Abstract
OBJECTIVE:
To assess a continuum of cervical length (CL) cutoffs for ultrasound-indicated cerclage efficacy in women with prior spontaneous preterm birth (PTB).
METHODS:
Planned secondary analysis of the NICHD-sponsored vaginal ultrasound cerclage trial. Cerclage efficacy for preventing recurrent PTB at <35, <32 and <24 wks gestation (GA) was assessed using multivariable logistic regression. Odds ratios (ORs) and confidence intervals (CIs) were estimated for a range of CL cutoffs using bootstrap regression. The 2.5th and 97.5th percentiles of bootstrapped ORs determined the CIs. Results are illustrated with smoothed curves superimposed on the estimated ORs by CL cutoff.
RESULTS:
Of 301 women with CL <25mm, 142 underwent ultrasound-indicated cerclage and 159 did not. Few cases of CL <10mm limited evaluation to CL cutoffs between <10 and <25mm. For the PTB <35 wks endpoint, statistically significant lower odds of PTB for CLs <25 mm are demonstrated and efficacy was maintained for smaller CL cutoffs. Results were similar for PTB <32 wks. For the PTB <24 wks endpoint, results differed, demonstrating that for CL cutoffs between <10 and <15mm, the ORs increased toward unity (no benefit) with wide CIs, attributed to few births <24 wks.
CONCLUSION:
Ultrasound-indicated cerclage efficacy in women with prior spontaneous PTB varies by CL action point cutoff and by PTB GA endpoint. Cerclage significantly reduces PTB <35 and <32 wks at CL cutoffs between <10mm and <25mm, reducing most for shorter CL’s and affirming that women with prior spontaneous PTB and shortened CL are appropriate candidates for ultrasound-indicated cerclage.
Keywords: cerclage, cervical length, preterm birth prediction, vaginal sonography
INTRODUCTION
Shortened cervical length (CL) is one of the most powerful biologic markers of preterm birth (PTB)1. It is most predictive when used in selected populations of high-risk gravidas, especially women with prior spontaneous PTB2. As previously demonstrated, CLs >25mm have a relatively stable and generally poor predictive value for PTB, even in high-risk women3. However, there is a very strong, inverse relationship between CLs <25mm and the risk of PTB2.
Given the continuum of increasing PTB risk as the CL shortens, clinicians and investigators have debated the “optimal” CL cutoff to recommend interventions (e.g., cerclage, progesterone). Both ≤15mm4,5 and <25mm6,7 have been utilized as action point CL cutoffs in randomized trials of cervical cerclage, a relatively expensive surgical intervention with known risks. The present analysis examines the efficacy of ultrasound-indicated cerclage for preventing PTB in high-risk women, where we consider action points along a continuum of CL cutoffs < 25mm, identified at mid-trimester ultrasound. We use data from a multicenter randomized clinical trial of ultrasound-indicated cerclage for the prevention of preterm birth in high-risk women. In the parent trial a significant benefit from cerclage placement was found in a predetermined stratified analysis of women with CL<15mm at randomization. A 15mm action point was selected primarily because this had been used in related intervention trials but without a recognized well-defined biologic justification. In this analysis, we more thoroughly examine cerclage efficacy along the continuum of cervical lengths observed at the time of randomization to cerclage or no cerclage.
METHODS
This is a planned secondary analysis of the multicenter randomized clinical trial sponsored by the Eunice Kennedy Shriver National Institute of Child Health and Human Development performed to investigate whether ultrasound-indicated cerclage can prevent recurrent PTB < 35 weeks in high-risk women. The trial protocol and primary results are summarized elsewhere7. Briefly, healthy multiparous women with singleton gestations and at least one prior spontaneous PTB between 17 and 33 6/7 weeks were screened for shortened CL<25mm between 16 0/7 and 22 6/7 weeks. Sonographic screening was scheduled every 2 weeks unless the measured CL was observed to be 25–29mm, at which point screening was scheduled weekly. Women with CL <25mm at any visit scheduled prior to 22 6/7 weeks were eligible for randomization. Exclusion criteria included fetal anomaly, planned history-indicated cerclage for a clinical diagnosis of cervical insufficiency, and maternal-fetal complications (e.g., treated chronic hypertension) that might elevate the risk of an indicated preterm birth. Between January 2003 to February 2007, 302 women at 15 U.S. clinical sites were randomized to receive McDonald cerclage or no cerclage. Gestational age (GA) at delivery was available for 301 women. Each center obtained institutional review board approval.
Preterm birth at <35, <32, and <24 weeks were the primary outcomes of interest. The efficacy of cerclage for the prevention of each primary study endpoint was investigated with logistic regression models where ultrasound-indicated cerclage placement, regardless of randomization assignment, was designated as the primary independent variable. Participants who received cerclage as per randomization assignment and crossover participants who received an ultrasound-indicated cerclage while randomized to the no-cerclage group were classified as receiving ultrasound-indicated cerclage. Participants who did not receive an ultrasound-indicated cerclage, regardless of randomization assignment, were defined as the no ultrasound-indicated cerclage group. The odds ratios for preterm birth in the ultrasound-indicated cerclage placement vs. no ultrasound-indicated cerclage placement groups were estimated and recorded. All women with known GA at delivery and cervical length <25mm at randomization were included in the data analyses. The statistical analyses were repeated for subsets of the study participants, where the sample was restricted to women with shorter CL’s (cutoffs) at randomization. That is, the odds of cerclage efficacy were estimated for women whose CL at randomization was <25mm, for those with CL<24mm, for those with CL <23mm, etc.
In a prior investigation, Mancuso et al8 identified a significant effect of both gestational age (GA) at randomization and the presence of a U-shaped funnel on cerclage efficacy. Hence, these characteristics were included as covariates in the statistical analyses described below. Additional participant characteristics were examined between patients who did and did not receive ultrasound-indicated cerclage.
For each subset of women included at each CL cutoff evaluated, we estimated 95% confidence interval (CI) bounds for the cerclage benefit by bootstrapping methods9. Briefly, a series of 300 new bootstrap analysis datasets (resamples) were created by complete case sampling, with replacement, from the data in the subset. By using complete case sampling, all patient data were retained in the resampling procedure. The sample size of each bootstrap resample was equal to the sample size of the subset and the numbers of women with and without ultrasound-indicated cerclage were the same in both the resample and the subset. Logistic regression, including the cerclage main effect and two covariates, was used to obtain an estimate of the adjusted odds ratio (OR) for each of the 300 new analysis datasets for each CL cutoff. The bootstrap 95% CI was selected as the lower 2.5th percentile and upper 97.5th percentile from the distribution of OR’s. This procedure was repeated for each subset of women where the CL cutoff of interest was systematically decreased from a starting point of <25 mm. Smoothed regression curves were superimposed on the OR point estimates to create the plots of the OR’s and CI’s derived at each cervical length cutoff. In the presence of sparse data as observed in this analysis, bootstrap regression allowed for estimating the variability in ORs for ultrasound-indicated efficacy and determining the 95% CIs.
All tests of significance were two-sided and evaluated at a 0.05 level of significance. SAS version 9.2 (SAS Institute Inc, Cary, NC) was used for all statistical analyses.
RESULTS
For this analysis, 301 women with CL <25 mm and available GA at delivery were included: 142 women who underwent ultrasound-indicated cerclage and 159 women who did not. Participant characteristics are presented in Table 1.
Table 1.
Patient Characteristics by Ultrasound-Indicated Cerclage Placement
| Characteristic | Cerclage (n=142) | No Cerclage (n=159) | P |
|---|---|---|---|
| Years of age (mean ± sd) | 26.4 ± 5.5 | 26.5 ± 5.1 | 0.91 |
| Race/ethnicity - n (%) | 0.26 | ||
| Pre-pregnancy BMI (mean ± sd) | 29.8 ± 8.2 | 29.4 ± 7.2 | 0.64 |
| Years of education (mean ± sd) | 12.0 ± 2.8 | 11.9 ± 2.4 | 0.89 |
| Cigarette use - n (%) | 23 (16%) | 31 (20%) | 0.46 |
| Any drug use - n (%) | 5 (4%) | 10 (6%) | 0.27 |
| One or more prior induced abortion - n (%) | 24 (17%) | 26 (16%) | 0.90 |
| Gestational age (wks) at randomization (mean ± sd) | 19.3 ± 1.9 | 19.5 ± 2.0 | 0.41 |
| Cervical length (mm) at randomization (mean ± sd) | 18.4 ± 6.3 | 19.7 ± 5.3 | 0.05 |
| U funnel – n (%) | 28 (20%) | 20 (13%) | 0.09 |
| Intent to use progesterone – n (%)* | 54 (40%) | 63 (41%) | 0.87 |
10 participants were randomized prior to adding this stratum to the study (6 received ultrasound-indicated cerclage; 4 did not).
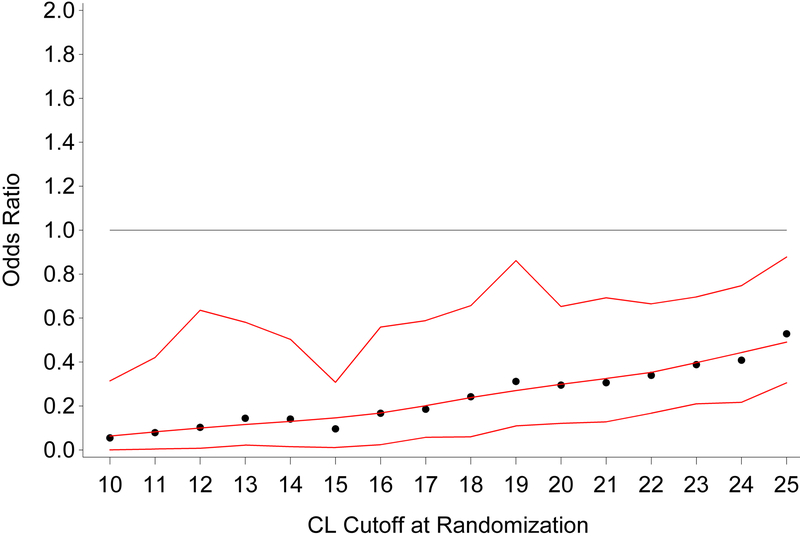
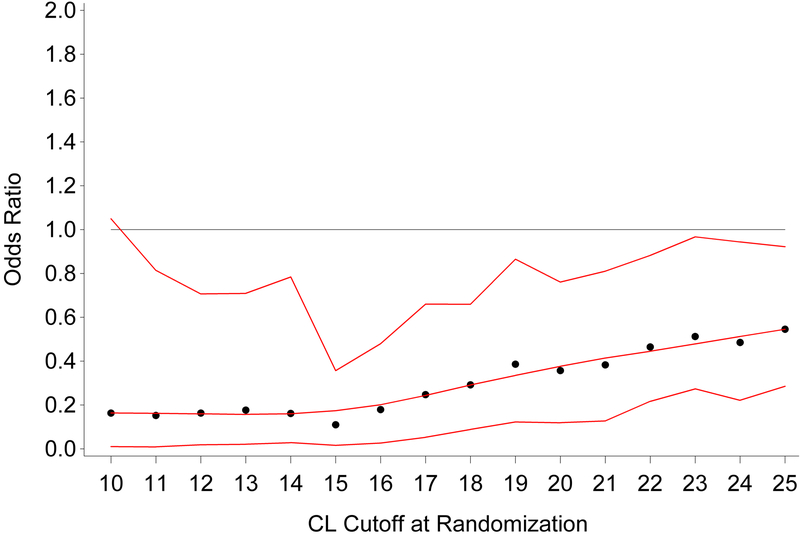
Crude rates of PTB <35 weeks and <24 weeks are presented in Table 2 and the adjusted ORs for the efficacy of ultrasound-indicated cerclage vs no ultrasound-indicated cerclage are shown in Figure 1. Figure 1 illustrates the efficacy of ultrasound-indicated cerclage (ORs < 1) for shorter CL cutoffs. The upper 95% CIs indicate a statistically significant lower odds of PTB for CL’s <25mm; however, too few cases of CL <10mm limited the analysis of cerclage efficacy as statistical modeling became unstable. Similar results are seen for the outcome of PTB<32 weeks (Figure 2), with the exception of CL <10mm where the upper bound of the 95% CI exceeds 1.0.
Table 2.
Crude Rates of Preterm Birth by Ultrasound-Indicated Cerclage Group
| Cervical Length | Preterm Birth <35 wks | Preterm Birth <24 wks | |||
|---|---|---|---|---|---|
| Cerclage | No Cerclage | Cerclage | No Cerclage | ||
| <25mm | 45/142 (32%) | 67/159 (42%) | 8/142 (6%) | 22/159 (14%) | |
| <24mm | 36/117 (31%) | 55/121 (45%) | 8/117 (7%) | 19/121 (16%) | |
| <23mm | 34/100 (34%) | 48/93 (52%) | 8/100 (8%) | 17/93 (18%) | |
| <22mm | 29/83 (35%) | 44/81 (54%) | 6/83 (7%) | 14/81 (17%) | |
| <21mm | 25/71 (35%) | 38/67 (57%) | 6/71 (8%) | 12/67 (18%) | |
| <20mm | 24/61 (39%) | 37/58 (64%) | 6/61 (10%) | 12/58 (21%) | |
| <19mm | 22/50 (44%) | 35/53 (66%) | 6/50 (12%) | 12/53 (23%) | |
| <18mm | 20/46 (43%) | 29/42 (69%) | 6/46 (13%) | 11/42 (26%) | |
| <17mm | 17/42 (40%) | 26/37 (70%) | 5/42 (12%) | 11/37 (30%) | |
| <16mm | 16/39 (41%) | 20/29 (69%) | 5/39 (13%) | 9/29 (31%) | |
| <15mm | 13/36 (36%) | 20/28 (71%) | 5/36 (14%) | 9/28 (32%) | |
| <14mm | 12/30 (40%) | 18/26 (69%) | 5/30 (17%) | 8/26 (31%) | |
| <13mm | 12/29 (41%) | 16/23 (70%) | 5/29 (17%) | 7/23 (30%) | |
| <12mm | 11/23 (48%) | 16/20 (80%) | 4/23 (17%) | 7/20 (35%) | |
| <11mm | 8/17 (47%) | 14/16 (88%) | 4/17 (24%) | 5/16 (31%) | |
| <10mm | 8/16 (50%) | 13/14 (93%) | 4/16 (25%) | 5/14 (36%) | |
Figure 1. Preterm delivery <35 weeks.
Estimated odds ratios and 95% bootstrap confidence intervals for preterm birth <35 weeks for patients receiving cerclage vs no cerclage. Odds ratios <1 indicate lower risk of preterm birth for patients receiving cerclage.
Figure 2. Preterm delivery <32 weeks.
Estimated odds ratios and 95% bootstrap confidence intervals for preterm birth <32 weeks for patients receiving cerclage vs no cerclage. Odds ratios <1 indicate lower risk of preterm birth for patients receiving cerclage.
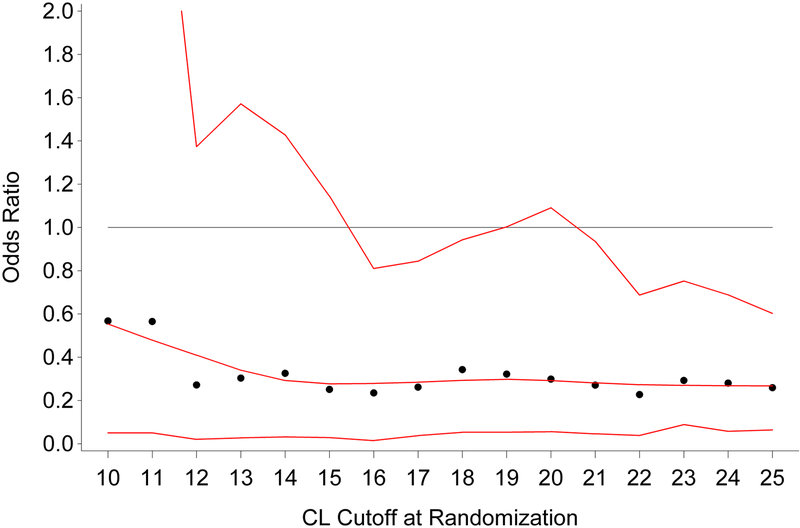
The predicted effect of varying CL cutoffs on cerclage benefit for PTB <24 weeks (raw rates in Table 2, adjusted odds ratios in Figure 3) differed as compared to the later PTB endpoints. For CL cutoffs <15 mm, the ORs increased toward unity. Conversely, the upper CIs for most CL cutoffs above 15 mm did not include 1, but CIs were generally wider in the <24 week plot than in the <35 and <32 week plots because of fewer <24 week births.
Figure 3. Preterm delivery <24 weeks.
Estimated odds ratios and 95% bootstrap confidence intervals for preterm birth <24 weeks for patients receiving cerclage vs no cerclage. Odds ratios <1 indicate lower risk of preterm birth for patients receiving cerclage.
DISCUSSION
The present analysis indicates that ultrasound-indicated cerclage efficacy for preventing recurrent PTB in a population of high-risk women varies both by the chosen CL cutoff and further by the PTB GA endpoint of interest. For PTB endpoints <32 and <35 weeks, cerclage efficacy is demonstrated for shorter CL cutoffs (95% CI completely below 1.0). There further appears to be a trend of declining adjusted OR’s for shorter CL cutoffs. However, at a PTB endpoint of <24 weeks, cerclage efficacy remains relatively constant down to a CL cutoff of <15mm, after which it appears to lose some efficacy (increasing odds ratios). The actual numbers of births <24 weeks were low in this study, and led to wide 95% confidence intervals, particularly below the <15mm cutoff. Thus, results in this range should be interpreted cautiously, and more investigation is needed to better understand the effect of cerclage for the prevention of PTB <24 weeks at CL cutoffs below 15 mm. Indeed, there are limited data examining efficacy of PTB interventions at CL cutoffs <10mm given low enrollment numbers in this range or because of planned study exclusion criteria7. Further investigation of treatment efficacy for the prevention of PTB <24 weeks at very short CL cutoffs (<10 mm) may be warranted. Given the rarity of the <24 week birth outcome and ultrasound-documented midtrimester CL<10mm in these high-risk women, the sample size and the number needed to screen for such a randomized clinical trial might be prohibitive. Nevertheless, we are reassured that cerclage has proven efficacy even at CLs of “zero”, as would be observed in cases of acute cervical insufficiency10. It is also important to realize that regardless of the chosen CL cutoff action point, the population will include some women with very shortened CLs.
This study is limited by the available data with low rates of preterm birth, particularly at very short randomization CL’s and few births <24 weeks. As a result, bootstrap regression was employed to estimate the distribution of OR’s for PTB and determine the 95% CI’s. In general, however, bootstrapping methods are not considered to be a foolproof solution to the small sample size problem. As a method that resamples from a single sample, bootstrapping relies on strong assumptions that the original sample is representative of the true population under study and that the bootstrap resamples are selected in a truly random manner. If these assumptions are not met, then one may obtain unreliable results. While our programs used random resampling procedures, we depend on the assumption that the original sample is representative of women with a shortened CL and prior preterm birth <35 wks. As our subset samples become progressively smaller for shorter CL cutoffs, this assumption may be less tenable. The low numbers also limited our ability to adjust for multiple covariates in logistic regression models, and as a result other potentially important covariates such as the intent to use (or the actual use of) progesterone7,11,12 or the rate of cervical shortening were not included in our models. Since progesterone was not systematically prescribed in the parent trial, dosing, methods of administration and uptake varied, and assessing the contribution of progesterone to cerclage efficacy is not straightforward. Despite these possible limitations, cerclage for recurrent PTB prevention is efficacious over a range of shortened CL cutoffs from <10mm to <25mm and PTB endpoints. That the effect of ultrasound-indicated cerclage appeared to diminish for preventing PTB <24 weeks at shorter CL cutoffs was unexpected and cannot be easily explained, but may be related to statistical uncertainty from the diminishing sample of women who experienced these early births. Alternatively it may identify a subset of women, some of whom are experiencing very early onset of parturition and in whom cerclage may not be beneficial or possibly even harmful.13
Although we were unable to identify a single “best” or “optimal” CL cutoff for ultrasound-indicated cerclage in high-risk women, this study affirms prior reports that cerclage is beneficial for women with prior spontaneous PTB and shortened CL<25mm at 16–24 wks gestation and further illustrates greater efficacy for preventing preterm birth <32 and <35 weeks across increasingly shorter CL cutoffs.
SOURCE OF FUNDING:
The Eunice Kennedy Shriver National Institute of Child Health and Development provided funding via grant U01 HD039939. ClinicalTrials.gov Identifier: , http://clinicaltrials.gov/show/NCT00059683
Footnotes
DISCLOSURE: The authors report no conflict of interest.
Presented in abstract form at the Annual Meeting of the Society for Maternal-Fetal Medicine, San Francisco, CA, February 7–12, 2011.
CONDENSATION: Ultrasound-indicated cerclage effectively reduces recurrent preterm birth <35, <32 and <24 weeks over a wide range of shortened cervical length action points.
REFERENCES
- 1.Prediction Spong C. and prevention of recurrent spontaneous preterm birth. Obstet Gynecol 2007;110:405–15. [DOI] [PubMed] [Google Scholar]
- 2.Owen J, Yost N, Berghella V, Thom E, Swain M, Dildy GA, Miodovnik M, Langer D, Sabai BM, McNellis D, for the National Institute of Child Health and Human Development, Maternal-Fetal Medicine Units Network. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA 2001;286:1340–8. [DOI] [PubMed] [Google Scholar]
- 3.Owen J, Szychowski JM, Hankins G, Iams JD, Sheffield JS, Perez-Delboy A, Berghella V, Wing DA, Guzman ER, for the Vaginal Ultrasound Trial Consortium. Does midtrimester cervical length ≥25mm predict preterm birth in high-risk women? Am J Obstet Gynecol 2010;203:393e1–e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hassan SS, Romero R, Maymon E, Berry SM, Blackwell SC, Treadwell MC, Tomlinson M. Does cervical cerclage prevent preterm delivery in patients with a short cervix? Am J Obstet Gynecol. 2001;184(7):1325–1331. [DOI] [PubMed] [Google Scholar]
- 5.To MS, Alfirevic Z, Heath VCF, Cicero S, Cacho AM, Williamson PR, Nicolaides KH, on behalf of the Fetal Medicine Foundation Second Trimester Screening Group. Cervical cerclage for prevention of preterm delivery in women with short cervix: randomised controlled trial. Lancet 2004;363:1849–53. [DOI] [PubMed] [Google Scholar]
- 6.Berghella V, Odibo AO, Tolosa JE. Cerclage for prevention of preterm birth in women with a short cervix found on transvaginal ultrasound examination: a randomized trial. Am J Obstet Gynecol. 2004. October; 191(4):1311–7. [DOI] [PubMed] [Google Scholar]
- 7.Owen J, Hankins G, Iams JD, Berghella V, Sheffield JS, Perez-Delboy A, Egerman RS, Wing DA, Tomlinson M, Silver R, Ramin SM, Guzman ER, Gordon M, How HY, Knudtson EJ, Szychowski JM, Cliver S, Hauth JC. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol 2009;201:375e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mancuso MS, Szychowski JM, Owen J, Hankins GD, Iams JD, Sheffield JS, Perez-Delboy A, Berghella V, Wing DA, Guzman ER, for the Vaginal Ultrasound Trial Consortium. Cervical funneling: effect on gestational length and ultrasound-indicated cerclage in high-risk women. Am J Obstet Gynecol. 2010;203(3):259–e1–5.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Efron B, Tibshirani RJ. An introduction to the bootstrap. Boca Raton, FL: CRC Press, 1998. [Google Scholar]
- 10.Althuisius SM, Dekker GA, Hummel P, van Geijn HP. Cervical incompetence prevention randomized cerclage trial: emergency cerclage with bed rest versus bed rest alone. Am J Obstet Gynecol. 2003. October;189(4):907–10. [DOI] [PubMed] [Google Scholar]
- 11.Berghella V, Figueroa D, Szychowski JM, Owen J, Hankins GD, Iams JD, Sheffield JS, Perez-Delboy A, Wing DA, Guzman ER, for the Vaginal Ultrasound Trial Consortium. 17-alpha-hydroxyprogesterone caproate for the prevention of preterm birth in women with prior preterm birth and a short cervical length. Am J Obstet Gynecol 2010;202:351.e1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Szychowski JM, Berghella V, Owen J, Hankins GD, Iams JD, Sheffield JS, Perez-Delboy A, Wing DA, Guzman ER, for the Vaginal Ultrasound Trial Consortium. Cerclage for the prevention of preterm birth in high risk women receiving intramuscular 17-alpha-hydroxyprogesterone caproate. J Matern Fetal Neonatal Med 2012;25(12):26863–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sakai M, Shiozaki A, Tabata M, Sasaki Y, Yoneda S, Arai T, Kato K, Yamakawa Y, Saito S. Evaluation of effectiveness of prophylactic cerclage of a short cervix according to interleukin-8 in cervical mucus. Am J Obstet Gynecol 2006;194:14–9. [DOI] [PubMed] [Google Scholar]