Abstract
Background:
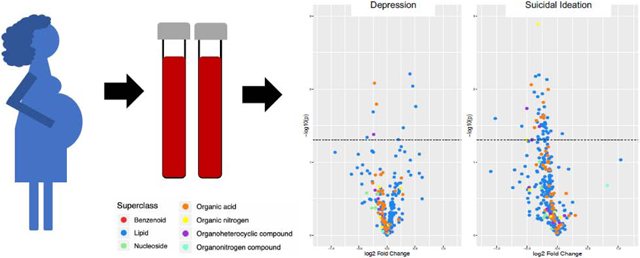
Recent analyses have described metabolomic markers for depression and suicidal ideation in non-pregnant adults. We examined the metabolomic profile of antepartum depression and suicidal ideation during mid-pregnancy, a time of high susceptibility to mood disorders.
Methods:
We collected fasting blood from 100 pregnant Peruvian women and profiled 307 plasma metabolites using liquid chromatography-mass spectrometry. We used the Patient Health Questionnaire 9 to define antepartum depression (score ≥10) and suicidal ideation (having thoughts that you would be better off dead, or of hurting yourself). Logistic regression was used to calculate odds ratios (ORs).
Results:
Three triacylglycerol metabolites (C48:5 triacylglycerol [OR=1.89; 95% confidence interval (CI): 1.14–3.14], C50:6 triacylglycerol [OR=1.88; 95%CI: 1.13–3.14], C46:4 triacylglycerol [OR=1.89; 95%CI: 1.11–3.21]) were associated with higher odds of antepartum depression and 4 metabolites (betaine [OR=0.56; 95%CI:0.33–0.95], citrulline [OR=0.58; 95%CI: 0.34–0.98], C5 carnitine [OR=0.59; 95%CI: 0.36–0.99], C5:1 carnitine [OR=0.59; 95%CI: 0.35–1.00]) with lower odds of antepartum depression. Twenty-six metabolites, including 5-hydroxytryptophan (OR=0.52; 95%CI: 0.30–0.92), phenylalanine (OR=0.41; 95%CI: 0.19–0.91), and betaine (OR=0.53; 95%CI: 0.28–0.99) were associated with lower odds of suicidal ideation.
Limitations:
Our cross-sectional study could not determine whether metabolites prospectively predict outcomes. No metabolites remained significant after multiple testing correction; these novel findings should be replicated in a larger sample.
Conclusions:
Antepartum suicidal ideation metabolomic markers are similar to markers of depression among non-pregnant adults, and distinct from markers of antepartum depression. Findings suggest that mood disorder in pregnancy shares metabolomic similarities to mood disorder at other times and may further understanding of these conditions’ pathophysiology.
Keywords: pregnancy, depression, suicidal ideation, Peru, metabolomics
Graphical Abstract
Introduction
Antepartum depression, a non-psychotic depressive episode of mild to major severity that occurs during pregnancy, affects about 13% of pregnant women in high-income countries (Gavin et al., 2005) and up to 25% in low-middle income countries (Gelaye et al., 2016b). In fact, many women are first diagnosed with depression during pregnancy (Dietz et al., 2007). Antepartum depression may be more common among women with other psychological stressors including low partner support, exposure to violence, low socioeconomic status, and history of depression before becoming pregnant (Biaggi et al., 2016; Lancaster et al., 2010; Leigh and Milgrom, 2008). Antepartum depression may also lead to poorer outcomes for mother and infant, such as an increased risk of preterm birth (Davalos et al., 2012; Eke et al., 2016; Wisner et al., 2009).
Antepartum suicidal ideation is another major determinant of maternal morbidity. Though antepartum depression is a risk factor for antepartum suicidal ideation, antepartum suicidal ideation can also occur among pregnant women without diagnosed antepartum depression (Gelaye et al., 2016a; Zhong et al., 2016). As many as a third of pregnant women report experiencing antepartum suicidal ideation, which greatly increases risk of attempting suicide (Gelaye et al., 2016a). Understanding the pathophysiology of antepartum depression and antepartum suicidal ideation may guide the development of effective and safe treatment of symptoms during pregnancy.
Several studies, primarily conducted in non-pregnant populations, have identified a number of potential plasma metabolites as predictors of depression. The identified metabolites have been associated with a variety of pathways such as neurotransmitter metabolism, energy metabolism, and lipid metabolism. The metabolites identified include several amino acids (e.g., isoleucine, phenylalanine, methionine, tyrosine, glutamine, and tryptophan) as well as creatine, kynurenine, and gamma-aminobutyric acid (Kawamura et al., 2018; Kuwano et al., 2018; Liu et al., 2015; Liu et al., 2016; Ogawa et al., 2018; Setoyama et al., 2016; Umehara et al., 2017; Zheng et al., 2016). To our knowledge, only one study has investigated the metabolomic signature associated with suicidal ideation; that study reported that citrate, kynurenine, 3-hydroxykynurenine, and kynurenate were specifically associated with suicidal ideation (Setoyama et al., 2016). A study of suicidal behavior within individuals with major depressive disorder additionally reported that serum lipid levels, cholesterol, glucose, and several amino acids could be used to discriminate those who had attempted suicide form other depressed individuals and healthy controls (Zheng et al., 2013).
To our knowledge, no study has yet investigated changes to the metabolome associated with these mental health conditions among women during pregnancy, a time of high susceptibility to mood disorders. Therefore, we sought to evaluate metabolomic signatures of antepartum depression and antepartum suicidal ideation in a population of pregnant women.
Methods
Study population
We analyzed data from the metabolomics sub-study of the Screening, Treatment, and Effective Management of Gestational Diabetes Mellitus (STEM-GDM) study. STEM-GDM is a cohort study designed to measure the prevalence of gestational diabetes among Peruvian women receiving prenatal care between February 2013 and February 2014 at Instituto Nacional Materno Perinatal (INMP) in Lima, Peru. Eligible women initiated prenatal care before 28 weeks of pregnancy. Women were excluded if they were younger than 18 years, were not able to speak and read in Spanish, or did not plan to deliver at INMP. In total, 1,032 women were recruited into the STEM-GDM study; of these 100 women were randomly selected to take part in the metabolomics sub-study. Sub-study women did not differ from the overall population in regard to sociodemographic or lifestyle factors.
Information about sociodemographic factors, lifestyle characteristics, and reproductive and medical history was collected in a structured interview between 24–28 weeks of pregnancy. Fasting blood samples were additionally collected between 24–28 weeks of pregnancy (25 weeks on average). All participants provided written informed consent. The research protocol was approved by the Institutional Review Board of the INMP (Lima, Peru) and the Harvard T.H. Chan School of Public Health Office of Human Research Administration (Boston, MA, USA).
Metabolomic profiling
Details of the metabolomic profiling method used in this cohort have been previously reported by our group (Gelaye et al., 2019). Briefly, we collected fasting blood samples. Samples were kept on wet ice and centrifuged within 20 minutes of collection before being stored at −80°C until analysis. To profile serum polar metabolites and lipids, four liquid chromatography-tandem mass spectrometry (LC-MS) methods were used as described previously (Gelaye et al., 2019). Non-targeted, positive ion mode analyses of polar metabolites and lipids were conducted using two separate methods as described previously (Mascanfroni et al., 2015). Data for both methods were acquired using a Nexera X2 U-HPLC system (Shimadzu Scientific Instruments; Marlborough, MA) coupled to a Q Exactive Orbitrap mass spectrometer (Thermo Fisher Scientific; Waltham, MA). Polar metabolite MS analyses were carried out using electrospray ionization in the positive ion mode.
Outcome definition
Antepartum depression
To evaluate antepartum depression, we used responses to the Patient Health Questionnaire 9 (PHQ-9) collected between 24–28 weeks of pregnancy. The PHQ-9 is a brief survey designed to diagnose depression in a clinical setting by asking participants to report whether they have been experiencing each of the 9 Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV criteria for depression (anhedonia, depressed mood, insomnia or hypersomnia, fatigue or loss of energy, appetite disturbances, guilt or worthlessness, diminished ability to think or concentrate, psychomotor agitation or retardation, and suicidal thoughts) over the last 2 weeks (Kroenke et al., 2001). Each symptom question on the PHQ-9 is scored from 0–3, with 0 indicating that the participant experienced that symptom “not at all” and 3 indicating that the participant experienced that symptom “nearly every day,” for a total possible score ranging from 0–27. The PHQ-9 has additionally been validated in pregnant populations (Sidebottom et al., 2012). Participants were classified as having antepartum depression if their PHQ-9 score was at least 10 (Kroenke et al., 2001).
Antepartum suicidal ideation
To evaluate antepartum suicidal ideation, we used responses to the last question on the Patient Health Questionnaire 9 (PHQ-9) collected between 24–28 weeks of pregnancy. The last question asks whether, over the last 2 weeks, a participant has been bothered by “thoughts that you would be better off dead, or of hurting yourself.” A participant was recorded as having antepartum suicidal ideation if she responded affirmatively to this question and reported experiencing these thoughts for several days, more than half the days, or nearly every day. Responses to this question have been shown in prior studies to be a robust predictor of suicide risk (Rossom et al., 2017).
Statistical analysis
After excluding 14 metabolites missing or undetected in at least 20% of samples, 307 metabolites remained for analysis. Undetected values in the 307 metabolites were replaced with one-half of the smallest detected value for the metabolite. Metabolites were then log-transformed to account for skewed distributions and z-score standardized to the overall distribution of the metabolite. We used unadjusted t-tests and multivariate linear regression and logistic regression to evaluate the association between each metabolite and antepartum depression and antepartum suicidal ideation. Multivariate models were adjusted for age (continuous), gestational age (continuous), and pre-pregnancy body mass index (BMI) (continuous). To account for multiple testing, we used the Benjamini-Hochberg false discovery rate (FDR) correction. FDR correction controls the proportion of false positives in the analysis by adjusting the p-value needed to reject the null hypothesis (Benjamini and Hochberg, 1995). Analyses were conducted in SAS 9.4 (Cary, NC).
Results
Most women participating in our study were Mestizo (mixed Indigenous American and European ancestry), were married or living with a partner (83%), took prenatal vitamins (71%) and had at least 7 years of formal education (94%); very few smoked or used alcohol in pregnancy (1% and 3%, respectively) (Table 1). Of the 100 participating women, 29 had antepartum depression and 18 had antepartum suicidal ideation (these groups are not mutually exclusive; of the 100 participating women, 15 had both antepartum depression and antepartum suicidal ideation). Compared to women without antepartum depression, women with antepartum depression were statistically significantly more likely to report poor sleep quality, higher perceived stress, and higher generalized anxiety (Table 1). Similarly, compared to women without antepartum suicidal ideation, women with antepartum suicidal ideation were statistically significantly more likely to report poor sleep quality, higher perceived stress, and higher generalized anxiety; they were also more likely to report difficulty paying for basics and were less likely to say that their pregnancy was planned (not shown).
Table 1.
Demographic characteristics overall and by antepartum depression status
| Characteristic | Total (n=100) | Antepartum depression (n=29) | No antepartum depression (n=71) | P-valueb |
|---|---|---|---|---|
| n(%) | n(%) | n(%) | ||
| Maternal age (years) | 0.30 | |||
| <20 | 5 (5.0) | 1 (3.5) | 4 (5.6) | |
| 20–29 | 54 (54.0) | 16 (55.2) | 38 (53.5) | |
| 30–34 | 18 (18.0) | 8 (27.6) | 10 (14.1) | |
| >34 | 23 (23.0) | 4 (13.8) | 19 (26.8) | |
| Pre-pregnancy BMI (mean (SD)) | 25.8 (3.8) | 26.6 (2.9) | 25.5 (4.1) | 0.11 |
| Maternal education (years) | 0.31 | |||
| ≤ 6 | 6 (6.0) | 3 (10.3) | 3 (4.2) | |
| 7–12 | 54 (54.0) | 17 (58.6) | 37 (52.1) | |
| >12 | 40 (40.0) | 9 (31.0) | 31 (43.7) | |
| Married or live with partner | 83 (83.0) | 23 (79.3) | 60 (84.5) | 0.56 |
| Maternal paid employment | 27 (27.0) | 6 (20.7) | 21 (29.6) | 0.36 |
| Maternal race | 0.99 | |||
| Mestizo | 97 (97.0) | 28 (96.6) | 69 (97.2) | |
| Other | 3 (3.0) | 1 (3.5) | 2 (2.8) | |
| Difficulty paying for basics | 0.066 | |||
| Hard or Very Hard | 14 (14.0) | 7 (24.1) | 7 (10.0) | |
| Somewhat or Not Very Hard | 85 (85.9) | 22 (75.9) | 63 (90.0) | |
| Sleep qualitya | <0.0001 | |||
| Good | 75 (75.0) | 14 (48.3) | 61 (85.9) | |
| Poor | 25 (25.0) | 15 (51.7) | 10 (14.1) | |
| PSS Score (mean(SD))c | 21.7 (5.2) | 24.7 (5.2) | 20.5 (4.7) | 0.0001 |
| GAD-7 score (mean(SD))d | 11.0 (3.0) | 12.8 (3.8) | 10.2 (2.3) | 0.0012 |
| Primiparous | 35 (35.0) | 6 (20.7) | 29 (40.9) | 0.055 |
| Gestational weeks (mean (SD)) | 25.6 (1.2) | 25.2 (1.0) | 25.7 (1.3) | 0.062 |
| Planned pregnancy | 37 (37.0) | 9 (31.0) | 28 (39.4) | 0.43 |
| Prenatal vitamins | 71 (71.0) | 20 (69.0) | 51 (71.8) | 0.77 |
| Smoking before pregnancy | 22 (22.0) | 4 (13.8) | 18 (25.4) | 0.21 |
| Smoking during pregnancy | 1 (1.0) | 0 (0) | 1 (1.4) | 0.71 |
| Alcohol before pregnancy | 27 (27.0) | 6 (20.7) | 21 (29.6) | 0.36 |
| Alcohol during pregnancy | 3 (3.0) | 2 (6.9) | 1 (1.4) | 0.20 |
Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI) question, “During the past month, how would you rate your sleep quality overall?”.
P-value for gestational weeks, GAD-7 score, and PSS score calculated using t-tests; all other p-values from chi-square or Fisher’s exact tests.
Perceived Stress Scale (PSS)
Generalized Anxiety Disorder 7-item scale (GAD-7)
Antepartum depression
First, we compared metabolite levels among participants with and without antepartum depression using unadjusted t-tests. In unadjusted t-tests, we found that levels of 10 metabolites (5 triacylglycerol metabolites, betaine, C36:4 PE plasmalogen, C5 carnitine, thiamine, and citrulline) were statistically significantly different between antepartum depression cases and non-cases (Supplemental Table S1). Next, we used regression models to calculate the association between each metabolite level and antepartum depression. In adjusted logistic models, 3 triacylglycerol metabolites were associated with higher odds of antepartum depression, and four metabolites (betaine (OR=0.56; 95% confidence interval (CI): 0.33–0.95), citrulline (OR=0.58; 95%CI: 0.34–0.98), C5 carnitine (OR=0.59; 95%CI: 0.36–0.99), and C5:1 carnitine (OR=0.59; 95%CI: 0.35–1.00) were associated with lower odds of antepartum depression (Table 2). We also calculated the association between each metabolite and continuous PHQ-9 score. In adjusted linear regression models, seven metabolites were associated with continuous PHQ-9 score (choline, phenylalanine, betaine, C4 carnitine, aspartate, glutamate, and C5 carnitine) (Table 3). Betaine and C5 carnitine were therefore statistically significantly inversely associated with both odds of antepartum depression and continuous PHQ-9 score. No metabolites remained statistically significant after FDR correction.
Table 2.
Odds ratios for antepartum depression.
| Metaboliteb | HMDB ID | Class | Adjusteda OR (95%CI) | p | FDR p |
|---|---|---|---|---|---|
| C48:5 triacylglycerol | N/A | Glycerolipid | 1.89 (1.14, 3.14) | 0.014 | 0.99 |
| C50:6 triacylglycerol | HMDB10497 | Glycerolipid | 1.88 (1.13, 3.14) | 0.015 | 0.99 |
| C46:4 triacylglycerol | N/A | Glycerolipid | 1.89 (1.11, 3.21) | 0.018 | 0.99 |
| Betaine | HMDB00043 | Carboxylic acid | 0.56 (0.33, 0.95) | 0.031 | 0.99 |
| Citrulline | HMDB00904 | Carboxylic acid | 0.58 (0.34, 0.98) | 0.043 | 0.99 |
| C5 carnitine | HMDB00688 | Fatty acyl | 0.59 (0.36, 0.99) | 0.046 | 0.99 |
| C5:1 carnitine | HMDB02366 | Fatty acyl | 0.59 (0.35, 1.00) | 0.049 | 0.99 |
Adjusted for age, gestational weeks, and pre-pregnancy BMI
Metabolites included in the table have adjusted regression p-value <0.05 before FDR correction
Table 3.
Parameter estimates for PHQ-9 score.
| Metaboliteb | HMDB ID | Class | Adjusteda Beta (SE) | p | FDR p |
|---|---|---|---|---|---|
| Choline | HMDB00097 | Organonitrogen compound | −1.22 (0.49) | 0.015 | 0.99 |
| Phenylalanine | HMDB00159 | Carboxylic acid | −1.16 (0.49) | 0.021 | 0.99 |
| Betaine | HMDB00043 | Carboxylic acid | −1.19 (0.52) | 0.024 | 0.99 |
| C4 carnitine | HMDB02013 | Fatty acyl | −1.07 (0.50) | 0.036 | 0.99 |
| Aspartate | HMDB00191 | Carboxylic acid | −1.02 (0.50) | 0.043 | 0.99 |
| Glutamate | HMDB00148 | Carboxylic acid | −1.02 (0.50) | 0.045 | 0.99 |
| C5 carnitine | HMDB00688 | Fatty acyl | −1.02 (0.52) | 0.050 | 0.99 |
Adjusted for age, gestational weeks, and pre-pregnancy BMI
Metabolites included in the table have adjusted regression p-value <0.05 before FDR correction
Antepartum suicidal ideation
As with antepartum depression, we first compared metabolite levels among participants with and without antepartum suicidal ideation using unadjusted t-tests. In unadjusted t-tests, we found that levels of 45 metabolites were statistically significantly different between antepartum suicidal ideation cases and non-cases (Supplemental Table S2). Next, we used regression models to calculate the association between each metabolite and antepartum suicidal ideation. In adjusted logistic regression models, 26 metabolites, including thiamine (OR=0.44; 95%CI: 0.22–0.85), choline (OR=0.29; 95%CI: 0.11–0.81), phenylalanine (OR=0.41; 95%CI: 0.19–0.91), and betaine (OR=0.53; 95%CI: 0.28–0.99), were associated with lower odds of antepartum suicidal ideation (Table 4). All statistically significant associations with antepartum suicidal ideation were inverse. As a secondary analysis, we additionally calculated adjusted associations between each metabolite and antepartum suicidal ideation restricted to the population of women with antepartum depression (i.e., comparing women with antepartum depression and suicidal ideation [n=15] to women with antepartum depression and not suicidal ideation [n=14]). Nine metabolites associated with antepartum suicidal ideation in this subpopulation overlapped with those associated with antepartum suicidal ideation in the whole population (C24:1 ceramide, C16:0 CE, C20:0 SM, C14:0 SM, docosahexaenoic acid, C38:6 ceramide (d18:1), C38:7 PE plasmalogen, C22:6 LPC) (not shown). No metabolites remained statistically significant in the main analysis or secondary analysis after FDR correction.
Table 4.
Odds ratios for antepartum suicidal ideation.
| Metaboliteb | HMDB ID | Class | Adjusteda OR (95%CI) | p | FDR p |
|---|---|---|---|---|---|
| C38:7 PE plasmalogen | HMDB11420 | Glycerophospholipid | 0.41 (0.21, 0.80) | 0.0087 | 0.47 |
| C40:7 PE plasmalogen | HMDB11394 | Glycerophospholipid | 0.42 (0.22, 0.82) | 0.011 | 0.47 |
| C14:0 SM | HMDB12097 | Sphingolipid | 0.41 (0.20, 0.82) | 0.012 | 0.47 |
| Thiamine | HMDB00235 | Diazine | 0.44 (0.22, 0.85) | 0.015 | 0.47 |
| Choline | HMDB00097 | Organonitrogen compound | 0.29 (0.11, 0.81) | 0.018 | 0.47 |
| C16:0 CE | HMDB00885 | Steroid | 0.44 (0.22, 0.88) | 0.019 | 0.47 |
| 5-Hydroxytryptophan | HMDB00472 | Indole | 0.52 (0.30, 0.92) | 0.023 | 0.47 |
| C20:0 SM | HMDB12102 | Sphingolipid | 0.47 (0.24, 0.90) | 0.023 | 0.47 |
| C24:1 Ceramide (d18:1) | HMDB04953 | Sphingolipid | 0.52 (0.29, 0.92) | 0.025 | 0.47 |
| Docosahexaenoic acid | HMDB02183 | Fatty acyl | 0.50 (0.27, 0.92) | 0.025 | 0.47 |
| Phenylalanine | HMDB00159 | Carboxylic acid | 0.41 (0.19, 0.91) | 0.027 | 0.47 |
| C34:0 PI | HMDB09805 | Glycerophospholipid | 0.55 (0.32, 0.94) | 0.029 | 0.47 |
| C22:6 LPC | HMDB10404 | Glycerophospholipid | 0.52 (0.28, 0.96) | 0.035 | 0.47 |
| Asymmetric dimethylarginine | HMDB01539 | Carboxylic acid | 0.42 (0.19, 0.95) | 0.037 | 0.47 |
| C4 carnitine | HMDB02013 | Fatty acyl | 0.51 (0.27, 0.96) | 0.037 | 0.47 |
| Lysine | HMDB00182 | Carboxylic acid | 0.47 (0.23, 0.96) | 0.038 | 0.47 |
| C38:6 PC plasmalogen | HMDB11319 | Glycerophospholipid | 0.52 (0.28, 0.97) | 0.039 | 0.47 |
| 8,11,14-Eicosatrienoic acid | HMDB02925 | Fatty acyl | 0.54 (0.30, 0.97) | 0.040 | 0.47 |
| C24:0 Ceramide (d18:1) | HMDB04956 | Sphingolipid | 0.54 (0.30, 0.97) | 0.041 | 0.47 |
| C56:8 triacylglycerol | HMDB05392 | Glycerolipid | 0.51 (0.27, 0.98) | 0.042 | 0.47 |
| C18:0 LPC | HMDB10384 | Carboxylic acid | 0.53 (0.29, 0.98) | 0.044 | 0.47 |
| Symmetric dimethylarginine | HMDB03334 | Carboxylic acid | 0.50 (0.25, 0.98) | 0.045 | 0.47 |
| Betaine | HMDB00043 | Carboxylic acid | 0.53 (0.28, 0.99) | 0.045 | 0.47 |
| Methionine sulfoxide | HMDB02005 | Carboxylic acid | 0.41 (0.17, 0.98) | 0.046 | 0.47 |
| C20:3 CE | HMDB06736 | Steroid | 0.57 (0.32, 1.00) | 0.048 | 0.47 |
| C38:6 PC | HMDB07991 | Glycerophospholipid | 0.56 (0.31, 0.99) | 0.048 | 0.47 |
Adjusted for age, gestational weeks, and pre-pregnancy BMI
Metabolites included in the table have adjusted regression p-value <0.05 before FDR correction
Discussion
In this study, we report statistically significant associations between numerous metabolites and antepartum depression and suicidal ideation in pregnant women. Specifically, we found that levels of 3 metabolites were significantly increased, and 4 metabolites were significantly decreased, among women with antepartum depression compared to those without antepartum depression; and levels of 26 metabolites were significantly decreased among women with antepartum suicidal ideation compared to those without antepartum suicidal ideation. No metabolites remained significantly associated with either outcome after multiple testing correction.
To our knowledge, this is the first study to describe the metabolomic signatures of antepartum depression and antepartum suicidal ideation. Our results can tentatively be interpreted in the context of similar findings in non-pregnant populations. Betaine was the only metabolite statistically significantly associated with both antepartum depression and antepartum suicidal ideation in adjusted models. Preliminary evidence links betaine to severity of depression in both medicated and unmedicated patients (Setoyama et al., 2016). In a trial of 46 participants, supplementing s-adenosyl-methionine with betaine in patients with mild-to-moderate depression improved symptoms more than treatment with s-adenosyl-methionine alone (Di Perro et al., 2015). Betaine has also been found to be inversely associated with first-episode schizophrenia (Koike et al., 2014). However, not all studies have reported positive findings. For example, in a study of pregnant women van Lee et al. reported that plasma betaine was not associated with mood disorder (van Lee et al., 2017). Similarly, in a study of 51 participants (32 with psychiatric disorders), Kageyama et al. found no association between betaine levels and schizophrenia, bipolar disorder or major depressive disorder (Kageyama et al., 2017). If betaine is indeed protective against mood disturbance, it may be a suitable target for supplementation in pregnancy. Betaine is found in foods such as quinoa (Ross et al., 2014) wheat, and spinach. It is formed through the metabolic reduction of choline, which was also inversely associated with SI in our study (Craig, 2004). Brain choline has been positively associated with major depressive disorder (Riley and Renshaw, 2018), but the association between choline in plasma and mental health is less clear. In three recent studies, plasma choline was inversely associated with anxiety in healthy adults (Bjelland et al., 2009), positively associated with depression and anxiety symptoms in pregnant women, (van Lee et al., 2017) and not associated with schizophrenia, bipolar disorder, or major depressive disorder (Kageyama et al., 2017). Further investigation into the role of betaine and choline and mental health may be warranted.
Several additional metabolites inversely associated with antepartum suicidal ideation in our analysis of pregnant women, including citrulline, thiamine, methionine sulfoxide, and asymmetric and symmetric dimethylarginine have also been associated with mental health outcomes in prior studies (Ali-Sisto et al., 2018; Dhir et al., 2019; Hess et al., 2017; Kageyama et al., 2017; Raw et al., 2014; Umehara et al., 2017). The strongest evidence is for thiamine. Supplementation trials have shown that thiamine supplements result in improvements in mood, energy, and cognitive function (Benton et al., 1997; Smidt et al., 1991); a recent trial reported that thiamine supplements in addition to selective serotonin reuptake inhibitors were associated with faster depression symptom alleviation than selective serotonin reuptake inhibitors alone (Ghaleiha et al., 2016). In observational data, thiamine levels are also inversely associated with depression symptoms (Pepersack et al., 1999; Zhang et al., 2013). Though we are the first to identify an association between thiamine and antepartum suicidal ideation, our finding aligns well with prior studies and suggests that mood disorder in pregnancy shares metabolomic similarities to mood disorder at other times.
Two metabolites statistically significantly inversely associated with antepartum suicidal ideation in our analysis, 5-hydroxytryptophan and phenylalanine, are molecular precursors of the neurotransmitters serotonin and dopamine, respectively. Downregulation of the serotonin and dopamine pathways has been previously implicated in mood disorders, including in metabolomics studies, which have identified inverse associations between tryptophan (parent of 5-hydroxytryptophan), phenylalanine, and major depressive disorder in non-pregnant adults (Kawamura et al., 2018; Kuwano et al., 2018; Liu et al., 2015; Setoyama et al., 2016). Recent preliminary evidence has also suggested that microglial cell activation in the brain may alter tryptophan signaling and lead to suicidal ideation in non-pregnant populations (Suzuki et al., 2019), providing a potential mechanism. Our results contribute to evidence that circulating neurotransmitter precursors may be markers for mood disorders.
We did not find statistically significant associations between antepartum depression or suicidal ideation and kynurenine or its metabolic descendants, although prior literature (including the only prior study on suicidal ideation (Setoyama et al., 2016)) linked elevated kynurenine pathway metabolites to both depression and suicidality in non-pregnant populations (Bryleva and Brudin, 2017; Serafini et al., 2017). Because tryptophan is metabolized into both serotonin and kynurenine, if the kynurenine pathway is upregulated, levels of serotonin theoretically might decrease, providing a mechanism to connect this pathway and major depressive disorder (Bryleva and Brudin, 2017). We profiled kynurenic acid, 3-hydroxyanthanilic acid, and 1-methylnicotinamide, which are metabolites on the kynurenine pathway, but none were statistically significantly associated with antepartum depression or antepartum suicidal ideation. Kynurenic acid was non-significantly inversely associated with both antepartum depression and antepartum suicidal ideation, while 3-hydroxyanthanilic acid was non-significantly positively associated with both antepartum depression and antepartum suicidal ideation. Metabolite 1-methylnicotinamide was non-significantly positively associated with antepartum suicidal ideation and inversely associated with antepartum depression. There is not a clear signal for the role of the kynurenine pathway in this analysis.
The metabolomic signatures of antepartum depression and antepartum suicidal ideation were dissimilar. We found few associations between metabolites and antepartum depression, and many of the metabolites previously associated with major depressive disorder in non-pregnant populations were associated with antepartum suicidal ideation in our sample. Only betaine was statistically significantly associated with the odds of both antepartum depression and antepartum suicidal ideation. Additionally, while some metabolites were positively significantly associated with antepartum depression, all significant associations with antepartum suicidal ideation were inverse. In fact, in adjusted models, 267 of 307 metabolites (87%) were inversely associated with antepartum suicidal ideation (including those not significantly associated), suggesting that antepartum suicidal ideation may be characterized by a broad downward shift in many metabolic pathways. A large number of inverse associations has been noted in several other diseases, including prodromal amyotrophic lateral sclerosis (Bjornevik et al., 2019), Alzheimer’s disease (Proitsi et al., 2015), and pre-diagnostic Parkinson’s disease (unpublished data). However, this broad downward metabolomic shift was seen only for antepartum suicidal ideation, and not for antepartum depression, in our data. These findings may indicate that antepartum suicidal ideation and antepartum depression represent distinct mood disorders with only partially overlapping pathophysiology in pregnancy.
Our study had many strengths. We are the first to characterize the metabolomic signature of antepartum depression and antepartum suicidal ideation in pregnancy, a time of high susceptibility to mood disorder, and utilized an existing treatment-naïve cohort, eliminating variability that would arise due to treatment. Our findings may, therefore, be used to better understand the pathophysiology of these common mood disorders and may also have predictive utility to determine which women are at risk of developing antepartum depression and antepartum suicidal ideation. We are also among the first to examine the metabolomics associated with antepartum suicidal ideation, which may help identify new clinical pathways to diagnose and treat this condition. A number of the statistically significant metabolites in this analysis have been linked to mood disorder in other studies, lending credibility to our findings in a pregnant population. Our work is also hypothesis generating, as we are among the first to identify betaine as a possible marker of depression. Finally, we used a validated, rigorous, and consistently applied protocol to profile metabolites, reducing the risk for differential measurement error by outcome status (Townsend et al., 2013).
Some caveats would be considered in interpreting our findings. Metabolites and psychiatric symptoms were measured at the same time, so we are not able to determine whether the identified metabolites are predictive or simply descriptive of antepartum depression and antepartum suicidal ideation. However, as the first analysis of antepartum depression and antepartum suicidal ideation in pregnancy, our results still make an important contribution. We did not collect information about diet. Differences in measured metabolites may therefore be due to dietary changes rather than underlying pathophysiology. However, changes in diet may be part of the disease process for antepartum depression and antepartum suicidal ideation and the metabolites may still be valid markers. Finally, after FDR correction no metabolites remained statistically significantly associated with either antepartum depression or antepartum suicidal ideation. This is likely a function of the small sample size and large number of statistical tests rather than an indication that no associations were meaningful, especially because many metabolites associated with antepartum suicidal ideation in our data have been previously linked to mental health in other populations. However, we cannot rule out the possibility that identified associations are due to chance.
In conclusion, we report for the first time that plasma levels of numerous metabolites are associated with antepartum depression and antepartum suicidal ideation in pregnancy. Our findings suggest that the metabolomic profile of antepartum suicidal ideation during pregnancy is physiologically similar to depression among non-pregnant adults, including involvement of the tryptophan and phenylalanine (serotonin and dopamine) metabolic pathways. The metabolites we identified as markers of antepartum suicidal ideation should be further tested as predictive metabolites in prospective studies. Because no metabolites remained significantly associated with antepartum depression or antepartum suicidal ideation after FDR correction, findings should be interpreted with caution and replication with a larger sample size is warranted.
Supplementary Material
Highlights.
We identified 7 metabolites associated with antepartum depression.
We identified 26 metabolites associated with antepartum suicidal ideation.
Metabolomic profiles of antepartum depression and suicidal ideation were distinct.
The profile of suicidal ideation is similar to depression in nonpregnant adults.
No metabolites were significant after multiple testing correction.
Acknowledgements
This study was funded by the National Institute of Environmental Health Sciences (T32ES007069), Roche Diagnostic Operations Inc. (project number 208617-5074547), and the National Institute on Minority Health and Health Disparities (T37-MD0001449). Sponsors had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Role of the Funding Source
This study was funded by the National Institute of Environmental Health Sciences (T32ES007069), Roche Diagnostic Operations Inc. (project number 208617-5074547), and the National Institute on Minority Health and Health Disparities (T37-MD0001449). Sponsors had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Declarations of interest: none.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ali-Sisto T, Tolmunen T, Viinamaki H, Mantyselka P, Valkonen-Korhonen M, Koivumaa-Honkanen H, Honkalampi K, Ruusunen A, Nandania J, Velagapudi V, Lehto SM, 2018. Global arginine bioavailability ratio is decreased in patients with major depressive disorder. J Affect Disord 229, 145–151. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y, 1995. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, Series B (Methodological) 57, 289–300. [Google Scholar]
- Benton D, Griffiths R, Haller J, 1997. Thiamine supplementation mood and cognitive functioning. Psychopharmacology 129, 66–71. [DOI] [PubMed] [Google Scholar]
- Biaggi A, Conroy S, Pawlby S, Pariante CM, 2016. Identifying the women at risk of antenatal anxiety and depression: A systematic review. Journal of Affective Disorders 191, 62–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjelland I, Tell GS, Vollset SE, Konstantinova S, Ueland PM, 2009. Choline in anxiety and depression: the Hordaland Health Study. Am J Clin Nutr 90, 1056–1060. [DOI] [PubMed] [Google Scholar]
- Bjornevik K, Zhang Z, O’Reilly EJ, Berry JD, Clish CB, Deik A, Jeanfavre S, Kato I, Kelly RS, Kolonel LN, Liang L, Le Marchand L, McCullogh ML, Paganoni S, Pierce KA, Schwarzschild MA, Shadyab AH, Wactawski-Wende J, Wang DD, Wang Y, Manson JE, Ascherio A, 2019. Prediagnostic plasma metabolomics and the risk of amyotrophic lateral sclerosis. Neurology 92, e2089–e2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryleva EY, Brudin L, 2017. Kynurenine pathway metabolites and suicidality. Neuropharmacology 112, 324–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig SAS, 2004. Betaine in human nutrition. Am J Clin Nutr 80, 539–549. [DOI] [PubMed] [Google Scholar]
- Davalos DB, Yadon CA, Tregellas HC, 2012. Untreated prenatal maternal depression and the potential risks to offspring: a review. Arch Womens Ment Health 15, 1–14. [DOI] [PubMed] [Google Scholar]
- Dhir S, Tarasenko M, Napoli E, Giulivi C, 2019. Neurological, psychiatric, and biochemical aspects of thiamine deficiency in children and adults. Front Psychiatry 10, 207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Perro F, Orsi R, Settembre R, 2015. Role of betaine in improving the antidepressant effect of S-adenosyl-methionine in patients with mild-to-moderate depression. J Multidisc Healthcare 8, 39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz PM, Williams SB, Callaghan WM, Bachman DJ, Whitlock EP, Hornbrook MC, 2007. Clinically identified maternal depression before, during, and after pregnancies ending in live births. Am J Psychiatry 164, 1515–1520. [DOI] [PubMed] [Google Scholar]
- Eke AC, Saccone G, Berghella V, 2016. Selective serotonin reuptake inhibitor (SSRI) use during pregnancy and risk of preterm birth: a systematic review and meta-analysis. BJOG 123, 1900–1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T, 2005. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol 105, 1071–1083. [DOI] [PubMed] [Google Scholar]
- Gelaye B, Clish CB, Denis M, Larrabure G, Tadesse MG, Deik A, Pierce K, Bullock K, Dennis C, Enquobahrie DA, Williams MA, 2019. Metabolomics signatures associated with an oral glucose challenge in pregnant women. Diabetes Metab 45, 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelaye B, Kajeepeta S, Williams MA, 2016a. Suicidal ideation in pregnancy: an epidemiologic review. Arch Womens Ment Health 19, 741–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelaye B, Rondon MB, Araya R, Williams MA, 2016b. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet 3, 973–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaleiha A, Davari H, Jahangard L, Haghighi M, Ahmadpanah M, Seifrabie MA, Bajoghli H, Holsboer-Trachsler E, Brand S, 2016. Adjuvant thiamine improved standard treatment in patients with major depressive disorder: results from a randomized, double-blind, and placebo-controlled clinical trial. Eur Arch Psychiatry Clin Neurosci 266, 695–702. [DOI] [PubMed] [Google Scholar]
- Hess S, Baker G, Gyenes G, Tsuyuki R, Newman S, Le Melledo J, 2017. Decreased serum L-arginine and L-citrulline levels in major depression. Psychopharmacology 234, 3241–3247. [DOI] [PubMed] [Google Scholar]
- Kageyama Y, Kasahara T, Morishita H, Mataga N, Deguchi Y, Tani M, Kuroda K, Hattori K, Yoshida S, Inoue K, Kato T, 2017. Search for plasma biomarkers in drug-free patients with bipolar disorder and schizophrenia using metabolome analysis. Psychiatry Clin Neurosci 71, 115–123. [DOI] [PubMed] [Google Scholar]
- Kawamura N, Shinoda K, Sato H, Sasaki K, Suzuki M, Yamaki K, Fujimori T, Yamamoto H, Osei-Hyiaman D, Ohashi Y, 2018. Plasma metabolome analysis of patients with major depressive disorder. Psychiatry Clin Neurosci 72, 349–361. [DOI] [PubMed] [Google Scholar]
- Koike S, Bundo M, Iwamoto K, Suga M, Kuwabara H, Ohashi Y, Shinoda K, Takano Y, Iwashiro N, Satomura Y, Nagai T, Natsubori T, Tada M, Yamasue H, Kasai K, 2014. A snapshot of plasma metabolites in first-episode schizophrenia: a capillary electrophoresis time-of-flight mass spectrometry study. Transl Psychiatry 8, e379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, 2001. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuwano N, Kato TA, Setoyama D, Sato-Kasai M, Shimokawa N, Hayakawa K, Ohgidani M, Sagata N, Kubo H, Kishimoto J, Kang D, Kanba S, 2018. Tryptophan-kynurenine and lipid related metabolites as blood biomarkers for first-episode drug-naive patients with major depressive disorder: An exploratory pilot case-control study. J Affect Disord 231, 74–82. [DOI] [PubMed] [Google Scholar]
- Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM, 2010. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol 202, 5–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh B, Milgrom J, 2008. Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Zheng P, Zhao X, Zhang Y, Hu C, Li J, Zhao J, Zhou J, Xie P, Xu G, 2015. Discovery and validation of plasma biomarkers for major depressive disorder classification based on liquid chromatography-mass spectrometry. J Proteome Res 14, 2322–2330. [DOI] [PubMed] [Google Scholar]
- Liu Y, Yieh L, Yang T, Drinkenburg W, Peeters P, Steckler T, Narayan VA, Wittenberg G, Ye J, 2016. Metabolomic biosignature differentiates melancholic depressive patients from healthy controls. BMC Genomics 17, 669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mascanfroni ID, Takenaka MC, Yeste A, Patel B, Wu Y, Kenison JE, Siddiqui S, Basso AS, Otterbein LE, Pardoll DM, Pan F, Priel A, Clish CB, Robson SC, Quintana FJ, 2015. Metabolic control of type 1 regulatory T cell differentiation by AHR and HIF1-α. Nat Med 21, 638–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogawa S, Koga N, Hattori K, Matsu J, Ota M, Hori H, Sasayama D, Teraishi T, Ishida I, Yoshida F, Yoshida S, Noda T, Higuchi T, Kunugi H, 2018. Plasma amino acid profile in major depressive disorder: Analyses in two independent case-control sample sets. J Psychiatr Res 96, 23–32. [DOI] [PubMed] [Google Scholar]
- Pepersack T, Garbusinski J, Robberecht J, Beyer I, Willems D, Fuss M, 1999. Clinical relevance of thiamine status amongst hospitalized elderly patients. Gerontology 45, 96–101. [DOI] [PubMed] [Google Scholar]
- Proitsi P, Kim MH, Whiley L, Pritchard M, Leung R, Soininen H, Kloszewska I, Mecocci P, Tsolaki M, Vellas B, Sham P, Lovestone S, Powell JF, Dobson RJB, Legido-Quigley C, 2015. Plasma lipidomics analysis finds long chain cholesteryl esters to be associated with Alzheimer’s disease. Transl Psychiatry 5, e494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raw A, Gallaher M, Powers RW, 2014. Arginine and ADMA in pregnant women with major depression. Psychosom Med 76, 430–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley CA, Renshaw PF, 2018. Brain choline in major depression: A review of the literature. Psychiatry Research: Neuroimaging 271, 142–153. [DOI] [PubMed] [Google Scholar]
- Ross AB, Zangger A, Guiraud SP, 2014. Cereal foods are the major source of betaine in the Western diet--analysis of betaine and free choline in cereal foods and updated assessments of betaine intake. Food Chem 15, 859–865. [DOI] [PubMed] [Google Scholar]
- Rossom RC, Coleman KJ, Ahmedani BK, Beck A, Johnson E, Oliver M, Simon GE, 2017. Suicidal ideation reported on the PHQ9 and risk of suicidal behavior across age groups. J Affect Disord 215, 77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serafini G, Adavastro G, Canepa G, Capobianco L, Conigliaro C,F,P, Murri MB, Valchera A, De Berardis D, Pompili M, Lindgvist D, Brundin L, Amore M, 2017. Abnormalities in kynurenine pathway metabolism in treatment-resistant depression and suicidality: A systematic review. CNS Neurol Disord Drug Targets 16, 440–453. [DOI] [PubMed] [Google Scholar]
- Setoyama D, Kato TA, Hashimoto R, Kunugi H, Hattori K, Hayakawa K, Sato-Kasai M, Shimokawa N, Kaneko S, Yoshida S, Goto YI, Yasuda Y, Yamamori H, Ohgidani M, Sagata N, Miura D, Kang D, Kanba S, 2016. Plasma Metabolites Predict Severity of Depression and Suicidal Ideation in Psychiatric Patients-A Multicenter Pilot Analysis. PLoS One 11, e0165267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidebottom AC, Harrison PA, Godecker A, Kim H, 2012. Validation of the Patient Health Questionnaire (PHQ)-9 for prenatal depression screening. Arch Womens Ment Health 15, 367–374. [DOI] [PubMed] [Google Scholar]
- Smidt LJ, Cremin FM, Grivetti LE, Clifford AJ, 1991. Influence of thiamin supplementation on the health and general well-being of an elderly Irish population with marginal thiamin deficiency. J Gerontology 46, M16–M22. [DOI] [PubMed] [Google Scholar]
- Suzuki H, Ohgidani M, Kuwano N, Chrétien F, Lorin de la Grandmaison G, Onaya M, Tominaga I, Setoyama D, Kang D, Mimura M, Kanba S, Kato TA, 2019. Suicide and Microglia: Recent Findings and Future Perspectives Based on Human Studies. Front Cell Neurosci 13, 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend MK, Clish CB, Kraft P, Wu C, Souza AL, Deik AA, Tworoger SS, Wolpin BM, 2013. Reproducibility of metabolomic profiles among men and women in 2 large cohort studies. Clin Chem 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umehara H, Numata S, Watanabe S, Hataleyama Y, Kinoshita M, Tomioka Y, Nakahara K, Nikawa T, Ohmori T, 2017. Altered KYN/TRP, Gln/Glu, and Met/methionine sulfoxide ratios in the blood plasma of medication-free patients with major depressive disorder. Sci Rep 7, 4855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Lee L, Quah PL, Saw SM, Yap FKP, Godfrey KM, Chong YS, Meaney MJ, Chen H, Chong MF, 2017. Maternal choline status during pregnancy, but not that of betaine, is related to antenatal mental-wellbeing: the Growing Up in Singapore Towards healthy Outcomes Cohort. Depress Anxiety 34, 877–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisner KL, Sit DK, Hanusa BH, Moses-Kolko EL, Bogen DL, Hunker DF, Perel JM, Jones-Ivy S, Bodnar LM, Singer LT, 2009. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry 166, 557–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang G, Ding H, Chen H, Ye X, Li H, Lin X, Ke Z, 2013. Thiamine nutritional status and depressive symptoms are inversely associated among older Chinese adults. J Nutr 143, 53–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng P, Fang Z, Xu XJ, Liu ML, Du X, Zhang X, Wang H, Zhou J, Xie P, 2016. Metabolite signature for diagnosing major depressive disorder in peripheral blood mononuclear cells. J Affect Disord 195, 75–81. [DOI] [PubMed] [Google Scholar]
- Zheng P, Gao HC, Qi ZG, Jia JM, Li FF, Chen JJ, Wang Y, Guo J, Melgiri PX, 2013. Peripheral metabolic abnormalities of lipids and amino acids implicated in increased risk of suicidal behavior in major depressive disorder. Metabolomics 9, 688–696. [Google Scholar]
- Zhong QY, Gelaye B, Miller M, Fricchione GL, Cai T, Johnson PA, Henderson DC, Williams MA, 2016. Suicidal behavior-related hospitalizations among pregnant women in the USA, 2006–2012. Arch Womens Ment Health 19, 463–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


