Abstract
Objective: Acupuncture is recognized as safe for use in pregnancy when correctly performed and has been provided at military healthcare facilities since 2005. Previous research identified a number of pregnant patients receiving acupuncture within the Military Health System (MHS). This study was conducted to describe trends in usage from 2006 to 2016 including patient and provider characteristics.
Materials and Methods: This study utilized TRICARE claims from the MHS Data Repository (MDR). Analysis was performed through the MDR for women ages 18 years and older, who had acupuncture treatments at military treatment facilities related to pregnancy, from 2006 to 2016. Descriptive statistics were collected on patient demographics, clinic types and provider specialties, major diagnostic categories associated with acupuncture, number of visits per patient, and utilization over time.
Results: Less than 0.3% of pregnant women in the MHS received acupuncture. The greatest usage was among patients who were white, ages 25–34, dependents of active duty personnel, and in the Army service. The most common diagnoses were for musculoskeletal system and connective tissue disorders (41.9%). Approximately 79% of care was delivered by physicians. The trend over time rose from 11 visits in 2006 to 130 visits in 2016.
Conclusions: Provision of acupuncture in pregnancy grew ∼12-fold between 2006 and 2016, although usage remains low overall. This greater proportion of physician-provided care in pregnant women versus the general patient population may reflect a cautionary attitude toward use in pregnancy. This research is expected to inform discussions for people seeking to increase access to acupuncture during pregnancy.
Keywords: acupuncture, pregnancy, Military Health System, pain management, Health Services Research, big data
Introduction
Acupuncture is becoming an increasingly popular choice in Western countries for managing the symptoms of pregnancy, including hyperemesis gravidarum, insomnia, prenatal depression, and low-back and pelvic pain; fetal version; induction, augmentation, and analgesia during labor; and pain control following cesarean section.1 Women who choose acupuncture are frequently motivated by a desire for fewer medications and reduced numbers of interventions during pregnancy and delivery.2,3 Acupuncture is generally considered safe in pregnancy when proper technique is followed,4 with reportedly low rates of adverse effects.5 However, this therapy is still considered “alternative” by the Cochrane Collaboration,6 and evidence for acupuncture's effectiveness in pregnancy is mixed.1
The U.S. Military Health System (MHS) has provided acupuncture at military treatment facilities (MTFs) since at least 2005.7 This system provides care to ∼9.5 million military and civilian beneficiaries, who may receive direct care at MTFs or purchase care through referrals to civilian providers, although acupuncture is provided only in the direct-care system.8 Notably, the MHS provides care for 41,150–43,500 deliveries in the direct-care system.9,10 A previous study by some of the current authors identified a small proportion (<1%) of acupuncture visits associated with pregnancy and childbirth in a single year (2014) but did not examine this factor in depth.8
This current, cross-sectional study is the first to investigate the use of acupuncture during pregnancy for women in the MHS and is expected to inform discussion for individuals seeking to increase access to this type of therapy.
Materials and Methods
This study utilized TRICARE claims for 2006 to 2016 from the MHS Data Repository (MDR). TRICARE is a healthcare insurance program that covers uniformed services personnel, retirees, and eligible dependents through several constituent plans. The population consists of ∼20% active-duty and ∼80% civilian beneficiaries, and is demographically representative of the U.S. population under age 65.11 TRICARE data have been used in previous studies investigating women's health,12,13 patient choice,14 effects of provider types,15,16 and other factors.
Analysis was performed through the MDR for women ages 18 years and older, who received acupuncture treatments at MTFs related to pregnancy, during fiscal years 2006–2016. Analysis was limited to direct care (MTFs), as TRICARE does not pay for referral of acupuncture to the private sector. Current Procedural Terminology (CPT) codes were used to identify acupuncture encounters (97810, 97811, 97813, 97814) with an associated pregnancy diagnosis on the same encounter, which was defined by the International Classification of Diseases (ICD), 9th and 10th rev., codes (ICD-9 and ICD-10; V22.xx, V23.xx, V91.xx, Z34.xx, O09.xx, Z3A.xx, O30.xx).
Descriptive statistics were collected on patient demographics (age group, race, beneficiary category, patient/sponsor service, and rank), clinic types, and provider specialties providing acupuncture, major diagnostic categories associated with acupuncture encounters, number of acupuncture visits per patient, and acupuncture utilization over time. All analyses were performed using SAS, version 9.4 (Cary, NC).
This study was carried out as part of the Comparative Effectiveness and Provider-Induced Demand Collaboration (EPIC): A Clinical and Economic Analysis of Variation in Military Healthcare/ Low Value Care in the National Capital Region project. The study was determined to be exempt by the institutional review board of the Uniformed Services University of the Health Sciences, Bethesda, MD.
Results
A total of 329 women received acupuncture during pregnancy over the study duration (2006–2016). The majority were white race, ages 25–34, dependents of active-duty service members, Army service, and other/unknown rank (Table 1). These women collectively had 615 visits during the study, with 53.5% having 1 visit, 17.4% having 2 visits, and 9.8% having 3 visits. A collective 17% had between 4 and 8 visits, and 2.3% had between 9 and 12 visits (Table 2).
Table 1.
Women Receiving Acupuncture During Pregnancy, FY 2006–2016
| Demographics | n (%) |
|---|---|
| Age group | |
| 18–24 | 91 (27.66) |
| 25–34 | 194 (58.97) |
| 35–54 | 44 (13.37) |
| Race | |
| White | 156 (47.42) |
| Black | 19 (5.78) |
| Asian | < 11 |
| Native American/Alaskan Native | < 11 |
| Other | 57 (17.33) |
| Missing/Unknown | 86 (26.14) |
| Beneficiary category | |
| Active duty | 132 (40.12) |
| Dependent of active duty | 173 (52.58) |
| Activated National Guard/Reserves | 13 (3.95) |
| Dependent of other | 11 (3.34) |
| Service | |
| Army | 141 (42.86) |
| Air Force | 95 (28.88) |
| Navy | 46 (13.98) |
| Marines | 44 (13.37) |
| Other | < 11 |
| Patient/sponsor's rank | |
| Enlisted Junior | 50 (15.20) |
| Enlisted Senior | 54 (16.41) |
| Junior Officer | 27 (8.21) |
| Senior Officer | 11 (3.34) |
| Other/Unknown | 187 (56.84) |
FY, fiscal year.
Table 2.
Number of Acupuncture Visits per Patient, Total Visits = 615
| # of acupuncture visits | # of Patients |
|---|---|
| (% of total visits) | |
| 1 | 329 (53.49) |
| 2 | 107 (17.40) |
| 3 | 60 (9.76) |
| 4 | 38 (6.18) |
| 5 | 26 (4.23) |
| 6 | 19 (3.09) |
| 7 | 12 (1.95) |
| 8 | 10 (1.63) |
| 9 | 5 (0.81) |
| 10 | 5 (0.81) |
| 11 | 3 (0.49) |
| 12 | 1 (0.16) |
The most common diagnostic categories for visits were Musculoskeletal and Connective Tissue (42.1%); Factors Influencing Health Status and Other Contacts with Health Services, which includes annual physical examinations (23.3%); and Nervous System (15.8%) (Table 3). The greatest number of visits occurred in family practice clinics (53.7%), followed by pain management (18.1%) and gynecology clinics (10.8%) (Table 4). Family practice and physical medicine physicians each accounted for ∼24%, and chiropractors accounted for 14.6%, of provider types delivering acupuncture to pregnant women (Table 5). Attending providers delivered 99% of these services.
Table 3.
Major Diagnostic Categories for Acupuncture Visits, N = 615
| Diagnostic categories | n (%) |
|---|---|
| Musculoskeletal System and Connective Tissue | 259 (42.11) |
| Factors Influencing Health Status and Other Contacts with Health Services | 143 (23.25) |
| Nervous System | 97 (15.77) |
| Pregnancy, Childbirth, and Puerperium | 68 (11.06) |
| Digestive System | 21 (3.41) |
| Mental Diseases and Disorders | 16 (2.60) |
| Skin, Subcutaneous Tissue, and Breast | 7 (1.14) |
| ENT | 1 (0.16) |
| Circulatory System | 1 (0.16) |
| Female Reproductive System | 1 (0.16) |
| Alcohol/Drug Use and Alcohol/Drug Induced Organic Mental Disorders | 1 (0.16) |
ENT, Ear, Nose, and Throat.
Table 4.
Clinics Associated with Acupuncture Visits, N = 615
| Types of clinics | # of visits (%) |
|---|---|
| Family practice | 330 (53.66) |
| Pain management | 111 (18.05) |
| Gynecology | 65 (10.57) |
| Physical medicine | 55 (8.94) |
| General surgery | 12 (1.95) |
| Obstetrics | 8 (1.30) |
| Neurology | 8 (1.30) |
| Psychology | 8 (1.30) |
| Emergency medical | 5 (0.81) |
| Orthopedic | 3 (0.49) |
| Primary care | 3 (0.49) |
| Physical therapy | 3 (0.49) |
| Mental health | 2 (0.33) |
| Podiatry | 1 (0.16) |
| Occupational health | 1 (0.16) |
Table 5.
Provider Specialties Associated with Acupuncture Visits, N = 615
| Type of practitioner | n (%) |
|---|---|
| Physical medicine physician | 145 (23.58) |
| Family practice physician | 143 (23.25) |
| Chiropractor | 90 (14.64) |
| Obstetrician/gynecologist | 62 (10.08) |
| Contract physician | 51 (8.29) |
| Emergency physician | 28 (4.55) |
| Psychiatrist | 21 (3.42) |
| Corpsman/technician | 15 (2.44) |
| Family practice physician resident/intern with license | 11 (1.79) |
| Anesthesiologist | 9 (1.46) |
| Neurologist | 8 (1.30) |
| Physical therapist | 6 (0.98) |
| Aerospace medical flight surgeon/family practice physician | 6 (0.98) |
| Physician assistant | 5 (0.81) |
| Primary Care nurse–practitioner | 4 (0.65) |
| Certified nurse–midwife | 3 (0.49) |
| Occupational medicine physician | 2 (0.33) |
| Podiatrist | 1 (0.16) |
| Dental officer general | 1 (0.16) |
| Internist | 1 (0.16) |
| General medical officer | 1 (0.16) |
| Social worker (providing therapy) | 1 (0.16) |
| Other service provider | 1 (0.16) |
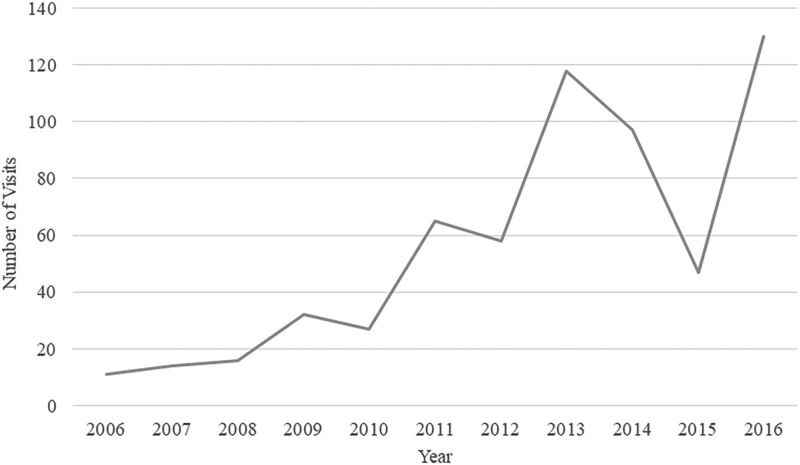
The number of visits per year varied across the study period but showed an upward trend, reaching a peak of 118 visits in 2013. Usage declined in 2014 and 2015, reaching a low of 47 visits in 2015, before increasing again to a peak of 130 visits in 2016 (Figure 1).
FIG. 1.
Use of acupuncture during pregnancy in the U.S. Military Health System (MHS), fiscal years 2006–2016. Claims data were used to assess the total number of acupuncture visits per year by pregnant women in the MHS. There was a general upward trend from 14 visits in 2006 to 130 visits in 2016, with a sharp decrease in 2014–2015.
Discussion
Major Findings
Overall, the greatest proportion of acupuncture was sought for diagnoses of the musculoskeletal system and provided by physicians. This is consistent with results from the previous study of acupuncture in the MHS,8 which included a general patient population of 15,761 men and women ages 18–64. However, the proportions of pregnant women and across the 10-year study period were different from the original study. Previously, 61% of patients received acupuncture associated with musculoskeletal diagnoses, compared to 43% of visits by pregnant women. The category Factors Influencing Health Status and Other Contacts with Health Services, which includes clinical check-ups, was not assessed directly in the original study but accounted for 23% of visits among pregnant women receiving acupuncture. Usage for diagnoses of the nervous system was similar between the 2 studies, accounting for 14.9% of patients in 2014 and 15.8% of visits among pregnant women across the study time. The previous study showed usage of acupuncture for mental health diagnoses in 8.8% of patients, compared with 2.6% of visits in the current study. Less than 1% of patients sought acupuncture for diagnoses related to pregnancy and childbirth in the more-inclusive, previous study, versus 11% of visits in the current study, which only included pregnant women.
While not comparable directly due to differences in inclusion criteria, these findings suggest that the greatest proportion of patients in both pregnant and nonpregnant populations seek acupuncture for pain control. Pain, especially of the low back and pelvis, is a common complaint of pregnancy,17 and the literature describes the effectiveness of acupuncture for relieving this type of pain.1
It is possible that some patients seeking acupuncture for pain control were coded under Pregnancy, Childbirth, and Puerperium; however, this information would be available in detailed clinical records rather than in claims data. Alternately, this difference may reflect the previous study's inclusion of older beneficiaries and of individuals recently returned from active duty, among whom chronic pain is estimated at 44% among those not seeking care.18 The comparatively lower level of usage in the category Pregnancy, Childbirth, and Puerperium, fifth overall by frequency in the current study, was also in line with previous findings that women in the United States more often use acupuncture for health concerns of pregnancy versus during labor and childbirth.3
The breakdown by provider types was also notable. Whereas the previous MHS acupuncture use study showed ∼60% of patients receiving acupuncture from physicians, 10% by physician extenders (nurses, corpsman, technicians), and 4% by chiropractors, this current study of acupuncture in pregnancy showed ∼79% of care delivered by physicians, 3.5% by physician extenders, and 14.6% by chiropractors. A total 99% of acupuncture treatments across all care episodes was delivered by the attending rather than assistant providers. However, this might reflect that service is delivered in line with recommendations by Shah, et al.17 that acupuncture during pregnancy should be provided by a physician.
The most notable finding was the sharp decrease in number of patients receiving acupuncture in pregnancy, from a peak of 118 patients in 2013, falling to 97 patients in 2014 and to a low of 47 patients in 2015. Although there is an upward trend overall, the data show periodicity beginning in 2009, with decreases in even years followed by increases in odd years. The sharp decrease in 2015 was unexpected both for its timing and its steepness. A close review of the data revealed no errors in analysis. The decrease also did not coincide with a known decrease of providers, changes in coding mechanisms, or published changes to policy or practice guidelines. Furthermore, the decrease occurred during the period when the Department of Defense and the Veterans Administration were actively working to increase access to acupuncture for their two health systems, through the Acupuncture Training Across Clinical Settings program.19
Similarly, the scientific literature shows no obvious reason for the decrease, even as a 2014 overview found acupuncture in pregnancy to be generally safe when performed correctly.4 This was supported by a 2015 overview showing that rates of adverse effects were similar in severity and rate of occurrence between acupuncture and nonacupuncture events, although the authors of that systematic review acknowledged that there was poor reporting for many acupuncture trials.5 As more recent data become available, there will be further opportunities to determine if the 2015 decrease was a sudden anomaly or a part of a larger pattern.
These findings must also be considered in the context of efforts to reduce opioid misuse, which is widely regarded as a nationwide epidemic. This is a particular concern for pregnant women, for whom efforts to control pain must be balanced with the potential of harm to the developing fetus. Both opioids and nonsteroidal anti-inflammatory drugs have been linked to birth defects.20 While prevalence of opioid use in pregnancy has not been documented in the MHS, studies suggest that overprescription occurs in obstetric and gynecologic contexts,10 and the 2017 National Defense Authorization Act specifically charged the MHS with greater oversight of opioids.21 Acupuncture potentially is a safer alternative for pain control in pregnancy, but, at a maximum of 130 visits across a minimum of 41,154 births9 per year, this therapy is provided to 0.3% or less women who receive obstetric care in the MHS.
Limitations
This study had several limitations. As with any secondary analysis, clinical nuances are not captured and coding could be subject to clinician error or using “best fit” codes. Care provided outside the MHS, or privately paid, was not captured in this data set. As previously described, the data were not sufficiently granular to determine which type of acupuncture these patients received (i.e., meridian-based, auricular, dry needling, etc.) nor to differentiate between non–needle-based acupuncture modalities, which lack specific CPT codes.8 Therefore, analysis was necessarily limited to needle-based acupuncture. Finally, as a study focused primarily on diagnoses and trends of usage over time, this study did not assess specific degrees of licensure among providers (i.e., medical acupuncturist versus licensed acupuncturist) nor outcomes among patients.
Conclusions
Provision of acupuncture for pregnant women in the MHS is generally low, but showed an approximately twelvefold increase between 2006 and 2016. The greatest proportion of usage appears to be associated with pain control, which is in line with previous studies of usage in the MHS. The comparatively lower usage associated with diagnoses of Pregnancy, Childbirth, and Puerperium is in line with other previous studies of usage during pregnancy for women in the United States. The field of acupuncture would benefit from future research on pregnancy-related outcomes in addition to studies of motivation or hesitancy to adopt this safe, complimentary therapy.
Acknowledgments
This research is part of the EPIC. The authors wish to thank Kitara Byerly, DAcOM, for her insight during the preparation of this article.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This research is supported by a grant from the United States Defense Health Agency (#HU0001-11-1-0023), administered by the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc.
References
- 1. Xu J, McKenzie IZ. The current use of acupuncture during pregnancy and childbirth. Curr Opin Obstet Gynecol. 2012;24(2):65–71 [DOI] [PubMed] [Google Scholar]
- 2. Modlock J, Nielsen BB, Uldbjerg N. Acupuncture for the induction of labour: A double-blind randomized controlled study. BJOG. 2010;117(10):1255–1261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Soliday E, Hapke P. Characteristics of a US obstetric acupuncture clinic patient sample. Explore (NY). 2014;10(2):109–114 [DOI] [PubMed] [Google Scholar]
- 4. Park J, Sohn Y, White AR, Lee H. The safety of acupuncture during pregnancy: A systematic review. Acupunct Med. 2014;32(3):257–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Clarkson CE, O'Mahony DO, Jones DE. Adverse event reporting in studies of penetrating acupuncture during pregnancy: A systematic review. Acta Obstet Gynecol Scand. 2015;94(5):453–464 [DOI] [PubMed] [Google Scholar]
- 6. Wieland LS. Manheimer E, Berman BM. Development and classification of an operational definition of complementary and alternative medicine for the Cochrane Collaboration. Altern Ther Health Med. 2011;17(2):50–59 [PMC free article] [PubMed] [Google Scholar]
- 7. Petri RP Jr, Delgado RE. Integrative medicine experience in the U.S. Department of Defense. Med Acupunct. 2015:27(5):328–334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Madsen C, Patel A, Vaughan M, Koehlmoos T. Use of acupuncture in the United States Military Health System. Med Acupunct 2018;30(1):33–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Watters J, Banaag A, Massengill J, Petersen S, Koehlmoos T, Staat B.. Postpartum opioid use among Military Health System beneficiaries: Lessons from direct and purchased care for the nation [poster]. American College of Obstetricians and Gynecologists Annual Clinical and Scientific Meeting, Nashville, TN, May 3–6, 2019 [Google Scholar]
- 10. TRICARE. Patient Care Numbers for the Military Health System. Online document at: www.tricare.mil/About/Facts/PatientCareNumbers Accessed June26, 2019
- 11. Schoenfeld AJ, Kaji AH, Haider AH. Practical guide to surgical data sets: Military Health System TRICARE encounter data. JAMA Surg. 2018;153(7):679–680 [DOI] [PubMed] [Google Scholar]
- 12. Ranjit A, Chaudhary MA, Jiang W, et al. Disparities in receipt of a laparoscopic operation for ectopic pregnancy among TRICARE beneficiaries. Surgery. 2017;161(5):1341–1347 [DOI] [PubMed] [Google Scholar]
- 13. Ranjit A, Jiang W, Zhan T, et al. Intrapartum obstetric care in the United States military: Comparison of military and civilian systems within TRICARE. Birth. 2017;44(4):337–344 [DOI] [PubMed] [Google Scholar]
- 14. Chaudhary MA, Leow JJ, Mossanen M, et al. Patient driven care in the management of prostate cancer: Analysis of the United States military healthcare system. BMC Urol. 2017;17(1):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dietrich EJ, Leroux T, Santiago CF, Helgeson MD, Richard P, Koehlmoos TP. Assessing practice pattern differences in the treatment of acute low back pain in the United States Military Health System. BMC Health Serv Res. 2018;18(1):720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hamlin L, Patel A.. Perinatal outcomes by provider type in a universally-insured population [poster]. 10th International Council of Nurses Nurse Practitioner/Advance Practice Nursing Conference., Rotterdam, The Netherlands, August 26–29, 2018 [Google Scholar]
- 17. Shah S, Bahn ET, Koury K, Bhatia G, Nandi R, Gulu P. Pain management in pregnancy: Multimodal approaches. Pain Res Treat 2015;2015:987483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Toblin RL, Quartana PJ, Riviere LA, Walper K, Hoge CW. Chronic pain and opioid use in US soldiers after combat deployment. JAMA Intern Med 2014;174(8):1400–1401 [DOI] [PubMed] [Google Scholar]
- 19. Office of the Secretary of Defense. Report to the Committees on Armed Services of the Senate and the House of Representatives: The Implementation of a Comprehensive Policy on Pain Management by the Military Health Care System for Fiscal Year 2015 (2015; pdf)
- 20. Interrante JD, Ailes EC, Lind JN, et al. ; National Birth Defects Prevention Study. Risk comparison for prenatal use of analgesics and selected birth defects: National Birth Defects Prevention Study 1997–2011. Ann Epidemiol. 2017;27(10):645–653.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McCain J. S.2943—National Defense Authorization Act for Fiscal Year 2017 [Conference Report to Accompany S2943, Pub. L. No. S2943 (2016)]. Online document at: www.congress.gov/bill/114th-congress/senate-bill/2943/text Accessed October7, 2019