Abstract
Background: Assisted reproductive technology (ART) is the routine treatment for infertility. The success rate for individual sessions is generally not high, and many patients need to undergo several cycles. To increase their chances of success, many patients turn to acupuncture to complement ART. Many clinical trials of acupuncture helping in vitro fertilization (IVF) have focused only on IVF–embryo transfer (ET). In some difficult cases, when even IVF cannot be offered, acupuncture and Chinese herbs can improve the patients' conditions to reach a level at which ART can be successful.
Cases: Six cases showed how acupuncture and Traditional Chinese Medicine (TCM), using Chinese herbs, can make IVF possible in difficult cases and how they can also help prevent miscarriage afterward. The cases included patients with amenorrhea, sperm disorders, polycystic ovary syndrome, diminished ovarian reserve (DOR), tubal blockage, premenopause, and premature ovarian insufficiency.
Results: Acupuncture and Chinese herbs worked together to help make ART possible or easier. The ART used for these patients included intrauterine insemination, IVF, IVF with a donor egg, and introcytoplasmic sperm injection. In 3 cases, IVF was not initially successful but was successful after TCM treatment.
Conclusions: These 6 cases demonstrated the positive effect of a combined approach, using acupuncture and herbs to reduce DOR and regulate hormonal disorders, creating sustainable environments for conceiving and maintaining pregnancy, thus, translating into clinical success. Clinical observation of these cases sheds new light on designing future clinical trials and practice of TCM for practitioners who provide infertility treatments.
Keywords: infertility, acupuncture, Chinese herb, ART, IVF, case study
Introduction
Assisted reproductive technology (ART) refers to a range of medical procedures broadly used to treat infertility.1 Some forms of ART are well-developed while others are constantly developing; all are considered the most useful tools for treating infertility worldwide. Among them, the most well-known ART is in vitro fertilization (IVF).2 ART has made revolutionary progress. However, the outcomes have not been very successful, with best performance in 2016 in the United Kingdom at 22% as measured by birth rates per embryo transfers (ETs).3 Many nonconventional methods have been introduced and tested to help improve clinical outcomes, particularly of IVF. Acupuncture is widely reported to be used together with IVF. Most up-to-date reports recommend the use of acupuncture before and after IVF-ET, as there is evidence that acupuncture improves the outcome of IVF-ET.4,5
A clinical trial published in 20186 focused on the effect of acupuncture for promoting ovarian development. Acupuncture treatment was applied during the ovarian-stimulating stage of IVF or introcytoplasmic sperm injection (ICSI cycle). The acupuncture improved ovarian blood flow. This, in turn, improved the quality of the female body and the eggs produced, resulting in a higher clinical pregnancy rate. The rate was 52.6% (in a verum acupuncture group) versus 33.3% (in a sham acupuncture group) and 32.8% (in an observational group). This report has echoed the experience of many practitioners who have used acupuncture in the ovarian-stimulating phase.
While acupuncture assisting IVF has been widely used and researched, Chinese herbal medicine (CHM) has been less-noticed in the same area. Initially, clinical trials testing successful pregnancy rates over the whole course of treatment have shown no real differences between groups receiving herbs (58%) and control groups (54%). However, it has been reported that CHM can increase endometrial thickness significantly, which is considered to favor conception.7
CHM is broadly used for treating infertility, and clinical trials have been mostly positive, without ART or IVF. According to Ried,8 40 randomized controlled trials (RCTs) involving 4247 women with infertility who were treated with CHM were reported in 2015; CHM improved pregnancy rates significantly, compared to drug therapy, boosting pregnancy rates from 30% to 60% over 3–6 months. Another systematic review had a similar result with a series of clinical trials that included a total 44,619 participants (of whom 6344 participants received acupuncture treatment) in 210 primary studies in 2018 on acupuncture-assisted IVF.9 However, the reported cases did not indicate if the inclusion criteria allowed conditions specifically requiring IVF, such as tubal blockage.
According to the current authors' clinical experience, Traditional Chinese Medicine (TCM) supports IVF best when the 2 approaches are combined in a whole-system approach. The majority of cases who have been treated with combined acupuncture and CHM have had more success than cases in whom only herbs or acupuncture were used separately. This opinion is broadly considered to reflect current practice, and Hullender Rubin et al.10 also gathered evidence for the whole-system practice of TCM assisting IVF.
Since 2003, to date, many clinical trials and systematic reviews have investigated the clinical effect of acupuncture-assisted IVF. Most reviews have revealed positive effects11–14; however, a few of studies were negative and suggested no benefit of this approach.15–17 In addition to these conflicting reports, a systematic review suggested that acupuncture might be beneficial for some clinical conditions.18
The current authors believe that these clinical trials were not designed to reflect the TCM view of fertility management, and therefore, the effects were limited. In most of the clinical trials, acupuncture was only administrated twice: once before ET and once immediately after ET. The patients were not prepared for ART by improving their fundamental conditions, which is the underlying role of TCM. After a birth, the advice is always to avoid another pregnancy for 18 months to let the body recover fully. This is the recommendation even for couples who have never experienced fertility difficulties, and is general principle, cited in a 2018 study by Schummers et al.19 and accepted by the UK's National Health Service (NHS), as advice for all couples.20 It is also important to ensure proper care during early pregnancy to prevent miscarriage. Current research oversimplifies the necessary interventions, and therefore does not reflect the focus of TCM.
The following cases are presented to demonstrate that the combined holistic approach of TCM should be considered instead of solely using acupuncture treatment. In many difficult cases, combined TCM has overcome many complicated problems and achieved good clinical outcomes.
Cases
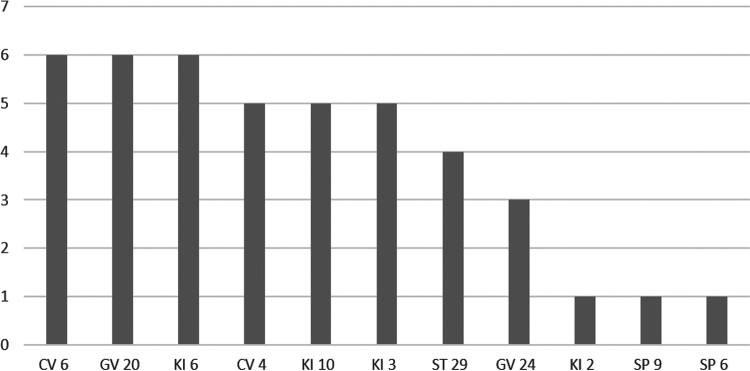
The 6 interesting cases presented here were all difficult cases in which the patients were informed either that ART was not recommended or that chances of its success were low. Yet, ultimately, using the combined TCM approach, they all achieved live births. Sharing the experiences of these difficult cases might provide some useful clues for further study. Key information about each case (Table 1), a summary of acupuncture points prescribed (Table 2), and the frequency of acupuncture points used (Fig. 1) are extracted from the cases for quick reference in 2 tables and 1 figure.
Table 1.
General Information on the 6 Cases
| Case # | Gender (age) | Clinical findings | ART offered initially | ART after TCM Tx | Tx type acupuncture/herbs | Length of Tx course | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | Female (29) | Infertility | IVF | IUI | Acupuncture & herbal pills | 3 months | Live birth of a boy |
| 2 | Female (34) | PCOS | IVF with ICSI | ICSI | Acupuncture & herbal powder | 5 months | Live birth of a boy |
| Male (37) | Sperm disorder | Herbal pills | |||||
| 3 | Female (36) | DOR | Refused | IVF | Acupuncture & herbal decoction | 12 months | Live birth of a girl |
| 4 | Female (49) | Blocked fallopian tube & premenopause | Refused after 2 failed IVF cycles | IVF | Acupuncture & herbal pills | 6 months | Live birth of a boy |
| 5 | Female (27) | Blocked fallopian tubes | 3 failed IVF cycles | IVF | Acupuncture & herbal powders | 24 months | Live birth a triplets (1 boy & 2 girls) |
| Male (35) | Sperm disorder | Herbal pills | |||||
| 6 | Female (41) | POI & miscarriage | Refused | IVF with donor egg | Acupuncture & herbal decoction | 3 months | Live birth of a boy and a girl in 2 years; followed by a fertilized embryo transferred again |
ART, assisted reproductive technology; TCM, Traditional Chinese Medicine; Tx, treatment; PCOS, polycystic ovary syndrome; DOR, diminished ovarian reserve; POI, primary ovarian insufficiency; IVF, in vitro fertilization; ICSI, introcytoplasmic sperm injection.
Table 2.
Acupuncture Points Prescribed for the Females in the 6 Cases
| Case #s & names | |
Main Acupoints |
|
||
|---|---|---|---|---|---|
| Moxi | Abdominal | Head | Limbs | Associated points | |
| 1 Ms. L.S. | CV 8 | CV 4, CV 6, ST 29 | GV 20, GV 24 | KI 10, KI 6, KI 3 | TE 5, GB 41, HT 7, SP 9, SP 6 |
| 2 Ms. H.F. | CV 8 | CV, ST 29 | GV 20, GV 24 | SP 9, SP 6 | TE 5, GB 41, ST 36 |
| 3 Ms. M.C. | CV 8 | CV 4, CV 6, Ext | GV 20, ST 8,aTaiyang | KI 10, KI 6, KI 3 | SP9, 6 TE5, GB41 |
| 4 Ms. M.S. | CV 8 | CV 4, CV 6, ST 29 | GV 20, GV 24, | KI 10, KI 3, KI 2, KI 6 | LR 4, LR 3, ST 36, SP 6 |
| 5 Ms. T.F. | CV 8 | CV 4, CV 6, Ext | GV 20 | KI 10, KI 3, KI 6 | TE 5, GB 41, ST 36, LR 4, LR 3 |
| 6 Ms. D.C. | CV 8 | CV 4, CV 6, ST 29 | GV 20 | KI 10, KI 3, KI 6 | TE 5, GB 41, SP 9, SP 6 |
ST 8 is situated in the reproductive area in the scarp acupuncture.
Moxi, moxibustion.
FIG. 1.
Frequency of the main acupoints used in the 6 cases.
Case 1
Ms. L.S., a 29-year-old receptionist presented with infertility of 2 years' duration. Her first visit was in June of 2010. She had been taking contraceptive pills since she was 15 years' old, for 12 years, and had stopped 2 years after she had gotten married. Her menstruation did not resume immediately after stopping this contraception. After 6 months, this patient commenced regular menstrual cycles of 4–5 days every 28–32 days. Worrying about her inability to become pregnant, she visited a local private infertility clinic (in Sheffield, UK) for help. Her hormonal tests and her husband's sperm examination results were found to be normal. Even so, the couple decided on IVF. based on advice from the clinic.
She visited one of the current authors (D.J.)'s clinic seeking help for her stress and insomnia, as she wanted to have a good result with her IVF treatment. She sought this treatment, based on the experience that a friend's had with receiving TCM before IVF, which reduced her anxiety and was considered to contribute to a successful pregnancy.
Clinical manifestations in TCM terms
The patient had stress, nervousness, restlessness, poor sleep, tiredness, and minor menstrual pain. She had a bright-red tongue with less coating, as well as a wiry and fine pulse.
TCM patterns
Liver Qi Stagnation with Blood Stasis as well as Kidney and Spleen Qi Deficiency.
Treatments
Moxibustion was given at CV 8 (Shenque). Acupuncture included use of the following groups of points:
GV 20 (Baihui), GV 24 (Shenting); CV 4 (Guanyuan), CV 6 (Qihai), and Ext (Zigong)
TE 5 (Waiguan), GB 41 (Zulinqi), HT 7 (Shenmen), and SP 9 (Yinlingquan)
SP 6 (Sanyinjiao), KI 3 (Taixi), KI 6 (Zhaohai), and KI 10 (Rangu).
The herbal preparations this patient was given were:
Jiaweixiaoyao Wan—Radix Bupleuri, Anglica Sinensis (Oliv.) Dies, Paeonia Lactiflora Pall, Atractylodes Macrocephala Koidz, Sclerotium Poriae Cocos, Cortex Moutan Radicis, Fructus Gardeniae Jasminoidis, Mentha Haplocalyx Brq., and Glycyrrhizae Uralensis Fisch
Renshenguipi Wan—Radix Ginseng, Rhizoma Atractylodis Macrocephalae, Radix Astragali, Poria, Radix Polygalae, Semen Ziziphi Spinosae, Arillus Longan, Radix Angelicae Sinensis, Fructus Zizyphi Jujubae, and Radix Glycyrrhizae.
Continuing treatment
The above acupuncture plan was given once per week. The herbal medicine was given in 15 pills each, twice daily. After this patient received 3 months of TCM treatment with the above regimen, her menstruation was maintained smoothly without pain. She subsequently visited a NHS gynecologic consultant, where she was advised to undergo intrauterine insemination (IUI) based on an evaluation of her overall situation.
Outcome
The patient conceived and carried a baby boy to full term.
Analysis
IUI is a simple form of ART. Due to a long period of taking contraceptive pills, although the patient had recovered her menstrual cycles and had normal hormonal test results, her ovaries were not sensitive enough. Her TCM diagnosis was Kidney Deficiency and Excess Liver Qi Stagnation. She was still in a preclinical state, so she was unable to conceive easily. Acupuncture was the most suitable treatment for her current state, giving her the stimulation she needed to rehabilitate her ovarian function completely. She was prescribed patent herbs to strengthen the effect of her ART treatment. The gynecologic consultant also recognized her improved state and that her husband had a good sperm. Thus, she was given IUI only and had conceived successfully after only one attempt.
Case 2
Ms. H.F., a 34-year-old housewife, had infertility for 3 years' duration. Her first visit was in Nov of 2014. Her husband, Mr. E.F., an information technology technician, was 37 years' old. He accompanied her.
She had started menarche at the age of 16. Since then, her cycle had been irregular and often delayed. She had taken contraceptive pills until 3 years ago. After stopping the pills, she was unable to conceive for 2 years and had begun receiving IVF in June of 2013. During that procedure, 13 oocytes were retrieved, of which 9 were fertilized. On the first IVF attempt, 2 embryos were placed into her uterus but did not result in a pregnancy. Since then, she had only two vaginal discharges in 1 year. Hormone testing showed the following levels: luteinizing hormone (LH), 24; follicle-stimulating hormone (FSH), 9; and folate, 19.7. Her last menstruation had been 7 months prior.
During this first visit, she reported having stress, nervousness, and restlessness due to infertility.
Her husband was found to have sperm disorder (density: 0.10 million/mL, <25% of sperm motility).
The couple were waiting for another IVF attempt and decided to try acupuncture at D.J.'s clinic. During this first visit to the TCM clinic, the couple were advised to receive simultaneous treatment with acupuncture and herbal medicine. They accepted this treatment plan.
Wife's clinical manifestations in TCM terms
This patient had irregular menstrual circles: for 4–5 days of menstruation only two times since IVF last year and no period came for the prior 7 months. She also had nervousness, restlessness, tiredness, and stress, some acne on her chin and chest, and loose bowel movements. She had a pink plump tongue with teeth marks and a wiry-fine pulse.
Wife's TCM patterns
Damp-Phlegm accumulation with Blood Stasis as well as Spleen and Kidney Deficiencies.
Wife's treatment
Moxibustion was given at CV 8 (Shenque). Acupuncture included use of the following groups of points:
CV 4 (Guanyuan), CV 6 (Qihai), ST 29 (Guilai), and GV 20 (Baihui)
GV 24 (Shenting), SP 9 (Yinlingquan), SP 6 (Sanyinjiao), ST 36 (Zusanli), TE 5 (Waiguan), and GB 41 (Zulinqi).
The wife was given the following herbs:
Shudihuang (Radix Rhemanniae Glutinosae Praeparata) 15
Xianmao (Rhizoma Curculiginis Orchioidis) 10
Yinyanghuo (Herba Epimedii) 20
Danggui (Radix Angelicae Sinensis) 10
Banxia (Rhizoma Pinelliae Ternatae) 10
Cangzhu (Rhizoma Atractylodis) 10
Chuanxiong (Radix Ligustici Wallichii) 10
Chishao (Radix Paeoniae Rubrae) 10
Yimucao (Herba Leonuri Heterophylli) 10
Fuling (Sclerotium Poriae Cocos) 10
Xiangfu (Rhizoma Cyperi Rotundi) 10
Honghua (Flos Carthami Tinctorii) 10
Before ovulation, Zishiying (Fluoritum) 10, and Taoren (Semen Pruni Persicae) 10 were added
Before menstruation, Tusizi (Semen Cuscutae Chinensis) 10–30, Zelan (Herba Lycopi Lucidi) 10 were added.
For the wife, the above acupuncture plan was applied once per week and 6 g of the herbal medicine, in powder form, was given orally, twice daily.
Husband's clinical manifestations in TCM terms
The husband had stress, but was generally feeling good. He had a pink tongue and a wiry pulse.
Husband's TCM patterns
Liver Qi Stagnation and Kidney Qi Deficiency.
Husband's treatment
He was not given acupuncture, but was given the following herbal preparations:
Wuziyanzongwan—Semen Plantaginis, Fructus Lycii, Fructus Rubi, Semen Cuseutae; and Fructus Schisandrae)
Jiaweixiaoyaowan—Radix Bupleuri, Anglica Sinensis (Oliv.) Dies, Paeonia Lactiflora Pall, Atractylodes Macrocephala Koidz, Sclerotium Poriae Cocos, Cortex Moutan Radicis, Fructus Gardeniae Jasminoidis, Mentha Haplocalyx Brq., and Glycyrrhizae Uralensis Fisch.
These herbs were in patent forms: 15 pills of each, which were given twice daily.
Outcome
After regular TCM treatment for 5 months, Ms. H has her menses every month for 4–5 days every 28–30 days. When the couple subsequently visited their gynecologic consultant, the specialist was very pleased about the wife's general condition and relevant hormonal levels. (FSH, 4.10; LH, 3.80; estradiol, 107.00) The husband's sperm count also improved (density 20 million/mL, 50% of sperm motility). These laboratory tests suggested that they could accept ICSI.
The couple underwent ICSI, in which the best-quality sperm were selected in the laboratory and injected into the wife's egg and then the egg was transferred into her uterus. She conceived, progressed through a normal pregnancy, and carried a healthy baby boy to full term.
Analysis
ICSI is a form of ART that is suitable for men with sperm disorders. Both members of this couple had problems affecting their fertility, and had tried to conceive for 3 years without positive results. The wife was treated for her irregular menstruation, and a regular menstrual cycle was established after she underwent TCM treatment. Meanwhile, the husband's sperm improved with patent herbs. Although, in theory, they might have achieved pregnancy naturally, the process would have taken much longer. The ICSI technique gave them quick success after sufficient preparation with TCM.
Case 3
Ms. M.C., a 36-year-old clerk, had infertility for 4 years. Her first visit was in November of 2012. She had received contraceptive injections for 10 years; these injections were stopped 4 years ago. She had suffered from very irregular menstrual cycles since her adolescence. The cycles gradually become more regular with the abovementioned treatment. After stopping contraceptive treatment, she presented with short menstrual cycles with long bleeding days: (6–7 days every 21–23 days, with 2 days of menstrual pain). She had visited a private fertility clinic where her tests results showed levels of FSH, 33 and anti-Müllerian hormone (AMH), 1.7. She was told that normal IVF was impossible but that it might be possible for her to receive IVF with donor eggs. She was very disappointed and upset, and then visited the current authors' TCM clinic for help.
Clinical manifestations in TCM terms
This patient had short menstrual cycles with long bleeding days, nervousness, restlessness, headache, poor sleep, abdominal pain, and a very upset mood. She had a light-red tongue with red at the tip and sides and many cracks, as well as a deep-wiry pulse.
TCM patterns
Liver Qi Stagnation with Heat and Blood Stasis as well as Kidney Yin Deficiency.
Treatment
Moxibustion was given at CV 8 (Shenque). Acupuncture was given at the following points: CV 3 (Zhongji); CV 6 (Qihai); Ext (Zigong); GV 20 (Baihui); Taiyang, SP 9 (Yinlingquan), SP 6 (Sanyinjiao), KI 3 (Taixi); KI 6 (Zhaohai); KI 10 (Rangu); TE 5 (Waiguan); and GB 41 (Zulinqi). She was given the following herbs:
Shudihuang (Radix Rhemanniae Glutinosae Praeparata) 30
Danggui (Radix Angelicae Sinensis) 10
Heshouwu (Radix Polygoni Multiflori) 10
Gouqizi (Fructus Lycii) 10
Nuzhenzi (Fructus Ligustri Lucidi) 10
Hanliancao (Herba Ecliptae Prostratae) 10
Chaihu (Radix Bupleuri) 10
Yujin (Tuber Curcumae) 10
Zhike (Fructus Citri Aurantii) 10
Honghua (Flos Carthami Tinctorii) 10
Shanyao (Radix Dioscoreae Oppositae) 10
Fuling (Sclerotium Poriae Cocos) 10
Chishao (Radix Paeoniae Rubrae) 10
Before ovulation, the following herbs were added: Zishiying (Fluoritum) 10; Huangbai (Cortex Phellodendri) 10; and Zhimu (Radix Anemarrhenae Asphodeloidis) 10
Before menstruation, the following herbs were added: Aiye (Folium Artemisiae Argyi) 10; Tusizi (Semen Cuscutae Chinensis) 10–30; and Xuduan (Radix Dipsaci Asperi) 10.
She received weekly acupuncture. The abovementioned herbs were decocted as 1 dose per day, and she was given 6 doses per week.
Outcome
After she received regular TCM treatment for 1 year, this patient's condition improved in general, and her menstrual cycles reverted to normal (4–5 days every 28–30 days). Her FSH levels normalized from 33, to 26, to 7.8, and her and AMH improved from 1.7 to 3.5. Her gynecologic consultant had originally evaluated potential success of IVF for her as 1%–9%; that evaluation was upgraded to 39%. Thus, the fertility clinic accepted her for ordinary IVF with her own egg. Two oocytes were retrieved for fertilization, which were transferred into her uterus easily after 4–5 days. She became pregnant soon after and gave birth to a healthy baby girl at full term.
Analysis
IVF is the typical kind of ART that is suitable for treating most forms of infertility. The infertility in this case might have been related to the patient's prolonged use of contraceptive injections, possibly creating an early weakness of her ovaries that manifested as a diminished ovarian reserve (DOR). Her low AMH level and her high FSH level could explain why she had a shorter menstrual cycle and longer bleeding days during her period. According to TCM, she was diagnosed as suffering from Liver Heat and Kidney Yin Deficiency. Therefore, she was given acupuncture and moxibustion to stimulate her ovarian function and herbal medicine to strengthen her Kidney to complement her Qi and Essences, both of which can promote ovarian function significantly. Because she was still young, her ovarian function had not completely been destroyed; therefore, her condition improved significantly with TCM, readying her to receive IVF.
Case 4
Ms. M.S., a 49-year-old teacher, had infertility for 26 years. Her first visit was in May of 2012. She had become pregnant at age 23 but miscarried at 6 weeks in her pregnancy. She had not conceived since that time. When she was in her 40s, she was diagnosed with blocked fallopian tubes, and received IVF twice, but it did not succeed. At age 49, she missed 2 menstruation cycles, and visited a gynecology clinic for treatment. However, the specialist refused her request of more IVF. In desperation, she visited D.J.'s clinic for help.
Clinical manifestations in TCM terms
This patient had exhaustion, hot flashes, depression, tinnitus, insomnia, and other symptoms. Her tongue was red, and she had a wiry-thin pulse.
TCM patterns
Kidney Yin Deficiency, Liver Qi Stagnation, and Spleen Deficiency.
Treatment
Moxibustion was given at CV 8 (Shenque). Acupuncture was given at the following points: GV 20 (Baihui); GV 24 (Shenting); CV 4 (Guanyuan); CV 6 (Qihai); CV 29 (Guilai); LI 4 (Hegu); LR 3 (Taichong); KI 3 (Taixi); KI 10 (Yingu); KI 2 (Rangu); ST 36 (Zusanli); and SP 6 (Sanyinjiao). The following patent herbal medicines were prescribed:
Zhi Bai Di Huang Wan—Cortex Phellodendri, Rhizoma Anemarrhenae, Radix Rehmanniae Praeparata, Rhizoma Dioscoreae, Fructus Corni, Cortex Moutan, Poria, and Rhizoma Alismatis
Jia Wei Xiao Yao Wan—Radix Bupleuri, Anglica Sinensis (Oliv.) Dies, Paeonia Lactiflora Pall, Atractylodes Macrocephala Koidz, Sclerotium Poriae Cocos, Cortex Moutan Radicis, Fructus Gardeniae Jasminoidis, Mentha Haplocalyx Brq., and Glycyrrhizae Uralensis Fisch.
She was given acupuncture once per week and herbal medicines in patent form, having 15 pills of each twice daily.
Outcome
After the first month of treatment, this patient's menstruation resumed. The same treatment was carried out for 6 months, and her menstruation remained regular. Based on this improved female function, she was given IVF and became pregnant. A healthy boy was born at full term.
Analysis
At 49, this patient's chance of natural pregnancy was extremely low. In addition, she had tubal blockage. Overall, the situation was not at all promising. Her clinical features suggested that she was in a premenopausal state. Therefore, the treatment was not aimed at conception, but more importantly to reestablish the functional status of this patient's reproductive system. Following treatment for 6 months, the function was consolidated after her menstruation was resumed. Even with regular menstruation, it was still difficult for her to conceive naturally, as the tubal blockage made the meeting of eggs and sperm impossible. However, her body was ready to house a fetus. Taking advantage of the situation, IVF ensured a successful pregnancy.
Case 5
Ms. T.F., a 27-year-old trainer, had infertility for 5 years, including 3 failed cycles of IVF. Her first visit was in February of 2009. Her husband, Mr. J.F., a 35 year-old engineer, accompanied her. After being unable to become pregnant for more than 5 years, the wife was initially diagnosed with a blockage in her left fallopian tube and cysts on her left ovary. Her husband was had antibodies in his sperm. Laparoscopy was performed to remove the wife's cysts, but, during the procedure, it emerged that both of her fallopian tubes were blocked. Thereafter, the couple tried IVF but the first 3 attempts failed.
The couple both accepted TCM treatment. The wife had regular acupuncture and concentrated herbal powders to regulate her menstrual cycle and the husband had some patent herbs for improving the condition of his sperm.
The wife's clinical manifestations in TCM terms
The wife's TCM patterns
Liver Qi Stagnation and Blood Stasis.
The wife's treatment
The treatment principle applied for the wife in this case was to move the Stagnant Liver Qi and end the Blood Stasis. She was given moxibustion at CV 8 (Shenque). Acupuncture was applied to the following groups of points:
GV 20 (Baihui), CV4 (Guanyuan), CV6 (Qihai), Ext (Zigong), and TE 5 (Waiguan)
LI 4 (Hegu), ST 36 (Zusanli), SP 6 (Sanyinjiao), KI 3 (Taixi), KI 6 (Zhao Hai), and LR 3 (Taichong).
She was prescribed concentrated herbal powders that were equivalent to daily dosages of raw herbs:
Chaihu (Radix Bupleuri) 10
Xiangfu (Rhizoma Cyperi Rotundi) 10
Zhike (Fructus Citri Aurantii) 10
Chishao (Radix Paeoniae Rubrae) 10
Chuanxiong (Radix Ligustici Wallichii) 10
Danggui (Radix Angelicae Sinensis) 10
Yimucao (Herba Leonuri Heterophylli) 10
Ezhu (Rhizoma Curcumae Ezhu) 10
Wangbuliuxing (Semen Vaccariae Segetalis) 10
Taoren (Semen Pruni Persicae) 10
Honghua (Flos Carthami Tinctorii) 10
The following herbs were added after her period: Nuzhenzi (Fructus Ligustri Lucidi) 10; Hanliancao (Herba Ecliptae Prostratae) 10; and Heshouwu (Radix Polygoni Multiflori) 10
• The following herbs were added during ovulation time: YueYueShu sachets were added around ovulation for 3 days; and Baishao (Radix Paeoniae Lactiflorae) 10 and Ejiao (Gelatinum Corii Asini) 10 were added after ovulation.
She was initially given acupuncture once per week, then once every 2 weeks. She also and took 6 g of the abovementioned herbal powders twice daily.
The husband's clinical manifestations in TCM terms
The husband's TCM patterns
Liver Qi Stagnation.
The husband's treatment
The husband was prescribed the following herbal preparations:
Chaihushugan Wan—Radix Paeoniae Alba, Herba Menthae, Pericarpium Citri Reticulatae, Radix Et Rhizoma Rhei, Radix Angelicae Sinensis, Fructus Amomi Cardamomi, Poria, Rhizoma Curcumae, Radix Saposhnikoviae Divaricatae, Radix Platycodi, Radix Scutellariae, Fructus Crataegi, Massa Fermentata Medicinalis, Rhizoma Cyperi, and Fructus Aurantii
Wuziyanzong Wan—Semen Plantaginis, Fructus Lycii, Fructus Rubi, Semen Cuseutae; and Fructus Schisandrae.
He was given the above herbs in patent forms, taking 15 pills each, twice daily.
Outcome
After 2 years of treatment, the couple underwent out a fourth cycle of IVF and had triplets born at full term—1 boy and 2 girls.
Analysis
This was a case of both fallopian tubes being blocked in the wife. IVF was the best option. Nevertheless, the many failures and exhausting IVF attempts made the patient's overall health condition more complicated. Frustration and low morale placed the couple in a difficult position to continue with more cycles of IVF. Acupuncture was used to calm the wife and to stimulate her reproductive function, while herbal powders regulated her unbalanced hormones. This preparation for IVF was not easy; it took 2 years to ensure that the couple were in the right conditions both mentally and physically to proceed to another cycle of IVF. When the couple's overall health reached optimal levels, the IVF was successful. As this case shows, management of both the mental and physical conditions are important.
Case 6
Ms. D.C., a 41-year-old university lecturer, had infertility for 7 years. Her first visit: was in August of 2006. Due to continuous stress from her PhD study and intensive workload, Ms. D.C.'s attempts to become pregnant for 7 years were without positive results. In the last year, her menstruation had become irregular and had ceased in the last 2 months before this first visit to the TCM clinic. Referred by her general practitioner to a local hospital, this patient had a small fibroid (1 × 1cm) in her uterus, which was detected by an ultrasound scan. She asked for IVF but was unable to receive it on through the NHS. In desperation, on advice from her friends, she visited the TCM clinic.
Clinical manifestations in TCM terms
This patient had amenorrhea for 2 months, stress, nervousness, abdominal discomfort, poor sleep, hot flashes, and general aching. She had a light-red tongue with less white coating, and had a wiry pulse.
TCM patterns
Liver Qi Stagnation with Blood Stasis as well as Liver and Kidney Yin Deficiency.
Treatment
This patient was given moxibustion at CV 8 (Shenque). Acupuncture was applied to the following groups of points:
CV 3 (Zhongji), C V6 (Qihai), ST 29 (Guilai), SP 9 (Yinlingquan), and SP 6 (Sanyinjiao)
KI 10 (Rangu), KI 6 (Zhaohai), KI 3 (Taixi), GV 20 (Baihui), TE 5 (Waiguan), and GB 41 (Zulinqi).
She was prescribed the following herbs:
Xiangfu (Rhizoma Cyperi Rotundi) 10
Shudihuang (Radix Rhemanniae Glutinosae Praeparata) 15
Dangguiwei (Radix Angelicae Sinensis [extr¨|mit¨| inf¨|rieure]) 10
Yimucao (Herba Leonuri Heterophylli) 10
Chishao (Radix Paeoniae Rubrae) 10
Honghua (Flos Carthami Tinctorii) 10
Chuanxiong (Radix Ligustici Wallichii) 10
Taoren (Semen Pruni Persicae) 10
Huangbai (Cortex Phellodendri) 10
Zhimu (Radix Anemarrhenae Asphodeloidis) 10
Nvzhenzi (Fructus Ligustri Lucidi) 10
Shanzhuyu (Fructus Corni Officinalis) 10
Hanliancao (Herba Ecliptae Prostratae) 10
Zishiying (Fluoritum) 10.
She was given acupuncture once per week; the above herbs were decocted for drinking twice daily. She took 1 dose per day, 6 dose per week.
Outcome
This patient's menstruation resumed 1 month after treatment. Subsequently, she received TCM treatments that maintained regular periods for 3 months. The couple then decided to go for private fertility treatment and underwent IVF with donor eggs in Barcelona, Spain. The IVF procedure went well, with 2 high-quality fertilized embryos transferred into her uterus. After returning to the United Kingdom, she accepted regular acupuncture again.
In her eighth week of pregnancy, she experienced severe nausea and mild vaginal bleeding. Herbal medicines were prescribed in an attempt to prevent a miscarriage. However, this patient did not wish to take any herbs during pregnancy. When she was checked, it was discovered that 1 fetus was lost. She began taking the prescribed herbal decoction and accepted acupuncture treatment until her twelfth week of pregnancy. Once her overall situation was stabilized, both acupuncture and herbal medicine were discontinued. The herbal prescription for preventing miscarriage of the remaining fetus was:
Sangjisheng (Ramulus Loranthi) 15
Baidoukou (Fructus Amomi Cardamomi) 10
Xiangfu (Rhizoma Cyperi Rotundi) 10
Duzhong (Cortex Eucommiae Ulmoidis) 10
Gouqizi (Fructus Lycii) 10
Huangqi (Radix Astragali Membranacei) 15
Tusizi (Semen Cuscutae Chinensis) 10
Chenpi (Pericarpium Citri Reticulatae) 10
Shanyao (Radix Dioscoreae Oppositae) 10
Fuling (Sclerotium Poriae Cocos) 10
Ejiao (Gelatinum Corii Asini) 10
Shenqu (Massa Medica Fermentata) 10
Zhigancao (Radix Glycyrrhizae Uralensis) 5.
She carried the remaining fetus, a healthy boy, to full term. Two years later, she underwent another transfer of a fertilized embryo. This time, she used acupuncture and herbal medicine for preparation and miscarriage prevention. This second pregnancy was smooth, and she carried a healthy girl to full term.
Analysis
IVF with a donor egg is suitable for those not able to produce good quality eggs. However, the receiver still needs to have a healthy body to support the whole term of pregnancy. Compared to IVF using one's own egg, the procedure is more challenging with higher risks of failure. Treatment to prevent miscarriage has been practiced using TCM for thousands of years with acupuncture and herbal medicine. However, according to most clinical observations, herbs are considered to be more reliable. In this case the patient managed to keep one baby after starting to take herbs. She lost another baby with her decision not to take the herbs due to her anxiety over her concern of the effect of the herbs on the growing fetus. It must be recognized that many medical professionals do not recommend their patients use herbs before and during pregnancy. Therefore, this case opens a window to rethink and re-evaluate the use of Chinese herbs for miscarriage management.
Discussion
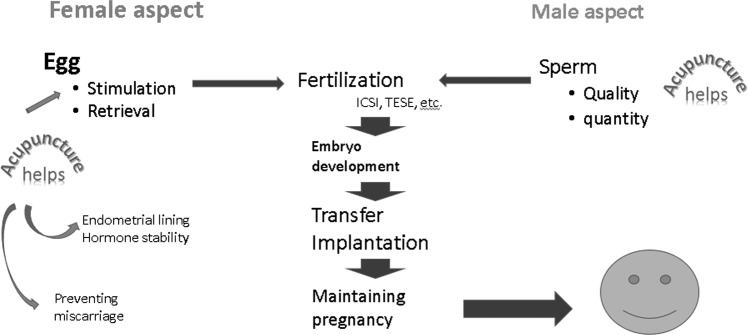
IVF as the most applied ART in practice can be briefly divided into several phases in a pragmatic way for acupuncture practitioners. The current authors' experience, particularly illustrated in the presented 6 cases presented here, suggests that there are three phases when acupuncture should be actively included into an overall treatment plan, namely, (1) the preparation phase, (2) the transplantation phase, and (3) the early pregnancy phase. In each phase, much research has revealed that acupuncture can make favorable changes to assist IVF. This is illustrated in Figure 2.
FIG. 2.
Keys for success in in vitro fertilization and acupuncture intervention. ICSI, introcytoplasmic sperm injection; TESE, testicular sperm extraction.
Holistic Preparation for IVF of Both Parties and Continuing Until Egg Retrieval
Currently, most of the clinical trials of acupuncture-assisted IVF have focused on before and after IVF-ET as the most-quoted trials by Paulus.11,12,18 In some early trials,21 acupuncture was also used before egg retrieval. This technique has not been repeated by other studies and is considered to be valuable only for controlling anxiety.
From their 20 years of clinical experience, the current authors agree that IVF-ET is a key stage at which acupuncture can help improve clinical outcomes. However, it is more important that acupuncture be applied before IVF procedures begin. There are many detrimental factors to ART, including alcohol, smoking, obesity, use of recreational drugs, sexual issues, and more.22 It is also very important to maintain a continuous course of acupuncture when pregnancy is confirmed, as this does not always result in live birth. Using acupuncture together with CHM in clinical practice is considered to be a complete TCM course for preparation of IVF.
It cannot be overlooked that the key from the beginning of treatment is to prepare the couple—both the male and the female—fully to a optimized conditions with combined acupuncture and herbal-medicine approaches. Whenever possible, a normal menstrual cycle should be established first; this can support an embryo to become implanted in the uterus. TCM can improve diminished ovarian reserves,23 increase embryo quality,24 promote endometrial receptivity,25 and harmonize the whole reproductive system.26 Combined treatment can produce a more-balanced state in general for the relevant organic functions to improve both the success rate of ART and the live birth rate.27
All couples who are advised to go through ART procedures should plan early, taking ∼3–6 months to improve the function of the reproductive system and achieve hormonal regulation, to prepare both the body and mind to a preferential condition for ART, and most importantly, to maintain stable physical and mental support for a fetus to stay and grow.
If you are “wanting a harvest, plough the soil before you put the seeds.” This proverb is also true about human reproduction. Representing “the work of the plough,” acupuncture, combined with herbal treatment, has been used for centuries. Both support the whole body, particularly the reproductive system. In TCM terms, the Kidney, Uterus, and the channels moving through the pelvic cavity (Belt, Thoroughfare, and Governor Vessels) must be maintained in an ideal condition to meet the new life and provide all the necessary support to make sure that life prospers inside the Uterus.
The Role of Acupuncture in Stress Management in ART as Well as in IVF-ET
There are many nonmedical aspects that affect ART. It has been observed that stress, financial pressures,28 increasing age, and anxiety linked to medical procedures can all add up to an uncontrollable situation. Two sessions of acupuncture can be effective for controlling anxiety but would not be enough to manage the situation for long, and the whole body condition could not be changed in such a short time.
Acupuncture has been demonstrated to be a very effective way of controlling anxiety, particularly mental anxiety,29 and general anxiety.30 The anxiety involved in undergoing IVF-ET is very similar in nature to mental anxiety; thus, it is expected that this could explain the mechanism of acupuncture's improving the success rate when used with IVF-ET.
It is also well-recognized that acupuncture is a powerful way of managing stress,31 which is one of the major issues affecting ART. Electroacupuncture and ear acupuncture are powerful treatment modalities for combating post-traumatic stress in the short term. However, the ART cycle usually lasts for weeks not just days. Therefore, this needs the solution of regular weekly traditional acupuncture.
The Importance of Preventing Miscarriage
In ART, miscarriage is the main threat to successful fertility treatment.32 Thus, when clinical pregnancy has been achieved, the risk of miscarriage should be evaluated. In particular, during IVF, most reports have cited differences in success rates in clinical pregnancies and live births. Most researchers recognize that the difference is mainly due to the increased risk of miscarriage with IVF in contrast to natural pregnancy.
However, due to concerns about the effect of chemicals ion the embryo and previous experience of damage to the fetus, the choices in conventional medicine are limited when attempting to prevent miscarriage. Yet, existing evidence strongly suggests the use of acupuncture and/or CHM to prevent miscarriage.33 Most importantly, these approaches comprise a nonchemical intervention with no increased risks.34 In all of the cases reported here, TCM treatments needed to be continued into the second trimester to minimize the risk of miscarriage.
Rationale for Selecting the Acupuncture Points Used in the 6 Cases
CV 8 was used with moxibustion for all 6 cases. This point is at the umbilicus, which is considered to be directly linked to the Kidney in Chinese Medicine, where the life essence is stored. It is also at the center of the abdomen (the digestive system, Spleen and Stomach in TCM terms), which supplies nutrition to the whole body. According to Li,35 the point connects the middle Jiao (nutrition source) to the lower Jiao (reproductive center), providing essential support for reproductive health. However, this is never mentioned as a main point for infertility in clinical trials. It is the current authors' clinical experience that warming this point mobilizes Yang Qi to encourage better Kidney (reproductive system) function.
CV 6 is another essential point in all difficult cases. Due to prolonged struggling and worrying, the body is exhausted. In TCM terms, the Qi and Blood are overconsumed. Reestablishing the levels of Qi and Blood can therefore facilitate reproduction. CV 6 is considered to be the “Sea of Qi.”36 This point is safe to use when preparing for IVF and is also safe to use in the early stage of pregnancy.
GV 20 is another point not often mentioned in clinical trials. It is the point shared by the Governor (DU) channel and the Liver (LR) channel.36 GV 20 is very often used to treat depression,37 premenstrual tension,38 and uterine prolapse.35 In the current authors' clinical experience, this point can be used to maintain a good balance of up–down movement of Qi to stabilize a fetus.
KI 6 is a commonly used point for reinforcing the Kidney, the dominant organ in TCM for reproduction. In most of the cases, it was used in combination with KI 3. The combination is considered to mutually boost action in strengthening the Kidney, particularly when there is Kidney Yin Deficiency. Clinical experience suggests that the combination can potentially improve the quality of eggs.39
CV 4 and ST 29 are 2 local points. CV 4 is a point that directly communicates with the Uterus, and ST 29 is located closely over the ovary on each side. Stimulating these local points can increase blood flow into the respective organs. Again, these points are used in the preparation stage and during pregnancy in the early stage.
According to TCM treating principles, the pattern of differentiation at the time of treatment will dictate the selection of the acupuncture points.
Conclusions
From the literature review and case analyses presented here, couples undergoing ART can benefit from combined acupuncture and Chinese herbal treatment, even in very difficult situations when IVF is not recommended by conventional medicine. This holistic approach that treats the individual as a complete life and the couple together as a “working unit” was demonstrated in these cases. Acupuncture should be implemented from the planning stage, for both partners, through to the live birth. The key stages are the stimulation of ovarian function, the preparation for implantation, the calming down of the body to conceive, and the stabilization of the body in early pregnancy to prevent miscarriage. These presented cases show that integrating acupuncture and CHM with IVF offers a much-greater chance of success. This experience should be considered in the future design of clinical trials and is also valuable to practitioners.
Acknowlegments
The current authors extend sincere thanks for the final version of this article to Ms. Jasmin Earnshaw.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Simei Wan was a visiting scholar to Lincoln College in 2019, sponsored by Anhui University of TCM; Fund No: gxgwfx2018039. No funding was received for the clinical review, research, or writing of this article.
References
- 1. Farquhar C, Marjoribanks J. Assisted reproductive technology: An overview of Cochrane reviews. Cochrane Database Syst Rev. 2018;8:CD010537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Johnson MH, Edwards R. The path to IVF. Reprod Biomed Online. 2011;23(2):245–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Human Fertilization & Embryology Authority. All IVF birth rates. In: Fertility Treatment 2014–2016: Trends and Figures. United Kingdom: Human Fertilization & Embryology Authority; 2018:14 Online document at: www.hfea.gov.uk/media/2563/hfea-fertility-trends-and-figures-2017-v2.pdf Accessed May30, 2019 [Google Scholar]
- 4. Zhang X, Lee MS, Smith CA, et al. Effects of acupuncture during in vitro fertilization or intracytoplasmic sperm injection: An updated systematic review and meta-analysis. Eur J Integr Med 2018;23:14–24 [Google Scholar]
- 5. Aquilina L, Bovey M. A Review of the Evidence Base Acupuncture for IVF or ICSI. London: British Acupuncture Council; 2019. [Google Scholar]
- 6. Xu Z-S, Gao Y. Effects of acupuncture on ovarian blood supply and pregnancy outcomes in patients receiving assisted reproduction. J Acupunct Tuina Sci. 2018;16(4):253–259 [Google Scholar]
- 7. Guo J, Li D, Liu C, Ji X, Li R, Du X. Effects of Chinese herbs combined with in vitro fertilization and embryo transplantation on infertility: A clinical randomized controlled trial. J Tradit Chin Med. 2014;34(3):267–273 [DOI] [PubMed] [Google Scholar]
- 8. Ried K. Chinese herbal medicine for female infertility: An updated meta-analysis. Complement Ther Med. 2015;23(1):116–128 [DOI] [PubMed] [Google Scholar]
- 9. Xi J, Chen H, Peng ZH, Tang ZX, Song X, Xia YB. Effects of acupuncture on the outcomes of assisted reproductive technology: An overview of systematic reviews. Evid-Based Complement Alternat Med. 2018;2018:7352735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hullender Rubin LE, Opsahl MS, Wiemer KE, Mist SD, Caughey AB. Impact of whole systems Traditional Chinese Medicine on in-vitro fertilization outcomes. Reprod Biomed Online. 2015;30(6):602–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Paulus WE, Zhang M, Strehler E, El-Danasouri I, Sterzik K. Influence of acupuncture on the pregnancy rate in patients who undergo assisted reproduction therapy. Fertil Steril. 2002;77(4):721–724 [DOI] [PubMed] [Google Scholar]
- 12. Dieterle S, Ying G, Hatzmann W, Neuer A. Effect of acupuncture on the outcome of in vitro fertilization and intracytoplasmic sperm injection: A randomized, prospective, controlled clinical study. Fertil Steril. 2006;85(5):1347–1351 [DOI] [PubMed] [Google Scholar]
- 13. Smith C, Coyle M, Norman RJ. Influence of acupuncture stimulation on pregnancy rates for women undergoing embryo transfer. Fertil Steril. 2006;85(5):1352–1358 [DOI] [PubMed] [Google Scholar]
- 14. Paulus W, Zhang M, Strehler E, Seybold B, Sterzik K. Placebo-controlled trial of acupuncture effects in assisted reproduction therapy [abstr O-052]. 19thAnnual Meeting of the ESHRE, Madrid Spain, June 30, 2003 in Hum Reprod. 2003;18:xviii8–xviii19 [Google Scholar]
- 15. Smith CA, de Lacey S, Chapman M, et al. Effect of acupuncture vs sham acupuncture on live births among women undergoing in vitro fertilization: A randomized clinical trial. JAMA. 2018;319(19):1990–1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Manheimer E, van der Windt D, Cheng K, et al. The effects of acupuncture on rates of clinical pregnancy among women undergoing in vitro fertilization: A systematic review and meta-analysis. Hum Reprod Update. 2013;19(6):696–713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Madaschi C, Braga DP, Figueira Rde C, Iaconelli A Jr, Borges E Jr. Effect of acupuncture on assisted reproduction treatment outcomes. Acupunct Med. 2010;28(4):180–184 [DOI] [PubMed] [Google Scholar]
- 18. Cheong YC, Dix S, Hung Yu Ng E, Ledger WL, Farquhar C. Acupuncture and assisted reproductive technology. Cochrane Database Syst Rev. 2013;7:CD006920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schummers L, Hutcheon JA, Hernandez-Diaz S, et al. Association of short inter-pregnancy interval with pregnancy outcomes according to maternal age. JAMA Intern Med. 2018;178(12):1661–1670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. National Health Service (NHS). Women “Should Leave At Least a Year Between Pregnancies.” October 30, 2018. Online document at: www.nhs.uk/news/pregnancy-and-child/women-should-leave-least-year-between-pregnancies/ Accessed April15, 2019
- 21. Udoff LC, McClamrock HD, Chen K, Zhang G. The effect of acupuncture on pregnancy outcomes in in-vitro fertilization (IVF): A randomized controlled trial. Fertil Steril. 2014;102(3[suppl]):594 [Google Scholar]
- 22. Szmelskyj I, Aquilian L. Acupuncture for IVF and Assisted Reproduction. Edinburgh: Churchill Livingstone; 2015:161 [Google Scholar]
- 23. Zhang Z, Zhang XH, He TY. Smoothing Gan reinforcing Shen method adjuvant treated poor response of diminished ovarian reserve patients in in vitro fertilization and embryo transfer: A clinical study [in Chinese]. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2015;35(10):1170–1174 [PubMed] [Google Scholar]
- 24. Ushiroyama T, Yokoyama N, Hakukawa M, Sakuma K, Ichikawa F, Yoshida S. Clinical efficacy of macrophage-activating Chinese mixed herbs (MACH) in improvement of embryo qualities in women with long-term infertility of unknown aetiology. Am J Chin Med. 2012;40(1):1–10 [DOI] [PubMed] [Google Scholar]
- 25. Guo J, Wang LN, Li D. Exploring the effects of Chinese Medicine in improving uterine endometrial blood flow for increasing the successful rate of in vitro fertilization and embryo transfer [in Chinese]. Zhong Xi Yi Jie He Xue Bao. 2011;9(12):1301–1306 [DOI] [PubMed] [Google Scholar]
- 26. Fang L, Rui-Xia W, Feng-Mei M, Zhen-Gao S, Li-Hong W, Lei S. Effects of Chinese medicines for tonifying the kidney on DNMT1 protein expression in endometrium of infertile women during implantation period. J Altern Complement Med. 2013;19(4):353–359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lu LR, Wu KM. Application of Traditional Chinese Medicine in IVF-ET [in Chinese]. Zhongguo Zhong Yao Za Zhi. 2015;40(16):3142–3146 [PubMed] [Google Scholar]
- 28. Kulkarni G, Mohanty NC, Mohanty IR, Jadhav P, Boricha BG. Survey of reasons for discontinuation from in vitro fertilization treatment among couples attending infertility clinic. J Hum Reprod Sci. 2014;7(4):249–254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Allan FK, Peckham E, Liu JP, et al. Acupuncture for anxiety in dental patients: Systematic review and meta-analysis. Eur J Integr Med. 2018;20(1):22–35. [Google Scholar]
- 30. Amorim D, Amado J, Brito I, et al. Acupuncture and electroacupuncture for anxiety disorders: A systematic review of the clinical research. Complement Ther Clin Pract. 2018;31(1):31–37. [DOI] [PubMed] [Google Scholar]
- 31. Kondo T, Kawamoto M. Acupuncture and moxibustion for stress-related disorders. Biopsychosoc Med. 2014;8(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cameron N, Bhattacharya S, Bhattacharya S, McLernon DJ. Cumulative live birth rates following miscarriage in an initial complete cycle of IVF: A retrospective cohort study of 112 549 women. Hum Reprod. 2017;32(11):2287–2297 [DOI] [PubMed] [Google Scholar]
- 33. Betts D, Smith CA, Hannah DG. Acupuncture as a therapeutic treatment option for threatened miscarriage. BMC Complement Alternat Med. 2012;12:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Carr DJ. The safety of obstetric acupuncture: Forbidden points revisited. Acupunct Med. 2015;33(5):413–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Li SZ. Clinical Application of Commonly Used Acupuncture Points. Hert, United Kingdom: Donica Publishing; 2007 [Google Scholar]
- 36. Deadman P, Al-Khafaji, Baker K. A Manual of Acupuncture. Hove, United Kingdom: Journal of Chinese Medicine Publications; 2007. [Google Scholar]
- 37. Cao H, Bourchier S, Liu J. Does syndrome differentiation matter? A meta-analysis of randomized controlled trials in Cochrane reviews of acupuncture. Med Acupunct. 2012;24(2):68–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Anıl A, Peker T, Göktaş T, Kilic S, Erbaş D. Importance of acupuncture on premenstrual syndrome. Clin Exp Obstet Gynecol. 2012;39(2):209–213 [PubMed] [Google Scholar]
- 39. Toni MA, Zhai XP. The acupuncture treatment of female infertility-with particular reference to egg quality and endometrial receptiveness. J Chin Med. 2012;98:13–21. [Google Scholar]