Abstract
Introduction:
Public access defibrillation (PAD) programs seek to optimize locations of automated external defibrillators (AEDs) to minimize the time from out-of-hospital cardiac arrest (OHCA) recognition to defibrillation. Most PAD programs have focused on static AED (S-AED) locations in high traffic areas; pervasive electronic data infrastructure incorporating real-time geospatial data opens the possibility for AED deployment on mobile infrastructure for retrieval by nearby non-passengers. Performance characteristics of such systems are not known.
Hypothesis:
We hypothesized that publicly accessible AEDs located on buses would increase publicly accessible AED coverage and reduce AED retrieval time relative to statically located AEDs.
Methods:
S-AED sites in Pittsburgh, PA were identified and consolidated to 1 AED per building for analysis (n=582). Public bus routes and schedules were obtained from the Port Authority of Allegheny County. OHCA locations and times were obtained from the Pittsburgh site of the Resuscitation Outcomes Consortium. Two simulations were conducted to assess the characteristics and impact of AEDs located on buses. In Simulation #1, geographic coverage area of AEDs located on buses (B-AEDs) was estimated using a 1/8th mile (201m) retrieval radius during weekday, Saturday and Sunday periods. Cumulative geographic coverage across each period of the week was compared to S-AED coverage and the added coverage provided by B-AEDs was calculated. In Simulation #2, spatiotemporal event coverage was estimated for historical OHCA events, assuming constraints designed to reflect real world AED retrieval scenarios. Event coverage and AED retrieval time were compared between B-AEDs and S-AEDs across periods of the week and residential / non-residential spatial areas.
Results:
Cumulative geographic coverage by S-AEDs was 23% across all periods, assuming uniform access hours. B-AEDs alone versus B-AEDs + S-AEDs covered 20% vs. 34% (weekday), 14% + 30% (Saturday), and 10% + 28% (Sunday). There was no statistically significant difference in 3-minute historical AED accessibility between only B-AEDs and only S-AEDs in standalone deployments (12% vs. 14%). However, when allowing for retrieval of either type of AED in the same scenario, event coverage was improved to 22% (p < 0.001).
Conclusion:
Deployment of B-AEDs may improve AED coverage but not as a standalone deployment strategy.
Introduction
It is well established that early defibrillation is linked to improved outcomes after out-of-hospital cardiac arrest, specifically in those cases wherein the presenting electrocardiogram rhythm is ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT).1–3 Public access defibrillation (PAD) programs seek to place automated external defibrillators (AEDs) strategically throughout the community to maximize the probability of early defibrillation in the event of an out-of-hospital cardiac arrest (OHCA). The principal rationale is that public AEDs may be closer to victims than those carried by emergency medical services (EMS), and in the right hands a defibrillating shock may be delivered prior to EMS arrival, netting an increased probability of survival.
Historically, PAD programs have focused on static AED (S-AED) placements. This is likely because AED placements in public buildings and other fixed structures (e.g., standalone outdoor cabinets and pavilions) provide a consistent location that passersby can acquaint themselves with and quickly go to in a nearby cardiac emergency, and likewise that emergency dispatch personnel can indicate over the telephone when referring to an AED database. S-AED locations can be optimized for proximity to pedestrian traffic or concentrations of high-risk individuals, where risk may be a function of age, medical history, and/or strenuous activity.4–7 There are also drawbacks to S-AEDs that include limited spatial coverage area, building access restrictions, and a general bias toward non-residential settings. An efficient AED deployment solution that addresses these limitations could save lives.
Public transportation systems, specifically those traveling on roads (i.e., buses, taxis, and rideshare vehicles), may possess features that could facilitate an efficient PAD deployment. To start, these networks tend to be widely distributed across geographic areas, linked by a well-defined communication infrastructure, and have clear delineations between on-duty and off-duty status (i.e., accessibility). Device accountability, including usage tracking and maintenance, for an AED stored on a vehicle could likely be streamlined as part of regular vehicle maintenance. Lastly, the utility of such AEDs would be twofold: for events occurring on board the vehicle and for events in the vicinity of the vehicle at a given time. In communities with high public transportation traffic but limited commercial development, this strategy might bring public AEDs where they otherwise would not exist.
In this study, we simulated a hypothetical mobile AED platform employing public transportation infrastructure, specifically public buses, as the target for AED placement. Our objective was not to determine the utility of bus-located AEDs (B-AEDs) for treating bus passengers per se, but to determine the utility of B-AEDs to the surrounding communities that they pass through during the course of normal operation. We hypothesized that B-AEDs would increase AED spatiotemporal coverage and reduce AED retrieval time relative to a PAD deployment solely based on S-AEDs.
Methods
Data Sources
This study was conceived as a simulation based on retrospective, observational data and publicly available infrastructure data collected from multiple sources.
The locations of S-AEDs (n = 582) within the Pittsburgh city limits were obtained from the University of Pittsburgh Resuscitation Logistics and Informatics Venture, which conducts AED location surveillance in the City of Pittsburgh and surrounding County of Allegheny. Location data were coded as latitude / longitude coordinates and for the sake of this study did not include information about floor level. For this study, multiple AEDs located in a single building with the same latitude / longitude coordinates were coded as a single device because it was assumed that only the existence of an AED at a given coordinate pair would be relevant to our study aims. Location of AEDs within buildings was not considered because floor-level (i.e., vertical) location of OHCA events for analysis, described below, was not available.
De-identified historical location data for all non-traumatic, EMS-treated OHCA events (n = 1,952) in the City of Pittsburgh between the years 2010 and 2015, were obtained from the Pittsburgh site of the Resuscitation Outcomes Consortium in latitude / longitude coordinates. Case data included the time of day, day of the week and the year of the event, but not the month or calendar date of the event, providing sufficient information to coordinate the event with local bus schedules.
Bus schedules current as of May 1, 2017 for the Port Authority of Allegheny County were obtained electronically from the Port Authority’s public data sharing website. Schedules included routes, defined by stop locations and bus arrival times, and separately tabulated weekday and weekend time frames. Stop locations were geocoded in latitude / longitude coordinates. Maps of the City of Pittsburgh were obtained from the City of Pittsburgh Department of City Planning and were current as of July 1, 2017. This system includes over 700 buses8, and based on the scheduling data for this time period, at any given time between 1 and 548 buses could be on the road at a time.
Simulation Details
We conducted two simulations to determine the impact of B-AED deployment. In the first, we asked the question, “On a typical day, how would the area covered by B-AEDs compare to the area covered by S-AEDs?” In the second simulation, we asked the question, “What proportion of historical OHCA events would be covered by B-AEDs, S-AEDs and a combination of the two?”
Simulation 1: Geographic and Temporal Coverage Estimation
We began by estimating the effective geographic and temporal coverage of existing S-AEDs by calculating the total area of the city within a 1/8-mile radius (201m) of each device. S-AEDs do not move throughout the day, so in their respective geographic coverage areas, these AEDs provided 100% (i.e., 24hr) temporal coverage by definition. We discuss the limitations of this assumption later. We then estimated the geographic coverage provided by B-AEDs, i.e. AEDs moving about the city on buses. In the simulation, B-AEDs could only be accessed at published bus stops from within a 1/8-mile radius around each bus stop. Therefore, the geographic coverage provided by B-AEDs was calculated as the proportion of the city falling within 1/8-mile of a bus stop. The amount of temporal coverage each B-AED afforded around a given bus stop was not 100% by default (unlike S-AEDs) – because buses are not guaranteed to be near a bus stop -and was calculated as the proportion of the day during which a bus was within 2-minutes (roughly the time needed to cover 1/8 mile on foot) of arriving. Lastly, we superimposed these results upon each other to estimate the total geographic and temporal coverage that would be provided by adding B-AEDs to the existing S-AED system.
Simulation 2: Event Coverage Estimation
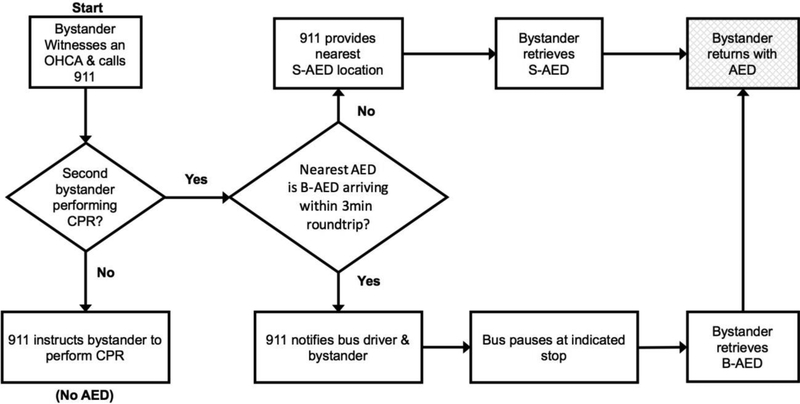
Next, we ran a simulation comparing AED accessibility and retrieval times between S-AEDs and B-AEDs using the location and event times of historical OHCAs. For each historical OHCA event, we first determined whether an S-AED was within 1/8-mile of the event. Then, for the same event, we determined if a B-AED would be accessible. In order to be accessible, a bus had to be arriving at a nearby bus stop in time to allow the bystander to retrieve the AED and return to the patient within 3 minutes, and without necessitating that the bus would deviate from its normal schedule (i.e., buses would not wait at the stop; the responder had to be there at or before its arrival). Figure 1 illustrates the details of this simulation.
Figure 1. Flow diagram of a combined B-AED and S-AED scenario.
A combined decision algorithm is shown encapsulating both scenarios simulated in Simulation #2. Following the upper path from the central node shows the S-AED retrieval process. Following the lower path shows the B-AED retrieval process. Abbreviations: B-AED – Bus AED, CPR – Cardiopulmonary Resuscitation, OHCA – Out-of-Hospital Cardiac Arrest, S-AED – Static AED.
Analysis
We summarized our geographic and temporal coverage results from Simulation 1 graphically in coverage-over-time plots for weekday, Saturday and Sunday transit schedules. We created a metric, Cumulative Geographic Coverage, with a range of [0 – 1] to gauge the total combined geographic and temporal coverage provided by B-AEDs and S-AEDs. To calculate this, we used custom MATLAB scripts (R2017a; The MathWorks, Natick, MA) to determine the total spatial area of the city that was within 1/8th mile of an AED at every minute of the day, summed these areas, and divided them by the total area of the city multiplied by the total number of minutes in a day. We also created heatmaps showing the geographic distribution of temporal coverage across the city.
For Simulation 2, we determined the proportion of the historical OHCA cases that had an AED that could be retrieved and returned to the patient’s side in 3 minutes for both the 1) B-AED and 2) S-AED scenarios, as well as the proportion of cases that had a retrievable AED under 3) either scenario. Event coverage proportions were compared separately between S-AED scenario and the two alternative scenarios with the Z-test for proportions, and by event residential status and weekday with the χ2 test. For those cases that did have an AED within a retrievable distance, average retrieval times were compared between scenarios 1, 2 and 3 while accounting for weekday/weekend period and residential event location status with ANOVA models.
To determine the potential influence of fluctuations in OHCA incidence on spatiotemporal coverage, we calculated the coefficient of variation (ratio of standard deviation to mean) of OHCA incidence across the capture period using a temporal comparative unit of year and geographic unit of city ward, a moderately sized political-geographic unit within the city, of which there are 32 in total. Coefficient of variation allows one to view the variability of a set of measures as a proportion of their mean instead of in absolute terms, affording a useful comparability between sets of measures across different time periods. All statistical calculations were performed in Stata 14 (Stata Corp, College Station, TX).
Results
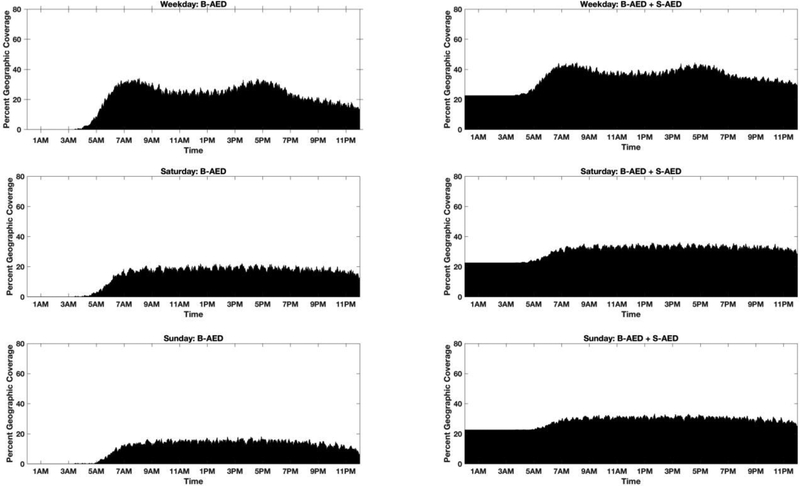
Figure 2 shows the temporal trends in geographic coverage across the City with B-AEDs alone and if B-AEDs were combined with S-AEDs. For B-AEDs alone, the minimum coverage was 0% given that buses did not run during late night / early morning hours. For a combination of both types of AED, minimal coverage (i.e., baseline S-AED coverage), in this scenario purely a function of the AED accessibility radius, was 23%. Cumulative geographic coverage on weekdays, Saturday and Sunday for B-AEDs alone were 20%, 14%, and 10%, respectively, compared to 34%, 30%, and 28% for a combined deployment of B-AEDs + S-AEDs. Weekday geographic coverage displayed a bimodality with peaks centered at times corresponding to peak commuter traffic (i.e., peak system demand), a phenomenon to that was not present in Saturday and Sunday coverage trends.
Figure 2. Temporal Trends in Geographic Coverage Across Time from Simulation #1.
Temporal trends in cumulative geographic AED coverage are shown for B-AEDs alone (left column) and B-AEDs combined with S-AEDs (right column) assuming a 1/8th mile accessibility radius. In the right column, the flat area of the plot during the early morning hours reflects availability of only S-AEDs when buses are not running. Abbreviations: B-AED – Bus AED, S-AED – Static AED.
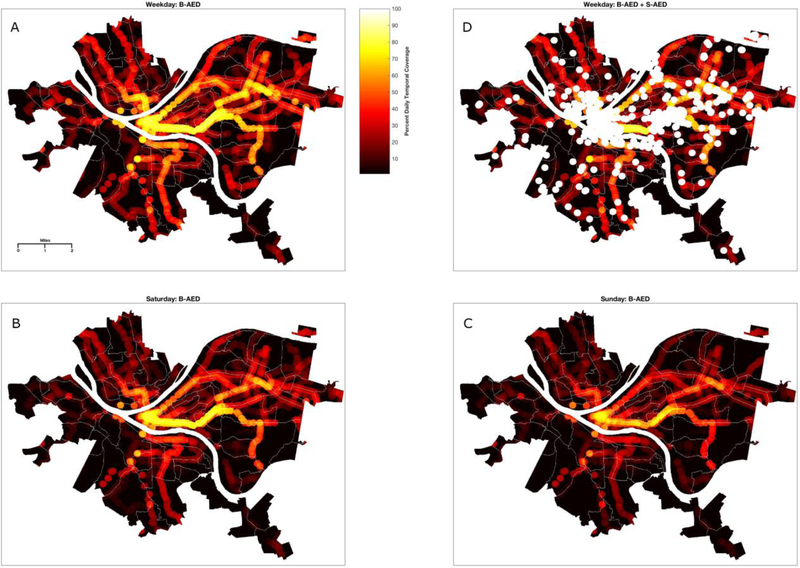
Figure 3 shows the geographic distribution of temporal coverage across the city for B-AEDs alone and when combined with S-AEDs. The theoretical maximum for any pixel on the plot is 100%, representing AED accessibility in that area for a full 24 hours a day, while the theoretical minimum is zero, representing no AED accessible within 1/8 mile at any time of day. The median (IQR) weekday temporal coverage with B-AEDs only was 5% (0 – 22) and with S-AEDs included was 9% (0 – 32). The maximum overall daily coverage observed in the Bus-Only scheme was 82%.
Figure 3. Geographic Distribution of Cumulative Temporal Coverage from Simulation #1.
The City of Pittsburgh, divided centrally by 3 major rivers, is shown with AED coverage radii of 1/8th mile superimposed in 4 panels. Lighter tone indicates a higher percentage of AED coverage throughout the day, while darker tone indicates a lower percentage of AED coverage throughout the day, with a range of 0 – 100%, where 100% indicates that an AED was with 1/8th mile of the applicable area for the entire 24-hour period. Panels A-C (counter clockwise from the top left) show B-AED coverage during weekdays, Saturday and Sunday. Panel D shows weekday B-AED coverage combined with S-AED coverage, which appears white relative to the same areas in Panel A due to the assumption of constant accessibility. Abbreviations: B-AED – Bus AED, S-AED – Static AED.
Table 1 summarizes the results of Simulation #2. OHCA event coverage was not different between B-AED and S-AED scenarios overall. However, allowing for retrieval of either type of AED resulted in a significantly higher event coverage proportion (22.4%; p<0.001) compared to the S-AED deployment. Mean qualifying AED retrieval times (i.e., times < 3min) did not differ between scenarios. Event coverage was significantly higher for events occurring in non-residential spaces than residential spaces for all scenarios, but qualifying retrieval times were only significantly lower in non-residential spaces than residential spaces for S-AEDs and the combined scenario. Weekday event coverage was significantly higher than weekend coverage for the B-AED scenario and the scenario allowing for retrieval of either type of AED, though qualifying retrieval times did not differ significantly. For comparison, among the historical cases included in this study, the actual mean (SD) time-to-arrival of the first EMS unit was 6.8 (2.8) minutes, with 95% of EMS response times being longer than 3 minutes, and 58% of EMS response times being longer than 6 minutes. Among this cohort, we also observed the following: the vast majority of events occurred in non-public residential settings (80.6%); bystanders witnessed the events only a fraction of the time (32.8%); among witnessed events, bystander resuscitation efforts were attempted 38.3% of the time; and AEDs were seldom applied by bystanders (9.2%).
Table 1.
Simulation #2 – Scenario Performance Characteristics
| Event Coverage, % (SE) | Overall | Weekday | Weekend | Residential | Non-Residential |
|---|---|---|---|---|---|
| B-AED | 12.3 (0.7) | 13.8 (0.9)† | 9.1 (1.2) | 9.4 (0.8)‡ | 21.4 (1.9) |
| S-AED | 14.0 (0.8) | 14.5 (1.0) | 12.8 (0.1) | 10.8 (0.8)‡ | 23.7 (1.9) |
| Either Available | 22.4 (0.9)* | 24.7 (1.20† | 19.5 (1.6) | 18.2 (1.0)‡ | 35.3 (2.2) |
| Mean Retrieval Time, s (SD) | |||||
| B-AED | 108.5 (47.0) | 108.8 (46.7) | 107.5 (48.6) | 112.4 (48.6) | 103.4 (44.5) |
| S-AED | 109.5 (44.5) | 108.6 (42.2) | 111.6 (50.3) | 117.8 (40.0)§ | 97.8 (47.9) |
| Either Available | 105.3 (46.2) | 103.9 (44.4) | 109.1 (50.9) | 113.3 (44.1)§ | 92.8 (46.9) |
Abbreviations: B-AED – Bus AED, S-AED – Static AED, s – Second, SE – Standard Error, SD – Standard Deviation.
Comparing event coverage between scenarios: “Either Available”, p < 0.001.
Comparing weekday to weekend event coverage: “B-AED”, p = 0.003; “Either Available”, p = 0.040.
Comparing residential to non-residential event coverage: p < 0.001 for all tests.
Comparing residential to non-residential retrieval times: “S-AED”, p = 0.0002; “Either Available”, p < 0.001.
Discussion
The results of our study provide a first look at the characteristics of a bus system-based AED deployment. Our results do not necessarily support unilateral deployment of AEDs on buses, but they provide an estimate of potential coverage benefits from a B-AED deployment under specific constraints. Considered alone, B-AEDs provided comparable response times and levels of historical event coverage but a lower level of geographic coverage relative to S-AEDs. When considered as a supplement to S-AEDs, B-AEDs resulted in a net increase in geographic and historical event coverage. This latter point indicates that B-AEDs go to areas that are not currently served by S-AEDs. The relative advantages and costs of addressing these gaps in AED coverage with limited B-AED deployments versus strategically placed S-AEDs remain to be seen.
The cost of deploying B-AEDs would be significant. In our study, we noted a local bus fleet of over 700 vehicles8, and analysis of the transit schedule reveals that there are between 1 and 548 buses on the road at any time. Therefore, at peak operating hours a B-AED system would require a “fleet” of at least 548 AEDs, a number comparable to the current S-AED deployment. Beyond initial device investment, B-AED deployment would depend on electronic infrastructure to manage the dispatching of the devices. The necessary integration of geospatial, infrastructure, and communication data streams has been demonstrated successfully in systems like PulsePoint9 and GoodSAM10, and likely could be adapted to B-AEDs if they proved worthwhile. But such systems would also contribute to B-AED system operating costs.
While AED use is known to be low in the United States on average, early defibrillation has saved lives and continues to be a goal of public health interventions to reduce OHCA mortality.11 Strategies to improve access to AEDs form part of a comprehensive approach to encouraging early defibrillation, but current PAD programs almost entirely limit publicly accessible AEDs to fixed locations, for lack of practicable competing strategies. Counterexamples include mobile, publicly accessible AEDs located on airplanes12,13 or ships14, which are clearly intended for use by their passengers, but perhaps more directly applicable are AEDs delivered by drones. Limited examples of the latter exist, although technological developments are increasing feasibility, which may increase usage.15,16 AED delivery via taxi service has also been attempted in at least one context.17 As with AED drones, the intent is to increase the reach of each AED by allowing it to travel to the OHCA event rather than rely on stationary devices happening to be nearby. B-AEDs offer a conceptually similar extension of AEDs beyond stationary deployments, offering an opportunity for accessibility across a broad geographic area, with the key difference that they could not practically be summoned with the destination specificity of a taxi or a drone. In this sense, they might present a practical middle ground between taxis/drones and S-AEDs for residential areas that have an existing bus network but do not have facilities to support S-AEDs, substantial taxi demand, or a drone network.
Designed as an initial investigation of a novel approach to public AED deployment, our study has several limitations. Most importantly, this study involved simulations, which made assumptions about AED accessibility distances (including the use of straight-line accessibility distances for our coverage estimates) and responder behavior that may not hold depending on geographic, cultural, or environmental conditions. The approach we chose gives a picture of what is possible under optimal circumstances; in real world circumstances, it is likely that event coverage and cumulative geographic coverage would be lower for myriad reasons. Additionally, our estimates did not directly take into account the proportion of population covered (although this is likely reflected in both the structure of the centrally planned bus network and the incidence of historical OHCA events), which might provide an additional dimension to our results. Relevant to the performance of public transportation systems in particular, we did not consider the effect of traffic fluctuations on system performance, nor did we consider the possible effects of construction detours, or holiday scheduling. Any reduction in the efficiency of the bus network would decrease the efficiency of buses as an AED delivery mechanism. We made assumptions about the accessibility of S-AEDs due to a lack of comprehensive building access schedule data, but actual accessibility may differ, and we could not fully account for vertical retrieval distance in the case of OHCAs occurring in high-rises, a difficult effect to estimate due to building heterogeneity. An inflation of coverage estimates resulting from not excluding potential building off-hours might be offset by the unlikelihood that bystanders would be available to retrieve an AED after hours, though this is not certain. Lastly, our observations with respect to event coverage must be tempered by consideration of the variability in incidence of cardiac arrest across the City (here quantified by the coefficient of variation); as in any city, PAD programs will be most successful when device locations closely match incidence patterns.
Conclusions
In these simulations, a standalone B-AED deployment in one city demonstrated less overall geographic coverage than existing S-AEDs. As a supplement to existing AEDs, B-AEDs increased historical event coverage and overall geographic coverage, indicating that a supplementary, rather than standalone, role may be worth additional exploration.
Acknowledgments
Dr. Salcido’s salary was supported during the study period by NHLBI grants (K12HL109068, R01HL117979, and R21HL135369) and grants from the Henry L. Hillman Foundation, which also supports the Resuscitation Logistics and Informatics Venture.
References
- 1.Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002. Oct 17;347(16):1242–7. [DOI] [PubMed] [Google Scholar]
- 2.Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000. Oct 26;343(17):1206–9 [DOI] [PubMed] [Google Scholar]
- 3.Berdowski J, Blom MT, Bardai A, Tan HL, Tijssen JG, Koster RW. Impact of onsite or dispatched automated external defibrillator use on survival after out-of-hospital cardiac arrest. Circulation. 2011. Nov 15;124(20):2225–32. [DOI] [PubMed] [Google Scholar]
- 4.Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, Zalenski R, Becker LB, Schron EB, Proschan M; Public Access Defibrillation Trial Investigators.. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004. Aug 12;351(7):637–46. [DOI] [PubMed] [Google Scholar]
- 5.Dahan B, Jabre P, Karam N, Misslin R, Bories MC, Tafflet M, Bougouin W, Jost D, Beganton F, Beal G, Pelloux P, Marijon E, Jouven X. Optimization of automated external defibrillator deployment outdoors: An evidence-based approach. Resuscitation. 2016. Nov;108:68–74. [DOI] [PubMed] [Google Scholar]
- 6.Sun CLF, Brooks SC, Morrison LJ, Chan TCY, and On behalf of the Rescu Epistry Investigators. Ranking Businesses and Municipal Locations by Spatiotemporal Cardiac Arrest Risk to Guide Public Defibrillator Placement. Circulation. 2017;135:1104–1119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Srinivasan S, Salerno J, Hajari H, Weiss LS, Salcido DD. Modeling a Novel Hypothetical Use of Postal Collection Boxes as Automated External Defibrillator Access Points. Resuscitation. 2017. Aug 25. pii: S0300–9572(17)30554–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Port Authority of Allegheny County (n.d.). Retrieved September 6, 2017 http://www.portauthority.org/paac/CompanyInfoProjects/AgencyProfile.aspx
- 9.Brooks SC, Simmons G, Worthington H, Bobrow BJ, Morrison LJ. The PulsePoint Respond mobile device application to crowdsource basic life support for patients with out-of-hospital cardiac arrest: Challenges for optimal implementation. Resuscitation. 2016. Jan;98:20–6. [DOI] [PubMed] [Google Scholar]
- 10.GoodSam App (n.d.). Retrieved September 6, 2017 https://www.goodsamapp.org/
- 11.Daya M, Schmicker R, May S, and Morrison L. 2015. Current burden of cardiac arrest in the United States: Report from the Resuscitation Outcomes Consortium. Paper commissioned by the Committee on the Treatment of Cardiac Arrest: Current Status and Future Directions. http://www.nationalacademies.org/hmd/%20~/media/Files/Report%20Files/2015/ROC.pdf. Retrieved September 6, 2017.
- 12.Groeneveld PW, Kwong JL, Liu Y, Rodriguez AJ, Jones MP, Sanders GD, Garber AM. Cost-effectiveness of automated external defibrillators on airlines. JAMA. 2001. Sep 26;286(12):1482–9. [DOI] [PubMed] [Google Scholar]
- 13.Bertrand C, Rodriguez Redington P, Lecarpentier E, Bellaiche G, Michel D, Teiger E, Morris W, Le Bourgeois JP, Barthout M. Preliminary report on AED deployment on the entire Air France commercial fleet: a joint venture with Paris XII University Training Programme. Resuscitation. 2004. Nov;63(2):175–81. [DOI] [PubMed] [Google Scholar]
- 14.Oldenburg M, Baur X, Schlaich C. Assessment of three conventional automated external defibrillators in seafaring telemedicine. Occup Med (Lond). 2012. Mar;62(2):117–22. [DOI] [PubMed] [Google Scholar]
- 15.Pulver A, Wei R, Mann C. Locating AED Enabled Medical Drones to Enhance Cardiac Arrest Response Times. Prehosp Emerg Care. 2016. May–Jun;20(3):378–89. [DOI] [PubMed] [Google Scholar]
- 16.Boutilier JJ, Brooks SC, Janmohamed A, Byers A, Buick JE, Zhan C, Schoellig AP, Cheskes S, Morrison LJ, Chan TCY; Rescu Epistry Investigators. Optimizing a Drone Network to Deliver Automated External Defibrillators. Circulation. 2017. Jun 20;135(25):2454–2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ng YY, Leong SH, Ong ME. The role of dispatch in resuscitation. Singapore Med J. 2017. Jul;58(7):449–452. [DOI] [PMC free article] [PubMed] [Google Scholar]