defined as:
The impact of oral diseases and disorders on aspects of everyday life that a patient or person values, that are of sufficient magnitude, in terms of frequency, severity or duration to affect their experience and perception of their life overall. (Locker & Allen 2007:409)
Evidence has shown that untreated caries is higher in CSNs (Nqcobo et al. 2012). Given that untreated dental caries can lead to difficulty with eating, speech, pain, sleep disturbances and missed days at school (Sheiham, Conway & Chestnutt 2015), it may contribute to poorer OHRQoL outcomes (Cushing, Sheiham & Maizels 1986).
The caregivers’ perceptions of children’s oral health status and OHRQoL influence their oral health-care-seeking behaviour and motivates them to access oral health services (Pradhan 2013; Vann et al. 2010). Caregiver perception of their children’s oral health is often used as a proxy measure (Baghdadi 2014; Pani et al. 2013) of the child’s OHRQoL. A range of factors such as caregivers’ gender, monthly family income, mother’s education, family structure and increased caregiver stress have an impact on the caregiver’s perception of the OHRQoL (Baghdadi 2014; Cushing et al. 1986; Pani et al. 2013)
The OHRQoL outcomes of CSNs in Johannesburg have not been established in the literature. The aim of this study was therefore to assess the OHRQoL outcomes because of dental caries rate among CSNs.
Research methods and design
Study setting
The study was conducted at Down Syndrome Association (DSA) outreach sites in Johannesburg. These sites cater for children with several types of disabilities including cerebral palsy, hydrocephalus, autism, epilepsy and developmental delays. The association schedules and facilitates support group meetings for the caregivers of children with Down syndrome and other disabilities. These meetings are held at the outreach sites that are located at different district hospitals and community health centres in Johannesburg, and are co-facilitated by the association’s outreach coordinator together with a team of physiotherapists, occupational therapists and speech therapists.
Study design, study population and sample
This cross-sectional study consisted of a convenient sample of caregiver and child pairs. Caregivers were defined as ‘all the parents, legal guardian or relatives’ who attend to the needs of a dependent child with special needs (Family Caregiver Alliance 2012). The participants were recruited between January and May 2015 from the DSA support groups, and from a special needs school in Johannesburg.
The DSA in Johannesburg has outreach sites which cater for children with several types of disabilities including cerebral palsy, hydrocephalus, autism, epilepsy and developmental delays. The association schedules and facilitates support group meetings for the caregivers of children with Down syndrome and other disabilities. These meetings are held at the outreach sites that are located at different district hospitals and community health centres in Johannesburg, and are co-facilitated by the association’s outreach coordinator together with a team of physiotherapists, occupational therapists and speech therapists. During the group meetings, the caregivers have facilitated group discussions and peer group education sessions wherein several topics are discussed, for example, caring for a child with Down syndrome and other disabilities and how to stimulate children with disabilities, developmental milestones, diet, oral health care, speech development and support, occupational health as well as social grant support issues and challenges, and so on. All the caregivers attending the support group meetings were invited to participate in the study and their children were also enrolled in the study.
At the end of a 4-month period of data collection, only 37% of the sample was collected as a result, a decision was made to purposively recruit the caregivers from a special needs school in Johannesburg which was visited by the department outreach team at the time of data collection. The researchers attended the school open day where parents were invited to participate in the study. The parents gave consent to have their children participate in the study and have an oral examination during school days. The children’s clinical assessment form and the parent or caregivers questionnaires were matched and identifiers were kept confidential so that participants were not identifiable to persons not involved in the study.’ According to the STATA 12 statistical sample size calculator, the sample size was calculated to be 150 caregiver–child pairs including the 20 attrition effect and the variables used were alpha of 0.05 and 80% power.
Data collection and study instrument
This study used the validated short-form Parent-Caregiver Perception Questionnaire (P-CPQ) (Thomson et al. 2013) which aims to assess parental perceptions of their children’s OHRQoL. The questionnaire consisted of 16 closed-ended questions grouped into four subscales or domains: oral symptoms (OS), functional limitations (FLs), emotional well-being (EW) and social well-being (SWB) domains. The questionnaires were administered by a trained interviewer who explained and gave clarifications to the caregivers. Training was essential to ensure the uniformity of the questioning by reducing interviewer error. The questionnaire was piloted at a site that was not included in the study. The caregivers also answered two questions that were related to the child’s OHRQoL global rating score. This score summarises how the caregivers perceive the children’s OHRQoL using two questions and is often used to test for construct validity. The first question asks the caregivers to rate their children’s overall oral health status (health of the teeth, lips, jaws and mouth) using a five-point Likert scale and the response options are from ‘excellent’ to ‘poor’. The second question focuses on how the overall well-being of the child is affected by the oral health status using a Likert scale ranging from ‘not at all’ to ‘very much’ (Jokovic, Locker & Guyatt 2005). When the global rating score correlates well with the perceived quality of life score, it indicates that the OHRQoL perception score is valid.
Clinical examination of the children
Dental caries was measured using the decayed, missing and filled teeth (dmft or DMFT) indices whereby dmft or DMFT stands for decayed missing filled teeth in primary dentition (dmft) and in permanent dentition (DMFT). Two calibrated examiners conducted the clinical examination. Inter- and intra-examiner reliability scores were assessed using the Cohen Kappa scores which were found to be 0.9 for diagnosis of dental caries. The children were examined on site under natural light, using a mouth mirror, in a seated position according to the modified World Health Organization guidelines (WHO 2013). The assessment form was used to record dmft or DMFT data and to collect information on the socio-demographic status of the child and the caregiver.
Data analysis
Data from the questionnaires were captured into Microsoft Excel and analysed using the Statistical Package for Social Sciences (SPSS) version 16. The independent variables were the demographic variables (caregiver age and gender), socio-economic condition (household income, caregiver’s education level and employment status) and clinical status (prevalence of untreated dental caries and dmft or DMFT scores). The dependent variable was the OHRQoL outcomes as determined by the P-CPQ total overall and domain scores. The scores were calculated from a five-point Likert scale and all the scores in each domain were added separately to give a domain score. The sum of the four domain scores made up the total P-CPQ score for each child. The scores ranged from 0 to 64 and the lower scores represented a high OHRQoL.
Descriptive statistics was used to describe the demographic profile of the caregiver–child pairs using means, standard deviations, frequency and ranges of the total and domain scores. T-test, Mann–Whitney and one-way analysis of variance (ANOVA) tests were carried out to assess the group differences between means and the Games–Howell post-hoc tests were also used to identify group differences. The statistical significance level was set at p < 0.05 and estimates were reported at the 95% confidence interval.
Ethical considerations
Permission to undertake the study was granted by the University of Witwatersrand Ethics Committee (Ethics Clearance Certificate number M140438), the Department of Education and the Downs Syndrome Association Johannesburg branch. Informed consent was obtained from all individual caregivers included in the study. The caregiver of each participant was given an information sheet and a written consent form for obtaining their permission to allow their children to participate in the study which they had to sign.
Results
Demographics
The study consisted of 150 caregiver and child pairs and the profile of the study participants is shown in Table 1. The mean age of the caregivers was 39.5 years (standard deviation [SD] 9.26) and 94.7% of the caregivers were women. Of these female caregivers, 87% were mothers to the children. The mean age of the children was 8.72 years (SD 6.07) and men were the predominant gender (59.30%). The majority of the caregivers (48%) had secondary education and 52.70% of them were employed. Analysis of source of income indicated that the majority of the caregivers (64.0%) earned a salary, while 27.30% received a monthly care dependency grant (a grant which a primary care giver applies for on behalf of a child who needs permanent care because of disability). Only 8% of the caregivers received a child support grant, that is, a grant that can be applied for by needy caregivers to help support the care of a child irrespective of health status (Table 1).
TABLE 1.
Frequency and percentage of caregivers by socio-demographic characteristics.
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
| Caregiver gender | 150 | 100 |
| Female | 142 | 94.7 |
| Male | 8 | 5.3 |
| Child gender | 150 | 100 |
| Female | 61 | 40.70 |
| Male | 89 | 59.30 |
| Level of education | 150 | 100 |
| No schooling | 2 | 1.30 |
| Primary (Grades 1–7) | 14 | 9.30 |
| High school (Grades 8–12) | 72 | 48.00 |
| College | 34 | 22.70 |
| University | 25 | 16.70 |
| Others | 3 | 2.00 |
| Employment status | 150 | 100 |
| Not employed | 60 | 40.00 |
| Employed | 79 | 52.70 |
| Self employed | 5 | 3.30 |
| Other | 6 | 4.00 |
| Source of income | 150 | 100 |
| Salary | 96 | 64.00 |
| Care dependency grant | 41 | 27.30 |
| Pension grant | 1 | 0.70 |
| Child grant | 12 | 8.00 |
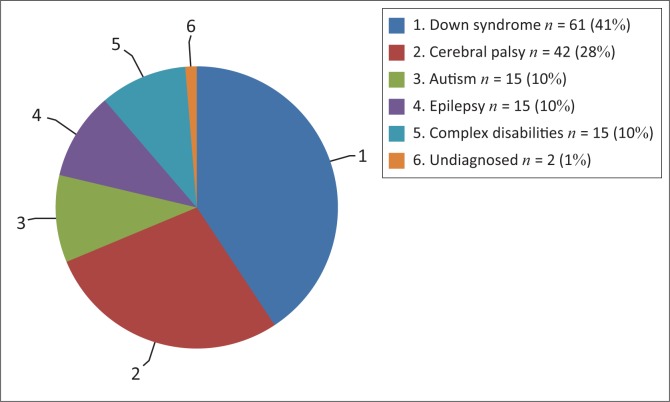
Figure 1 provides information about the distribution of the child participants according to type of disability. The majority of the children had Down syndrome (41%), while 10% of the children had disabilities which are grouped as complex disabilities. These include conditions like myotonic dystrophy (n = 5), severe physical disability (n = 6) and syndromes such as Noonan syndrome (n = 2) and Cornelia de Lange syndrome (n = 2).
FIGURE 1.
Number and percentage of children by type of disability.
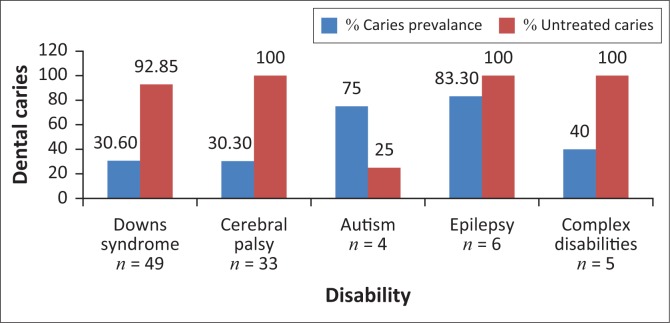
Dental caries status
The overall caries prevalence was 42% and the dmft score was found to be 1.45 (SD 2.58). Figure 2 provides information on the caries prevalence and untreated caries in the primary dentition of the participants in each of the disabilities. The highest caries prevalence was found in the epilepsy (83.3%) and the autism groups (75%) compared to Down syndrome and cerebral palsy. The untreated caries remained high (93% – 100%) across all the disabilities regardless of caries prevalence and disability.
FIGURE 2.
Dental caries prevalence and untreated caries in primary dentition by disability.
Oral health relate quality of life
The data for the OHRQoL are reported based on the overall as well as domain scores of the P-CPQ as indicated in Table 2. The majority of the caregivers (91%) indicated that oral conditions had a negative impact on the OHRQoL (P-CPQ > 0). The overall mean P-CPQ score was relatively lower (12.88 SD 12.14) as it ranged from 0 to 44. High scores were found in all the domains except the SWB domain (2 SD 3.0). There was no significant difference in the mean P-CPQ scores among the different disabilities.
TABLE 2.
Mean, standard deviations, ranges of domains and total parent-caregiver perception (Parent-Caregiver Perception Questionnaire) scores.
| Domains and overall P-CPQ scores | Mean | SD | Expected range | Observed range |
|---|---|---|---|---|
| Oral symptoms | 4.62 | 3.91 | 0–16 | 0–16 |
| Functional limitations | 4.38 | 4.06 | 0–16 | 0–14 |
| Emotional well-being | 3.95 | 4.02 | 0–16 | 0–16 |
| Social well-being | 2.23 | 3.00 | 0–16 | 0–11 |
| P-CPQ | 12.88 | 12.14 | 0–64 | 0–44 |
P-CPQ, Parent-Caregiver Perception Questionnaire; SD, standard deviation.
Tables 3 and 4 show that there were significant differences in the domain scores of OS, functional limitation domain as well as the overall OHRQoL between those individuals with dental caries and those without caries in primary dentition. Those with dental caries expressed a higher negative impact on their quality of life, whereas those with caries in the permanent dentition only expressed a greater negative impact on the OS domain compared to those with a caries-free dentition.
TABLE 3.
Comparison of Parent-Caregiver Perception Questionnaire overall and domain scores and caries status in primary dentitions.
| Domains | Primary dentition | n | Mean score | SD | t | p |
|---|---|---|---|---|---|---|
| Oral symptoms | Caries free | 62 | 3.44 | 3.37 | −2.35 | 0.021* |
| Caries present | 35 | 5.14 | 3.57 | |||
| Functional limitation | Caries free | 62 | 2.90 | 3.46 | −2.27 | 0.025* |
| Caries present | 35 | 4.66 | 3.96 | |||
| Emotional well-being | Caries free | 62 | 2.65 | 3.97 | −0.37 | 0.715 |
| Caries present | 35 | 2.94 | 3.60 | |||
| Social well-being | Caries free | 61 | 1.05 | 2.50 | −1.15 | 0.253 |
| Caries present | 35 | 1.63 | 2.14 | |||
| P- CPQ score | Caries free | 61 | 9.82 | 10.40 | −2.13 | 0.035* |
| Caries present | 35 | 14.37 | 9.42 |
P-CPQ, Parent-Caregiver Perception Questionnaire; SD, standard deviation.
, Significant p value.
TABLE 4.
Comparison of Parent-Caregiver Perception Questionnaire overall and domain scores and caries status in permanent dentitions.
| Domains | Permanent dentition | n | Mean | SD | t | p |
|---|---|---|---|---|---|---|
| Oral symptoms | Caries free | 30 | 3.17 | 2.63 | −2.29 | 0.026* |
| Caries present | 38 | 5.05 | 3.87 | |||
| Functional limitation | Caries free | 30 | 3.33 | 3.17 | −1.39 | 0.169 |
| Caries present | 38 | 4.55 | 3.89 | |||
| Emotional well-being | Caries free | 30 | 3.27 | 2.95 | −1.12 | 0.267 |
| Caries present | 38 | 4.26 | 4.11 | |||
| Social well-being | Caries free | 30 | 2.67 | 2.94 | 1.76 | 0.083 |
| Caries present | 37 | 1.57 | 2.17 | |||
| P- CPQ score | Caries free | 30 | 12.43 | 8.19 | −1.26 | 0.212 |
| Caries present | 37 | 15.22 | 9.57 |
P-CPQ, Parent-Caregiver Perception Questionnaire; SD, standard deviation.
, Significant p value.
Spearman Rho correlation coefficient was used to measure the extent of the association between dental caries and P-CPQ and global rating scores and the results are displayed in Table 5. The number of teeth affected by dental caries in the primary dentition was significantly correlated with OS, FL and SWB domains. However, the strength of the association was mild (ρ coefficient ranged between 0.23 and 0.25). Furthermore, the number of teeth affected by dental caries was also found to be moderately correlated with the global rating score and the overall oral health rating (ρ = 0.349; p = 0.005).
TABLE 5.
Correlation between decayed, missing and filled teeth, global rating scores and total Parent-Caregiver Perception Questionnaire scores.
| Variable | dmft |
DMFT |
||
|---|---|---|---|---|
| ρ** | p | ρ** | p | |
| Oral symptoms | 0.246 | 0.034* | 0.051 | 0.793 |
| Functional limitation | 0.231 | 0.041* | −0.091 | 0.511 |
| Emotional well-being | 0.078 | 0.494 | 0.054 | 0.692 |
| Social well-being | 0.252 | 0.038* | −0.24 | 0.103 |
| P-CPQ | 0.154 | 0.273 | -0.256 | 0.261 |
| Global rating-oral health | 0.349 | 0.005* | 0.349 | 0* |
| Global rating-overall well-being | 0.02 | 0.84 | 0.117 | 0.339 |
, Spearman’s correlation coefficient;
, significant at p < 0.05.
dmft or DMFT, decayed, missing and filled teeth; P-CPQ, Parent-Caregiver Perception Questionnaire.
Bold text indicate the correlation between overall P-CPQ score and dental caries.
Caregivers’ perceptions
When the caregivers were asked to comment on the effect of any oral condition on the overall well-being of the child, 60.7% (n = 91) caregivers reported that their children’s overall well-being was not affected by the oral conditions. The majority (56.7%) of the caregivers rated the children’s overall oral health status as average and only 12% rated it to be poor.
Spearman’s correlation coefficient was also used to assess construct validity of the study instrument (questionnaire). There was a strong correlation between the P-CPQ scores and the global rating of overall well-being scores (ρ = 0.56; p ≤ 0.001) and global rating of oral health score (ρ = 0.653; p < 0.001), respectively.
The impact of the socio-demographic factors of the caregiver, the caries status of the children and P-CPQ scores was evaluated using the linear regression model. The dependent variables were added into the equation in a stepwise form. The results displayed in Table 6 showed that there was no significant relationship between all the variables that were entered into the regression model and the P-CPQ scores.
TABLE 6.
Linear regression of socio-demographic variables of the caregiver, decayed, missing and filled teeth of the children and Parent-Caregiver Perception Questionnaire.
| Model | Variables | B | s.e. | t | p | Confidence interval |
|
|---|---|---|---|---|---|---|---|
| Low | Upper | ||||||
| - | (Constant) | −1.46 | 17.78 | −0.08 | 0.94 | −43.5 | 40.57 |
| 1 | Caregiver age group | 0.52 | 3.27 | 0.16 | 0.88 | −7.21 | 8.26 |
| 2 | Relationship | −3.99 | 4.17 | −0.96 | 0.37 | −13.85 | 5.87 |
| 3 | Disability | 1.1 | 2.13 | 0.52 | 0.62 | −3.93 | 6.13 |
| 4 | Level of education | 8.4 | 4.47 | 1.88 | 0.10 | −2.17 | 18.98 |
| 5 | Employment | −5.48 | 4 | −1.37 | 0.21 | −14.94 | 3.98 |
| 6 | dmft | −0.4 | 1.08 | −0.37 | 0.72 | −2.96 | 2.16 |
| 7 | DMFT | 4.81 | 3.50 | 1.38 | 0.21 | −3.47 | 13.09 |
dmft or DMFT, decayed, missing and filled teeth; s.e., standard error.
Discussion
Children with special needs are faced with the daily burden of dealing with the negative impact of their individual disabilities, and more specifically, the effect of these disabilities on oral health. Caregivers in this study were predominantly women and this is consistent with the findings of previous studies on caregivers’ perceptions of OHRQoL (Abanto et al. 2014; Baghdadi & Muhajarine 2014; Kumar, Kroon & Lalloo 2014). The reason for this has been attributed to the worldwide societal norm of women being regarded as primary caregivers (American Psychological Association 2015; Hlabyago & Ogunbanjo 2009). The gender distribution of the child participants favoured males rather than females. A possible reason for the male predominance in the CSNs could be that boys are more genetically predisposed to having one form or another of disability than are girls (Werling & Geschwind 2013).
Caries status
Dental caries is a major public health problem in South Africa. Several reports have shown the prevalence of dental caries to be higher in children with disabilities compared to the general population (Nemutandani et al. 2013; Purohit, Acharya & Bhat 2010; Shyama 2001). Conversely, this current study and an earlier study by Nqcobo et al. (2012) found caries prevalence to be lower in CSNs in Johannesburg. Each child had at least one carious lesion. This is lower than the caries prevalence reported in the general population of South African children which is 60.3% in 6 year olds. Furthermore, this prevalence is lower than those reported by Shukla et al. (2014), in India (76%) and by Abanto et al. (2014), in Brazil (55%). The reason for the lower prevalence in this cohort studied could be that the special needs school had an established daily tooth brushing routine after lunch and the caregivers who attended the outreach sites were already exposed to ongoing oral health education at the outreach sites during support group discussions.
The highest caries prevalence was found in the primary dentition of the epilepsy group (83.30%) followed by the autism group (75%). Similarly, Gurbuz and Tan (2010) found the caries prevalence in children with epilepsy in Turkey to be high (96.7%). The reason for the high prevalence among this group may be as a result of medications which predispose them to gingival hyperplasia and dry mouth (Ghafoor, Rafeeq & Dubey 2014). This, in turn, facilitates plaque retention and ultimately increases the risk for dental caries (Ghafoor et al. 2014). The autism group also had a high caries prevalence in the current study, which is similar to the findings by Jaber et al. (2011). The reason for this high prevalence could be that children with autism have multiple medical and behavioural problems, which make their oral hygiene care extremely difficult (Lewis et al. 2015). It has been reported that children with autism prefer soft and sweetened foods. They also tend to pouch food inside the mouth instead of swallowing it because of poor tongue coordination, thus increasing the susceptibility to caries (Jaber 2011). In this study cohort, caution needs to be exercised when interpreting the high prevalence recorded for epilepsy and autistic groups because of the small sample sizes.
In keeping with other studies (Altun et al. 2010; Purohit et al. 2010), the prevalence of untreated caries among children with disabilities such as Down syndrome, cerebral palsy, epilepsy and other complex disabilities in this study was high. The reason may be because of lack of access to oral health services, long waiting lists for general anaesthesia and caregiver’s perception of oral health care as not being as much a priority as general health problems (Lewis et al. 2015).
Oral-health-related quality of life
The present study showed that all the caregivers of CSNs reported that dental caries had a negative impact on OHRQoL outcomes as measured by P-CPQ scores. This is similar to the studies conducted by Abanto et al. (2012) and Pani et al. (2013) which showed a negative impact of oral diseases on OHRQoL of children with cerebral palsy and autism. All the caregivers, irrespective of the disabilities, reported that OS and FL domains in the primary dentition had an impact on the OHRQoL. This could be because of the consequences of untreated caries which may have progressed into the pulp and periapical tissues resulting in severe pain. The pain resulting from untreated dental caries has an impact on feeding and sleeping which may alert the caregiver to the extent of the pain.
Caregivers’ perceptions
It is important to note that while the caregivers have reported that dental caries had a negative impact on the OHRQoL of CSN, overall well-being of the children was not significantly affected by oral conditions and the children’s overall oral health status was rated to be average. In contrast, Abanto et al. (2012) found that a lower proportion of caregivers rated their children’s oral health as excellent. The reason could be that the overall well-being of the children is mostly perceived by caregivers to be affected by the severity of the disability rather than the oral condition. This highlights the caregivers’ lack of awareness on the importance of oral health for general health. Oral health is not considered to be life-threatening by most population groups. It is also not considered important to overall well-being, especially when oral health diseases co-exist with some debilitating illnesses or disabilities. It is important that policy makers and health educators begin to make concerted efforts to educate the growing population of caregivers on the importance of oral health and the role it plays in general health. Pani et al. (2013) also support this assertion.
Conclusion and recommendations
The caregivers did not perceive oral conditions to affect the overall well-being of the children and this could have been attributed to a lack of awareness of the importance of the contribution oral health to general health. There was a high burden of untreated dental caries and it is thus recommended that caregiver and teacher education on oral health should be expanded in all special needs schools and primary health care centres, especially the maternal and child health centres. This would facilitate early detection of oral diseases and early intervention. Oral health education and promotion, especially designed for individual disabilities, and proven preventive methods such as the use of fissure sealants, are recommend to be implemented in this group of children.
Acknowledgements
The author would like to acknowledge Casa do Sol School staff members, parents, guardians and learners for participating in the study, the Downs Syndrome Association Johannesburg branch for providing access to the sites and participants and the outreach coordinator and Professor Reed for reviewing and editing the drafts of the manuscript.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors’ contributions
C.N. carried out the study as part of her MDent research project and was responsible for all parts of the project and made contributions to conception, design of the research project and drafting of the manuscript. T.R. contributed to the design of the project and manuscript revision. T.E. made substantial contributions with data analysis, interpretation as well as drafting and revision of the manuscript. Y.M.K. and V.Y. supervised the project while critically revising the manuscript for important intellectual content. All authors read and approved the final manuscript.
Funding
This study was funded by the Faculty Research Committee (FRC) individual grant (grant number 00140185111035121105RMCOMD015) through the University of the Witwatersrand Faculty of Health Sciences Research Office.
Data availability statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
Footnotes
How to cite this article: Nqcobo, C., Ralephenya, T., Kolisa, Y.M., Esan, T. & Yengopal, V., 2019, ‘Caregivers’ perceptions of the oral-health-related quality of life of children with special needs in Johannesburg, South Africa’, Health SA Gesondheid 24(0), a1056. https://doi.org/10.4102/hsag.v24i0.1056
References
- Abanto J., Carvalho T.S., Bönecker M., Ortega A.O., Ciamponi A.L. & Raggio D.P, 2012, ‘Parental reports of the oral health-related quality of life of children with cerebral palsy’, BMC Oral Health 12, 15 10.1186/1472-6831-12-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abanto J., Ortega A.O., Raggio D.P., Bönecker M., Mendes F.M. & Ciamponi A.L, 2014, ‘Impact of oral diseases and disorders on oral-health-related quality of life of children with cerebral palsy’, Special Care in Dentistry 34(2), 56–63. 10.1111/scd.12028 [DOI] [PubMed] [Google Scholar]
- Altun C., Guven G., Akgun O.M., Akkurt M.D., Basak F. & Akbulut E, 2010, ‘Oral health status of disabled individuals attending special schools’, European Journal of Dentistry 4(4), 361–366. [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association , 2015, Family caregiving, viewed 12 July 2015, from http://www.apa.org/about/gr/issues/cyf/caregiving-facts.aspx.
- Baghdadi Z.D, 2014, ‘Effects of dental rehabilitation under general anesthesia on children’s oral health-related quality of life using proxy short versions of OHRQoL instruments’, The Scientific World Journal 2014 10.1155/2014/308439 [DOI] [PMC free article] [PubMed]
- Baghdadi Z.D. & Muhajarine N, 2014, ‘Effects of dental rehabilitation under general anesthesia on children’s oral-health-related quality of life: Saudi Arabian parents’ perspectives’, Dentistry Journal 3(1), 1–13. 10.3390/dj3010001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cushing A., Sheiham A. & Maizels J, 1986, ‘Developing socio-dental indicators – The social impact of dental disease’, Community Dental Health 3(1), 3–17. [PubMed] [Google Scholar]
- Family Caregiver Alliance , 2012, Selected caregiver statistics, viewed 20 June 2015, from https://caregiver.org/selected-caregiver-statistics.
- Ghafoor P.A., Rafeeq M. & Dubey A, 2014, ‘Assessment of oral side effects of antiepileptic drugs and traumatic oro-facial injuries encountered in Epileptic children’, Journal of International Oral Health 6(2), 126–128. [PMC free article] [PubMed] [Google Scholar]
- Gurbuz T. & Tan H, 2010, ‘Oral health status in epileptic children’, Pediatrics International 52(2), 279–283. 10.1111/j.1442-200X.2009.02965.x [DOI] [PubMed] [Google Scholar]
- Hlabyago K.E. & Ogunbanjo G.A, 2009, ‘The experiences of family caregivers concerning their care of HIV/AIDS orphans’, South African Family Practice 51(6), 506–511. 10.1080/20786204.2009.10873915 [DOI] [Google Scholar]
- Jaber M.A, 2011, ‘Dental caries experience, oral health status and treatment needs of dental patients with autism’, Journal of Applied Oral Science 19(3), 212–217. 10.1590/S1678-77572011000300006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaber M.A., Sayyab M. & Abu Fanas S.H, 2011, ‘Oral health status and dental needs of autistic children and young adults’, Journal of Investigative and Clinical Dentistry 2(1), 57–62. 10.1111/j.2041-1626.2010.00030.x [DOI] [PubMed] [Google Scholar]
- Jokovic A., Locker D. & Guyatt G, 2005, ‘What do children’s global ratings of oral health and well-being measure?’, Community Dentistry and Oral Epidemiology 33(3), 205–211. 10.1111/j.1600-0528.2005.00210.x [DOI] [PubMed] [Google Scholar]
- Kumar S., Kroon J. & Lalloo R, 2014, ‘A systematic review of the impact of parental socio-economic status and home environment characteristics on children’s oral health related quality of life’, Health and Quality of Life Outcomes 12(1), 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis C., Vigo L., Novak L. & Klein E.J, 2015, ‘Listening to parents: A qualitative look at the dental and oral care experiences of children with Autism spectrum disorder’, Pediatric Dentistry 37(7), E98–E104. [PubMed] [Google Scholar]
- Locker D. & Allen F, 2007, ‘What do measures of “oral health-related quality of life” measure?’, Community Dentistry and Oral Epidemiology 35(6), 401–411. 10.1111/j.1600-0528.2007.00418.x [DOI] [PubMed] [Google Scholar]
- Nemutandani M., Adedoja D. & Nevhuhlwi D, 2013, ‘Dental caries among disabled individuals attending special schools in Vhembe district, South Africa: Research’, South African Dental Journal 68(10), 458–461. [PubMed] [Google Scholar]
- Nqcobo C., Yengopal V., Rudolph M., Thekiso M. & Joosab Z, 2012, ‘Dental caries prevalence in children attending special needs schools in Johannesburg, Gauteng Province, South Africa’, SADJ: Journal of the South African Dental Association 67(7), 308–313. [PubMed] [Google Scholar]
- Oredugba F.A. & Akindayomi Y, 2008, ‘Oral health status and treatment needs of children and young adults attending a day centre for individuals with special health care needs’, BMC Oral Health 8(1), 30 10.1186/1472-6831-8-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pani S.C., Mubaraki S.A., Ahmed Y.T., AlTurki R.Y. & Almahfouz S.F, 2013, ‘Parental perceptions of the oral health-related quality of life of autistic children in Saudi Arabia’, Special Care in Dentistry 33(1), 8–12. 10.1111/j.1754-4505.2012.00294.x [DOI] [PubMed] [Google Scholar]
- Pradhan A, 2013, ‘Oral health impact on quality of life among adults with disabilities: Carer perceptions’, Australian Dental Journal 58(4), 526–530. 10.1111/adj.12124 [DOI] [PubMed] [Google Scholar]
- Purohit B.M., Acharya S. & Bhat M, 2010, ‘Oral health status and treatment needs of children attending special schools in South India: A comparative study’, Special Care in Dentistry 30(6), 235–241. 10.1111/j.1754-4505.2010.00160.x [DOI] [PubMed] [Google Scholar]
- Sheiham A., Conway D. & Chestnutt I, 2015, 1.1 Impact of oral diseases and oral health inequalities. Social inequalities in oral health: From evidence to action, viewed 14 March 2015, from https://media.news.health.ufl.edu/misc/codoralhealth/docs/posts_frontpage/SocialInequalities.pdf#page=4.
- Shukla D., Bablani D., Chowdhry A., Jafri Z., Ahmad N. & Mishra S, 2014, ‘Oral health status and dental caries experience in mentally challenged individuals’, Annals of Public Health and Research 1(2), 1008. [Google Scholar]
- STATSSA , 2014, Profile of persons with disabilities in South Africa Statistics, viewed 12 July 2015, from http://www.statssa.gov.za/?p=3180.
- Shyama M., Al-Mutawa S.A., Morris R.E., Sugathan T. & Honkala E, 2001, ‘Dental caries experience of disabled children and young adults in Kuwait’, Community Dental Health 18(3), 181–186. [PubMed] [Google Scholar]
- Thomson W.M., Foster Page L.A., Gaynor W.N. & Malden P.E, 2013, ‘Short-form versions of the Parental-Caregivers Perceptions Questionnaire and the Family Impact Scale’, Community Dentistry and Oral Epidemiology 41(5), 441–450. 10.1111/cdoe.12036 [DOI] [PubMed] [Google Scholar]
- UNICEF , 2012, Children with disabilities in South Africa: A situation analysis: 2001–2011, C.a.P.w.D.U. Department of Social Development/Department of Women, viewed 12 July 2015, from https://www.unicef.org/southafrica/SAF_resources_sitandisabilityes.pdf. [Google Scholar]
- Vann W., Lee J., Baker D. & Divaris K, 2010, ‘Oral health literacy among female caregivers impact on oral health outcomes in early childhood’, Journal of Dental Research 89(12), 1395–1400. 10.1177/0022034510379601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werling D.M. & Geschwind D.H, 2013, ‘Sex differences in autism spectrum disorders’, Current Opinion in Reurology 26(2), 146 10.1097/WCO.0b013e32835ee548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO , 2013, Oral health surveys: Basic methods, 5th edn., viewed 03 December 2014, from http://www.who.int/oral_health/publications/9789241548649/en/.
- WHO , 2014, Disability and health, viewed 12 July 2015, from http://www.who.int/mediacentre/factsheets/fs352/en/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.