Abstract
Aims
To explore the experiences and needs of patients on the endovascular therapy pathway.
Design
A qualitative design using a phenomenological–hermeneutic approach.
Methods
Semi‐structured interviews and participant observations were carried out. Data were collected from April 2016–January 2017. Data were analysed using Ricoeur's theory of interpretation, capturing meaning and ensuring comprehensive understanding. The Consolidated Criteria for Reporting Qualitative Research checklist was used as a guideline.
Results
The findings of this study show that the impact of stroke goes far beyond physical disability. During the structural analysis, four themes were identified: (1) Acute admission to a stroke unit – an overwhelming and blurred experience. (2) Being helpless and next to yourself. (3) The important care when you worry about dying. (4) Poststroke feelings of loneliness and uncertainty.
Keywords: acute admission, endovascular therapy, experience, nursing, qualitative research, Ricoeur, stroke, support
1. INTRODUCTION
Ischaemic stroke is the third leading cause of death and the most common cause of acquired disability among adults in the Western world (WHO, 2009). In Denmark, there are about 12,500 stroke incidents annually and up to 50,000 Danes live with stroke sequelae (Dansk Selskab for Apopleksi, 2012). Overall, stroke has reached epidemic proportions: 15 million people worldwide suffer a stroke each year, 5 million of whom are estimated to survive with permanent disabilities (WHO, 2009). The most recently approved treatment for major stroke is endovascular therapy (EVT). Its timing is critical (Goyal et al., 2016); ischaemic stroke is a serious diagnosis and demands urgent action to reduce the extent of brain damage. A stroke incident often occurs abruptly with no or few warnings and unfamiliar symptoms like paralysis, aphasia or cognitive impairment constitute a shocking experience for most individuals (Kirkevold, 2002). The intensity of acute hospital admission and uncertainty about the meaning of symptoms, the stroke diagnosis and treatment outcomes may lead to situational stress and emotional strain.
2. BACKGROUND
Shortly after a clot occludes a cerebral artery, brain tissue starts dying. EVT is a mechanical removal of a clot in cerebral arteries, and the goal of treatment is to restore blood flow as soon as possible (Leary et al., 2003). Much research into stroke has been directed at understanding the physiological mechanisms of stroke (Counsell & Dennis, 2001; Liu et al., 2014; Pantoni, Fierini, & Poggesi, 2014), and most qualitative studies of stroke have been conducted with the aim of examining poststroke experiences. Differences and similarities poststroke are related to self‐perceived health, practical activities, participation in society, changed lives, uncertainty and loss (Burton, 2000; Dowswell et al., 2000; Taule & Råheim, 2014). These studies contain few findings about the immediate experiences of acute hospitalization, and no studies have yet investigated patients’ experiences of the EVT pathway. For similarities in acute hospital settings, a Swedish study of patient experiences in emergency departments documents a culture of fragmentation of care, with one nurse assigned to triage, another to checking the patient's temperature and a third to perform blood tests and so on. They describe situations where patients felt abandoned, exposed and vulnerable and state that under such circumstances the concept of “care” is only meaningful in practical terms (Nystrom, Dahlberg, & Carlsson, 2003). Other studies from similar emergency settings argue that in the stressful and sometimes frightening situation of being admitted to an emergency department, patients value empathy and respect (Nyden, Petersson, & Nystrom, 2003). Acute admission to a stroke unit involves similar fragmentation due to the urgent character of the stroke incident; however, there are fundamental differences between the variety of conditions that cause acute admission to emergency departments, the experiences of these patients and how the acute stroke incident, including EVT treatment, affects the stroke patient. About acute stroke admission, similarities in the findings of these studies emphasize the absence of caring behaviour that is needed by patients. We found no recent studies that focused on the hospitalization period including acute stroke treatment. Moreover, as all studies were conducted retrospectively, they may have missed important perceptions of the immediate experiences of acute admittance and the first days in hospital (Olofsson, Andersson, & Carlberg, 2005; Pound, Bury, Gompertz, & Ebrahim, 1995). As clinical professionals, we believe that we need a better understanding of what is going on in patients' minds, especially under extreme circumstances, to be able to accommodate their specific needs. In‐depth research describing the experiences of the EVT pathway from the patients’ perspective could inform the choice of care and support provided by health professionals both in the immediate, acute phase and in the longer term. The aim of this study was to explore the experiences and needs of patients on the EVT pathway.
3. THE STUDY
3.1. Design
This study follows the newly published study on the experiences and needs of relatives whose family members are on an EVT pathway (Sorensen, Dreyer, Rasmussen, Simonsen, & Andersen, 2018); both studies are based on a qualitative design with a phenomenological–hermeneutic approach. Encouraging participants to talk about their lives is a way of capturing life experience (Kvale & Brinkmann, 2008). The essential meaning of a phenomenon can be expressed through narratives and by the actions of the research object. Whereas phenomenology focuses on how essential meanings arise through subjective experiences, hermeneutics highlights the necessary conditions for text interpretation (Lindseth & Norberg, 2004). We generated data through interviews, adopting a narrative approach. To enhance our understanding of the complexity in the acute situation and to strengthen the findings of the interviews, participant observations were carried out (Spradley, 1980). Field notes were taken on aspects like time, surroundings and statements to enable the researcher to characterize a given situation. The data obtained were interpreted using the French philosopher Paul Ricoeur's approach. According to Ricoeur (1973), interpretation of a text means seeing something new in what is taken for granted. In this process, the authors consider their preunderstanding from being professionals within either the stroke or the acute area. The first author is employed as a nurse in the stroke unit that also entails the acute admittance of stroke patients.
3.2. Participants and setting
This study is part of a larger single‐centre randomized trial “Goliath” (General or Local anaesthesia in Intra Arterial Therapy), which aimed to determine whether the use of general anaesthesia or conscious sedation during EVT influences patient outcomes (Simonsen et al., 2016). In this study, the EVT pathway reflects the time from stroke onset, during acute hospital admission, diagnosing and treatment, transition to the stroke unit and a follow‐up period of 3 months. The patient is admitted directly to the stroke unit, bypassing the emergency department and transferred directly from the ambulance stretcher onto the magnetic resonance imaging (MRI) table. Then, a rapid examination including the National Institutes of Health Stroke Scale (NIHSS) is performed. After the emergency MRI, the medical treatment starts immediately and the patient is wheeled to the angio suite as rapidly as possible. After the procedure, the patient is transferred to the recovery unit to be monitored until stable and then forwarded to the stroke unit to further monitoring and care. The average time of stay in the stroke unit is 48 hr where after the patient is transferred to rehabilitation in the community or discharged (Figure 1). Eighteen patients randomized in “Goliath” were asked to participate in the present study. We used purposeful sampling for the identification and selection of information‐rich cases of the phenomenon of interest. Patients were recruited from the Danish Stroke Centre at Aarhus University Hospital. Inclusion criteria were as follows: (a) acute stroke and EVT treatment, (b) ability to speak Danish and (c) signed informed consent. Data were collected from April 2016–January 2017. To get different perspectives according to the principle of divergence, the selection was also influenced by considerations of gender, age, civil status, status of symptoms and type of anaesthesia (Table 1). Participants were recruited in the acute setting. The researcher was called by the nurse in charge when a patient with expected large ischaemic stroke was on his or her way to the hospital. Shortly after the patient's admission, the observations began. During hospitalization within the first days, the patients (in some cases accompanied by relatives) were further invited to participate in an interview.
Figure 1.
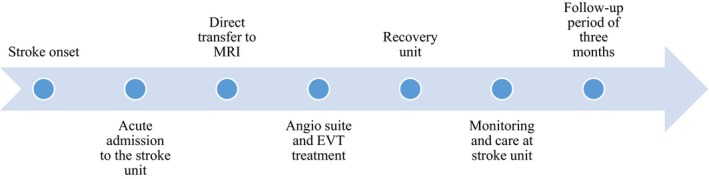
Endovascular therapy pathway
Table 1.
Sociodemographic and clinical characteristics of the sample
| Code | Age | Gender | Marital status | Stroke site | NIHSS Score at hospital admittance | Type of anaesthesia |
|---|---|---|---|---|---|---|
| 01 | 55 | M | M | R | 15 | LA |
| 02 | 75 | F | W | L | 12 | GA |
| 03 | 73 | M | M | L | 10 | GA |
| 04 | 85 | M | M | R | 17 | GA |
| 05 | 76 | M | M | R | 12 | LA |
| 06 | 57 | M | S | L | 21 | GA |
| 07 | 73 | M | S | R | 19 | GA |
| 08 | 67 | F | M | L | 17 | LA |
| 09 | 70 | F | M | R | 15 | LA |
| 10 | 72 | F | M | L | 12 | GA |
| 11 | 70 | F | M | R | 17 | LA |
| 12 | 76 | M | W | L | 18 | LA |
| 13 | 78 | F | W | L | 22 | GA |
| 14 | 83 | M | M | R | 18 | LA |
| 15 | 77 | M | M | R | 12 | GA |
| 16 | 72 | F | M | L | 22 | GA |
| 17 | 61 | F | S | L | 23 | GA |
| 18 | 66 | F | W | L | 10 | GA |
Abbreviations: GA, general anaesthesia; LA, local anaesthesia; M, married; S, single; W, widowed.
3.3. Data collection
Observations were carried out in the acute setting with the first author as the passive participating observer, meaning that the observer was a part of a situation, simultaneously as a researcher being outside of it making observations (Spradley, 1980). At this stage, the first author made an effort to hold the preunderstanding in abeyance, focusing on the recognition of patterns to illuminate the essence of the phenomenon. To minimize confusion about the presence of the observer, she was dressed in civilian clothes and if any interaction in the social situation was necessary, it would only be as a bystander or a spectator. Field notes were described immediately. Once written consent was obtained, the researcher followed the patient to the intervention room where EVT treatment was performed, the recovery unit and back to the neurological ward when the patient was stable. Observations lasted up to 8 hr and provided a basis for the interviews that followed (Spradley, 1980). Interviews took place in a private room to ensure that interviewees could speak freely. The patients were interviewed again after 3 months to capture experiences in the follow‐up period and ensure identification of any experiences and thoughts postadmission. Follow‐up interviews were conducted after the standard follow‐up in the outpatient clinic, where all patients treated with EVT had a neurological consultation with a stroke specialist. The interviews lasted 30–60 min, were tape‐recorded and transcribed verbatim. A pilot interview was conducted to validate the interview questions.
3.4. Data analysis
Ricoeur's interpretation theory includes three steps: naïve reading, structural analysis and critical analysis and discussion (Lindseth & Norberg, 2004; Ricoeur, 1973). In the naïve reading, the entire content of the interviews was read for an overall impression about the EVT pathway. This stage yields a general sense of the text and gives the reader an immediate understanding of the meaning content. Then in the structural analysis, the interpretation began and was carried out at four levels; what is said (quotations), what is seen (field notes), what the text speaks about (meaning) and the themes (interpretations) (Table 2). The observations were not analysed systematically but served as a basis for the interpretation of the interviews because of a primary limitation of interview data: that it concentrates on thoughts and experiences at the expense of actions (Kvale & Brinkmann, 2008). The meaning content of the structural analysis was compared with the observations. In the critical analysis, the themes were discussed and interpreted in light of the authors’ preunderstanding and the literature to achieve a final comprehensive understanding. The diverse pieces of data in combination were used to find trustworthy answers of the phenomenon and to produce a clear and complete explanation.
Table 2.
Example of structural analysis
|
Quote “What is said” |
Field notes from observations “What is seen” |
Meaning “What the text speaks about” |
Interpretation “The theme” |
|---|---|---|---|
|
“But the days I was at the stroke unit, I was all done for, I didn't hear anything, I didn't see anything.” “When everything suddenly is taken away from you and you are completely helpless, then it's nice to have the nurses.” “I thought if I would be able to walk again, I am used to going out in the morning and do stuff around the house, but now I can't.” “At night I felt unpleasant, I was restless, I wasn't awake, but I didn't sleep either” “I woke up feeling bad and then she just stood there caressing my arm and that was nice.” |
The patient is sitting in the wheelchair crying, he is talking to the nurse about his former functional level. The nurse places a chair beside the patient and sits down. She puts her hand on his arm and talks to him about the early stage of the stroke phase, where nothing is yet determined. The patient smiles at the nurse when she arrived at the recovery unit |
The new life situation with sudden bodily challenges makes patients feel helpless. Feelings of being in a bubble occur. Thoughts about the future and ability to walk again and handle usual responsibilities reigned in the patients’ minds. The nights are hard to endure because of racing thoughts interrupting the sleep |
Being helpless and next to yourself |
3.5. Rigour
To ensure rigour in the study and to strengthen credibility (Wu, Thompson, Aroian, McQuaid, & Deatrick, 2016), prolonged engagement with the participants was prioritized and the use of field notes during the entire observational period enhanced memory of exact episodes of importance for the conception of the whole (Spradley, 1980). To strengthen the trustworthiness of the data, interviews were tape‐recorded and transcribed by the interviewer without subjective interpretation at this phase. Statements were frequently summarized and restated by the interviewer to verify the meaning content (Kvale & Brinkmann, 2008).
3.6. Ethical considerations
The first author informed the patients about the study both orally and in writing. They were reassured that their participation was voluntary, that they could withdraw from the study at any time and that data would be anonymized. The study was approved by the appropriate ethics committee (Record number 1‐16‐02‐647‐14).
4. RESULTS
4.1. Naive reading
The naive reading gave an initial, spontaneous understanding of how the patients experienced the EVT pathway. Below, this understanding is expressed in terms of the meaning of the whole experience.
Acute admission to a stroke unit was an overwhelming experience and entailed feelings of anxiety and concern. One specific action, the MRI, was generally considered an unpleasant experience. However, loss of memory of specific actions or procedures seemed to occur. Loss of independence and inability to communicate led to feelings of powerlessness, where both the body and the mind seemed uncontrollable. Patients appreciated being able to hand over responsibility to a team of professionals, and the receiving nurse played a pivotal role throughout the entire pathway. After discharge, the patients became aware that the stroke had changed their physical and mental lives forever and there seemed to be a commonly felt need for support, reassurance and information.
4.2. Structural analysis
During the structural analysis, four themes were identified.
4.3. Acute admission to a stroke unit – an overwhelming and blurred experience
An overall impression is that patients had a clear memory of the circumstances of stroke onset with respect to how they felt, acted and thought, but only recalled little about the initial acute management. Some memories recovered when they were asked directly, but for the most part, all episodes from the acute phase were dim: “I was driven on something that rumbled, I don´t know what it was, but that I remember. Actually, I have no memory of yesterday's happenings, it is all gone.” Despite memory loss of the acute admission, MRI remained a fearful experience for most, and feelings of anxiety were reported: “Getting into that devil not knowing what is happening, you are feeling quite bad actually and at the same time you are terribly afraid. That was a horrible experience for me.” The patients did not recall what kind of anaesthesia was used for the EVT procedure, and it seemed that it was not important for them to know: “No, I can´t recall, but… it is just sedation.” It is especially noteworthy that no differences in the patients’ memory were registered in the two groups of sedation types. The patients did not remember the staff present before or during the procedure, nor to which extent they were addressed. The acute phase of the EVT pathway was nearly erased from their memories: “Actually, I do not recall the first hours of my hospitalisation (…). What you gave me and what you have done to me, I know nothing about and I do not recall anything about the sedation.” In relation to the health professionals, one patient was convinced that he would be able to recognize the involved health professionals who had been involved if he saw them again, despite memory loss. The professionals made an impression on him and left him with an experience of being treated competently and with the best intentions: “No, I do not remember exactly, but when I see them, I will know that they were there. I think that the nurses were professional; they do a lot for you.” Several patients stated that their first recollections were in the recovery room when their relatives arrived. Despite scant memories, it seemed that the receiving nurse was very important to the patient. A wife of one patient reported that when the patient saw the nurse who was in charge of his acute admission for the first time after the EVT treatment, he recognized her immediately and was very pleased with her presence, as if she had played a vital role in the situation: “He said, ‘Oh, there she is, the little nurse’.” This is supported by a statement from a patient who stated that the only memory he recalled for sure was that of the admitting nurse: “No, I don't remember, but xxx (name of the nurse) was there.”
4.4. Being helpless and next to yourself
Stroke was characterized as a sudden and overwhelming catastrophe that made both the body and the mind uncontrollable. Voluntary movement is lost; the body is invaded by equipment and loss of independence; and the inability to communicate entails feelings of powerlessness, anxiety and uncertainty: “What is all this? What is going on? I felt completely helpless.” The bedrooms on the ward were fraught with disturbing noises and unpleasant procedures that prevented rest and sleep. Especially, the nights were reported as being hard to endure because of racing thoughts and strange noises interrupting sleep: “At night, I felt uneasy, I was restless, I wasn't awake, but I didn't sleep either.” It seems that support and awareness from nurses at this stage are essential: “I woke up feeling bad and then she just stood there caressing my arm and that was nice.” In general, patients described experiences of the acute phase as being intense and exhausting, resulting in them needing peace and quiet: “And then, suddenly, I began to communicate a little. I had no idea what time it was, or how much time had passed. I just needed some rest.” Patients appreciated the fact that procedures around them were calm and that communication was slow and understandable. Several described the feeling of being in a bubble, with what happened around them seeming to happen outside them and not inside them: “But the days I was at the stroke unit, I was all done for. I didn't hear anything, I didn't see anything” and many felt resigned to a passive role and complete helplessness. In the early stages of the pathway, thoughts about the future began to arise. Thoughts about prognosis and whether they would be able to manage their normal lives dominated the patients’ minds: “I wondered if I would be able to walk again. I am used to going out in the morning and doing stuff around the house, but now I can't.”
4.5. The important care when you worry about dying
The nurse played a central role during acute admission and the MRI. Most of the patients reported feelings of anxiety and uncertainty about what was going on. The nurse who was present during the acute phase provided the patients with a sense of security. During the uncomfortable MRI session, it was calming when the nurse placed her hand on the patients’ leg. That made them feel cared for in an unpleasant situation: “A nurse was present right from the beginning. She was absolutely wonderful and I appreciated that more than anything. After all, you worry a lot. I wondered if this was a one‐way ticket.” During admission to the stroke unit, the patients put themselves under the charge of the staff. They adopted a passive role without any demands or expectations and became more of an object to be saved: “I felt totally safe. At that time, I had surrendered, I normally don't, but…”. Patients appreciated being able to hand over responsibility to a team of people who could take decisive actions on their behalf, and feelings of helplessness, anger and frustration were eliminated in the presence of health professionals: “When everything is torn apart and you can do nothing, you are completely helpless, it is nice to have the nurses.” The patients did not notice panic despite the critical situation and that made them feel that they were in the hands of competent health professionals who all knew their specific roles in the acute phase. Many patients noted that the conduct of routine tests provided reassurance: “they came in all the time to test my arms and legs and asked me questions. That was nice and made me feel safe.”
4.6. Poststroke feelings of loneliness and uncertainty
Over time, participants became aware that the stroke had forever changed their lives both physically and psychologically and that stroke sequelae had a significant impact on emotions, personality, abilities, activities, roles and social relationships. These overwhelming changes caused feelings of anxiety and uncertainty about what the future might hold and the fear of another stroke was always present: “I feel terrible. It is in my head and it became worse after my panic attack.” After coming home, several lingering questions and feelings of being left alone were reported by several patients. Evident in their statements was the sadness of realizing that some tasks that they had appreciated and that moments that were attainable prestroke were now unattainable. They were uncertain about which institution could help them and about what resources were available at all: “I didn't know where to go. I had all these questions and I didn't know where I should go to address them.” There was a general need for support, encouragement, reassurance, advice, information about medication, information about the risk of a setback and, perhaps most importantly, information about their respective impairments: “the stroke made me fearful. I am terrified that another stroke might hit me again.” They found that their GP did not fulfil their needs in this regard: “My house doctor cannot help me with that.”
After discharge, the patients asked to gain access to the healthcare system before the standard follow‐up in the neurological outpatient clinic. There were indications of disappointment about the lack of someone to turn to and concerns that nobody with professional knowledge of stroke would be there to reassure them about their condition: “I did not know where to go and where to seek help with these feelings of anxiety. I was very frightened and it would have been nice to have been prepared that this could happen to me.” After follow‐up in the stroke unit, it seemed that these unanswered questions and confusing experiences of feeling no longer oneself were clarified: “I feel kind of relieved now that all these pieces had fallen into place.” These findings suggest that patients may have undefined needs after discharge and that follow‐up helped to organize feelings of chaos. Some patients requested contact with other individuals with stroke as confirmation that they were not alone in their situation, as well as having the opportunity to talk about the main challenges and worries of the poststroke period: “I did a search for groups who had had a stroke, a place to talk with others with the same problems as me, but I couldn't find any.” Particularly, stroke victims who have a positive recovery seemed to seek out patient courses, networking, continued training or other options that might help their cognition or understanding of their own situation. They felt like they were running against a brick wall when they tried to find initiatives in line with their specific challenges and wishes: “what they offered in the rehabilitation centre was targeted at patients with aphasia or with worse disabilities than me.” It is clear from the statements that patients felt powerless and that they were left with unsolved problems poststroke.
5. DISCUSSION
The findings of this study show that patients had very limited memories of the acute phase of their hospitalization, which is in line with previous studies of stroke (Kirkevold, 2002; McKevitt, Redfern, Mold, & Wolfe, 2004). However, being part of the emergency admission in the EVT pathway entailed anxiety and intimidating thoughts. Our study reveals that the MRI scan remained a powerful experience despite memory loss of specific actions and management of the stroke incident. The presence of a nurse ameliorated the experience in the MRI scanner. This illustrates the need for particular attention to care during the early phase of emergency admission. The immediate needs of stroke patients in the acute hospital setting were expressed as the ability to hand over responsibility to experienced and trusted health professionals who would take all the actions needed to ensure survival and provide warmth and reassurance during the crisis. This finding is supported by a Swedish study, which suggests that health professionals are considered to be knowledgeable and competent (Olofsson et al., 2005). Relatively few studies document patients’ views of acute stroke care and those that did seem to concur that patients with stroke focused much more on the recovery process than on acute admission (Salisbury, Wilkie, Bulley, & Shiels, 2010).
In summary, the above statements indicate that health professionals should be aware of patients’ feelings of anxiety and their need for support during acute admission and the impression of the nurse being “a physical person who took care of me” not just “a nurse” is essential to keep in mind. The bodily memories seem to exceed the memories of information. This suggests that attention from health professionals in the very acute phase should concentrate on overall care instead of providing vast quantities of information since patients do not recall this information later on. As the acute phase passes, patients may increasingly desire support about emotional aspects of their recovery. Nurses are considered vital in this effort. Nurses are perhaps the most important professionals as they are with the patients throughout the 24 hr of the day (Wade, 1987). This is consistent with our findings, where nurses’ support and awareness day and night seem to be essential.
Another major issue raised in our study involves the challenges that arose after discharge – in particular, patients’ uncertainty about what services they were entitled to and whom to contact in case they had any questions. Patients commonly feared a new stroke, an intense fear of which could be the primary cause of episodes of anxiety. Reed, Harrington, Duggan, and Wood (2010) explored stroke survivors' needs and their perceptions of whether a community stroke scheme met these needs. They found that stroke survivors need a variety of internal and external resources to regenerate their lives, and that a specially targeted scheme, based on exercise, goal setting and peer group interaction, makes a remarkable difference in patients’ ability to recover. They claimed that through acquiring knowledge, patients might be able to understand their condition and identify ways they could support themselves (Reed et al., 2010). In the light of the present findings, we suggest that anxiety could have been reduced if more information and support had been provided. The perceived effectiveness of social support networks has a positive influence on both physical recovery and quality of life poststroke (Salter, Hellings, Foley, & Teasell, 2008) and might prevent the challenges in differentiating between available services or lack thereof.
Our study highlights that patients with a positive recovery felt like they were running against a brick wall when seeking actual services. Almost half of the patients treated with EVT regain functional independence (Goyal et al., 2016), which seems to be considered quite positively by authorities. However, the patients expressed uncertainty about their challenges poststroke and whether these challenges were to be expected. We found that explanation of what they had been through was of great importance. Knowledge about what had happened, the extent of brain damage and what consequences may follow prompts calmness so that the whole situation suddenly makes more sense. Further information about how to prevent a new stroke and reassurances about medical treatment made patients feel secure.
Our findings support research that reveals that many patients with good functional outcomes continue to be cognitively impaired, unable to socially reintegrate and experience symptoms of depression (Kapoor et al., 2017). While these patients may have recovered in terms of physical disability, having returned to their prestroke functional level and being able to perform activities of daily living independently, they still experienced dysfunction at multiple levels (Kapoor et al., 2017). On the other hand, our results lead us to urge caution about use of the term “cognitive impairment.” We suggest that most patients are actually capable of integrating the knowledge obtained to understand and improve their new condition.
Our findings show that the need for follow‐up is true for more than the medical condition. The standard follow‐up in hospital after 3 months with a neurologist specialized in stroke is indispensable and provides reassurance. However, within this 3‐month period, patients have existential needs that most probably would be met if the opportunity to have a specialist consultation was available. This leads to considerations about whether a nurse‐led outpatient clinic would meet the needs of these patients and help them cope with the existential issues and prevent them from feeling like they were running into a brick wall and abandoned. Experiences from an aftercare clinic in the UK set up to optimize aftercare in stroke patients may be transferable to the Danish setting (Peskett & Gibb, 2009).
It could be speculated whether recognition of service gaps in the poststroke period could be explained by the lack of clear national rehabilitation guidelines (Dansk Selskab for Apopleksi, 2012). According to the Scottish Intercollegiate Guidelines Network (SIGN) (2010), stroke victims should be assessed by members of the primary care team, community rehabilitation team and care agencies after discharge and it is especially noteworthy that it is recommended that there be continual evaluation of the patient's progress in a partnership with the patient and their carer(s). These recommendations may be worth acknowledging in future efforts to optimize stroke care; however, further research that supports these statements is required.
5.1. Limitations
The sample size used in this study was suitable for a qualitative study and afforded an in‐depth understanding of the phenomenon. However, the sample size is not sufficiently large to allow findings to be generalized to other communities. As an employee in the stroke unit, the first author's preunderstanding may have limited what was regarded relevant and important. However, efforts were made to meet the phenomenon open minded by reflecting on own position and interpretations made. The fact that patients with severe stroke, with aphasia, cognitive impairment or other symptoms which means that they would not be able to consent to this study is a weakness, as experiences from this group could have contributed vital knowledge.
6. CONCLUSION
The impact of the EVT pathway emphasized rapid triage, treatment and transfer; however, it became obvious that the EVT pathway itself did not eclipse the stroke and its consequences. Importantly and in conclusion, the EVT treatment leaves patients with a higher functional outcome. This means that more patients are discharged without rehabilitation needs and the kind of safety net that the rehabilitation period provides. Attention to patients’ feelings of anxiety, concern and general uncertainty about their new situation therefore needs to be prioritized both acutely and over time. Ideally, the admitting nurse should assist the patient during the MRI by providing a sense of security and by supporting the patient through this difficult experience. In general, the admitting nurse plays an essential role throughout the EVT pathway and featured strongly in patients’ memories, where events and procedures were otherwise blurred. Our study highlights that explaining how to interpret respective impairments facilitates insight and entails a new acceptance of these patients’ being in the world. It is important to raise awareness of the potentially subtle but consequential residual impairments following stroke. These impairments seem to be missed in patients who appear to have functionally recovered but may struggle with more complex activities, affecting their everyday life. Overall follow‐up after discharge is important, particularly with specialists in stroke. Important knowledge is presented with respect to the development of structured follow‐up based on patients’ actual needs. This study provides a starting point for future research within the care chain of the EVT pathway.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
ACKNOWLEDGEMENTS
Thanks are given to the participants in this study, and the authors appreciate the support received from the Neurological Department, the Department of Anaesthesiology and Intensive care and the “Research Programme the acute patient.
Sørensen KE, Dreyer P, Rasmussen M, Simonsen CZ, Andersen G. Experiences and needs of patients on the endovascular therapy pathway after acute ischaemic stroke: Being helpless and next to yourself. Nursing Open. 2020;7:299–306. 10.1002/nop2.391
Funding information
The study received financial support from Aarhus University Hospital.
REFERENCES
- Burton, C. R. (2000). Living with stroke: A phenomenological study. Journal of Advanced Nursing, 32(2), 301–309. 10.1046/j.1365-2648.2000.01477.x [DOI] [PubMed] [Google Scholar]
- Counsell, C. , & Dennis, M. (2001). Systematic review of prognostic models in patients with acute stroke. Cerebrovascular Diseases (Basel, Switzerland), 12(3), 159–170. 10.1159/000047699 [DOI] [PubMed] [Google Scholar]
- Dansk Selskab for Apopleksi (2012). Referenceprogram for behandling af patienter med apopleksi (national guideline for stroke treatment). Retrieved from http://www.dsfa.dk/wpcontent/uploads/REFERENCEPROGRAMFINAL20131.pdf [Google Scholar]
- Dowswell, G. , Lawler, J. , Dowswell, T. , Young, J. , Forster, A. , & Hearn, J. (2000). Investigating recovery from stroke: A qualitative study. Journal of Clinical Nursing, 9(4), 507–515. 10.1046/j.1365-2702.2000.00411.x [DOI] [PubMed] [Google Scholar]
- Goyal, M. , Menon, B. K. , van Zwam, W. H. , Dippel, D. W. , Mitchell, P. J. , Demchuk, A. M. , … HERMES Collaborators (2016). Endovascular thrombectomy after large‐vessel ischaemic stroke: A meta‐analysis of individual patient data from five randomised trials. Lancet (London, England), 387(10029), 1723–1731. 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- Kapoor, A. , Lanctôt, K. L. , Bayley, M. , Kiss, A. , Herrmann, N. , Murray, B. J. , & Swartz, R. H. (2017). “Good outcome” isn’t good enough. Stroke, 48(6), 1688–1690. 10.1161/STROKEAHA.117.016728 [DOI] [PubMed] [Google Scholar]
- Kirkevold, M. (2002). The unfolding illness trajectory of stroke. Disability and Rehabilitation, 24(17), 887–898. 10.1080/09638280210142239 [DOI] [PubMed] [Google Scholar]
- Kvale, S. , & Brinkmann, S. (2008). Interviews: Learning the craft of qualitative research interviewing. Los Angeles, CA: SAGE. [Google Scholar]
- Leary, M. C. , Saver, J. L. , Gobin, Y. P. , Jahan, R. , Duckwiler, G. R. , Vinuela, F. , … Starkman, S. (2003). Beyond tissue plasminogen activator: Mechanical intervention in acute stroke. Annals of Emergency Medicine, 41(6), 838–846. 10.1067/mem.2003.194 [DOI] [PubMed] [Google Scholar]
- Lindseth, A. , & Norberg, A. (2004). A phenomenological hermeneutical method for researching lived experience. Scandinavian Journal of Caring Sciences, 18(2), 145–153. 10.1111/j.1471-6712.2004.00258.x [DOI] [PubMed] [Google Scholar]
- Liu, J. , Wang, Y. , Akamatsu, Y. , Lee, C. C. , Stetler, R. A. , Lawton, M. T. , & Yang, G. Y. (2014). Vascular remodeling after ischemic stroke: Mechanisms and therapeutic potentials. Progress in Neurobiology, 115, 138–156. 10.1016/j.pneurobio.2013.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKevitt, C. , Redfern, J. , Mold, F. , & Wolfe, C. (2004). Qualitative studies of stroke: A systematic review. Stroke, 35(6), 1499–1505. 10.1161/01.STR.0000127532.64840.36 [DOI] [PubMed] [Google Scholar]
- Nyden, K. , Petersson, M. , & Nystrom, M. (2003). Unsatisfied basic needs of older patients in emergency care environments ‐ obstacles to an active role in decision making. Journal of Clinical Nursing, 12(2), 268–274. 10.1046/j.1365-2702.2003.00737.x [DOI] [PubMed] [Google Scholar]
- Nystrom, M. , Dahlberg, K. , & Carlsson, G. (2003). Non‐caring encounters at an emergency care unit–a life‐world hermeneutic analysis of an efficiency‐driven organization. International Journal of Nursing Studies, 40(7), 761–769. 10.1016/S0020-7489(03)00053-1 [DOI] [PubMed] [Google Scholar]
- Olofsson, A. , Andersson, S. O. , & Carlberg, B. (2005). 'If only I manage to get home I'll get better'–interviews with stroke patients after emergency stay in hospital on their experiences and needs. Clinical Rehabilitation, 19(4), 433–440. 10.1191/0269215505cr788oa [DOI] [PubMed] [Google Scholar]
- Pantoni, L. , Fierini, F. , & Poggesi, A. (2014). Thrombolysis in acute stroke patients with cerebral small vessel disease. Cerebrovascular Diseases (Basel, Switzerland), 37(1), 5–13. 10.1159/000356796 [DOI] [PubMed] [Google Scholar]
- Peskett, M. , & Gibb, P. (2009). Developing and setting up a patient and relatives intensive care support group. Nursing in Critical Care, 14(1), 4–10. 10.1111/j.1478-5153.2008.00302.x [DOI] [PubMed] [Google Scholar]
- Pound, P. , Bury, M. , Gompertz, P. , & Ebrahim, S. (1995). Stroke patients' views on their admission to hospital. BMJ (Clinical Research Ed.), 311(6996), 18–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed, M. , Harrington, R. , Duggan, A. , & Wood, V. A. (2010). Meeting stroke survivors' perceived needs: A qualitative study of a community‐based exercise and education scheme. Clinical Rehabilitation, 24(1), 16–25. 10.1177/0269215509347433 [DOI] [PubMed] [Google Scholar]
- Ricoeur, P. (1973). The hermeneutical function of distanciation. Philosophy Today, 17, 129–141. Retrieved from https://search-proquest-com.ez.statsbiblioteket.dk:12048/docview/42571557?accountid=14468 10.5840/philtoday197317233 [DOI] [Google Scholar]
- Salisbury, L. , Wilkie, K. , Bulley, C. , & Shiels, J. (2010). 'After the stroke': Patients' and carers' experiences of healthcare after stroke in Scotland. Health & Social Care in the Community, 18(4), 424–432. 10.1111/j.1365-2524.2010.00917.x [DOI] [PubMed] [Google Scholar]
- Salter, K. , Hellings, C. , Foley, N. , & Teasell, R. (2008). The experience of living with stroke: A qualitative meta‐synthesis. Journal of Rehabilitation Medicine, 40(8), 595–602. 10.2340/16501977-0238 [DOI] [PubMed] [Google Scholar]
- Scottish Intercollegiate Guidelines Network . (2010). Management of patients with stroke: Rehabilitation, prevention and management of complications and discharge planning: A national clinical guideline. Edinburgh, UK: SIGN; Retrieved from https://www.sign.ac.uk/sign-118-management-of-patients-with-stroke-rehabilitation,-prevention-and-management-of-complicati.html [Google Scholar]
- Simonsen, C. Z. , Sorensen, L. H. , Juul, N. , Johnsen, S. P. , Yoo, A. J. , Andersen, G. , & Rasmussen, M. (2016). Anesthetic strategy during endovascular therapy: General anesthesia or conscious sedation? (GOLIATH – general or local anesthesia in intra arterial therapy) A single‐center randomized trial. International Journal of Stroke, 11(9), 1045–1052. 10.1177/1747493016660103 [DOI] [PubMed] [Google Scholar]
- Sorensen, K. E. , Dreyer, P. , Rasmussen, M. , Simonsen, C. Z. , & Andersen, G. (2018). Endovascular therapy after acute ischaemic stroke‐experiences and needs of relatives. Journal of Clinical Nursing, 28(5‐6), 792–800. 10.1111/jocn.14664 [DOI] [PubMed] [Google Scholar]
- Spradley, J. P. (1980). Participant observation. Belmont, CA: Wadsworth Thomson Learning. [Google Scholar]
- Taule, T. , & Råheim, M. (2014). Life changed existentially: A qualitative study of experiences at 6–8 months after mild stroke. Disability & Rehabilitation, 36(25), 2107–2119. 10.3109/09638288.2014.904448 [DOI] [PubMed] [Google Scholar]
- Wade, D. T. (1987). Who looks after stroke patients? British Journal of Hospital Medicine, 37(3), 200–204. [PubMed] [Google Scholar]
- WHO (2009). Cardiovascular diseases (CVDs). Retrieved from https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) [Google Scholar]
- Wu, Y. P. , Thompson, D. , Aroian, K. J. , McQuaid, E. L. , & Deatrick, J. A. (2016). Commentary: Writing and evaluating qualitative research reports. Journal of Pediatric Psychology, 41(5), 493–505. 10.1093/jpepsy/jsw032 [DOI] [PMC free article] [PubMed] [Google Scholar]


