Abstract
Women are disproportionately impacted by pain compared to men, highlighting the need to better understand factors that contribute to this gender disparity. Previous findings suggest weight-related stigma may be associated with pain among women attempting to lose weight. The goal of this study is to determine if experienced and/or internalized weight bias mediate the relationship between body mass index (BMI) and pain-related impairment in a large, community-based sample of women across the weight spectrum (N = 309; MAge = 56.5, SD = 14.5; MBMI = 28.5, SD = 7.1), and to evaluate whether this relationship differs for women with a pain condition. Analyses were performed using the Conditional-PROCESS Macro to examine the relationships between BMI, pain-related impairment, internalized and experienced weight-stigma, and the potentially moderating effect of pain-related conditions on these relationships. After adjusting for covariates, both experienced stigma and internalized weight stigma statistically mediated the BMI and pain-related impairment relationship; however, in the tests of moderated mediation, the indirect effect of internalized weight bias only held true for those without pain conditions. These findings offer a preliminary conceptual model and highlight the importance of pain research to include weight-related stigma.
Keywords: Bodily pain, weight stigma, weight, pain management, mediation, internalized weight bias
1. Introduction
Pain management is an urgent healthcare issue in the United States. An estimated 25 million US adults experience daily pain, and chronic pain conditions range from 10–55% depending on the population (Nahin, 2015). Pain interferes with patient quality of life, complicates management of other medical conditions, and results in significant economic burden (Andrew, Derry, Taylor, Straube, & Phillips, 2014). As researchers, healthcare providers, and policy advocates grapple with the fall out of the opioid crisis, there is an ever-increasing need to package and deliver new pain management interventions (Tompkins, Hobelmann, & Compton, 2017).
Women are disproportionately impacted by pain and experience greater pain-related impairment compared to men (Fillingim, King, Ribeiro-Dasilva, Rahim-Williams, & Riley, 2009). While biological factors have long been the focus of potential explanations for this disparity, psychological and social factors are increasingly identified as important contributors to gender differences in the experience of pain (Keogh & Herdenfeldt, 2002). Factors such as affective distress, coping style, and social support are consistently associated with pain outcomes and are thought to contribute to gender-related differences in pain experience and long-term results (Meintz & Edwards, 2018). A failure to consider psychological and social influences on the pain experience coupled with an overreliance on monotherapy (use of analgesic medications targeting physiological mechanisms of pain) is believed to contribute to the underwhelming quality of pain management. The oversight of psychological and social factors in pain management is likely to disproportionately impact women compared to men (Mogil, 2012).
There are a number of ways forward to better understand pain among women and to guide development of more effective treatment models. One key area for advancement includes shifting focus from pain severity as the primary indicator of treatment effects in favor of functional outcomes such as interference in daily function. Pain assessment has relied on single-item measures of pain intensity (often on a 0–10 scale), and movement on this scale has been used to assess the efficacy of interventions (Merboth & Barnason, 2000). This assessment has been criticized for oversimplifying the pain experience. Moreover, focusing on decreasing pain severity with medications (i.e., opioids) has led to iatrogenic effects on a catastrophic scale (Sullivan & Ballantyne, 2016). In turn, understanding factors that relate to greater interference of pain on quality of life is encouraged in the service of developing treatments that reduce disability and promote return to functioning rather than elimination of pain. This approach is aligned with evidence-based treatments for pain such as Acceptance and Commitment Therapy, where treatment goals are focused on reducing functional impairment related to pain rather than pain severity (Hughes, Clark, Colclough, Dale, & McMillan, 2017).
In addition to reconsidering the targets/clinical outcomes of pain management, it may be advantageous to identify underlying factors for women that promote multiple empirically-backed risk factors which could then be targeted in order to produce more diffuse positive effects. Emerging findings among higher weight women suggest that weight-related stigma may be one novel contributor to pain-related interference in daily life. Weight-related stigma is a pervasive form of social rejection experienced in overt and covert ways by many individuals (Puhl et al., 2015). Individuals may have stigmatizing experiences (experienced stigma) and may also internalize negative weight-related attributes about themselves (internalized weight bias). Both forms of weight stigma are robustly linked with psychological distress, maladaptive coping, as well as loneliness and less social support (Papadopoulos & Brennan, 2015). As factors such as depression, anxiety, low social support/isolation prospectively predict worse outcomes in the context of pain (Karayannis, Baumann, Sturgeon, Melloh, & Mackey, 2018; Lerman, Rudich, Brill, Shaley, & Shahar, 2015), weight stigmatization may be a common factor contributing to these well-established risk factors for poor adjustment among individuals who are experiencing pain. Indeed, preliminary data suggest that both experienced stigma and internalized weight bias are associated with greater symptoms of bodily pain in those higher on the weight spectrum (Olson, Landers, Thaxton & Emery, 2018; Olson, Landers, & Emery, 2018; Pearl, White, & Grilo, 2014).
Because societal standards of beauty for women promote thinness, experiences of weight stigma and internalization of weight bias may adversely impact women across the weight spectrum (Eisenberg, Berge, Fulkerson, & Neumark-Sztainer, 2011; Hunger, Blodorn, Miller, & Major, 2018; Pearl & Puhl, 2014). Further, it is unclear if weight-related stigmas (experienced and internalized bias) influence pain outcomes similarly in the context of non-chronic versus chronic pain. There may be important neuroanatomical differences among individuals with non-chronic pain compared to those with chronic pain conditions that suggests findings in one sample should not be assumed to transfer to the other (Bushnell, Ceko, & Low, 2013). As such, it is advantageous to study psychosocial factors in those with and without chronic pain to advance our understanding of pain phenomenology. The goal of the current study is to extend the existing evidence base on body mass index (BMI), weight stigma, and pain-related outcomes by: (a) determining if experienced stigma and/or internalized weight bias mediate the BMI to pain-related impairment relationship in a community-based sample of women with varying body weights, and (b) evaluating if these relationships differ based on presence or absence of a pain-related condition.
2. Method
2.1. Participants and Procedure
The current study is a secondary analysis of data collected from a sample of US women who were recruited online for a cross-sectional, observational study of healthcare avoidance (Mensinger, Tylka, & Calamari, 2018). Data collection was coordinated by a Qualtrics project manager (Qualtrics, Provo, UT) who aids with securing targeted samples for survey research. The database consists of large samples of individuals who register through Qualtrics to receive emails about opportunities to participant in research. Information about studies in which they may be eligible to participate is emailed to registrants on a regular and ongoing basis. Eligibility for participation in the study that is the source for this secondary analysis included being a US-dwelling female and between 25–85 years of age. Data collection was completed during a 2-week period during Fall 2016. A series of quality checks (i.e., attention checks that ensure participants were reading items, e.g., “Please mark 3 for this item.”) were implemented in accordance with best standards for online data collection to ensure the validity of the final data set. The IRB of the second author’s institution reviewed and approved the protocol for collecting the study data.
A total of 309 women were included in the study. Six women were excluded (four for reported/suspected pregnancy, and two for unlikely BMI values [i.e., < 10]). No data were missing given that the survey required responses to all items. Demographic information for the final sample is described in Table 1.
Table 1.
Demographic characteristics of the study sample.
| Characteristic | n (%) |
|---|---|
| Education | |
| Less than high school degree | 3 (1.0) |
| High school degree or equivalent (e.g., GED) | 58 (18.8) |
| Some college or trade school | 120 (38.8) |
| Bachelor’s Degree | 86 (27.8) |
| Master’s Degree or equivalent | 40 (12.9) |
| Doctoral Degree (e.g., MD, PhD, JD) | 2 (0.6) |
| Employment Status | |
| Employed full-time (40 or more hours per week) | 94 (30.4) |
| Employed part-time (1–39 hours per week) | 45 (14.6) |
| Not working (e.g., disability, student, homemaker) | 62 (20.1) |
| Retired | 108 (35.0) |
| Race/ Ethnicity | |
| Black/ African-American | 14 (4.5) |
| Hispanic/ Latinx | 12 (3.9) |
| White/ Caucasian | 266 (86.1) |
| Asian | 9 (2.9) |
| Native American/ Alaskan Native | 1 (0.3) |
| Multi-racial/ Mixed | 4 (1.3) |
| Other*/ None of the above | 3 (1.0) |
| Marital Status | |
| Married or cohabiting with partner | 181 (58.6) |
| Widowed | 34 (11.0) |
| Divorced or separated | 48 (15.5) |
| Single/ never married | 46 (14.9) |
| Annual Household Income, USD | |
| Less than $20,000 | 34 (11.0) |
| $20,000-$39,999 | 72 (23.3) |
| $40,000-$59,999 | 77 (24.9) |
| $60,000-$79,999 | 42 (13.5) |
| $80,000-$99,999 | 34 (11.0) |
| More than $100,000 | 50 (16.2) |
| Children | |
| Yes | 198 (64.1) |
| No | 111 (35.9) |
| Pain-related condition | |
| Yes | 40 (12.9) |
| No | 269 (87.1) |
| Mean Age, years (SD) (Range) | 56.5 (14.5) (25.0–84.0) |
| Mean Body Mass Index, kg/m2 (SD) (Range) | 28.5 (7.1) (16.0–54.2) |
N = 309; after excluding four women who identified as pregnant, and two whose BMI < 10.
The ‘Other’ category included a collapsed group of people identifying as either Native Hawaiian/Pacific Islander or Middle Eastern
2.2. Measures
2.2.1. Demographics.
Basic demographic information was collected from all participants including age, race/ethnicity, marital status, and socioeconomic information.
2.2.2. Pain conditions.
Participants were asked “Do you, or have you had a longstanding illness, disability, or infirmity?” and were prompted to choose from the following answers; yes-current, yes-past, or no. Individuals who selected yes-current were then asked to list or describe the condition(s). For descriptive purposes, the self-reported conditions were categorically grouped into the following pain-related conditions: headaches/migraines, knee pain, back pain, fibromyalgia, arthritis, and other. For analyses, a dichotomous yes/no variable was used to indicate whether or not the participant reported a pain condition.
2.2.3. Body mass index (BMI).
Current height and weight were self-reported by participants in pounds and inches. Values were converted into metric measurement units and used to calculate BMI (kilograms/meter2).
2.2.4. Experienced weight stigma.
We used the abbreviated Stigmatizing Situations Inventory (SSI-Brief; Vartanian, 2015) to assess the experience of weight stigma. The SSI-Brief is a 10-item self-report questionnaire in which individuals are asked to report the frequency of experiencing common types of weight-related stigmatization on a 9-point Likert-type scale (0 = never to 9 = daily). Cronbach’s alpha for the SSI-Brief in the current study is .91.
2.2.5. Internalized weight stigma.
The Weight Bias Internalization Scale-Modified (WBIS-M; Pearl & Puhl, 2014) was used to assess the degree to which participants report believing society’s negative attitudes towards higher body weights are accurate and/or true for themselves. The WBIS-M was modified from the Weight Bias Internalization Scale (WBIS; Durso & Latner, 2008) so that the language was appropriate for a range of body weights. Participants rate statements that are consistent (or inconsistent) with internalized weight bias on a 7-point Likert scale (1 = strongly disagree to 7 = strongly agree). For the current study, a 10-item version of the questionnaire was used, as the first item of the measure was excluded to be consistent with current practices in the field (Hilbert et al., 2014). Cronbach’s alpha for the WBIS-M in the current study is .96.
2.2.6. Pain-related impairment.
Pain-related impairment was assessed with one item from the SF-12v2 (Kosinski, Ware, Turner-Bowker, & Gandek, 2007). The SF-12v2 is a brief, validated version of one of the most commonly used measures of generic health status (SF-36). The pain item in the SF-12v2 asks “During the past 4 weeks, how much did pain interfere with your normal work (including both work outside the home and housework)?” and participants select one of the following ratings: not at all (1), a little bit (2), moderately (3), quite a bit (4), or extremely (5).
2.3. Analytic Strategy
The PROCESS (Hayes, 2013) macro (version 3.3) in SPSS was used to evaluate the hypotheses that experienced stigma and/or internalized weight bias mediate the relationship between BMI and pain-related impairment and to evaluate pain condition (yes/no) as a moderating variable. Conditional mediation models using 5000 percentile bootstrapped samples with 95% confidence intervals were used to test direct and conditional indirect effects among the predictor, BMI, and the pain-related impairment outcome variable. Pain condition was tested as a moderator of the relationship between BMI and weight stigma and also of the relationship between weight stigma and pain interference. Covariates included demographic factors robustly linked to pain phenomenology (Edwards, Filingim, & Keefe, 2001; Gibson & Farrell, 2004; Poleshuck & Green, 2008) including race (White/Ethnic Minority), age, and income.
3. Results
The average values for BMI, SSI-Brief, WBIS-M, and the SF-12v2 pain item are presented in Table 1 along with a correlation matrix of these key variables. BMI, both stigma measures, and pain interference were all significantly and positively associated. Almost 13% of the sample reported a pain condition, with arthritis being the most common condition followed by back pain, fibromyalgia, knee pain, headaches/migraine, and then other conditions where pain was noted (e.g., Meniere’s disease, Crohn’s disease, muscular sclerosis, tendonitis). Individuals who reported a pain condition had a higher BMI (Non-pain: M = 28.0 kg/m2, SD = 6.7; Pain: M = 31.7 kg/m2, SD = 8.8, p < .01), were older (Non-pain: M = 61.2 years, SD = 12.1; Pain: M = 55.7 years, SD = 14.7, p = .02), and reported greater pain interference (Non-pain: M = 1.66, SD = 0.92; Pain: M = 2.95, SD = 0.99, p < .01), but no differences in experienced stigma or internalized weight bias were observed.
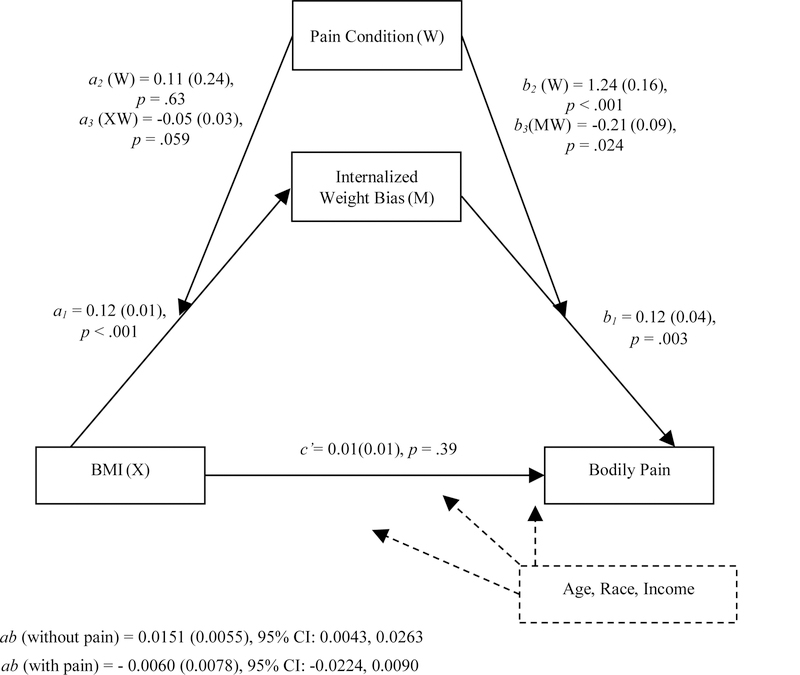
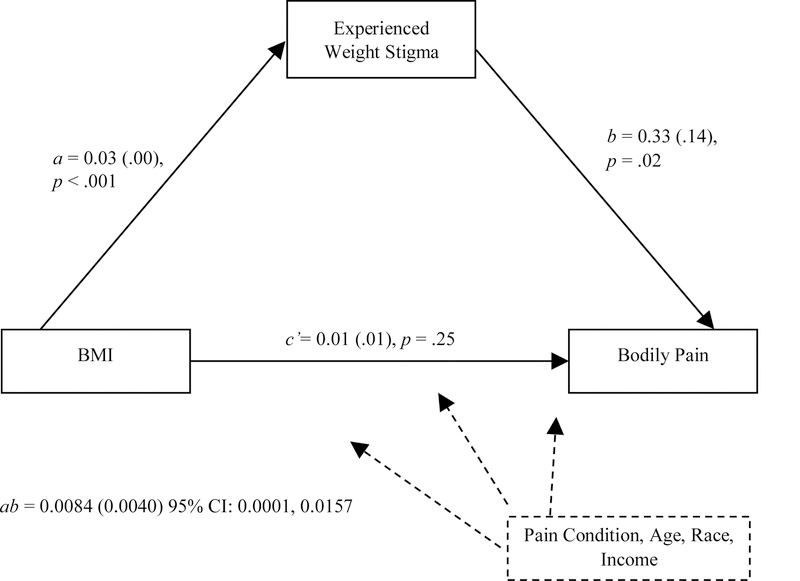
In the conditional mediation model for internalized weight bias, the Index of Moderated Mediation was significant, β = −0.0212, SE = 0.0091, 95% CI: −0.0395, −0.0038. As shown in Figure 1, the indirect effect of internalized weight bias was upheld for individuals without a pain condition but not among those who reported a pain condition. The Index of Moderated Mediation, however, was not significant for experienced stigma, β = −0.0025, SE = 0.0175, 95% CI: −0.0394, 0.0292. This suggests that the presence of a pain condition does not significantly change the mediation effect of experiences of weight stigma on the relationship between BMI and pain interference. Thus, we modeled the simple mediation effect of experiences of weight stigma on the BMI and pain interference relationship (see Figure 2). This analysis demonstrated that the indirect effect of BMI on pain interference through experienced stigma was significant, ab = 0.0084 (0.0040); 95% CI: 0.0001, 0.0202.
Figure 1.
Internalized weight bias conditionally mediates the relationship between BMI and interference of bodily pain on daily functioning controlling for age, race, and income on all pathways. Values reported are beta coefficients and standard errors for direct and indirect effects.
Figure 2.
Experienced weight stigma mediates the relationship between BMI and the interference of bodily pain on daily functioning controlling for the presence of a pain condition, age, race, and income on all pathways. Values reported are beta coefficients and standard errors for direct and indirect effects.
4. Discussion
This study demonstrates that weight-related stigma is associated with pain symptoms in a non-clinical/community sample of women and that these relationships are evident for individuals across the weight spectrum. The current findings are consistent with earlier work that focused on the relationship between body weight, weight-related stigmas, and pain symptoms exclusively among weight management treatment-seeking individuals of higher body weight. Increasingly, higher BMI has been implicated as a risk factor for increased pain and more recently for reduced benefit from pain management treatment (Hitt, McMillen, Thornton-Neaves, Koch, & Cosby, 2007; Kaleth, Slaven, & Ang, 2018; Sellinger et al., 2010). While previous research has relied on physiological explanations (such as greater biomechanical loading on joints) for why higher body weight might relate to increased pain symptoms among individuals with chronic pain (Okifuji & Hare, 2015), the current findings suggest that stress induced by anti-fat bias may be involved in greater experiences of pain for individuals with and without pain conditions and of all sizes.
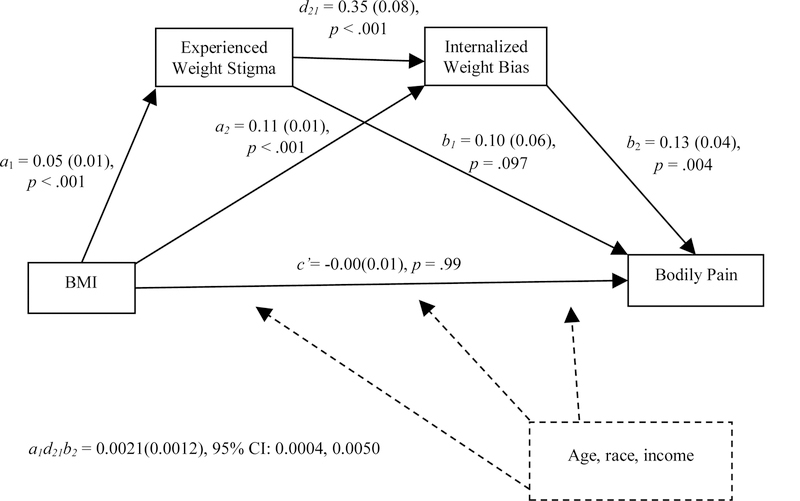
Internalized weight bias statistically mediated the relationship between body mass and pain-related impairment only among individuals who did not have a pain-related condition. Increasingly, internalized weight bias has been shown to mediate the effects of experienced weight stigma on a variety of health behaviors and outcomes (e.g., eating behavior, exercise, healthcare avoidance; Mensinger et al., 2018; O’Brien et al., 2016; Pearl, Puhl, & Dovidio, 2015). Therefore, among individuals without a chronic pain condition (given the presence of the significant moderation of pain for internalized weight bias) we evaluated a post-hoc serial mediation test evaluating BMI → experienced weight stigma → internalized weight bias → pain-related impairment. This model was significant, serial indirect effect = 0.0021(0.0012), 95% CI: 0.0004, 0.0050, suggesting that higher body weight is associated with greater experiences of weight-related stigmatization, which contribute to greater internalization of negative weight-related attitudes about the self, and ultimately this is associated with greater pain-related impairment in daily life (see Figure 3).
Figure 3.
For individuals without a pain condition (n = 269), experienced weight stigma and internalized weight bias serially mediate the relationship between BMI and the interference of bodily pain on daily functioning, controlling for age, race, and income on all pathways. Values reported are beta coefficients and standard errors for direct and indirect effects.
Additionally, our findings showed that experienced weight stigma mediated the BMI to pain interference relationship among all individuals, regardless of pain condition. Taken together, these findings suggest that weight-related stigmatization directly impacts pain interference among everyone, while internalization of weight bias may play an important intermediate role for those without a pain condition. This is likely because of the stronger overriding factors at play for those with chronic pain conditions. Indeed, factors directly related to pain severity and treatment may account for such a significant amount of the variance in pain-related interference that a contribution of internalized weight bias may not be relevant or detectable given the relatively smaller number of individuals with chronic pain in our sample. Given the post hoc nature of this serial mediation model, it is critical to replicate such findings before any further investigation of the proposed pathways.
The cross-sectional nature of these data prevents true mechanistic or causal conclusions, but the findings highlight an understudied factor that may be relevant for understanding pain among women. There are a number of existing frameworks that may clarify how weight stigmas influence the experience of pain. As discussed previously, weight-related stigma is consistently associated with psychological distress, difficulties with coping, and decrements in social functioning (reduced social support and loneliness; Papadopoulos & Brennan, 2015). As such, women who experience weight stigmatization may exist within a psychosocial landscape that results in reduced resources for coping or greater barriers to adjustment. This is consistent with Minority Stress Theory (Meyer, 2003), which suggests that marginalized individuals experience unique and chronic stress that interferes with functioning and quality of life. There is also evidence suggesting that social pain and physical pain are processed through similar neuroanatomical and physiological mechanisms (Eisenberger & Lieberman, 2004), suggesting that the social rejection of weight stigmatization may directly contribute to pain symptoms and greater activation of pain response processes makes it more challenging to adapt. Similarly, Dickerson and colleagues (2004) proposed that threats to the social self induces a stress response that increases proinflammatory cytokine activity, which is similar to Tomiyama’s (2014) model proposing that weight-related stigmatization causes stress resulting in dysregulated cortisol reactivity. As such, there is plenty of empirical context and theoretical scaffolding on which to place this new area of exploration and help guide our understanding of weight stigma and pain. Just as best practices in pain management call for integrated and multidisciplinary treatment approaches, the study of weight stigma and pain will benefit from multiple areas of expertise collaborating to better understand these relationships.
There are a number of limitations of the current study. The data were collected online and rely entirely on self-report information. While this is advantageous for reaching a wider range of individuals, and methods were implemented to ensure validity of the data, it is important to consider this potential source of error. Similarly, individuals without chronic pain were disproportionately represented in the current sample. The relatively smaller subset of individuals with chronic pain conditions may have contributed to the nonsignificant effects of internalized weight bias. As this was a secondary analysis, future studies designed to replicate and expand the presented findings will benefit from a more balanced sample. The assessment of pain in the current study was a single item focusing specifically on pain-related impairment from the SF-12v2, and thus should be interpreted cautiously. While it is consistent with pain assessment methodology and drawn from a validated measure based on the bodily pain subscale of one of the most widely used pain assessment tools (SF-36), the assumption is that pain is present when interference in life due to pain is endorsed, but the cause or severity of pain remains unknown. Future research will benefit from a more comprehensive assessment of pain severity, degree of impairment (interference with functioning), location on the body, etc.
Lastly, the current study is limited due to its exclusive reliance on cross-sectional data. The use of mediation analysis with cross-sectional data is controversial due to the inability to determine the time course of one variable’s effect on the subsequent variable in the model (Hayes, 2017). Although cross-sectional data is useful for establishing preliminary conceptual models for ultimately testing in more rigorous experimental and longitudinal designs, we are unable to draw any causal conclusions about the relationships found. Certainly, the reverse direction may be plausible (the presence of pain symptoms may causally exacerbate internalized weight bias related to self-blame, or elicit stigmatizing reactions from health care providers or interpersonal contacts, which may in turn promote dysregulation of cortisol resulting in higher body weight, as discussed above in Tomiyama [2014]). It seems that both possible directions would be of clinical interest and warrant further investigation.
In conclusion, these findings highlight weight-related stigma as an overlooked area within pain research. The current findings suggest that for women of varying body weights, weight stigma (both experienced and internalized) may contribute to greater interference of pain symptoms in daily life and that these relationships are most salient for those without a pain-related health condition. Indeed, further research is necessary and if substantiated, these findings suggest that weight-related stigma may be an important topic to consider incorporating into biopsychosocial models of pain management.
Weight stigma and internalized weight bias are associated with pain-related interference.
Stigma mediated the relationship between body mass and pain among all individuals.
Internalized bias only mediated the relationship among women without a pain condition.
Acknowledgements:
We greatly appreciate the information given and time dedicated by the research participants without whom this work would be impossible
Funding Support: The data collection for this paper was supported by an internal research award granted to the second author by Drexel University’s College of Nursing and Health Professions. The first author is funded on an NIH training grant (T32 HL076134).
Footnotes
Conflict of interest: The authors declare that they have no conflicts of interest.
References
- Andrew R, Derry S, Taylor RS, Straube S, & Phillips CJ. (2014). The costs and consequences of adequately managed chronic non‐cancer pain and chronic neuropathic pain. Pain Practice, 14, 79–94. doi: 10.1111/papr.12050 [DOI] [PubMed] [Google Scholar]
- Bushnell MC, Čeko M, & Low LA. (2013). Cognitive and emotional control of pain and its disruption in chronic pain. Nature Reviews Neuroscience, 14, 502–511. doi: 10.1038/nm3516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson SS, Gruenewald TL, & Kemeny ME. (2004). When the social self is threatened: Shame, physiology, and health. Journal of Personality, 72, 1191–1216. doi: 10.1111/j.1467-6494.2004.00295.x [DOI] [PubMed] [Google Scholar]
- Durso LE, & Latner JD. (2008). Understanding self‐directed stigma: Development of the Weight Bias Internalization Scale. Obesity, 16, S80–S86. doi: 10.1038/oby.2008.448 [DOI] [PubMed] [Google Scholar]
- Edwards CL, Fillingim RB, & Keefe F. (2001). Race, ethnicity and pain. Pain, 94, 133–137. doi: 10.1016/S0304-3959(01)00408-0 [DOI] [PubMed] [Google Scholar]
- Eisenberg ME, Berge JM, Fulkerson JA, & Neumark-Sztainer D. (2011). Weight comments by family and significant others in young adulthood. Body Image, 8, 12–19. doi: 10.1016/j.bodyim.2010.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI, & Lieberman MD. (2004). Why rejection hurts: A common neural alarm system for physical and social pain. Trends in Cognitive Sciences, 8, 294–300. doi: 10.1016/j.tics.2004.05.010 [DOI] [PubMed] [Google Scholar]
- Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, & Riley JL. (2009). Sex, gender, and pain: A review of recent clinical and experimental findings. The Journal of Pain, 10, 447–485. doi: 10.1016/j.jpain.2008.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson SJ, & Farrell M. (2004). A review of age differences in the neurophysiology of nociception and the perceptual experience of pain. The Clinical Journal of Pain, 20, 227–239. doi: 10.1097/00002508-200407000-00004 [DOI] [PubMed] [Google Scholar]
- Hayes AF. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford. [Google Scholar]
- Hilbert A, Baldofski S, Zenger M, Löwe B, Kersting A, & Braehler E. (2014). Weight Bias Internalization Scale: Psychometric properties and population norms. PLoS One, 9, e86303. doi: 10.1016/j.bodyim.2016.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitt HC, McMillen RC, Thornton-Neaves T, Koch K, & Cosby AG. (2007). Comorbidity of obesity and pain in a general population: Results from the Southern Pain Prevalence Study. The Journal of Pain, 8, 430–436. doi: 10.1016/j.jpain.2006.12.003 [DOI] [PubMed] [Google Scholar]
- Hughes LS, Clark J, Colclough JA, Dale E, & McMillan D. (2017). Acceptance and Commitment Therapy (ACT) for chronic pain. The Clinical Journal of Pain, 33, 552–568. doi: 10.1097/AJP.0000000000000425 [DOI] [PubMed] [Google Scholar]
- Hunger JM, Blodorn A, Miller CT, & Major B. (2018). The psychological and physiological effects of interacting with an anti-fat peer. Body Image, 27, 148–155. 10.1016/j.bodyim.2018.09.002 [DOI] [PubMed] [Google Scholar]
- Kaleth AS, Slaven JE, & Ang DC. (2018). Obesity moderates the effects of motivational interviewing treatment outcomes in fibromyalgia. The Clinical Journal of Pain, 34, 76–81. doi: 10.1097/AJP.0000000000000500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karayannis NV, Baumann I, Sturgeon JA, Melloh M, & Mackey SC. (2018). The impact of social isolation on pain interference: A longitudinal study. Annals of Behavioral Medicine, 53, 65–74. doi: 10.1093/abm/kay017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keogh E, & Herdenfeldt M. (2002). Gender, coping and the perception of pain. Pain, 97, 195–201. doi: 10.1016/S0304-3959(01)00427-4 [DOI] [PubMed] [Google Scholar]
- Kosinski M, Ware JE, Turner-Bowker DM, & Gandek B. (2007). User’s manual for the SF-12v2 health survey: With a supplement documenting the SF-12® health survey. Lincoln, RI: QualityMetric Incorporated. [Google Scholar]
- Lerman SF, Rudich Z, Brill S, Shalev H, & Shahar G. (2015). Longitudinal associations between depression, anxiety, pain, and pain-related disability in chronic pain patients. Psychosomatic Medicine, 77, 333–341. doi: 10.1097/PSY.0000000000000158 [DOI] [PubMed] [Google Scholar]
- Meints SM, & Edwards RR. (2018). Evaluating psychosocial contributions to chronic pain outcomes. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 87, 168–182. doi: 10.1016/j.pnpbp.2018.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mensinger JL, Tylka TL, & Calamari ME. (2018). Mechanisms underlying weight status and healthcare avoidance in women: A study of weight stigma, body-related shame and guilt, and healthcare stress. Body Image, 25, 139–147. doi: 10.1016/j.bodyim.2018.03.001 [DOI] [PubMed] [Google Scholar]
- Merboth MK, & Barnason S. (2000). Managing pain: The fifth vital sign. The Nursing Clinics of North America, 35, 375–383. [PubMed] [Google Scholar]
- Meyer IH. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. doi: 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogil JS. (2012). Sex differences in pain and pain inhibition: Multiple explanations of a controversial phenomenon. Nature Reviews Neuroscience, 13, 859–866. doi: 10.1038/nrn3360 [DOI] [PubMed] [Google Scholar]
- Nahin RL. (2015). Estimates of pain prevalence and severity in adults: United States, 2012. The Journal of Pain, 16, 769–780. doi: 10.1016/j.jpain.2015.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien KS, Latner JD, Puhl RM, Vartanian LR, Giles C, Griva K, & Carter A. (2016). The relationship between weight stigma and eating behavior is explained by weight bias internalization and psychological distress. Appetite, 102, 70–76. doi: 10.1016/j.appet.2016.02.032 [DOI] [PubMed] [Google Scholar]
- Olson KL, Landers JD, Thaxton TT, & Emery CF. (2018). The pain of weight-related stigma among women with overweight or obesity. Stigma and Health. Advance online publication. doi: 10.1037/sah0000137 [DOI] [PMC free article] [PubMed]
- Olson KL, Landers J, & Emery CF. (2018, June). Does weight stigma hurt? Exploring the overlap of physical and emotional pain. Paper presented at the International Weight Stigma Conference, Leeds, UK. [Google Scholar]
- Okifuji A, & Hare BD. (2015). The association between chronic pain and obesity. Journal of Pain Research, 8, 399–408. doi: 10.2147/JPR.S55598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papadopoulos S, & Brennan L. (2015). Correlates of weight stigma in adults with overweight and obesity: A systematic literature review. Obesity, 23, 1743–1760. doi: 10.1002/oby.21187 [DOI] [PubMed] [Google Scholar]
- Pearl RL, & Puhl RM. (2014). Measuring internalized weight attitudes across body weight categories: Validation of the modified Weight Bias Internalization Scale. Body Image, 11, 89–92. doi: 10.1016/j.bodyim.2013.09.005 [DOI] [PubMed] [Google Scholar]
- Pearl RL, Puhl RM, & Dovidio JF. (2015). Differential effects of weight bias experiences and internalization on exercise among women with overweight and obesity. Journal of Health Psychology, 20, 1626–1632. doi: 10.1177/1359105313520338 [DOI] [PubMed] [Google Scholar]
- Pearl RL, White MA, & Grilo CM. (2014). Weight bias internalization, depression, and self‐reported health among overweight binge eating disorder patients. Obesity, 22, e142–e148. doi: 10.1002/oby.20617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poleshuck EL, & Green CR. (2008). Socioeconomic disadvantage and pain. Pain, 136, 235–238. doi: 10.1016/j.pain.2008.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl RM, Latner JD, O’Brien K, Luedicke J, Danielsdottir S, & Forhan M. (2015). A multi-national examination of weight bias: Predictors of anti-fat attitudes across four countries. International Journal of Obesity, 39, 1166–1173. doi: 10.1038/ijo.2015.32 [DOI] [PubMed] [Google Scholar]
- Sellinger JJ, Clark EA, Shulman M, Rosenberger PH, Heapy AA, & Kerns RD. (2010). The moderating effect of obesity on cognitive–behavioral pain treatment outcomes. Pain Medicine, 11, 1381–1390. doi: 10.1111/j.1526-4637.2010.00935.x [DOI] [PubMed] [Google Scholar]
- Sullivan MD, & Ballantyne JC. (2016). Must we reduce pain intensity to treat chronic pain? Pain, 157, 65–69. doi: 10.1097/j.pain.0000000000000336 [DOI] [PubMed] [Google Scholar]
- Tomiyama AJ. (2014). Weight stigma is stressful. A review of evidence for the Cyclic Obesity/Weight-Based Stigma model. Appetite, 82, 8–15. doi: 10.1016/j.appet.2014.06.108 [DOI] [PubMed] [Google Scholar]
- Tompkins DA, Hobelmann JG, & Compton P. (2017). Providing chronic pain management in the “Fifth Vital Sign” Era: Historical and treatment perspectives on a modern-day medical dilemma. Drug and Alcohol Dependence, 173, S11–S21. doi: 10.1016/j.drugalcdep.2016.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vartanian LR. (2015). Development and validation of a brief version of the Stigmatizing Situations Inventory. Obesity Science & Practice, 1, 119–125. doi: 10.1002/osp4.11 [DOI] [PMC free article] [PubMed] [Google Scholar]