Abstract
Aims
This review study aimed to investigate the strategies for implementing the nursing process in the clinical practice and the assessment of the implementation rate of this process in clinical settings of lower‐income countries.
Design
An integrative review.
Method
The search was conducted of EMBASE, MEDLINE, CINAHL, Scopus and ISI databases from 1975–July 2018. Following the formation of the research team, two researchers independently selected the eligible studies; finally, 39 articles were approved by the research team for this study.
Results
The researchers identified three themes: Effects of implementing the NP in clinical settings, Development and application of electronic software in the NP and Factors affecting the implementation of the NP. This review revealed that nurses and nursing managers in hospitals are interested in implementing the nursing process in the form of widely and continuously. But the necessary infrastructure, such as manpower, electronically or manually tools, has not yet been provided, and the implementation of the nursing process is done either imperfectly or not done.
Keywords: integrative review, nursing, nursing process
What does this paper contribute to the wider global clinical community?
The nursing process is not implemented nursing in Iran, Ethiopia, Kenya, Taiwan and generally in lower‐income countries, for the following three reasons:
Inadequate knowledge of nursing faculty members from the nursing process.
Lack of necessary infrastructures in hospitals.
Lack of support from nursing institutions (Nursing Organization and The Nursing Board).
1. INTRODUCTION
One of the most important care standards is the nursing process (NP) that helps nurses making a clinical decision. The nursing process is a scientific method that uses scientific reasoning, problem‐solving and critical thinking for delivering holistic and quality nursing care (Wagoro & Rakuom, 2015). Implementation of the nursing process in the clinical settings improves the quality of nursing care, enhances the level of nurses “knowledge, improves the quality and quantity of nurses” documentation and increases their job satisfaction and self‐efficacy (Hagos, Alemseged, Balcha, Berhe, & Aregay, 2014; Potter & Perry, 2017; Semachew, 2018). In this process, the nurse needs to assess and identify the problem, review the existing solutions, select and implement the best option and ultimately evaluate them (Potter & Perry, 2017). All the steps are done with the patient's participation (Potter & Perry, 2017). The NP is a tool for helping the nurse to make appropriate clinical decision‐making and critical thinking (Ghanbari, Monfared, Hoseinzadeh, Moaddab, & Sedighi, 2017). The NP as the most effective nursing care planning and implementation method leads to effective communication between the nurses and the patients, increasing both the participation of the patient in self‐care and the quality of nursing care (Muller‐Staub, Needham, Odenbreit, Lavin, & van Achterberg, 2008). Furthermore, it is functional and adaptable in any clinical setting and manages the time of care, and it also prevents the occurrence or repetition of the mistakes (Paese, Sasso, & Colla, 2018). The NP is used to provide services to all clients, including individuals, families, groups or communities, and it is unique to nursing (Potter & Perry, 2017). The main element of the NP is the nursing diagnosis that helps the nurses in guiding nursing care and in promoting the documentation process (Paans, Nieweg, van‐der‐Schans, & Sermeus, 2011). Despite the importance of this process for patients and nurses, the conditions for its implementation in low‐income countries (IPNA & Residents/nationals of these countries qualify for low‐income country rates, 2018) are unclear and dissatisfaction with nursing care has been widely reported in these countries (Ghafouri Fard, Haririan, Aghajanloo, Akbari, & Shirvani, 2012; Lotfi, Zamanzadeh, Valizadeh, & Khajehgoodari, 2019; Rajabpoor et al., 2018; Semachew, 2018).
2. BACKGROUND
Nursing as a process was described for the first time by Lydia Hall in 1955. She introduced 3 STEPs for nursing as a process: Observation, Administration of care and Validation (de la Cuesta, 1983), and Orlando, in 1961, used the term "NP" in his theory and described the process as patient behaviour, nurse response and nursing practices (Orlando, 1961). In 1967, Yura and Walsh described the NP in four steps: Assessment, Planning, Implementing and Evaluating in their book. Authors, such as Iyer, Taptich, & Bernocchi‐Losey (1995), Phaneuf, López, & Ruíz (1993) or Alvarez (1987), considered the nursing diagnosis, which was traditionally seen as part of the nursing assessment as a separate phase and described the process as containing five phases (Potter & Perry, 2017). Nowadays, the NP is a systematic problem‐solving with five steps: assessment, diagnosis, planning, implementation and evaluation to identify, prevent and treat actual or potential health problems and promote wellness (Potter & Perry, 2017). For the emphasis of the American Nursing Association (ANA) on passing the course of nursing process after formal education to upgrade their qualifications, approval of a law on the validation of nursing care based on patient care plans by the Joint Commission on the Accreditation of Hospitals (JCAH) in the 1970s and increased nurses' concern for their development as a profession due to the developments in nursing education leading to the nursing process was seen as an important means for that development (Yura & Walsh, 1978).
In a decade, it was used as a teaching tool in educational settings, and when this process was used in hospitals, it appeared useful and effective for most countries (de la Cuesta, 1983).
The acceptance and emergence of the nursing process in England were related to the professional dimension. In this period, dissatisfaction wave from the nursing care provided in the United Kingdom. Major factors of dissatisfaction include denial of a task‐orientated approach to nursing, the lack of individualized care, the low level of nurses’ job satisfaction and the superficial nature of the nurse–patient communication. The nursing process, as an antidote for the treatment of toxins, destroyed most nursing dissatisfactions in the country (de la Cuesta, 1983; Walton, 1986).
In lower‐income countries (IPNA, & Residents/Nationals of These Countries Qualify for Low‐Income Country Rates, 2018) due to the dissatisfaction of care provided by nurses, poor quality of care and nurses' dissatisfaction from their profession have led use the nursing process; since 1980, studies have begun on the implementation of the NP in the clinical settings (de la Cuesta, 1983; Vanaki & Zamanzadeh, 1994; Zamanzadeh, Valizadeh, Jabbarzadeh‐Tabrizi, Behshid, & Lotfi, 2015). In several studies, the usefulness of this process has been confirmed in accordance with the context of different countries (Semachew, 2018; Zamanzadeh et al., 2015).
However, the acceptance and application of the nursing process are clear in the high‐income countries (Di Mauro, Vanalli, Alberio, & Ausili, 2018), but in low‐income countries after about 40 years of the development of and usefulness of this process in these countries, it is not yet known how much the nursing process is implemented, the acceptability of the nursing process and the importance of this process in the clinic settings (Fernández‐Sola et al., 2011; Wagoro & Rakuom, 2015; Zamanzadeh et al., 2015).
3. AIM
To evaluate the strategies for implementing the NP in the clinical practice and the assessment of the implementation rate of this process in clinical settings of lower‐income countries.
Research question:
Is the nursing process implemented with specific strategies in lower‐income countries in the form of widely and continuously?
4. METHODS
4.1. Design
The integrative review (Whittemore & Knafl, 2005) was applied in this study. Considering that scientific information is increasing in all fields and professions nowadays, practitioners do not have enough time to review all the information on their interested background to get the most valuable information; the integrative review (IR) method is an approach that by combining different methods and examining all the findings of particular issues or subjects, and provides useful and valuable information to the researcher or practitioners on that subject (Whittemore & Knafl, 2005). Mixed studies review (MSR) can be more appropriate for decision‐makers and practitioners by providing a rich and practical understanding of complex health interventions and programmes (Pace et al., 2012). In this research, we used the Whittemore and Knafl's (2005) integrative review framework stages, which included Problem identification, Literature search, Data evaluation, Data analysis and Presentation.
4.2. Stage 1: Problem Identification
The first step in the review method is the clear identification of the problem; then, variables of interest are defined theoretically and practically. The NP has five consecutive steps, and nurses can improve the quality of their care by implementing this process. The NP as a systematic and dynamic way to deliver nursing care included five interrelated steps: assessment, diagnosis, planning, implementation and evaluation. This process is a cycle that never ends, the guideline that ensures good nursing care and improves patient outcomes (Fernández‐Sola et al., 2011; Potter & Perry, 2017). There are many effective factors in the implementation of the nursing process including knowledge of faculty members, nursing managers and nurses about the NP, the interest and attitude of nurses towards the implementation of the process, manager's support in the implementation of the NP and implementing the NP in clinical settings (Potter & Perry, 2017; Shoorideh & Ashktorab, 2011; Zamanzadeh et al., 2015).
4.3. Stage 2: Literature Search
The research question was designed based on the SPICE (setting, perspective, intervention, comparison and evaluation) framework that is more valuable than PICO (population, intervention, comparison and outcomes) framework with two statistically significant changes (Cooke, Smith, & Booth, 2012). These changes included dividing the population component into both “setting” and “perspective” and “evaluation” instead of outcomes (Andrew, 2006; Crumley & Koufogiannakis, 2002). These new concepts of the SPICE framework authenticate that data practice is a social science, not a hard science, and incorporates other concepts such as “outputs” and “impact” together with less tangible effects of a library or instructional intervention (Andrew, 2006). SPICE framework is a more appropriate framework for health and social sciences (Andrew, 2006; Eldredge, 2001) and helps practitioners to identify their practice‐based questions (Andrew, 2006). This framework was also used for matching the research design to the question, inclusion and exclusion criteria and guide the database search strategy (Andrew, 2006).
All databases were searched using the terms: (Nursing Process OR Nursing Process software OR Nursing Diagnosis OR Nursing assessment) AND (quality of care OR implementation strategies OR outcome) AND (nurse OR nurses OR registered nurses) AND (clinical setting OR hospital unit).
To determine the type of extracted studies, the method of searching, and determining the inclusion and exclusion criteria, the research group was formed on 5 May 2018. In the first, two researchers (MK and ME (health librarian)) independently searched for articles in EMBASE, MEDLINE, CINAHL, Scopus and ISI databases from 1975–July 2018 without any language restrictions. Grey literature searching was conducted using professional databases and dissertations (Masters and Ph.D.). Then, the final papers were extracted according to the inclusion and exclusion criteria of the study (Table 1). The reasons for choosing low‐income countries including Iran, Brazil, Bolivia, Taiwan, Ethiopia, Mexico and Egypt in this study were that the challenges of nursing care in their clinical settings were similar (Fernández‐Sola et al., 2011; Ledesma‐Delgado & Mendes, 2009; Rajabpoor et al., 2018; Semachew, 2018; Yeh et al., 2009).
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria |
Studies that: Published between 1975–2018 Conducted the implementation NP (manually or electronically) in the clinical setting Evaluated the relationship between the NP or nursing diagnosis and outcomes Assessment of the nursing record systems Published on the documentation of the NP Published on evaluated nursing diagnosis, facilitators and barriers to the implementation of the NP Published related to clinical settings in lower‐income countries including Iran, Brazil, Bolivia, Taiwan, Ethiopia, Mexico and Egypt Published in English or Persian language |
| Exclusion criteria |
Studies that: NP is evaluated outside the hospital Presented as a lecture Containing conference proceedings or letters to the editor. |
The initial search resulted in 4,350 records from databases and 327 records from grey literature and reference by reference based on the search terms. Subsequently, 887 papers were duplicates and excluded from the study and the total records identified were 3,790. Finally, 39 articles were identified consistent with the inclusion and exclusion criteria. The process of identifying, evaluating and selecting articles is presented based on preferred reporting items for systematic reviews and meta‐analyses (PRISMA) (Moher, Liberati, Tetzlaff, & Altman, 2009) in Figure 1.
Figure 1.
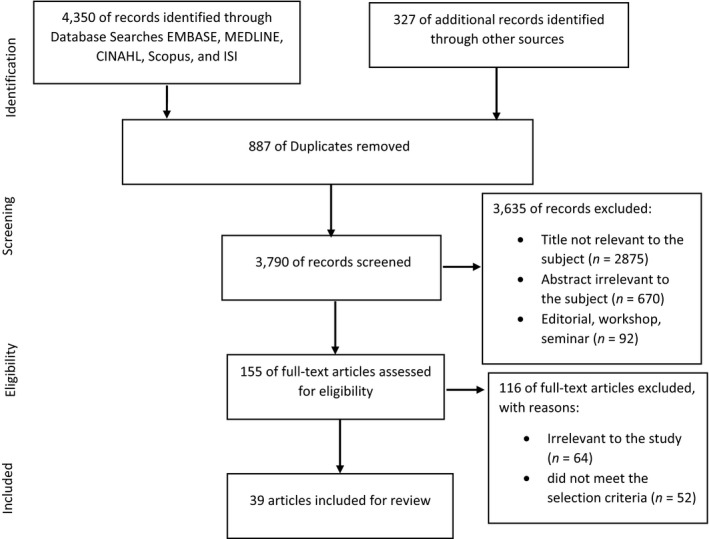
PRISMA flow chart showing article selection stages
4.4. Stage 3: Data Evaluation
Critical appraisal of methodological features is complex to evaluate the quality of studies in integrative reviews (Whittemore & Knafl, 2005). Due to lack of guidelines for evaluating research quality in integrative reviews, the Mixed Methods Appraisal Tool (MMAT) was adopted as it helps overcome challenges associated with evaluating the methodological quality of varied studies (Hong et al., 2018; Pace et al., 2012; Whittemore & Knafl, 2005). We used this method to evaluate the quality of selected studies and also to increase the validity of the study.
The Mixed Methods Appraisal Tool (MMAT) seems to be a useful and unique tool for evaluating MSR (qualitative, quantitative and mixed methods) with scores varying between 25% (meeting one criterion)–100% (meeting all four criteria) (Crowe & Sheppard, 2011). The MMAT is designed for the appraisal stage of systematic mixed studies reviews and permits to appraise the methodological quality of five categories to studies of qualitative research, randomized controlled trials, non‐randomized studies, quantitative descriptive studies and mixed methods studies (Crowe & Sheppard, 2011; Hong et al., 2018). This tool is recommended by the National Institute of Excellence in Health Services in Quebec (INESS) and increasingly popular because of their potential for addressing complex interventions and phenomena, specifically for assessing and improving clinical practice (Hong, Gonzalez‐Reyes, & Pluye, 2018).
The eligibility of articles was discussed in the research team. To appraise the papers selected in this study, at first, two reviewers independently evaluated the quality of the papers with the MMAT method, and then, it was discussed in the research team, and in cases where there were disagreements, the articles and scores of the two reviewers were examined to until consensus was reached. Articles with a score of less than 50 percent were excluded from the review. None of the studies was excluded during the quality appraisal of the articles by the research team.
According to the evaluation of studies based on MMAT, it was found that the quality of studies was moderate. The quality scores for the studies are included in Tables 2, 3 and 4. Data collection was performed in most quantitative studies using researcher‐made questionnaires; therefore, the necessity of designing and psychometrics of a functional tool seems essential for evaluating the implementation of the NP.
Table 2.
Effects of implementing the nursing process in clinical settings
| Author(s)/ year & country | Research aim | Study design | Study population | Data collection | Setting | Results/key findings | MMAT score |
|---|---|---|---|---|---|---|---|
|
(Rasouli, Hagiamiri, Mahmoudi, & Mostoufian, 1996) Iran |
In order to use the nursing process to prevent and reduce pressure ulcers in orthopaedic wards | Semi‐experimental |
Nurses (n = 30) Convenience sampling method |
Multichoice questionnaire | Orthopaedic wards of hospitals affiliated to Tehran University of Medical Sciences | Training based on the nursing process increased nurses' knowledge and change in the degree of pressure ulcer. | 50% |
|
(Rahgooy, Vanaki, Golestan, & Soulati, 1999) Iran |
For the effect of nursing process education on the quality of care provided to psychiatric patients | Experimental with control group |
Nurses (n = 44) Random sampling method |
The QualPaks standard checklist | Razi Psychiatric Center of Tehran | The quality of nursing care after the training of the case group was improved from moderate to good rather than before training and the control group. | 50% |
|
(Vanaki & Zamanzadeh, 1994) Iran |
In order to investigate the effect of nursing process implementation using problem‐based recording in quantity and quality of nurses documentation | Semi‐experimental |
Nurses (n = 42) Convenience sampling method |
Researcher checklist | The Imam Hussein Hospital Tehran | The urgent need for an accurate documentation system and the improvement in the quality and quantity of nursing documentation after the implementation. | 75% |
|
(Akbari & Farmahani, 2011) Iran |
In order to influence the nursing process on the quality of care of schizophrenic patients | Semi‐experimental with control group |
Nurses (n = 30) Convenience sampling method |
The QualPaks standard checklist | Shaheed Lavasani Hospital of Tehran | The quality of care provided in the physical–psychological needs and the relationship of the patient well‐promoted. | 50% |
|
(Oshvandi, PourYousef, & Bikmoradi, 2013) Iran |
To effect of clinical education by exploration on the skill of using nursing process by nursing students | Semi‐experimental with control group |
Nursing students (n = 38) Convenience sampling method |
Checklist | Surgical wards of Besat hospital in Hamadan | Exploration education has a more positive effect on nursing students' clinical skills learning than conventional education. | 50% |
|
(Aein & Frouzandeh, 2012) Iran |
Determining the effectiveness of conceptual mapping in nursing process learning in clinical nursing education in children | Semi‐experimental |
Nursing students (n = 30) Convenience sampling method |
Checklist | Shahrekord Children's Hospital | Quantitative and qualitative evaluation of conceptual maps showed a statistically significant progression of students in understanding the nursing process, which improved from the weak level on the first day to the excellent level on a ninth day. | 50% |
|
(Habibzadeh, Khajehali, Khalkhali, & Mohammadpour, 2013) Iran |
To analyse the impact of evidence‐based nursing education on five scopes of nursing process among nursing students. | Quasi‐experimental study with control group |
Nursing students (n = 48) Convenience sampling method |
Checklist | Orthopaedic wards of Orumieh Hospital | Members of the intervention group had better performance in all five scopes of the nursing process in comparison with the control group. | 50% |
|
(Rastian, Borzabady Farahani, Rasouli, Sarbakhsh, & Niromand, 2014) Iran |
To determine the effect of nursing process implementation on quality of nursing care of patients hospitalized in surgical wards | Quasi‐experimental study with before–after design |
Nurses (n = 48) Purposive sampling method |
Quality patient care scale (QualPacS) checklist | Surgical wards of teaching hospitals affiliated to Yasoj Medical University | Nursing process implementation can improve the quality of nursing care of patients in surgical wards. | 50% |
|
(Zamanzadeh et al., 2015) Iran |
Carried out to assess the key challenges associated with the implementation of the nursing process | Systematic review | 125 articles were selected from databases of Iranmedix, SID, MagIran, PUBMED, Google scholar and ProQuest, which were assessed using the main keywords of nursing process and nursing process systematic review | ‐ | Tabriz University of Medical Sciences | Main challenges include intangible understanding of the concept of the nursing process, different views of the process, lack of knowledge and awareness among nurses related to the execution of process, supports of managing systems and problems related to recording the nursing process. | 50% |
|
(Khosravan, Saadat, & Moradi Kosha, 2014) Iran |
To determine the effect of nursing process on job satisfaction of employed nurses | Semi‐empirical study |
Nurses (n = 47) by census methods |
Manokian questionnaire and process registration checklists of Hasson and Arnetz | Intensive care units of Gonabad hospitals | The nursing process is beneficial in clinical settings also leads to job satisfaction of nurses. | 75% |
|
(Lotfi Mojgan, 1998) Iran |
In order to effect the implementation of the nursing process on the quality of nursing care from patients admitted in critical care units | Quasi‐experimental study |
Patients (n = 52) Convenience sampling method |
Questionnaire made by researcher | Intensive care units | The implementation of the nursing process showed a small effect on the quality of nursing care in critical care units. | 75% |
|
(Rahmani et al., 2016) Iran |
To determine the effect of nursing process the way "accessible care cards" on patients' satisfaction from care in intensive care units | Cross‐sectional interventional study | patients (n = 76) | Questionnaire made by researcher | Intensive care units in the Golestan hospital in Ahwaz | Implementation of the nursing process, in a manner of available cards, led to an increase in patient satisfaction compared with the routine manner | 50% |
|
(Yeh et al., 2009) Taiwan |
To develop and implement NPSSC enabling computerized documentation for nursing home residents, evaluate the efficiency of NPSSC, obstacles to the use of the NPSSC and assess nurse users’ satisfaction with the NPSSC | Quasi‐experimental one group pre‐/post‐test | Nurses (n = 27) & medical records (n = 396) | Satisfaction Questionnaire and checklist efficacy of the NPSSC | Nursing home residents in Taiwan |
Obstacles use of the NPSSC was identified. The use of the NPSSC significantly improved nursing documentation in that resident's records were organized and consistent and nurses were able to complete a comprehensive care plan in 48 hr. Nurses' satisfaction with nursing documentation increased. |
100% |
|
(Semachew, 2018) Ethiopia |
To evaluate the implementation of the nursing process at three randomly selected governmental hospitals | Hospital‐based descriptive and retrospective study design |
Records (n = 338) Samples were proportionally allocated for each hospital based on the total number of inpatients in the last 6 months |
Nursing process implementation checklist | Governmental hospitals | Nursing process documentation should be promoted and nursing managers should supervise the implementation of the nursing process and facilities its implementation. | 50% |
|
(Fernández‐Sola et al., 2011) Bolivia |
To identify those factors that favours or hinder the NP implementation and the SCP both in the clinical areas and academic environment | Participatory action research | Research team and nurses (n = 35) | Meetings with key informants, Interviews, observation and workshops | Hospitals and universities | The implementation of standard care plans requires much effort. Making the most of cooperation projects to make improvements and undertake scientific research is an excellent opportunity to promote the nursing profession in less‐developed countries. | 75% |
|
(Lopes et al.., 2010) Brazil |
To evaluate how the nursing process has been registered at a Brazilian teaching hospital | Descriptive and retrospective study | Medical records (n = 68). | Researcher‐made form | Women's Hospital CAISM/UNICAMP, a public tertiary university hospital | All steps in the nursing process were not documented, especially the nursing diagnosis. | 50% |
|
(Lima & Kurcgant, 2007) Brazil |
To understand the meanings nurses at a university hospital attribute to the implementation process of the Nursing Diagnosis Classification System (DEn) as a phase in the Nursing Care System | Qualitative methodological approach | Nurses (n = 8) | Interviews | Hospital | Throughout the process, with the gradual increase in theoretical–practical training and participation, the collaborators became agents of change, disclosing a positive transformation in their feelings, after their initial discomfort and unfavourable perception about the implementation of the nursing diagnosis in the NCS. | 50% |
|
(Ledesma‐Delgado & Mendes, 2009) Mexican |
To understand the meanings attributed to the nursing process by clinical nurses at a Mexican hospital | Qualitative study based on grounded theory | Nurses (n = 16) | Semi‐structured interviews, participant observation and document research | Medicine unit at the General Hospital | The nursing process was described as a nursing care routine that different from what was taught at the university. | 75% |
Table 3.
Development and application of electronic software in "the nursing process"
| Author(s)/ year & country | Research aim | Study design | Study population | Data collection | Setting | Results/key findings | MMAT score |
|---|---|---|---|---|---|---|---|
|
(Paese et al., 2018) Brazil |
To structure and organize the data and information of the computerized nursing process through ICNP® version 2.0 for emergency units | Hybrid research with quantitative and technological production in 5 stages | Nurses | The data organized in Excel worksheets and divided by human systems and degrees of complexity | Emergency care units | In the emergency ward, it was found that ICNP has a strong and solid form for the development of the computerized nursing process able to support nurses in safe decision‐making to improve the quality of health care. | 50% |
|
(Dal G.T Sasso, Peres, & Silveira, 2006) Brazil |
Describing the development of the computerized nursing process in intensive therapy from the CIPE version Beta 2 and demonstrating the contributions to the improvement of nurse care | Methodological study and technological production in three phases | Nurses (n = 5) | Semi‐structured questionnaire | CCU ward of hospital | The programme allows a continuous learning and explicit clinical decision‐making of the nurse. | 75% |
|
(G. T. M. Dal Dal Sasso et al., 2013) Brazil |
To examine the relationship between the data and information in the nursing process, which were computerized according to ICNP version 1.0 and to establish associations between detailed clinical evaluations of each human system and diagnoses, interventions and patient outcomes. | Technological product and a methodological study in three main steps | Nurses and students in the ICU and Emergency units of hospital | General meetings to review associations and enter data. | ICU and Emergency units of hospital | The success of this technology lies in its achievement of the integration of research, professional practice and teaching. Also, provide support for decision‐making with associations between clinical evaluations, diagnoses, interventions and the results. | 75% |
|
(Sperandio & Evora, 2009) Brazil |
To demonstrate that high‐tech solution can give nurses more time for direct patient care | Descriptive/exploratory study | Nurses (n = 11) | ‐ | School hospital of the state of Sao Paulo | He results showed that the incorporation of the mobile, wireless computer technology in the nursing care process provided an environment with mobility for actions and made communication and documentation of the care easier. | 50% |
|
(Silva, Evora, & Cintra, 2015) Brazil |
To develop software to support decision‐making in the selection of nursing diagnoses and interventions for children and adolescents. | Methodological applied study based on software engineering, as proposed by Pressman, developed in three cycles | Nursing professionals and students | ‐ | University hospital in Paraiba | This software improves the quality of nursing care and nursing decision‐making skills, and it also facilitates the documentation of nurses. | 50% |
|
(Mazlom & Rajabpoor, 2014) Iran |
To design and assess the local nursing process computerized software | Two phases of software design and assessment: | Students and nurses (n = 20) were convenience sampling method | Researcher‐made questionnaire | ICU ward of Ghaem hospital in Mashhad | Application of this software leads to increased accuracy, decreased error and shared labour that is counted as factors promoting patient care services. | 75% |
|
(Sayadi & Rokhafroz, 2013) Iran |
To study nursing students’ opinions about a nursing process mobile software (as a means for facilitating nursing process implementation) for bedside use | Pre‐experimental study | Nursing students (n = 30) | Researcher‐made questionnaire | Cardiology ward of Golestan hospital in Ahvaz | Using this software and can improve the clinical skills of nursing students and encourage them to learn and implement the nursing process. | 50% |
|
(Lima et al., 2018) Brazil |
To construct a mobile technology capable of assisting the nurse in performing nursing prescription in neonate patients | Methodological study with a qualitative approach in three phases | Nurses | Ruby on Rails, IONIC 2, Postgres SQL and Amazon EC2 | Neonatal units of hospital | Computerized tool the nursing process, facilitated the data collection, diagnostic reasoning and identification and grouping of the clinical signs indicated by the newborn in neonatal units. | 75% |
|
(Domingos et al., 2017) Brazil |
To identify in the literature the evidence on the use of nursing process applied to software | Integrative review | Articles (n = 23) | The selected articles were evaluated for the level of evidence | Federal University of Viçosa | Two categories of analysis include development and use of software and, in general, the use of NP software enhances nursing practice. | 50% |
Table 4.
Factors affecting the implementation of the nursing process
| Author(s)/year & country | Research aim | Study design | Study population | Data collection | Setting | Results/key findings | MMAT score |
|---|---|---|---|---|---|---|---|
|
(Akbari & Shamsi, 2011) Iran |
To diagnose the nursing process barriers from the perspective of the intensive care units’ nurses | Cross‐sectional descriptive study |
Nurses (n = 63) based on cluster‐random sampling method |
Questionnaire | Hospitals of Tehran | The most important individual and managerial barriers were determined to include lack of sufficient information about the concept of the nursing process and lack of belief in doing the patient care according to the nursing process and lack of enough time for doing the nursing process due to the excessive number of the patients. | 50% |
|
(Nohi, Karimi, & Najmaei, 2010) Iran |
Determining the different barriers to practical application of nursing process from the point of view of nursing managers and nursing students | Descriptive study | All nurse managers (n = 103) and senior nursing students (n = 50) with Census sampling | Researcher‐made questionnaire | Hospitals of Kerman University of Medical Sciences | Most of the obstacles in both groups were related to the barriers of execution of 75%, and the minimum barriers to scientific barriers were 12 per cent. | 50% |
|
(AtashzadehShoorideh & Ashktorab, 2011) Iran |
To explore the factors that may influence the implementation of nursing process by nurses | Qualitative research based on grounded theory | Nurses, nurse educators and nurse managers (n = 36) with purposeful and theoretical sampling | Semi‐structured interviews | Shahid Beheshti University of Medical Sciences | Factors which influence the implementation of the nursing process by nurses are varied and complex and related to personal and managerial factors. | 75% |
|
(Ghafouri Fard et al., 2012) Iran |
Identifying barriers to implementing nursing process from the point of view of nursing faculty members and students | Cross‐sectional descriptive study | Faculty members (n = 14) and students (n = 48) | Researcher‐made questionnaire | Nursing and Midwifery Faculty of Zanjan | The lack of adequate knowledge of the concept of the nursing process, its inadequate learning and the lack of supervision and follow‐up of nursing officials in implementing this process were identified as the most important barriers to individual and managerial management in the implementation of the nursing process. | 50% |
|
(Mohammadi et al., 2016) Iran |
To determine the nursing process barriers from the view of the nurses and nurse managers | Descriptive cross‐sectional study | Nurses (n = 73) and nurse managers (n = 17) with Census sampling | Researcher‐made questionnaire | Surgical wards of Imam Reza hospital | It was determined that not having knowledge of the concept of the nursing process as the most important individual barrier and not having enough time to implement the nursing process was identified as the most important management barrier due to a large number of patients. | 50% |
|
(Matbouei, Mohammadi, & Zargarzadeh, 2013) Iran |
To assess nurses and nurse manager's point of view about the barriers to documenting the nursing diagnosis | Descriptive cross‐sectional approach to problem‐solving | Nurses and nursing managers (n = 97) | Researcher‐made questionnaire | Trbiat‐e‐Modares university of Tehran | The main obstacles to recording nursing diagnosis are numerous written works by nurses, transfer of non‐nursing activities to nurses, not assigning privileges to nurses who identify and record nursing diagnosis, failure to perform a care system for each patient individually and lack of in‐service training. | 50% |
|
(Rajabpoor et al., 2018) Iran |
To determine the barriers to the implementation of the nursing process from the viewpoint of the faculty members, nursing managers, nurses and nursing students | Analytical cross‐sectional study | Nursing lecturers and students (n = 90) and nurses and nursing managers (n = 134) were selected by convenience sampling method | Research‐oriented questionnaire | Mashhad University of Medical Sciences | The lack of a checklist for recording the process in the medical records of the patients, the high number of patients under the care of each nurse and the lack of a principal training of the nursing process during their studentship were the most important obstacles to the implementation of the nursing process. | 75% |
|
(Lee, 2005) Taiwan |
To explore factors that may affect nurses’ use of nursing diagnoses in charting standardized nursing care plans in their daily practice. | Qualitative research | Nurses (n = 12) | Interviews | Medical Center in Taiwan | Nurses were reluctant to match the patient's condition with nursing diagnosis and care required due to lack of knowledge about nursing diagnosis, nursing care programme and interventions. | 75% |
|
(Takahashi et al., 2008) Brazil |
To identify the difficult and easy aspects of performing the different stages of the nursing process, according to the reports of nurses | Descriptive/exploratory study | Nurses (n = 83) | Questionnaires (both structured and open‐ended) | The university hospital belonging to that institution |
The most important obstacle to the implementation of the nursing process is the lack of knowledge associated with theoretical and practical knowledge phases of the nursing process. Nurses also had difficulty in applying and recording nursing diagnosis and evaluation. |
75% |
|
(Shewangizaw & Mersha, 2015) Ethiopia |
To assess factors affecting implementation of nursing process among nurses | Cross‐sectional study | Nurses (n = 105) randomly sampling method | Self‐administered pre‐tested semi‐structured questionnaire and observational checklist | Arbaminch General Hospital | The study has identified a lack of facility from organizational factors, economic status of the patient to collect material for nursing care, early discharge, lack of cooperation and complicated problems from patient‐related factors and level of knowledge were among those factors highly affecting nursing process implementation. | 75% |
|
(Manal & Bayoumy, 2014) Egypt |
To explore barriers and facilitators for execution of nursing process from nurses' perspective. | Descriptive exploratory design | Nurses (n = 148) Convenience sampling method | Questionnaire | Najran General Hospital and King Khalid Hospital | Data collection identified by the majority as the difficult phase. Nurses identified barriers related to work as the most commonly encountered barriers. | 50% |
|
(Aseratie, Murugan, & Molla, 2014) Ethiopia |
To assess factors affecting implementation of nursing process among nurses in selected governmental hospitals | Cross‐sectional quantitative study | Nurses (n = 202) Simple random sampling method | Questionnaire | Governmental hospitals at Addis Ababa | Organizational factors, patient‐related factors and level of knowledge and skill were among those factors highly influenced nursing process implementation. | 50% |
4.5. Data analysis
The data analysis stage is one of the most difficult aspects and potentially fraught with error. Similar data are categorized and grouped, after compared data. Then, these coded categories are compared which improves the analysis and synthesis process (Whittemore & Knafl, 2005). The first, to manage data for a better understanding and enhance the visualization of patterns, shows the relationships between primary data sources, and the following characteristics are considered as the initial subgroups: author, country, year, study design, data collection and results. Then, data synthesis from the selected studies was coded by highlighting relevant parts of the text and assigning code words to these areas. Following this, an iterative process was used to develop categories by combining codes. Descriptive themes were attached to each category and are discussed in data comparison (Dal Sasso et al., 2013; Frigstad, Nøst, & André, 2015; Ghafouri Fard et al., 2012; Ledesma‐Delgado & Mendes, 2009; Mazlom & Rajabpoor, 2014; Mohammadi, Ghafori Fard, & Esmaeilivand, 2016; Rahmani, Alijani, Dashtbozorge, & Haghighizadeh, 2016; Rajabpoor et al., 2018; Semachew, 2018; Zamanzadeh et al., 2015).
4.5.1. Ethic
Given that this review article was part of a Ph.D. thesis, a code of ethics was obtained from the Ethics Committee with number: IR.TBZMED.REC.1397.170.
5. RESULTS
Of the 39 studies identified in this review, 18 (46%) focused on the effects of implementing the nursing process in the clinical setting, nine focused (23%) addressed the development and application of software to support the NP, and 12 (31%) discussed factors that affected the implementation of the NP. The papers studied were mainly quantitative papers, and fourteen articles were conducted using descriptive, exploratory and cross‐sectional design. Twelve articles were conducted using the quasi‐experimental or RCT research design, five articles were conducted using technological products and methodological studies, five articles were conducted using qualitative research design, and three articles were conducted using the review articles. Most quantitative studies used researcher‐made questionnaires to collect the required information.
After data are compared with each other to identify the specific patterns of studies and the precise and important themes in them, three themes were identified that the description of each is given below:
Effects of implementing the NP in clinical settings
Development and application of electronic software in the NP
Factors affecting the implementation of the NP.
6. EFFECTS OF IMPLEMENTING THE NP IN CLINICAL SETTINGS
Of the 39 studies reviewed, 18 studies were studied in this scope (Table 2). The implementation of the NP in the clinical practice improves the quality of nursing care, increases the quantity and quality of the curriculum, improves nurses “knowledge, improves the quality and quantity of nurses” documentation and increases job satisfaction and self‐efficacy.
7. DEVELOPMENT AND APPLICATION OF ELECTRONIC SOFTWARE IN THE NP
Nine studies were examined on designing NP software and its application (Table 3). The NP electronically documentation is a reliable tool for measuring the quality of diagnostic documents, interventions and nursing outcomes and more efficient than a manual documentation system. The development of this tool and its application can help in decision‐making and quality of care. It also reduces errors and increases the care of nurses in inpatient care.
8. FACTORS AFFECTING THE IMPLEMENTATION OF THE NP
Out of 12 studies on the factors influencing the implementation of the NP, 6 papers examined the barriers to the implementation of the NP, 6 studied on the factors affecting the implementation of the process, and its barriers have been discussed (Table 4). In general, the factors affecting the implementation of the NP can be divided into two categories, individual factors and management factors.
The following factors were considered as individual factors: inadequate knowledge of faculty members from the concept of NP and consequently poor learning by students and nurses and nurses' lack of desire to implement NP in the clinical practice due to low knowledge.
Management factors include shortage or lack of infrastructure for the implementation of NP, incomplete documentation system in nursing reports, nurses' high workload, nursing staff shortages in hospitals, weak in in‐service training, lack of supervision of managers on implementation of NP, lack of punishment and encouragement for the implementation of the process and lack of support nursing institutions for the implementation of the NP.
8.1. Stage 4: Presentation
In the final stage of the framework, more precise details of the primary sources and evidence as a logical chain to provide a result consistent with the findings provide for the reader of the review (Whittemore & Knafl, 2005).
Studies that conducted the NP manually or electronically in the clinical practice did not indicate the way of patient's assessment, signs and symptoms specific to any nursing diagnosis, the number of nursing diagnoses that were recorded in the software or that they were trained and the number of diagnoses that nurses identified after completing the process at the wards (Cho & Park, 2003; Dal Sasso et al., 2013; Di Mauro et al., 2018; Dykes et al., 2007; Frigstad et al., 2015; Lima & Kurcgant, 2007; Lima, Vieira, & Nunes, 2018; Lopes, Higa, Reis, Oliveira, & Christóforo, 2010; Mazlom & Rajabpoor, 2014; Minthorn & Lunney, 2012; Paese et al., 2018; Rahmani et al., 2016; Saba & Feeg, 2005; Sayadi & Rokhafroz, 2013; Semachew, 2018; Silva, Évora, & Cintra, 2015; Zamanzadeh et al., 2015).
Studies of Mazlom and Rajabpoor (2014) and Sayadi and Rokhafroz (2013) was done on the software design of the NP, and the software testing was limited to one ward of a hospital and was not used in other wards or other hospitals in Iran. And their software became for the lack of implementation of this software in hospitals, the lack of necessary infrastructures and the lack of supporting by responsible institutions. Virtually, the NP in Iran is not executed either manually or electronically. Moreover, except for the study of Dal Sasso et al. (2013) and Saba and Feeg (2005), information on the use of others designed the NP software in other countries is not available.
9. DISCUSSION
Based on the findings of this study, it was found that the nursing process can be used continuously and extensively in lower‐income countries. The findings of the study indicate that the nursing process is consistent with the context of clinical settings in these countries (Manal & Bayoumy, 2014; Semachew, 2018; Zamanzadeh et al., 2015).
The NP is accepted as a care standard with the stages of assessment, nursing diagnosis, planning, implementation and evaluation in the world. The NP has been of great help for nurses in the development of the nursing profession, nursing research and facilitating management activities in nursing (Potter & Perry, 2017).
The implementation of this process increases patients' satisfaction due to an increase in patient–nurse communication, improves the quality of nursing care and documentation. If the nursing process is implemented electronically, it saves time and nursing errors are reduced (Ghafouri Fard et al., 2012; Rajabpoor et al., 2018; Semachew, 2018; Takahashi, Barros, Michel, & Souza, 2008). But, in lower‐income countries for three reasons, the NP is not conducted extensively and continuously at the hospitals or performed very poorly: low proficiency of faculty members from the concept of the NP, lack of necessary infrastructure and lack of supporting nursing institutions and managers (Rahmani et al., 2016; Rajabpoor et al., 2018; Semachew, 2018).
Faculty members do not provide the necessary conditions for transferring student learning from the knowledge stage to the application stage and higher levels of Bloom's taxonomy (Anderson & Sosniak, 1994; Johnsen, Fossum, Vivekananda‐Schmidt, Fruhling, & Slettebo, 2016).
The lack of infrastructures such as lack of appropriate nursing documentation system manually, lack of software NP, poor HIS in hospitals, lack of standard tools for assessing nursing care based on NP and lack of tools supervising the implementation of the NP is the second reason that the nursing process is not implemented in these countries (Rahmani et al., 2016; Rajabpoor et al., 2018; Semachew, 2018).
The third reason for not institutionalizing the NP in lower‐income countries (lack of supporting nursing institutions and managers) includes lack of belief in improving the quality of nursing care based on the NP, lack of supervision on the implementation of the NP at the time of implementation as a pilot, lack of appropriate encouragement and punishment system, increased workload of nurses by caring for a large number of patients, shortage of nursing staff and lack of awareness of the concept of the NP (Akbari & Farmahani, 2011; Mohammadi et al., 2016; Takahashi et al., 2008; Parvan, Hosseini, & Bagherian, 2018).
With these problems, even if a nurse has a high degree of critical thinking, this thinking will be suppressed gradually, and he/she should be taken care of the patient in accordance with traditional nursing care. Also, they will not have an attitude towards the NP or that their attitude may be negative. Specifically, when the nurse does not have enough knowledge about the NP, there are no available facilities in the hospital, supervision and support for the NP is not available, and nurses will not have a good attitude towards the NP.
The use of the NP, especially the nursing diagnosis stage, allows nurses to use critical thinking for their clinical judgement and their clinical care activities (Ghanbari et al., 2017; Wolter Paans, Sermeus, Nieweg, & Van der Schans, 2010). The NP with critical thinking as a flexible tool and along with the contemporary integrate nursing philosophy ensures the high quality of care (Rahmani et al., 2016).
The existence of the NP by electronic means provides a valuable opportunity for nurses and nursing students to improve their clinical performance (Frigstad et al., 2015). Due to legal issues, nurses spend a lot of time writing their reports; if the NP is implemented electronically, this writing time will be reduced and nurses will have more time to evaluate the patient and pay attention to them (Semachew, 2018). Its implementation requires a lot of effort by nursing institutions and administrators because most nurses have little knowledge about the NP (Aein & Frouzandeh, 2012; Semachew, 2018).
The institutionalization of the NP in hospitals and its continuous implementation by nurses will depend on countries' economic, educational and access to care services. In the United States of America and Europe, this process despite numerous challenges runs manually or electronically (Di Mauro et al., 2018; Zamanzadeh et al., 2015).
The acceptance and emerge of this process in the clinical settings in the United States can be examined through two dimensions: sociological dimension and professional dimension (de la Cuesta, 1979). These two dimensions led to the massive movement to lead the nursing towards professional. The NP was a professional strategy for nurses in accordance with contemporary American society (de la Cuesta, 1983).
The acceptance and emergence of the NP in the high‐income countries including England, Italy, Switzerland, South Korea and China were related to the professional dimension. Dissatisfaction wave from the nursing care provided in these countries. Major factors of dissatisfaction include dissatisfaction of care provided by nurses, poor quality of care and nurses' dissatisfaction from their profession and denial of a task‐orientated approach to nursing. But with the implementation of the nursing process in these countries, many problems and dissatisfaction have solved (de la Cuesta, 1983; Semachew, 2018).
10. CONCLUSION
The NP as a scientific standard improves the quality and quantity of nursing care and documentation, and save time and cost with its implementation as electronically; improves nurse‐patient communication and with evidence‐based nursing care; and promotes critical thinking in nurses. Therefore, lower‐income countries must provide the necessary background for the implementation of this process.
11. RELEVANCE TO CLINICAL PRACTICE
Top managers and institutions of nursing should provide infrastructures such as e‐NP (electronically of NP) in the clinical settings; then, they will support the implementation of the NP, increase their supervision over the implementation of NP and increase nurses' motivation to nursing care based on the NP and designing a checklist for NP monitoring and attached them to patients' records. Therefore, appropriate policies must be adopted to implement the nursing process in the clinical settings of the lower‐income countries in the form of widely and continuously.
Considering the inadequate knowledge of nurses and faculty members about the NP, nursing diagnosis textbooks in accordance with the context of the country must be translated and used in clinical practice and nursing process training courses are also mandatory for graduate nurses.
An appropriate tool for assessing the quality of nursing care based on the NP is not psychometric, native software tailored to each country and in accordance with international standards in lower‐income countries has not been widely used, and the NP is still not implemented in these countries. Therefore, studies with instrumental research, software development and action research are necessary to institutionalize the NP.
CONFLICTS OF INTEREST
No conflicts of interest declared.
ETHICAL APPROVAL
Approval code of ethics with number: IR.TBZMED.REC.1397.170.
ACKNOWLEDGEMENTS
This review article is part of PhD thesis in Tabriz University of Medical Sciences and was supported by the research deputy of Tabriz University of Medical Sciences, and we would like to thank Naser Khalilzad and Tabriz University of Medical Sciences for the guidance and resources provided for this review.
Lotfi M, Zamanzadeh V, Valizadeh L, Khajehgoodari M, Ebrahimpour Rezaei M, Khalilzad MA. The implementation of the nursing process in lower‐income countries: An integrative review. Nursing Open. 2020;7:42–57. 10.1002/nop2.410
Funding information
The funding was provided by Tabriz University of Medical Sciences, Tabriz, Iran.
REFERENCES
- Aein, F. , & Frouzandeh, N. (2012). Investigating the efficacy of concept mapping in student’s learning of the nursing process of pediatric patients. Journal of Shahrekord University of Medical Sciences, 14(2), 55–63. http://eprints.skums.ac.ir/id/eprint/3893 [Google Scholar]
- Akbari, K. M. , & Farmahani, F. B. (2011). The effect of nursing process education on nursing care quality of schizophrenic patients. Feyz Journal of Kashan University of Medical Sciences, 15(1), 32–37. http://feyz.kaums.ac.ir/article-1-1103-en.html [Google Scholar]
- Akbari, M. , & Shamsi, A. (2011). A Survey on Nursing Process Barriers from the Nurses’ View of Intensive Care Units. Iranian Journal of Critical Care Nursing, 3(4), 181–186. [Google Scholar]
- Alvarez, M. G. (1987). Methodology in nursing: A necessary goal. Rev Enferm, 10(101), 22–26. [PubMed] [Google Scholar]
- Anderson, L. W. , & Sosniak, L. A. (1994). Bloom's taxonomy. Chicago, IL: University of Chicago Press. [Google Scholar]
- Andrew, B. (2006). Clear and present questions: Formulating questions for evidence based practice. Library Hi Tech, 24(3), 355–368. 10.1108/07378830610692127 [DOI] [Google Scholar]
- Aseratie, M. , Murugan, R. , & Molla, M. (2014). Assessment of factors affecting implementation of nursing process among nurses in selected governmental hospitals, Addis Ababa, Ethiopia: Cross Sectional Study. Journal of Nursing Care, 3(3), 170. [Google Scholar]
- AtashzadehShoorideh, F. , & Ashktorab, T. (2011). Factors influencing implementation of nursing process by nurses: A qualitative study. Knowledge & Health, 6(3), 16–23. [Google Scholar]
- Cho, I. , & Park, H.‐A. (2003). Development and evaluation of a terminology‐based electronic nursing record system. Journal of Biomedical Informatics, 36(4), 304–312. 10.1016/j.jbi.2003.09.004 [DOI] [PubMed] [Google Scholar]
- Cooke, A. , Smith, D. , & Booth, A. (2012). Beyond PICO: The SPIDER tool for qualitative evidence synthesis. Qualitative Health Research, 22(10), 1435–1443. [DOI] [PubMed] [Google Scholar]
- Crowe, M. , & Sheppard, L. (2011). A review of critical appraisal tools show they lack rigor: Alternative tool structure is proposed. Journal of Clinical Epidemiology, 64(1), 79–89. 10.1016/j.jclinepi.2010.02.008 [DOI] [PubMed] [Google Scholar]
- Crumley, E. , & Koufogiannakis, D. (2002). Developing evidence‐based librarianship: Practical steps for implementation. Health Information & Libraries Journal, 19(2), 61–70. 10.1046/j.1471-1842.2002.00372.x [DOI] [PubMed] [Google Scholar]
- Dal Sasso, G. T. M. , Barra, D. C. C. , Paese, F. , Almeida, S. R. W. D. , Rios, G. C. , Marinho, M. M. , & Debétio, M. G. (2013). Computerized nursing process: Methodology to establish associations between clinical assessment, diagnosis, interventions and outcomes. Revista Da Escola De Enfermagem Da USP, 47(1), 242–249. 10.1590/S0080-62342013000100031 [DOI] [PubMed] [Google Scholar]
- de la Cuesta, C. (1979). Nursing process: From theory to implementation, MSc thesis, unpublished. London University. [Google Scholar]
- de la Cuesta, C. (1983). The nursing process: From development to implementation. Journal of Advanced Nursing, 8(5), 365–371. 10.1111/j.1365-2648.1983.tb00459.x [DOI] [PubMed] [Google Scholar]
- Di Mauro, S. , Vanalli, M. , Alberio, M. , & Ausili, D. (2018). Developing a subset of ICNP nursing diagnoses for medical and surgical hospital settings, informed by an Italian nursing conceptual model: A multicenter cross‐sectional study. Annali Di Igiene, 20(1), 21–33. 10.7416/ai.2018.2192 [DOI] [PubMed] [Google Scholar]
- Domingos, C. S. , Boscarol, G. T. , Brinati, L. M. , Dias, A. C. , de Souza, C. C. , & de Oliveira Salgado, P. (2017). The application of computerized nursing process: Integrative review. Enfermería Global, 16(4), 637–652. [Google Scholar]
- Dykes, P. C. , Carroll, D. L. , Benoit, A. , Coakley, A. , Chang, F. , Empoliti, J. , … Li, Q. (2007). A randomized trial of standardized nursing patient assessment using wireless devices. AMIA Annual Symposium Proceedings, 2007, 206–210. [PMC free article] [PubMed] [Google Scholar]
- Eldredge, J. (2001). The most relevant and answerable research questions facing the practice of health sciences librarianship. Hypothesis, 15(1), 9–17. [Google Scholar]
- Fernández‐Sola, C. , Granero‐Molina, J. , Aguilera‐Manrique, G. , Peredo‐de Gonzales, M. , Castro‐Sánchez, A. , & Perez Galdeano, A. (2011). Strategies to develop the nursing process and nursing care plans in the health system in Bolivia. International Nursing Review, 58(3), 392–399. 10.1111/j.1466-7657.2011.00884.x [DOI] [PubMed] [Google Scholar]
- Frigstad, S. A. , Nøst, T. H. , & André, B. (2015). Implementation of free text format nursing diagnoses at a University Hospital’s Medical Department. Exploring Nurses’ and Nursing Students’ Experiences on Use and Usefulness. A qualitative study. Nursing Research and Practice, 2015, 179275 10.1155/2015/179275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghafouri Fard, M. , Haririan, H. , Aghajanloo, A. , Akbari, M. , & Shirvani, Y. (2012). Obstacles of nursing process application from perspective of the nursing instructor and nursing students in Zanjan Faculty of Nursing and Midwifery. Journal of Medical Education Development, 5(8), 69–77. [Google Scholar]
- Ghanbari, A. , Monfared, A. , Hoseinzadeh, T. , Moaddab, F. , & Sedighi, A. (2017). The impact of the nursing process education on critical thinking of nursing students. Research in Medical Education, 9(2), 25–33. 10.29252/rme.9.2.33 [DOI] [Google Scholar]
- Habibzadeh, H. , Khajehali, N. , Khalkhali, H. , & Mohammadpour, Y. (2013). Effect of evidence‐based nursing training on nursing students ability in executive skill of nursing process in Urmia University of Medical Sciences, 2013. Journal of Nursing and Midwifery Urmia University of Medical Sciences, 11(4), 284–292. [Google Scholar]
- Hagos, F. , Alemseged, F. , Balcha, F. , Berhe, S. , & Aregay, A. (2014). Application of nursing process and its affecting factors among nurses working in Mekelle Zone Hospitals. Northern Ethiopia. Nursing Research and Practice, 2014, 675212 10.1155/2014/675212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong, Q. N. , Gonzalez‐Reyes, A. , & Pluye, P. (2018). Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). Journal of Evaluation in Clinical Practice, 24(3), 459–467. 10.1111/jep.12884 [DOI] [PubMed] [Google Scholar]
- Hong, Q. N. , Fàbregues, S. , Bartlett, G. , Boardman, F. , Cargo, M. , Dagenais, P. , … O’Cathain, A. (2018).The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Education for Information (Preprint). 1–7. [Google Scholar]
- IPNA, & Residents/Nationals of These Countries Qualify for Low‐Income Country Rates (2018). http://ipna2019.org/wp-content/uploads/2019/01/Low-income-country-list.pdf.2009/02/04. 2019.
- Iyer, P. W. , Taptich, B. J. , & Bernocchi-Losey, D. (1995). Nursing process and nursing diagnosis, (3rd ed.). Philadelphia, PA: WB Saunders Company. [Google Scholar]
- Johnsen, H. M. , Fossum, M. , Vivekananda‐Schmidt, P. , Fruhling, A. , & Slettebo, A. (2016). Teaching clinical reasoning and decision‐making skills to nursing students: Design, development and usability evaluation of a serious game. International Journal of Medical Informatics, 94, 39–48. 10.1016/j.ijmedinf.2016.06.014 [DOI] [PubMed] [Google Scholar]
- Khosravan, S. , Saadat, S. , & Moradi Kosha, F. (2014). The effect of nursing process application on Job satisfaction in Intensive Care Units. Scientific Journal of Hamadan Nursing & Midwifery Faculty, 22(2), 33–42. [Google Scholar]
- Ledesma‐Delgado, E. , & Mendes, M. M. (2009). The nursing process presented as routine care actions: Building its meaning in clinical nurses' perspective. Revista Latino‐Americana De Enfermagem, 17(3), 328–334. 10.1590/S0104-11692009000300008 [DOI] [PubMed] [Google Scholar]
- Lee, T. T. (2005). Nursing diagnoses: Factors affecting their use in charting standardized care plans. Journal of Clinical Nursing, 14(5), 640–647. 10.1111/j.1365-2702.2004.00909.x [DOI] [PubMed] [Google Scholar]
- Lima, A. F. , & Kurcgant, P. (2007). Implementation of nursing diagnosis at a university hospital: A participatory experience. Rev Gaucha Enferm, 28(4), 576–581. 10.1590/S0104-11692006000500005 [DOI] [PubMed] [Google Scholar]
- Lima, J. J. , Vieira, L. G. D. , & Nunes, M. M. (2018). Computerized nursing process: Development of a mobile technology for use with neonates. Rev Bras Enferm, 71(suppl 3), 1273–1280. 10.1590/0034-7167-2017-0267 [DOI] [PubMed] [Google Scholar]
- Lopes, M. D. M. , Higa, R. , Reis, M. D. , Oliveira, N. D. , & Christóforo, F. (2010). Evaluation of the nursing process used at a Brazilian teaching hospital. International Journal of Nursing Terminologies and Classifications, 21, 116–123. 10.1111/j.1744-618X.2010.01157.x [DOI] [PubMed] [Google Scholar]
- Lotfi, M. , Zamanzadeh, V. , Valizadeh, L. , & Khajehgoodari, M. (2019). Assessment of nurse‐patient communication and patient satisfaction from nursing care. Nursing Open, 6(3), 1189–1196. 10.1002/nop2.316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manal, H. M. , & Bayoumy, H. M. (2014). Barriers and facilitators for execution of nursing process from nurses perspective. International Journal of Advanced Research, 2(2), 300–315. [Google Scholar]
- Matbouei, M. , Mohammadi, E. , & Zargarzadeh, M. (2013). Assessment of barriers for recording nursing diagnoses by nurses and proposing a solution. Journal of Shahid Beheshti School of Nursing & Midwifery, 24(84), 27–33. [Google Scholar]
- Mazlom, S. R. , & Rajabpoor, M. (2014). Development and assessment of computerized software for nursing process: A step toward promotion of nursing education and care. Iranian Journal of Medical Education, 14(4), 312–322. http://ijme.mui.ac.ir/article-1-3162-en.html [Google Scholar]
- Minthorn, C. , & Lunney, M. (2012). Participant action research with bedside nurses to identify NANDA‐International, Nursing Interventions Classification and Nursing Outcomes Classification categories for hospitalized persons with diabetes. Applied Nursing Research, 25(2), 75–80. 10.1016/j.apnr.2010.08.001 [DOI] [PubMed] [Google Scholar]
- Mohammadi, M. , Ghafori Fard, M. , & Esmaeilivand, M. (2016). Assessing the barriers nursing process by nurses and nurse managers in surgical wards in Imam Reza Hospital, Kermanshah, 2015. Iranian Journal of Nursing Research, 11(3), 58–65. http://ijnr.ir/article-1-1768-en.html [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. PLoS Medicine, 6(7), 264–269. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojgan, L. (1998). The effect of nursing process implementation on nursing care quality in critical care units. Mashhad University of Medical Sciences and Health Services School of Nursing and Midwifery, dissertation. [Google Scholar]
- Muller‐Staub, M. , Needham, I. , Odenbreit, M. , Lavin, M. A. , & van Achterberg, T. (2008). Implementing nursing diagnostics effectively: Cluster randomized trial. Journal of Advanced Nursing, 63(3), 291–301. 10.1111/j.1365-2648.2008.04700.x [DOI] [PubMed] [Google Scholar]
- Nohi, E. , Karimi, H. , & Najmaei, E. (2010). Application obstacles of nursing process from view of the nursing managers and interns in Kerman University of Medical Sciences. Journal of Qualitative Research in Health Sciences, 10(1), 52–58. [Google Scholar]
- Orlando, J. (1961). The dynamic nurse‐patient relationship. New York, NY: Putnams. [Google Scholar]
- Oshvandi, K. , PourYousef, S. , & Bikmoradi, A. (2013). The effects of inquiry‐based clinical instruction of nursing students on applying nursing process skill. Scientific Journal of Hamadan Nursing & Midwifery Faculty, 21(1), 5–15. [Google Scholar]
- Paans, W. , Nieweg, R. M. B. , van der Schans, C. P. , & Sermeus, W. (2011). What factors influence the prevalence and accuracy of nursing diagnoses documentation in clinical practice? A systematic literature review. Journal of Clinical Nursing, 20(17–18), 2386–2403. 10.1111/j.1365-2702.2010.03573.x [DOI] [PubMed] [Google Scholar]
- Paans, W. , Sermeus, W. , Nieweg, R. , & Van der Schans, C. (2010). Determinants of the accuracy of nursing diagnoses: Influence of ready knowledge, knowledge sources, disposition toward critical thinking and reasoning skills. Journal of Professional Nursing, 26(4), 232–241. 10.1016/j.profnurs.2009.12.006 [DOI] [PubMed] [Google Scholar]
- Pace, R. , Pluye, P. , Bartlett, G. , Macaulay, A. C. , Salsberg, J. , Jagosh, J. , & Seller, R. (2012). Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. International Journal of Nursing Studies, 49(1), 47–53. 10.1016/j.ijnurstu.2011.07.002 [DOI] [PubMed] [Google Scholar]
- Paese, F. , Sasso, G. , & Colla, G. W. (2018). Structuring methodology of the Computerized Nursing Process in Emergency Care Units. Rev Bras Enferm, 71(3), 1079–1084. 10.1590/0034-7167-2016-0619 [DOI] [PubMed] [Google Scholar]
- Parvan, K. , Hosseini, F. A. , & Bagherian, S. (2018). The relationship between nursing instructors’ clinical teaching behaviors and nursing students’ learning in Tabriz University of Medical Sciences in 2016. Education for Health, 31(1), 32. [DOI] [PubMed] [Google Scholar]
- Phaneuf, M. , López, C. M. G. , & Ruíz, J. L. (1993). Cuidados de enfermería: el proceso de atención de enfermería: orientación para el diagnóstico de enfermería. Spain: Interamericana-McGraw-Hill. [Google Scholar]
- Potter, P. A. , & Perry, A. G. (2017). fundamental of nursing. St. Louis, MO: Mosby Company, Elsevier Health Sciences. [Google Scholar]
- Rahgooy, A. , Vanaki, Z. , Golestan, B. , & Soulati, R. (1999). The effect use the nursing process on the quality of nursing care in patients with schizophrenia in Razi Psychiatric Center in 1999. Dissertation.
- Rahmani, M. , Alijani, H. , Dashtbozorge, B. , & Haghighizadeh, M. H. (2016). Effect of the nursing process using via "accessible care cards" on the patients' satisfaction of nursing care in intensive care units of Golestan Hospital, Ahvaz. Journal of Clinical Nursing and Midwifery, 5(2), 75–83. http://eprints.skums.ac.ir/id/eprint/4927 [Google Scholar]
- Rajabpoor, M. , Zarifnejad, G. H. , Mohsenizadeh, S. M. , Mazloum, S. R. , Pourghaznein, T. , Mashmoul, A. , & Mohammad, A. (2018). Barriers to the implementation of nursing process from the viewpoint of faculty members, nursing managers, nurses and nursing students. Journal of Holistic Nursing and Midwifery, 28(2), 137–142. 10.29252/hnmj.28.2.137 [DOI] [Google Scholar]
- Rasouli, F. , Hagiamiri, P. , Mahmoudi, M. , & Mostoufian, F. (1996). The effect of nursing education on the prevention and change of pressure ulcers in immobilized patients on the rate of nurses' use of orthopedic units in hospitals affiliated to Tehran University of Medical Sciences in 1995. Dissertation.
- Rastian, M. L. , Borzabady Farahani, Z. , Rasouli, M. , Sarbakhsh, P. , & Niromand, Z. K. (2014). The effect of nursing process implementation on nursing care quality in surgical wards. Advances in Nursing & Midwifery, 24(87), 29–36. [Google Scholar]
- Saba, V. K. , & Feeg, V. (2005). A bedside PC charting system for nursing students using clinical care classification (CCC) system. AMIA Annual Symposium Proceedings, 2005, 1101–1101. http:///PMC1560569/pdf/amia2005_1101 [PMC free article] [PubMed]
- Sasso, D. G. T. , Peres, H. C. , & Silveira, D. T. (2006). Computerized nursing process in critical care unit using the ICNP–Beta2. Studies in Health Technology and Informatics, 122, 1021–1023. [PubMed] [Google Scholar]
- Sayadi, N. , & Rokhafroz, D. (2013). Nursing students’ perspectives about a mobile software on nursing process for bedside use. Iranian Journal of Medical Education, 12(12), 975–981. http://ijme.mui.ac.ir/article-1-2198-en.html [Google Scholar]
- Semachew, A. (2018). Implementation of nursing process in clinical settings: The case of three governmental hospitals in Ethiopia, 2017. BMC Research Notes, 11(1), 173 10.1186/s13104-018-3275-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shewangizaw, Z. , & Mersha, A. (2015). Determinants towards implementation of nursing process. American Journal of Nursing, 4(3), 45–49. 10.11648/j.ajns.20150403.11 [DOI] [Google Scholar]
- Shoorideh, F. A. , & Ashktorab, T. (2011). Factors influencing implementation of nursing process by nurses: A qualitative study. Knowledge & Health, 6(3), 16–23. 10.1234/jkh.v6i3.102 [DOI] [Google Scholar]
- Silva, K. D. L. , Évora, Y. D. M. , & Cintra, C. S. J. (2015). Software development to support decision making in the selection of nursing diagnoses and interventions for children and adolescents. Revista Latino‐Americana De Enfermagem, 23(5), 927–935. 10.1590/0104-1169.0302.2633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva, L. , Evora, Y. D. , & Cintra, C. S. (2015). Software development to support decision making in the selection of nursing diagnoses and interventions for children and adolescents. Rev Lat Am Enfermagem, 23(5), 927–935. 10.1590/0104-1169.0302.2633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperandio, D. J. , & Evora, Y. D. (2009). The use of mobile computational technology in the nursing process: A new challenge for Brazilian nurses. Stud Health Technol Inform, 146, 721–722. [PubMed] [Google Scholar]
- Takahashi, A. A. , Barros, A. L. B. L. D. , Michel, J. L. M. , & Souza, M. F. D. (2008). Difficulties and facilities pointed out by nurses of a university hospital when applying the nursing process. Acta Paulista De Enfermagem, 21, 32–38. 10.1590/S0103-21002008000100005 [DOI] [Google Scholar]
- Vanaki, Z. , & Zamanzadeh, V. (1994). The Effect of Nursing Process Implementation Using Problem‐Circuit documentation in the quantity and quality of the registration of nurses. Dissertation.
- Wagoro, M. C. A. , & Rakuom, C. P. (2015). Mainstreaming Kenya‐Nursing Process in clinical settings: The case of Kenya. International Journal of Africa Nursing Sciences, 3, 31–39. 10.1016/j.ijans.2015.07.002 [DOI] [Google Scholar]
- Walton, I. (1986). The nursing process in perspective: A literature Review. York, UK: Nursing Process Evaluation Working Group, Department of Social Policy and Social Work, University of York. [Google Scholar]
- Whittemore, R. , & Knafl, K. (2005). The integrative review: Updated methodology. Journal of Advanced Nursing, 52(5), 546–553. 10.1111/j.1365-2648.2005.03621.x [DOI] [PubMed] [Google Scholar]
- Yeh, S. H. , Jeng, B. , Lin, L. W. , Ho, T. H. , Hsiao, C. Y. , Lee, L. N. , & Chen, S. L. (2009). Implementation and evaluation of a nursing process support system for long‐term care: A Taiwanese study. Journal of Clinical Nursing, 18(22), 3089–3097. 10.1111/j.1365-2702.2009.02879.x [DOI] [PubMed] [Google Scholar]
- Yura, H. , & Walsh, M. B. (1978). The nursing process: Assessing, planning, implementing, evaluating. New York, NY: Appleton‐Century‐Crofts. [Google Scholar]
- Zamanzadeh, V. , Valizadeh, L. , Jabbarzadeh‐Tabrizi, F. , Behshid, M. , & Lotfi, M. (2015). Challenges associated with the implementation of the nursing process: A systematic review. Iranian Journal of Nursing and Midwifery Research, 20(4), 411–419. 10.4103/1735-9066.161002 [DOI] [PMC free article] [PubMed] [Google Scholar]


