Abstract
Background/Objectives:
Weight-related quality of life (WRQOL) and generic health-related quality of life (HRQOL) have been identified as important patient reported outcomes for obesity treatment and outcome research. This study evaluated patterns of WRQOL and HRQOL outcomes for adolescents at 24-months post-bariatric surgery relative to a non-surgical comparator sample of youth with severe obesity, and examined potential weight-based (e.g., BMI, weight dissatisfaction) and psychosocial predictors and correlates of these outcomes.
Subjects/Methods:
Multi-site data from 139 adolescents undergoing bariatric surgery (Mage=16.9; 79.9% female, 66.2% White; MBody Mass Index [BMI]= 51.5kg/m2) and 83 comparators (Mage=16.1; 81.9 % female, 54.2% White; MBMI= 46.9kg/m2) were collected at pre-surgery/baseline, 6-, 12-, and 24-months post-surgery/baseline with high participation rates across time points (>85%). Self-reports with standardized measures of WRQOL/HRQOL as well as predictors/covariates (e.g., weight dissatisfaction, social support, peer victimization, family dysfunction, loss of control eating, self-worth, and internalizing symptoms) were obtained. Growth curve models using structural equation modeling examined WRQOL/HRQOL over time and linear regressions examined predictors and correlates of WRQOL/HRQOL outcomes.
Results:
Significant improvement in WRQOL and Physical HRQOL, particularly in the first post-operative year with a leveling off subsequently, was found for the surgical group relative to comparators, but with no significant Mental HRQOL change. At 24 months, the surgical group had signficantly greater WRQOL/HRQOL across most subscales. Within the surgical group at 24 months, weight-based variables were signficantly associated with WRQOL and Physical HRQOL, but not Mental HRQOL. Mental HRQOL was associated with greater internalizing symptoms and loss of control eating.
Conclusions:
For adolescents undergoing bariatric surgery, most clinically meaningful changes in WRQOL and Physical HRQOL occurred early post-operatively, with weight-based variables as the primary drivers of 24-month levels. In contrast, expectations for Mental HRQOL improvement following surgery should be tempered, with 24-month levels significantly associated with psychosocial rather than weight-based correlates.
Introduction
Consistent with precision medicine initiatives in obesity treatment (1), it is imperative to examine who most benefits from bariatric surgery, and further, what factors account for variability in outcomes, to inform individualized treatment pathways. Inherent in this precision is an informed selection of patient-reported outcomes (PROs). Quality of life (QOL) is a key PRO recommended for use in clinical trials and observational studies (e.g., FDA(2), CONSORT(3)). Accordingly, QOL assessments pre/post-surgery serve as a primary PRO of bariatric surgery, tracking the patient’s perspective on how surgical weight loss affects day-to-day life across multiple domains (e.g., physical, social, emotional). Overall, the resounding message is that QOL is markedly impaired in adolescents with severe obesity (4, 5), yet improves rapidly and early, post-bariatric surgery (6–12). With two exceptions (13, 14), these studies have been of short duration, cross-sectional, lacked non-surgical comparison groups, and/or used measures not developed or validated with adolescents.
To date, multiple QOL measures have been used in the adolescent bariatric literature, from generic (e.g., health-related quality of life [HRQOL]) to condition-specific (e.g., weight-related quality of life [WRQOL]). Given this variability, it is unclear in which QOL domains the most benefits lie. For example, the adult bariatric literature suggests that a focus on “total” scores can obscure significantly greater post-operative improvements in physical QOL domains relative to psychosocial domains (15, 16). The Swedish Adolescent Morbid Obesity Study (AMOS) reported significant improvements two years following Roux-en-Y gastric bypass (RYGB) in the Physical but not Mental HRQOL summary scores of the generic Short Form-36 (SF-36) (11). In addition, a growing literature suggests there is heterogeneity across other secondary psychosocial or behavioral outcomes. For example, for some adolescents, pre-operative psychopathology or loss of control (LOC) eating persist even with surgical weight loss (17–19) while problematic risk behaviors (e.g., alcohol use disorder), may newly emerge post-operatively (20). Moreover, most continue to meet criteria for obesity, or even severe obesity. Whether these contexts affect QOL outcomes is less well known.
Despite the importance of QOL as a PRO, minimal research has addressed potential predictors and correlates. In addition to post-surgical weight loss, other weight-based correlates have been demonstrated as influential on QOL. For instance, while perceptions of current body size at 12 months post-surgery were unrelated to total WRQOL in a small sample of adolescent patients, the discrepancies between these perceptions and ideal body size were significantly associated with WRQOL (21). Beyond weight-based factors, psychosocial and behavioral factors (e.g., LOC eating (22), depressive symptoms and binge eating (5)) have been found to be significant correlates of impaired WRQOL prior to surgery. These psychosocial factors may gain increasing importance after the first year post-operatively when the effects of surgery lessen (23). In the adult literature, consistent pre-operative predictors of post-operative HRQOL have included depressive symptomatology (23, 24) and binge eating severity (24).
Although the extant pediatric obesity literature has identified several predictors and correlates of HRQOL/WRQOL (e.g., depressive symptoms (5, 25, 26), social support (26), peer victimization (25, 27), parent distress (25)), to our knowledge, comprehensive modeling of predictors and correlates of QOL after bariatric surgery is limited. Broadening the scope of predictors/correlates beyond the current literature will aid in understanding QOL variability and in identifying both risk and protective factors after surgery to inform adolescent intervention efforts.
We utilized a unique and well-characterized longitudinal sample of adolescents with severe obesity who underwent bariatric surgery to evaluate patterns of HRQOL/WRQOL outcomes through 24-months post-operatively. Based on extant literature, we expected the surgical group to demonstrate significant improvements over time in summary scores of Physical HRQOL and WRQOL (Total), but no significant change in Mental HRQOL. This first aim was enhanced by including a nonsurgical group of adolescent comparators with severe obesity followed over the same course of time. Our second aim was to examine potential weight-based correlates of QOL outcomes at 24 months. Pre-operative BMI as well as 24-month measures (percent weight loss, post-operative BMI and body dissatisfaction), were expected to be associated with total WRQOL and Physical HRQOL, but not Mental HRQOL. Finally, our third aim was to examine whether pre-surgical or concurrent psychosocial factors explained QOL 24-month outcomes. We hypothesized that adolescents with greater internalizing symptoms, family dysfunction, and peer victimization; lower social support and global self-worth; and LOC eating would report poorer QOL at 24-months, particularly Mental Health HRQOL.
Method
Study Design Overview
The present analyses utilized data from the TeenView study and its parent study, the Teen Longitudinal Assessment of Bariatric Surgery (Teen-LABS) consortium, a prospective observational cohort study at five academic tertiary care centers in the United States documenting the safety and efficacy of bariatric surgery in 242 adolescents (enrollment 2007–2011) (12, 28, 29). TeenView recruitment (2008–2012) included Teen-LABS participants (“surgical”) as well as a demographically similar group of adolescents with severe obesity (“comparators”). TeenView was designed, not as a comparative intervention trial, but to examine psychosocial benefits and risks associated with bariatric surgery relative to a “natural course” of those with severe obesity. Each Institutional Review Board approved study protocols, and participants provided written assent/consent.
Participants
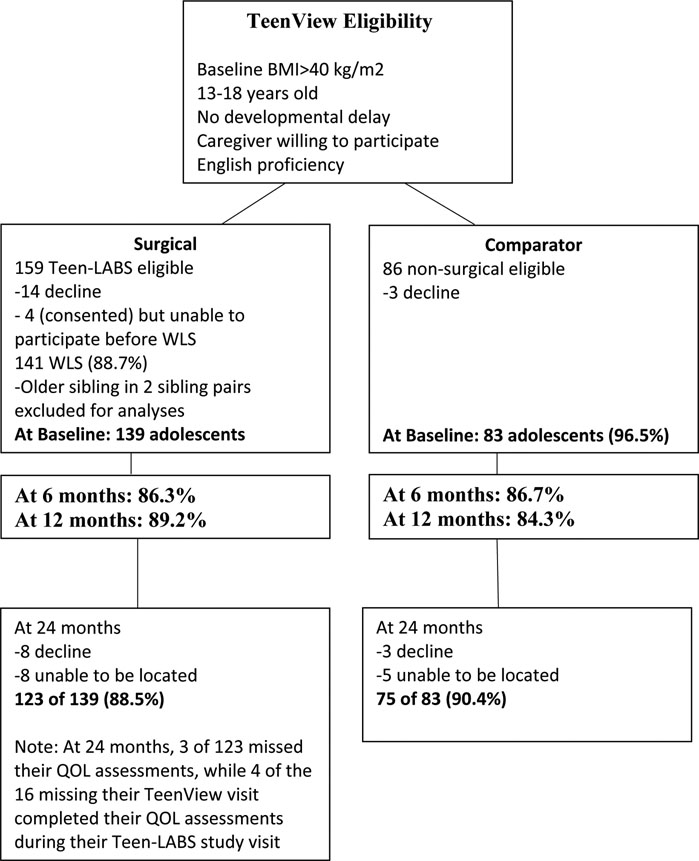
TeenView participants and procedures have been reported previously (30–32) with eligibility criteria and participation rates detailed in Figure 1. Comparators were recruited from TeenView research registries identifying eligible youth presenting at lifestyle modification programs at each care center whose families agreed to be contacted should the adolescent become a demographic match (i.e., sex, ethnicity, +/− 6 months in age) to a surgical participant at any site.
Figure 1.
TeenView participant recruitment and retention.
Procedure
Baseline/pre-surgery (within 30 days prior to surgery) and follow-up assessments were completed at each care center with heights/weights measured by trained personnel. Participants not attending a 24-month visit in person completed paper/pencil forms at home or via a web-based platform, with height/weight obtained via field visits by study affiliates for the surgical group (n=18) or as self-report for comparators (n=5). For the present analyses, adolescent self-reported QOL at baseline/pre-surgery, 6-, 12-, and 24-months were used. All other measures were adolescent-report at baseline and 24 months, with the exception of adolescent-reported weight dissatisfaction (24 months only) and caregiver reported demographics (baseline only).
Measures
Primary Outcomes
Impact of Weight on Quality of Life-Kids (IWQOL-Kids) (33).
The IWQOL-Kids is a 27-item report of WRQOL with a Total score and subscales indicating the impact of weight on: comfort and mobility (i.e., Physical Comfort); feelings about their body (i.e., Body Esteem); peer relationships (i.e., Social Life); and family members’ feelings about the adolescent and their weight (i.e., Family Life). Raw scores were transformed (0–100 scale), with higher scores representing better WRQOL. This measure has excellent psychometrics, including internal consistency for the current sample (Cronbach’s alpha: surgical=0.83–0.94; comparators=0.81–93). Minimal clinically important difference scores (MCIDs) have been defined as: 4.8 (Total), 8.8 (Physical Comfort), 7.7 (Body Esteem), 8.1 (Social Life), and 6.2 (Family Relations) (34).
Short Form-36 (SF-36) (35).
The SF-36 is a self-report of generic HRQOL with subscales of Physical Function, Role-Physical, Body Pain, General Health Perceptions, Vitality, Social Function, Role-Emotional, and Mental Health. The Mental Component Summary (Mental HRQOL) and the Physical Component Summary (Physical HRQOL) are norm-based, standardized scores, with higher scores representing better functioning. This measure has excellent psychometrics and can be used for adolescents 14 years and older (36, 37), with good internal consistency for the current sample (Cronbach’s alpha: surgical=0.74–0.93; comparators=0.70–0.89). Effect size estimates between time points were used to describe MCIDs similar to other QOL research.(38)
Predictors and Correlates
BMI, percent weight loss, and weight dissatisfaction.
Height and weight were used to calculate BMI. Percent weight loss was calculated as ([weightpre-surgery – weightfollow-up] /weightpre-surgery)*100. Participants were also asked to provide their current “dream weight” which was subtracted from current weight to create a discrepancy score, with larger scores representing greater weight dissatisfaction.
Children’s Social Support Questionnaire (CSSQ) (39).
The CSSQ measured perception of social support quality. Adolescents listed people in their “social network” and rated how happy they were with each relationship (1=very unhappy to 5=very happy), with ratings averaged across individuals. This measure has acceptable psychometrics (39).
Family Assessment Device (FAD) (40).
The FAD General Functioning scale assessed adolescent perception of family dysfunction, with higher scores representing greater dysfunction. This scale has demonstrated good validity, with good internal consistency for the current sample (αbaseline=0.88; α24-month=0.88).
Questionnaire on Eating and Weight Patterns-Revised (QEWP-R)(41).
Using items adapted from the QEWP-R, LOC eating was classified as present if participants endorsed yes to: “During the past 6 months, have you had times when you eat continuously during the day or parts of the day without planning what and how much you would eat?”; and “Did you experience a loss of control, that is, you felt like you could not control your eating?”. The QEWP-R has acceptable psychometrics (41).
Revised Peer Experiences Questionnaire (RPEQ)(42).
The RPEQ is a self-report of overt (e.g., “hit, kicked, or pushed”), relational (e.g., “left me out”), and reputational (e.g., “gossiped about me”) victimization during the past year (1=never to 5=a few times/week). This measure has acceptable psychometrics (42, 43). A total score averaging all subscale items was used, with good internal consistency for the current sample (αbaseline=0.78; α24-month=0.75).
Self-Perception Profile for Adolescents (SPPA) (44).
The SPPA is 45-item measure assessing self-perceptions of competence, rated from “1” (low) to “4” (high). Although self-concept is multi-dimensional, the global self-worth scale (5 items), indicating how happy adolescents are with themselves, was selected for use. This measure has demonstrated good validity (44), as well as good internal consistency for global self-worth for the current sample (αbaseline= 0.80; α24-months= 0.87).
Youth Self-Report (YSR) (45).
Self-reported internalizing symptoms in the past 6 months were assessed via the YSR which has well-established psychometric properties (45, 46), and has been used extensively with youth with chronic medical conditions (47).
Statistical Analyses
Missing data (0.8%−4.0%) were handled via maximum likelihood estimation. Nesting of participants within the five sites was controlled via specialized commands (i.e., ‘Cluster=site’ and ‘Type=Complex’) in Mplus v7.3 to avoid Type-1 errors. All p-values were two-tailed. T-tests and chi-square tests were used to examine demographic factors and BMI for surgical versus comparator groups and those completing 24-month assessments versus those who did not.
For Aim 1, group differences (surgical vs comparator) in mean levels of WRQOL/HRQOL were tested with analyses of covariance (ANCOVA). Cohen’s d effect sizes were computed. Growth curve models were estimated using structural equation modeling to test for change over time in WRQOL/HRQOL by group. For Aims 2 and 3, a series of linear regression analyses for the surgical group examined weight-based and psychosocial predictors of Physical HRQOL, Mental HRQOL, and total WRQOL at 24 months. Each weight-based variable was tested in a separate model due to potential collinearity, along with covariates. For psychosocial variables, a pre-surgical and 24-month model were completed for each QOL score.
Results
Participant Characterisitics
At baseline, adolescents in the surgical group were signficantly older with a higher BMI relative to comparators, but by 24-months, had a significantly greater percent weight loss and lower BMI (Table 1). Participants completing 24-month QOL assessments (n=199) were not signifcantly different from those who did not (n=23) for baseline QOL subscales, as well as group (surgical versus comparators), sex, ethnicity, age, and BMI.
Table 1.
Demographic characteristics of adolescents in the surgical group and nonsurgical comparators.
|
Demographic characteristics |
Surgical | Comparator | |
|---|---|---|---|
| Mean ± SD n (%) |
Mean ± SD n (%) |
pa | |
| Pre-surgery/Baseline | n=139 | n=83 | |
| Sex (% Female) | 111 (79.9%) | 68 (81.9%) | 0.71 |
| Ethnicity (% White) | 92 (66.2%) | 45 (54.2%) | 0.08 |
| Caregiver Education (% ≤ High School Graduation)b | 53 (39.0%) | 40 (48.2%) | 0.18 |
| BMI | 51.52±8.32 | 46.85±6.12 | <0.001 |
| Surgical Procedure | |||
| RYGB | 86 (61.9%) | ||
| SG | 50 (36.0%) | ||
| AGB | 3 (2.2%) | ||
| 24 Months | n=124 | N=75 | |
| Age | 19.09±1.35 | 18.28±1.36 | <0.001 |
| BMIc | 36.01±8.55 | 48.65±8.37 | <0.001 |
| % Change in Weightd | −29.96±11.15 | 6.97±10.81 | <0.001 |
| Living with Parent or other Relative at 24 monthse | 97 (78.9%) | 68 (93.2%) | 0.01 |
Note: AGB= adjustable gastric banding; BMI= Body Mass Index; RYGB=Roux-en-Y gastric bypass; SG=sleeve gastrectomy
p-values are based on two-tailed independent t-tests when examining mean values and on Chi-Square tests when examining percentages.
Missing for n=3 Surgical and n=0 Comparator.
Missing for n=2 Surgical and n=8 Comparator.
((weight24-months - weightpre-surgery/baseline) /weightpre-surgery/baseline)*100; Missing for n=8 Comparator.
Missing for n=1 Surgical and n=2 Comparator.
Aim 1: Change in WRQOL and HRQOL
Table 2 presents the means and standard deviations for WRQOL (i.e., IWQOL-Kids) and HRQOL (SF-36) for surgical and comparator groups across time, with analysis presented for the 24-month timepoint. Given unequal group sizes and the lack of homogeneity of variance, the significance level for these analyses was set at p≤0.01 to control for Type-1 errors. Controlling for age, baseline BMI, and corresponding baseline QOL, the surgical group reported significantly higher WRQOL (i.e., all scales with the exception of Family Relations) relative to comparators at 24-months. The surgical group also reported significantly higher Physical HRQOL and for all subscales, with the exception of Mental HRQOL and the Role-Emotional and Mental Health subscales. Effect sizes were generally medium to large for WRQOL and the physical subscales of HRQOL, but medium for mental subscales of HRQOL. Supplemental Table 1 presents WRQOL/HRQOL means and standard deviations for the surgical group by procedure (RYGB, Sleeve Gastrectomy).
Table 2.
Mean quality of life at pre-surgery/baseline, and at 6-, 12-, and 24-months post-surgery/post-baseline for adolescents in the surgical group and comparators.
| Pre-surgical/ Baseline |
6 Months | 12 Months | 24 Months | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Surg n=137 Mean (SD) |
Comp n=83 Mean (SD) |
Surg n=120 Mean (SD) |
Comp n=72 Mean (SD) |
Surg n=123 Mean (SD) |
Comp n=70 Mean (SD) |
Surg n=124 Mean (SD) |
Comp n=75 Mean (SD) |
Esta | p | Cohen’s db | |
| IWQOL-Kids | |||||||||||
| Total Score | 63.67 (17.40) | 66.02 (18.25) | 83.31 (13.88) | 69.24 (18.59) | 86.52 (13.59) | 71.43 (19.09) | 86.52 (13.60) | 71.44 (16.99) | 17.75 | <0.001 | 1.01 |
| Physical Comfort | 54.71 (24.62) | 69.28 (20.74) | 85.59 (16.34) | 69.71 (20.70) | 91.43 (12.84) | 69.62 (23.47) | 90.26 (15.11) | 68.83 (22.84) | 29.71 | < 0.001 | 1.16 |
| Body Esteem | 46.47 (27.97) | 48.90 (28.93) | 70.86 (23.88) | 53.04 (28.48) | 74.71 (25.13) | 58.27 (27.42) | 73.68 (25.78) | 55.90 (28.71) | 21.26 | < 0.001 | 0.66 |
| Social Life | 70.35 (21.96) | 71.02 (26.31) | 86.74 (16.29) | 77.20 (24.55) | 89.16 (15.98) | 79.46 (23.01) | 92.37 (12.24) | 81.74 (17.32) | 13.07 | <0.001 | 0.77 |
| Family Relations | 91.73 (15.28) | 83.17 (23.08) | 96.32 (10.24) | 85.07 (22.24) | 96.68 (8.13) | 84.82 (23.10) | 96.17 (9.70) | 87.06 (17.43) | 4.61 | 0.03 | 0.69 |
| SF-36 | |||||||||||
| Physical HRQOL | 44.95 (8.46) | 45.63 (7.88) | 53.08 (6.83) | 46.98 (8.81) | 53.93 (6.48) | 46.52 (8.38) | 53.45 (6.83) | 47.30c (8.49) | 7.10 | <0.001 | 0.82 |
| Mental HRQOL | 49.69 (9.70) | 44.79 (9.68) | 51.31 (9.65) | 46.03 (10.54) | 51.16 (10.37) | 44.89 (11.09) | 49.73 (11.12) | 44.38c (10.98) | 3.17 | 0.09 | 0.48 |
| Physical Functioning | 66.46 (23.62) | 67.23 (26.75) | 85.86 (20.98) | 75.63 (22.09) | 87.80 (20.95) | 70.16 (26.04) | 89.48 (19.67) | 75.66c (22.54) | 15.04 | <0.001 | 0.66 |
| Role - Physical | 70.62 (35.21) | 68.07 (37.92) | 91.46 (21.62) | 69.44 (34.91) | 91.06 (21.74) | 73.93 (32.81) | 91.13 (22.81) | 76.33 (31.00) | 16.34 | <0.001 | 0.57 |
| Bodily Pain | 72.89 (24.42) | 70.57 (20.24) | 83.70 (18.77) | 68.58 (25.62) | 83.80 (20.65) | 67.63 (23.27) | 79.58 (23.05) | 67.21 (23.33) | 10.95 | <0.001 | 0.53 |
| General Health | 51.81 (18.61) | 45.50 (17.96) | 69.40 (17.52) | 48.40 (21.82) | 72.61 (18.13) | 48.19 (24.61) | 69.29 (17.91) | 45.52c (21.50) | 22.37 | <0.001 | 1.23 |
| Vitality | 53.13 (18.11) | 49.76 (19.71) | 65.24 (19.72) | 55.25 (21.16) | 68.09 (18.64) | 50.43 (20.14) | 60.32 (21.32) | 49.51 (20.70) | 10.15 | <0.001 | 0.51 |
| Social Functioning | 76.46 (23.58) | 72.29 (22.09) | 85.94 (19.55) | 76.74 (25.64) | 86.08 (19.75) | 73.21 (23.73) | 86.19 (21.73) | 74.67 (24.66) | 10.41 | 0.01 | 0.50 |
| Role - Emotional | 80.54 (29.88) | 66.27 (38.07) | 89.17 (27.04) | 70.37 (39.78) | 86.72 (26.90) | 70.48 (39.94) | 87.90 (28.62) | 72.89 (37.04) | 10.12 | 0.14 | 0.47 |
| Mental Health | 73.15 (17.94) | 65.06 (19.58) | 77.37 (16.81) | 66.29 (19.75) | 77.56 (19.42) | 64.06 (17.79) | 74.74 (19.92) | 63.36 (19.30) | 7.46 | 0.02 | 0.58 |
Note: Comp= Comparator; IWQOL-Kids = Impact of weight of quality of life-Kids; SF-36 = Short Form-36; Surg=Surgical
Comparing outcomes at 24 months for Surgical and Comparator groups using multivariate analysis of covariance after controlling for baseline age, BMI, and the corresponding quality of life measure. Given unequal group sizes and the lack of homogeneity of variance, the significance level for these analyses was set at p≤0.01 (two-tailed) to control for Type-1 errors.
Effect sizes at 24 months are reported as Cohen’s d, and are defined at small = 0.20, medium = 0.50, and large = 0.80.
Missing for n=1.
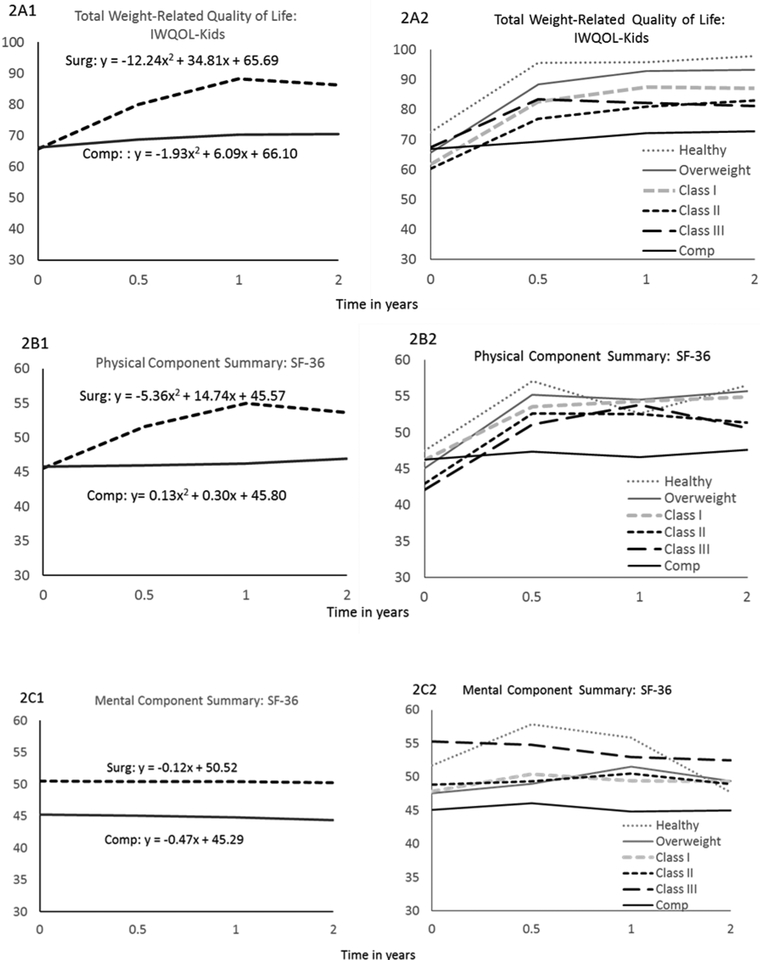
Change over time in Total WRQOL, Physical HRQOL, and Mental HRQOL are presented in Figure 2 (2A.1, 2B.1,2C.1) for surgical and comparator groups. Total WRQOL (p=0.78) and Physical HRQOL (p=0.88) intercepts did not significantly differ by group for either measure, indicating that surgical and comparator groups reported similar WRQOL and Physical HRQOL at baseline. A significant quadratic slope for the group by time interaction was indicated for Total WRQOL (p<0.001) as well as for Physical HRQOL (p<0.001), with the surgical group exhibiting improvement in both to the first post-operative year with a subsequent leveling off and slight decline across the second year. For Mental HRQOL, analyses indicated a significant intercept group difference (p<0.001) and a non-signficant linear group by time interaction for slope (p=0.57), indicating the surgical group reported significantly higher initial Mental HRQOL than comparators, yet similar patterns of change over time.
Figure 2.
Change in total weight-related quality of life (WRQOL), physical health-related quality of life (HRQOL), and mental health-related quality of life over time.
Note: The Total score of the Impact of Weight on Quality of Life-Kids (IWQOL-Kids) was created by transforming raw scores to a 0–100 scale, with higher scores representing better total WRQOL. The Physical Component Summary (Physical HRQOL) and Mental Component Summary (Mental HRQOL) of the Short Form-36 (SF-36) are norm-based, standardized scores based on the general population of the United States with a mean of 50 and a standard deviation of 10. The y-axes of the graphs above are adjusted accordingly. Expected means (2A.1, 2B.1, 2C.1) were plotted from longitudinal analyses within a structural equation modeling framework for each outcome over time for surgical patients (Surg) and non-surgical comparators (Comp). Observed means (2A.2, 2B.2, 2C.2) for each outcome are plotted over time for surgical patients classified by BMI group at 24 months and comparators. BMI classifications were healthy (BMI=18.5–24.9, n=6), overweight (BMI=25.0–29.9, n=25), Class I obesity (BMI=30.0–34.9, n=37), Class II obesity (BMI=35.0–39.9, n=24), and Class III obesity (BMI≥40.0, n=30).
Clinically meaningful improvements based on MCID parameters were detected for the surgical group for Total WRQOL as well as the weight-related Physical Comfort, Body Esteem, and Social Life subscales from baseline to 6 months post-operatively, with none subsequently. For the SF-36, a large effect size (Cohen’s d=1.05) was indicated for Physical HRQOL from baseline to 6 months post-operatively, with small effects from 6- to 24-months (d6–12m= 0.13; d12–24m=0.07). Small effects were indicated for all times for Mental HRQOL (d=0.01–0.17). Although longitudinal and MCID analyses indicate clear group patterns/trajectories for mean QOL, there is much heterogeneity within the surgical group, evident when observed QOL means are plotted over time after classifying participants into weight status groups (i.e., healthy weight, overweight, Class I-III obesity) using 24-month BMI (Figure 2A.2, 2B.2, 2C.2).
Aim 2: Weight-based correlates of WRQOL and HRQOL at 24 months
Separate regression models were tested to examine weight-based predictors of Total WRQOL, Physical HRQOL, and Mental HRQOL for the surgical group at 24 months, with sex, ethnicity, age and corresponding baseline QOL as covariates (Table 3). Lower post-surgical BMI, greater percent weight loss, and lower weight dissatisfaction were concurrently associated with significantly higher WRQOL, while only greater percent weight loss was associated with significantly higher Physical HRQOL.
Table 3.
Pre-operative predictors and concurrent (24-month) correlates of weight-related and health-related quality of life for adolescents in the surgical group.
| Total WRQOLa at 24 | Physical HRQOLb at 24 | Mental HRQOLc at 24 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Regression models for Weight-based Variablesd | βe | p | 95% CI for β | βe | p | 95% CI for β | βe | p | 95% CI for β |
| 1. Pre-surgical BMI | −0.09 | 0.51 | [−0.32, 0.27] | 0.09 | 0.20 | [−0.001, 0.22] | 0.19 | 0.03 | [0.12, 0.46] |
| 2. BMI at 24 months | −0.53 | <0.001 | [−0.73, −0.12] | −0.11 | 0.15 | [−0.34, −0.03] | 0.12 | 0.32 | [−0.11, 0.21] |
| 3. % Weight Loss (24 months)f | 0.55 | <0.001 | [0.32, 0.70] | 0.19 | <0.001 | [0.11, 0.29] | 0.06 | 0.56 | [−0.09, 0.28] |
| 4. Weight Dissatisfaction (24 months) | −0.30 | <0.01 | [−0.46, −0.13] | −0.06 | 0.10 | [−0.15, −0.01] | 0.01 | 0.94 | [−0.16, 0.07] |
| Baseline Psychosocial Variables | βe | p | 95% CI for β | βe | p | 95% CI for β | βe | p | 95% CI for β |
| Sex (0=male, 1=female) | −7.62 | 0.01 | [−10.27, −0.10] | −1.69 | 0.09 | [−3.93, −0.21] | −5.17 | 0.03 | [−10.01, −0.72] |
| Ethnicity (0=White, 1=non-White) | 1.60 | 0.54 | [−0.49, 8.36] | −2.45 | 0.06 | [−3.61, 0.70] | 3.84 | 0.03 | [0.22, 5.87] |
| Age | −1.46 | 0.24 | [−3.94, 0.16] | −0.19 | 0.65 | [−1.34, 0.27] | −1.11 | 0.13 | [−2.74, −0.32] |
| Baseline of Dependent Variableg | 0.22 | <0.01 | [0.12, 0.36] | 0.38 | <0.01 | [0.25, 0.58] | 0.13 | 0.39 | [−0.14, 0.20] |
| Family Dysfunction | 1.80 | 0.49 | [−1.59, 7.46] | 1.39 | 0.65 | [−1.08, 9.22] | −1.00 | 0.74 | [−9.14, 1.80] |
| Internalizing | −0.03 | 0.85 | [−0.12, 0.51] | −0.01 | 0.96 | [−0.33, 0.12] | −0.22 | 0.39 | [−0.51, 0.42] |
| Global Self-Worth | 4.26 | 0.06 | [−1.63, 6.12] | 0.43 | 0.60 | [−0.68, 2.23] | 0.17 | 0.91 | [−2.52, 2.95] |
| Loss of Control Eating | −0.41 | 0.91 | [−7.24, 2.32] | −0.43 | 0.83 | [−2.84, 5.29] | 0.06 | 0.97 | [−3.30, 2.17] |
| Total Victimization | 1.48 | 0.75 | [−12.87, 5.64] | −0.19 | 0.84 | [−1.03, 1.68] | −0.15 | 0.97 | [−10.09, 3.15] |
| Happiness with Social Support | 0.79 | 0.61 | [−2.58, 2.79] | 0.74 | 0.16 | [0.12, 2.02] | 0.04 | 0.98 | [−3.27, 1.27] |
| 24 Month Psychosocial Variables | βe | p | 95% CI for β | βe | p | 95% CI for β | βe | p | 95% CI for β |
| Sex (0=male, 1=female) | −7.48 | <0.01 | [−8.95, 0.42] | −2.00 | 0.24 | [−5.23, 0.16] | −4.43 | 0.03 | [−7.81, 1.81] |
| Ethnicity (0=White, 1=non-White) | 0.20 | 0.92 | [−2.70, 4.37] | −2.90 | 0.05 | [−5.56, −0.01] | 1.41 | 0.52 | [−2.82, 5.23] |
| Age | −0.81 | 0.47 | [−2.97, 0.57] | −0.28 | 0.56 | [−1.53, 0.22] | −0.07 | 0.91 | [−1.05, 1.00] |
| Baseline of Dependent Variableg | 0.14 | 0.03 | [−0.003, 0.27] | 0.39 | <0.001 | [0.20, 0.56] | 0.12 | 0.47 | [−0.19, 0.22] |
| Family Dysfunction | 2.57 | 0.50 | [−1.58, 10.03] | 0.26 | 0.89 | [−3.04, 3.04] | −0.17 | 0.92 | [−3.73, 2.74] |
| Internalizing | −0.30 | 0.02 | [−0.46, 0.02] | −0.02 | 0.81 | [−0.18, 0.06] | −0.50 | <0.01 | [−0.74, −0.16] |
| Global Self-Worth | 5.15 | 0.26 | [2.48,14.84] | −2.09 | 0.05 | [−3.23, 0.78] | 2.39 | 0.11 | [0.81, 7.12] |
| Loss of Control Eating | −1.62 | 0.74 | [−9.79, 6.23] | −0.01 | 0.99 | [−4.21, 6.66] | −6.27 | 0.04 | [−10.26, 0.76] |
| Total Victimization | −2.20 | 0.63 | [−10.46, 8.89] | −4.53 | 0.23 | [−9.23, 4.28] | 2.15 | 0.42 | [−3.30, 5.42] |
| Happiness with Social Support | 0.42 | 0.72 | [−1.13, 2.42] | 0.19 | 0.86 | [−2.15, 1.31] | −0.15 | 0.81 | [−0.91, 1.50] |
Note: WRQOL=weight-related quality of life; HRQOL=health-related quality of life
As measured by the Impact of Weight on Quality of Life-Kids (IWQOL-Kids) Total score, with higher scores representing better functioning.
As measured by the 36-Item Short Form Survey (SF-36) physical component summary score, with higher scores representing better functioning.
As measured by the SF-36 mental component summary score, with higher scores representing better functioning
Separate regression models were run for each weight-based variable with sex, ethnicity, age, and the baseline corresponding quality of life measure controlled.
Unstandardized betas, two-tailed p-values and 95% confidence intervals for betas presented from each regression model.
For these analyses, % weight loss was computed as ((weightpre-surgery - weight24-months) /weightpre-surgery)*100
All analyses controlled for the corresponding measure of quality of life at baseline.
Higher pre-surgical BMI was predictive of significantly higher Mental HRQOL at 24 months. Post-hoc analyses to understand this unexpected finding indicate that adolescents with Class III obesity status at 24 months may be a unique sub-sample (see Figure 2C.2). At baseline, they had significantly higher BMI (M=59.01±9.54) relative to the remaining (≤Class II at 24 months) surgical group (M=49.10±6.37, p<0.001) and comparators (M=46.29±5.20, p<0.001), and by 24 months, their BMI (M=48.21±6.67) was not significantly different from comparators (M =48.65±8.37, p=0.80) but higher than the remaining surgical group (M=32.02±4.23, p<0.001). However, they report higher Mental HRQOL at pre-surgery (M=55.28±7.31) and 24 months (M=52.51±8.25) relative to comparators (pbaseline<0.001, p24-months=0.001) and the remaining surgical group (Mbaseline=48.29±10.00, p=0.001; M24-months=49.13±11.31, p=0.08).
Aim 3: Psychosocial correlates of WRQOL and HRQOL outcomes at 24 months
Psychosocial predictors and correlates of Total WRQOL, Physical HRQOL, and Mental HRQOL at 24 months for the surgical group were examined in separate regression models (Table 3). Beyond the corresponding baseline QOL measures, being female was significantly associated with lower WRQOL and Mental HRQOL in both predictive and concurrent models, while White ethnicity was significantly associated with lower Mental HRQOL in the predictive model. There were no other significant pre-operative predictors across QOL outcomes. In the concurrent models, greater internalizing symptoms were associated with lower Total WRQOL, while greater internalizing symptoms and post-operative LOC eating were significantly associated with lower Mental HRQOL. No significant correlates were identified for Physical HRQOL.
Discussion
As bariatric surgery gains acceptance in the treatment of adolescents with severe obesity, and new procedures emerge, it becomes increasingly important to understand its impact from the adolescent patient perspective through measures such as QOL. The current study examined outcomes and potential explanatory factors of QOL using a variety of constructs (i.e., multiple domains of WRQOL/HRQOL) and measurement tools (IWQOL-KIDS, SF-36) in adolescents at 24 months post-surgery relative to comparators with severe obesity not undergoing surgery.
As a condition-specific QOL measure, the IWQOL-Kids was designed to be sensitive to degree of excess weight or change in weight as evidenced by its strong psychometric properties (33, 34). Thus, as hypothesized and consistent with extant literature, the surgical group (who lost weight and were of lower BMI) reported significantly higher 24-month WRQOL than comparators (who did not lose weight and were of higher BMI) across most domains. Longitudinal examination of WRQOL was also consistent with the literature (8, 10), with the greatest change, both via statistical testing and clinically meaningful change metrics, occurring in the first 6-months post-operatively, with little change for comparators. However, noteworthy heterogeneity was observed within the surgical group based on 24-month weight status (i.e., remaining obese vs. achieving overweight or healthy weight) that is not adequately captured when focusing only on overall group means (Figure 2A.2 vs 2A.1). Accordingly, examination of risk and protective factors is informative. Predictors of poorer WRQOL outcomes that were not weight-based (e.g., weight loss) included being female, pre-surgical WRQOL, and/or self-reporting internalizing symptomatology at 24-months. WRQOL outcomes were unrelated to a range of psychosocial factors, including family dysfunction, LOC eating, self-worth, peer victimization, or social support.
Physical HRQOL (SF-36) focuses on an individual’s perception of overall functional ability, physically fulfilling roles, pain, and general health status. The surgical group reported significantly greater improvement in Physical HRQOL over time relative to comparators, with higher 24-month scores across physical subdomains. Interestingly, these findings demonstrate a marked improvement in the adolescent’s perception of physical well-being following surgery, even as the majority remained obese (Class I:30.3%; Class II:19.7%) or severely obese (Class III: 24.6%) at 24 months. In fact, among weight-based correlates, only percent weight loss (as opposed to BMI endpoint) was significantly associated with Physical HRQOL, with adolescents who experienced the greatest weight loss perceiving the highest Physical HRQOL. This may be due to greater resolution of physical comorbidities (e.g., joint pain reduction with weight loss) resulting in improved perception of physical health. Recent Teen-LABS studies have linked WRQOL and medical comorbidities pre-surgically. For instance, Bout-Tabuku and colleagues (48) reported that pre-surgically, adolescents who perceived greater lower extremity pain had poorer Total WRQOL and Physical Comfort than those who did not. Understanding the role of changes in physical health and comorbidities post-surgically on QOL in this population is imperative to their management. In contrast, no psychosocial variables were significantly associated with Physical HRQOL outcomes beyond pre-surgical levels. While it has been speculated that after the first year post-operatively, psychosocial factors should account for more variance in HRQOL (23), the current results indicate that for adolescent patients at 24 months, weight-based variables seem to be the primary drivers of Physical HRQOL and WRQOL.
No significant differences between surgical and comparator groups were identified for Mental HRQOL, and Mental Health and Role-Emotional subscales (i.e., inability to fulfill work/daily activities due to emotional problems). Further, no significant change over time for either group was identified for Mental HRQOL, similar to previous findings (11, 15, 16, 23). This lack of change is also consistent with other psychosocial findings from the TeenView cohort. We found most adolescents undergoing surgery maintained their psychological status from baseline to 24 months in the context of weight loss, with the majority reporting a healthy (i.e., non-symptomatic) status at both times, while a minority (25.4%) exhibited persistent impairment.(17) In contrast, adolescents in AMOS experienced improvement in mean levels of general mental health (e.g., anxiety, self-concept) over 2 years post-surgery, although percent weight loss was not significantly associated with this improvement.(49) Taken together, these findings as well as the lack of significant weight-based correlates of Mental HRQOL, suggest weight has little impact on the Mental HRQOL of adolescents post-operatively. Instead, greater post-operative, but not pre-operative, internalizing symptoms and LOC eating were associated with greater Mental HRQOL impairment at 24 months. Interestingly, post-surgical LOC eating has been shown to be predictive of lower percent change in BMI at 1-, 2-, and 3-years post-surgery(19), yet in the current study, was unrelated concurrently to WRQOL and Physical HRQOL. Future research should address the complex long-term associations among these variables.
It is noteworthy that the present longitudinal analyses indicated a significantly higher Mental HRQOL for the surgical group since pre-surgery/baseline relative to comparators. The American Society for Metabolic and Bariatric Surgery guidelines have continued to recommend that, with few exceptions, mental health symptoms are not a contraindication for bariatric surgery in adolescents when managed through adjunctive care.(50) However, as we have suggested, (30, 51) in contrast to presenting for first-line behavioral weight treatment, the demands of achieving surgical candidacy, including navigating a complex process with multiple decision-makers (i.e., adolescents/caregivers, referring physicians, clinical team, insurance) may result in adolescents with greater psychosocial impairment (i.e., lower Mental HRQOL) being less likely to pursue or be referred for surgery, dropping out of the intensive bariatric care pathway pre-operatively, as well as being deferred or denied surgery (52).
Finally, post-hoc analyses seem to suggest that the counter-intuitive finding, that higher pre-surgical BMI significantly predicted higher Mental HRQOL in the surgical group at 24 months, may be the result of a subgroup (i.e., adolescents with Class III obesity at 24 months). These adolescents had a post-surgical weight similar to the comparators at 24 months, and thus, might arguably be most negatively affected by their weight, yet report higher Mental HRQOL at pre-surgery and 24 months relative to comparators and the remaining surgical group. These findings may be suggestive of psychosocial hardiness for this subgroup of patients who may have continued physical challenges due to weight. Alternately, higher Mental HRQOL scores may indicate a repressive adaptation style (53) in which youth faced with the stressors of a serious chronic condition minimize affective distress. In a recent study of adults who were overweight/obese and in behavioral weight management, repressive copers reported higher Mental HRQOL but not Physical HRQOL compared with non-repressors, although groups did not differ in BMI.(54) This is an area for future research.
Strengths of the present study include the multi-site and controlled design prospectively following adolescents over time as well as the inclusion of participants with differing surgical procedures. Moreover, a multi-dimensional approach to understanding QOL and its associations with a diverse set of predictors/correlates was taken using measures with well-established psychometrics validated for adolescents. Limitations included a primarily female and White bariatric sample, limiting generalizability for males and other racial/ethnic groups at risk for severe obesity (55). In addition, future research should assess QOL at later post-surgical times when weight regain and changing comorbidity status might become significant for some. For instance, Ryder and colleagues reported QOL outcomes for young adults who had RYGB approximately 8 years earlier as adolescents(14). Those classified as re-gainers had significantly lower total WRQOL as well as in domains of physical function, self-esteem, sexual life, public distress and work than weight loss maintainers. Moreover, potential bi-directionality between QOL and weight should be assessed to determine if patients who “feel better” are more likely to engage in weight loss maintenance behaviors. Given the number of analyses completed, results need to be both replicated in future research as well as used to guide more mechanistic model testing with a larger sample to explore complex interrelationships in understanding QOL outcomes.
Clinical Implications
The inclusion of patient reported outcomes such as QOL are vital to fully understand the “success” of bariatric surgery, with promotion of QOL identified as a primary goal of Healthy People 2020.(56) However, QOL constructs should not be considered equivalent to psychosocial or medical (e.g., comorbidities, laboratory tests) measures. WRQOL proves uniquely sensitive to the effects of weight change on daily functioning, while Physical HRQOL provides a patient-focused perception of physical health distinct from objective medical measures. In contrast, Mental HRQOL appears comparable with many other psychosocial outcome measures, with findings suggesting that like those other measures, there should be a tempering of expectations about potential for improvement following bariatric surgery as well as a clear plan for providing psychosocial post-operative assessment and care.
Supplementary Material
Acknowledgements:
The authors would like to acknowledge the contributions of additional TeenView and Teen-LABS Study Group Co-Investigators and staff. Cincinnati Children’s Hospital Medical Center: Faye Doland, BS, Ashley Morgenthal, BS, Taylor Howarth, BS, Sara Comstock, MA, April Carr, BS, Lindsey Shaw, MS, Cynthia Spikes, CRC, Shelley Kirk, PhD, Michael Helmrath, MD, PhD, Jane Khoury, PhD; Texas Children’s Hospital, Baylor Medical Center: Margaret Callie Lee, MPH, David Allen, BS, Gia Washington, PhD, Beth Garland, PhD, Mary L. Brandt, MD; University of Pittsburgh Medical Center: Ronette Blake, BS, Nermeen El Nokali, PhD, Silva Arslanian, MD, Anita P. Courcoulas, MD, MPH, Children’s Hospital of Alabama University of Alabama: Krishna Desai, MD, Amy Seay, PhD, Beverly Haynes, BSN, Carroll Harmon, MD, PhD; Nationwide Children’s Hospital Medical Center: Melissa Ginn, BS, Karen Carter, CCRC, Kevin Smith, PhD, Amy E. Baughcum, PhD, Marc P. Michalsky, MD; Teen-LABS Data Coordinating Center: Michelle Starkey Christian, Jennifer Andringa, BS, Carolyn Powers, RD, Rachel Akers, MPH, Tara Schafer-Kalkhoff, MA, CCRP, Jennifer Black, MSSA, LSW, Rosie Miller, RN, CCRC.
Funding Source: TeenView (R01DK080020; PI: Zeller) was conducted in collaboration with the Teen-LABS Consortium. Teen-LABS was funded by cooperative agreements with the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), through grants: U01DK072493, UM1DK072493, and UM1DK095710 (University of Cincinnati). Dr. Ley and Dr. Kidwell’s effort was supported by an NIH post-doctoral training grant (T32 DK063929).
Footnotes
Competing Interest Statement: Thomas H. Inge has served as a consultant for Zafgen Corporation, Biomedical Insights, and L&E Research, and received honoraria from Standard Bariatrics, UpToDate, and Independent Medical Expert Consulting Services, all unrelated to this project. All other authors declare no potential competing interests.
References
- 1.Yanovski SZ, Yanovski JA. Toward Precision Approaches for the Prevention and Treatment of Obesity. JAMA. 2018;319(3):223–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sloan JA, Halyard MY, Frost MH, Dueck AC, Teschendorf B, Rothman ML, et al. The Mayo Clinic manuscript series relative to the discussion, dissemination, and operationalization of the Food and Drug Administration guidance on patient-reported outcomes. Value Health. 2007;10 Suppl 2:S59–63. [DOI] [PubMed] [Google Scholar]
- 3.Calvert M, Brundage M, Jacobsen PB, Schunemann HJ, Efficace F. The CONSORT Patient-Reported Outcome (PRO) extension: implications for clinical trials and practice. Health Qual Life Outcomes. 2013;11:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Modi AC, Loux TJ, Bell SK, Harmon CM, Inge TH, Zeller MH. Weight-specific health-related quality of life in adolescents with extreme obesity. Obesity (Silver Spring). 2008;16(10):2266–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeller MH, Inge TH, Modi AC, Jenkins TM, Michalsky MP, Helmrath M, et al. Severe obesity and comorbid condition impact on the weight-related quality of life of the adolescent patient. J Pediatr. 2015;166(3):651–9.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paulus GF, de Vaan LE, Verdam FJ, Bouvy ND, Ambergen TA, van Heurn LW. Bariatric surgery in morbidly obese adolescents: a systematic review and meta-analysis. Obes Surg. 2015;25(5):860–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.White B, Doyle J, Colville S, Nicholls D, Viner RM, Christie D. Systematic review of psychological and social outcomes of adolescents undergoing bariatric surgery, and predictors of success. Clin Obes. 2015;5(6):312–24. [DOI] [PubMed] [Google Scholar]
- 8.Zeller MH, Modi AC, Noll JG, Long JD, Inge TH. Psychosocial functioning improves following adolescent bariatric surgery. Obesity (Silver Spring). 2009;17(5):985–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sysko R, Devlin MJ, Hildebrandt TB, Brewer SK, Zitsman JL, Walsh BT. Psychological outcomes and predictors of initial weight loss outcomes among severely obese adolescents receiving laparoscopic adjustable gastric banding. J Clin Psychiatry. 2012;73(10):1351–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zeller MH, Reiter-Purtill J, Ratcliff MB, Inge TH, Noll JG. Two-year trends in psychosocial functioning after adolescent Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2011;7(6):727–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olbers T, Gronowitz E, Werling M, Marlid S, Flodmark CE, Peltonen M, et al. Two-year outcome of laparoscopic Roux-en-Y gastric bypass in adolescents with severe obesity: results from a Swedish Nationwide Study (AMOS). Int J Obes (Lond). 2012;36(11):1388–95. [DOI] [PubMed] [Google Scholar]
- 12.Inge TH, Courcoulas AP, Jenkins TM, Michalsky MP, Helmrath MA, Brandt ML, et al. Weight Loss and Health Status 3 Years after Bariatric Surgery in Adolescents. N Engl J Med. 2016;374(2):113–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olbers T, Beamish AJ, Gronowitz E, Flodmark CE, Dahlgren J, Bruze G, et al. Laparoscopic Roux-en-Y gastric bypass in adolescents with severe obesity (AMOS): a prospective, 5-year, Swedish nationwide study. Lancet Diabetes Endocrinol. 2017;5(3):174–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ryder JR, Gross AC, Fox CK, Kaizer AM, Rudser KD, Jenkins TM, et al. Factors associated with long-term weight-loss maintenance following bariatric surgery in adolescents with severe obesity. Int J Obes (Lond). 2018;42(1):102–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lindekilde N, Gladstone BP, Lubeck M, Nielsen J, Clausen L, Vach W, et al. The impact of bariatric surgery on quality of life: a systematic review and meta-analysis. Obes Rev. 2015;16(8):639–51. [DOI] [PubMed] [Google Scholar]
- 16.Hachem A, Brennan L. Quality of Life Outcomes of Bariatric Surgery: A Systematic Review. Obes Surg. 2016;26(2):395–409. [DOI] [PubMed] [Google Scholar]
- 17.Hunsaker SL, Garland BH, Rofey D, Reiter-Purtill J, Mitchell J, Courcoulas A, et al. A Multisite 2-Year Follow Up of Psychopathology Prevalence, Predictors, and Correlates Among Adolescents Who Did or Did Not Undergo Weight Loss Surgery. J Adolesc Health. 2018;63(2):142–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jarvholm K, Karlsson J, Olbers T, Peltonen M, Marcus C, Dahlgren J, et al. Characteristics of adolescents with poor mental health after bariatric surgery. Surg Obes Relat Dis. 2016;12(4):882–90. [DOI] [PubMed] [Google Scholar]
- 19.Goldschmidt AB, Khoury J, Jenkins TM, Bond DS, Thomas JG, Utzinger LM, et al. Adolescent Loss-of-Control Eating and Weight Loss Maintenance After Bariatric Surgery. Pediatrics. 2018;141(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zeller MH, Washington GA, Mitchell JE, Sarwer DB, Reiter-Purtill J, Jenkins TM, et al. Alcohol use risk in adolescents 2 years after bariatric surgery. Surg Obes Relat Dis. 2017;13(1):85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ratcliff MB, Eshleman KE, Reiter-Purtill J, Zeller MH. Prospective changes in body image dissatisfaction among adolescent bariatric patients: the importance of body size estimation. Surg Obes Relat Dis. 2012;8(4):470–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Utzinger LM, Gowey MA, Zeller M, Jenkins TM, Engel SG, Rofey DL, et al. Loss of control eating and eating disorders in adolescents before bariatric surgery. Int J Eat Disord. 2016;49(10):947–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wimmelmann CL, Dela F, Mortensen EL. Psychological predictors of mental health and health-related quality of life after bariatric surgery: a review of the recent research. Obes Res Clin Pract. 2014;8(4):e314–24. [DOI] [PubMed] [Google Scholar]
- 24.Brunault P, Frammery J, Couet C, Delbachian I, Bourbao-Tournois C, Objois M, et al. Predictors of changes in physical, psychosocial, sexual quality of life, and comfort with food after obesity surgery: a 12-month follow-up study. Qual Life Res. 2015;24(2):493–501. [DOI] [PubMed] [Google Scholar]
- 25.Janicke DM, Marciel KK, Ingerski LM, Novoa W, Lowry KW, Sallinen BJ, et al. Impact of psychosocial factors on quality of life in overweight youth. Obesity (Silver Spring). 2007;15(7):1799–807. [DOI] [PubMed] [Google Scholar]
- 26.Zeller MH, Modi AC. Predictors of health-related quality of life in obese youth. Obesity (Silver Spring). 2006;14(1):122–30. [DOI] [PubMed] [Google Scholar]
- 27.Jensen CD, Steele RG. Longitudinal associations between teasing and health-related quality of life among treatment-seeking overweight and obese youth. Journal of pediatric psychology. 2012;37(4):438–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Inge TH, Zeller M, Harmon C, Helmrath M, Bean J, Modi A, et al. Teen-Longitudinal Assessment of Bariatric Surgery: methodological features of the first prospective multicenter study of adolescent bariatric surgery. Journal of pediatric surgery. 2007;42(11):1969–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Michalsky MP, Inge TH, Teich S, Eneli I, Miller R, Brandt ML, et al. Adolescent bariatric surgery program characteristics: the Teen Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study experience. Seminars in pediatric surgery. 2014;23(1):5–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rofey DL, Zeller MH, Brode C, Reiter-Purtill J, Mikhail C, Washington G, et al. A multisite view of psychosocial risks in patients presenting for bariatric surgery. Obesity (Silver Spring). 2015;23(6):1218–25. [DOI] [PubMed] [Google Scholar]
- 31.Zeller MH, Hunsaker S, Mikhail C, Reiter-Purtill J, McCullough MB, Garland B, et al. Family factors that characterize adolescents with severe obesity and their role in weight loss surgery outcomes. Obesity (Silver Spring). 2016;24(12):2562–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeller MH, Noll JG, Sarwer DB, Reiter-Purtill J, Rofey DL, Baughcum AE, et al. Child Maltreatment and the Adolescent Patient With Severe Obesity: Implications for Clinical Care. Journal of pediatric psychology. 2015;40(7):640–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kolotkin RL, Zeller M, Modi AC, Samsa GP, Quinlan NP, Yanovski JA, et al. Assessing weight-related quality of life in adolescents. Obesity (Silver Spring). 2006;14(3):448–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Modi AC, Zeller MH. The IWQOL-Kids((c)): establishing minimal clinically important difference scores and test-retest reliability. Int J Pediatr Obes. 2011;6(2–2):e94–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 36.Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ (Clinical research ed). 1992;305(6846):160–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McHorney CA, Ware JE Jr., Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical care. 1993;31(3):247–63. [DOI] [PubMed] [Google Scholar]
- 38.Kolotkin RL, Davidson LE, Crosby RD, Hunt SC, Adams TD. Six-year changes in health-related quality of life in gastric bypass patients versus obese comparison groups. Surg Obes Relat Dis. 2012;8(5):625–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bogat GA, Chin R, Sabbath W, & Schwartz C The children’s social support questionnaire (technical report #3). East Lansing: Michigan State University; 1985. [Google Scholar]
- 40.Epstein NB, Baldwin LM, Bishop DS. THE McMASTER FAMILY ASSESSMENT DEVICE*. Journal of Marital and Family Therapy. 1983;9(2):171–80. [Google Scholar]
- 41.Spitzer RL, Yanovski SZ, & Marcus MD The Questionnaire of Eating and Weight Patterns-Revised (QEWP-R, 1993). 722 West 168th Street New York, NY 10032: New York State Psychiatric Intistute; 1993. [Google Scholar]
- 42.Prinstein MJ, Boergers J, Vernberg EM. Overt and relational aggression in adolescents: social-psychological adjustment of aggressors and victims. J Clin Child Psychol. 2001;30(4):479–91. [DOI] [PubMed] [Google Scholar]
- 43.De Los Reyes A, Prinstein MJ. Applying depression-distortion hypotheses to the assessment of peer victimization in adolescents. J Clin Child Adolesc Psychol. 2004;33(2):325–35. [DOI] [PubMed] [Google Scholar]
- 44.Harter S Self-Perception Profile for Adolescents: Manual and Questionnaires. Denver, CO: University of Denver, Department of Psychology; 2012. [Google Scholar]
- 45.Achenbach TM, & Rescorla LA Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth & Families; 2001. [Google Scholar]
- 46.Song LY, Singh J, & Singer M The Youth Self-Report inventory: A study of its measurement fidelity. Psychological Assessment. 1994;6(3):326–45. [Google Scholar]
- 47.Pinquart M, Shen Y. Behavior problems in children and adolescents with chronic physical illness: a meta-analysis. Journal of pediatric psychology. 2011;36(9):1003–16. [DOI] [PubMed] [Google Scholar]
- 48.Bout-Tabaku S, Michalsky MP, Jenkins TM, Baughcum A, Zeller MH, Brandt ML, et al. Musculoskeletal Pain, Self-reported Physical Function, and Quality of Life in the Teen-Longitudinal Assessment of Bariatric Surgery (Teen-LABS) Cohort. JAMA pediatrics. 2015;169(6):552–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jarvholm K, Karlsson J, Olbers T, Peltonen M, Marcus C, Dahlgren J, et al. Two-year trends in psychological outcomes after gastric bypass in adolescents with severe obesity. Obesity (Silver Spring). 2015;23(10):1966–72. [DOI] [PubMed] [Google Scholar]
- 50.Pratt JSA, Browne A, Browne NT, Bruzoni M, Cohen M, Desai A, et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis. 2018;14(7):882–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Reiter-Purtill J, Gowey MA, Austin H, Smith KC, Rofey DL, Jenkins TM, et al. Peer Victimization in Adolescents With Severe Obesity: The Roles of Self-Worth and Social Support in Associations With Psychosocial Adjustment. Journal of pediatric psychology. 2017;42(3):272–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cohen MJ, Curran JL, Phan TT, Reichard K, Datto GA. Psychological contributors to noncompletion of an adolescent preoperative bariatric surgery program. Surg Obes Relat Dis. 2017;13(1):58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Phipps S, Steele RG, Hall K, Leigh L. Repressive adaptation in children with cancer: a replication and extension. Health Psychol. 2001;20(6):445–51. [PubMed] [Google Scholar]
- 54.Truong EAK, Olson KL, Emery CF. Repressive coping, stigmatization, psychological distress, and quality of life among behavioral weight management participants. Eat Behav. 2016;22:206–10. [DOI] [PubMed] [Google Scholar]
- 55.Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, Steinberger J, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128(15):1689–712. [DOI] [PubMed] [Google Scholar]
- 56.U.S. Department of Health and Human Services. CitationArticleTitle. The Vision, Mission, and Goals of Healthy People 2020. Overarching Goals [Available from: https://www.healthypeople.gov/sites/default/files/HP2020Framework.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.