Abstract
Background:
Smoking, alcohol abuse and dual substance use represent significant public health problems and are thought to contribute to disparities in morbidity and mortality in the United States. Associations of food insecurity with these substances are poorly characterized, particularly concerning heavy alcohol consumption and dual substance use. Additionally, demographic factors may moderate these associations.
Methods:
In a cross-sectional, representative sample of Wisconsin adults (n=1,616), logistic regression was used to examine whether food insecurity was associated with cigarette smoking, heavy alcohol use and dual substance use. Interactions of food insecurity with gender, marital status and age group tested moderation by demographic factors.
Principal Findings:
Food insecurity was associated with cigarette smoking in men and women (odds ratio (OR)=3.0, 95% confidence interval (CI)=2.1-4.4); however, only among men was food insecurity associated with heavy alcohol use (OR=1.5; 95% CI=1.0-2.2) and dual substance use (OR=5.2; 95% CI=1.5-18.6). Marital status and age group did not moderate associations of food insecurity with substance use.
Conclusions:
Food insecurity was more common among those who smoke cigarettes. Heavy alcohol consumption and dual use were positively correlated with food insecurity among men, but not among women. Longitudinal analyses are needed to disentangle temporality and underlying pathways of observed associations. Additionally, future work should determine whether interventions and policies targeting food insecurity can simultaneously reduce cigarette and alcohol use.
Keywords: Social Determinants of Health, Tobacco Use, Health Disparities, Alcohol Consumption, Social Epidemiology
1. Introduction
Smoking cigarettes and heavy alcohol use are a significant public health concern in the United States. Tobacco contributes to over $300 billion a year in U.S. economic costs, and to a litany of medical morbidities as the leading cause of preventable death (Federal Trade Commission (FTC) 2019; Department of Health and Human Services (DHHS) 2014; Xu et al., 2015). Heavy and excessive alcohol use is also economically costly and implicated in greater morbidity and mortality among U.S. adults (Rehm et al., 2014; Sacks et al., 2015). Dual use of cigarettes and alcohol is particularly burdensome given an increased risk for several diseases (e.g. cirrhosis, aerodigestive tract cancers) beyond either substance alone (McKee and Weinberger 2013; Hashibe et al., 2007), and; both smoking cessation and alcohol disorder remission are more difficult among dual users (Weinberger et al., 2015; Weinberger, Gbedemah, and Goodwin 2017). Smoking cigarettes and alcohol disorders are disproportionately prevalent among those who are socially or economically disadvantaged, and subsequently represent considerable health disparities in life expectancy and mortality (Östergren et al., 2019).
Targeting food insecurity to reduce tobacco- and alcohol-related health disparities could be particularly effective. Food insecurity refers to both the physical pain of hunger as well as worrying about having enough nutritious food to eat. As a social determinant of health, food insecurity has a complex relationship with other social and economic factors at the individual- and macro-level to influence health and health behavior—including substance use (Adler, Glymour, and Fielding 2016). Physical and economic access to adequate food by all individuals at all times is declared a human right by the United Nations, emphasizing the public health obligation to address food insecurity (Committee on Economic, Social and Cultural Rights 1999). Despite having the largest economy in the world, roughly 12% of the U.S. population is food insecure, with rates particularly high among persons of color (20%) and single mothers (30%) (Coleman-Jensen et al., 2018; International Monetary Fund 2019). Food insecurity is associated with a number of negative health outcomes, including depression, poor diet quality and disordered eating—even after accounting for other indicators of socioeconomic status (Bergmans, Zivin, and Mezuk 2019; Bergmans, Palta, et al., 2018; Rasmusson et al., 2019). Prior work demonstrates that food insecurity and its health impacts can be ameliorated using food assistance programs (Nord 2010; Frongillo and Wolfe 2010; Bergmans, Berger, et al., 2018). Thus, if food insecurity is linked with cigarette and heavy alcohol use, such programs could offer a unique opportunity to concurrently address substance use.
A number of underlying pathways could link food insecurity with substance use. Smoking cigarettes and heavy alcohol consumption may be a strategy used by individuals who are food insecure to cope with the unique psychological strain of not having reliable access to food, and the stigma associated with social assistance dependence. Evidence suggests that while there is a strong desire to quit smoking among those with low-income due to health concerns, disapproval by significant others and financial burden; smoking cessation is perceived to be extremely challenging (Wiltshire et al., 2003). Individuals who have low-income express that smoking cigarettes is one of the few luxuries they can still afford (Peretti-Watel and Constance 2009). Prior work has suggested that smoking may provide a strategy for appetite suppression during times of significant food scarcity (Jo, Talmage, and Role 2002). Additionally, cigarette and alcohol purchases may deplete financial resources that would otherwise be used to purchase food, thus exacerbating food insecurity (Hernandez et al., 2017).
While food insecurity is correlated with greater severity of tobacco use, less is known when considering alcohol disorders or the dual use of tobacco and alcohol with food insecurity (Hobkirk, Krebs, and Muscat 2018; Carim-Todd, Mitchell, and Oken 2016). Additionally, evidence is limited concerning whether associations of food insecurity with cigarette and alcohol use differ across population subgroups—specifically age, gender and marital status. Overall substance use is more common among younger age groups and men (Jamal 2016; Drope et al., 2018; Linden-Carmichael et al., 2017), which may be due to greater impulsivity and higher rates of externalizing behaviors, particularly when younger persons and men in general are exposed to social stressors (Ayer et al., 2011; Corbin, Farmer, and Nolen-Hoekesma 2013). Additionally, in post hoc analyses, Bergmans (2019) observed that becoming food insecure was associated with an increase in daily cigarette consumption among older women who smoke, whereas this was not the case for men. Marriage is another factor that may moderate the association of food insecurity with substance use. Marriage as a source of social support is considered to have protective health effects, especially for men (Reczek and Umberson 2012; Umberson, Crosnoe, and Reczek 2010). For both men and women, those who are married are less likely to smoke tobacco or abuse alcohol than those who are not currently married.
This study aimed to determine associations of food insecurity with smoking cigarettes, heavy alcohol use and dual use. Additionally, we examined whether associations were moderated by age group, gender or marital status. We hypothesized that food insecurity would be associated with greater odds of smoking, heavy alcohol use and dual use—independent of other socioeconomic factors. Additionally, we hypothesized that associations of food insecurity and substance use would be stronger for younger age groups, males and unmarried persons.
2. Methods
2.1. Sample
Cross-sectional data from the Survey of the Health of Wisconsin (SHOW) collected between 2014-2016 was used. SHOW includes a randomly selected household-based sample of Wisconsin adults (aged ≥18 years) (Nieto et al., 2010). A three-stage probability-based stratified cluster sampling approach was used to select participants. County served as the primary sampling unit stratified by mortality. The secondary sampling unit was census block groups stratified by poverty and randomly selected with probability proportional to size. The tertiary sampling unit included all persons residing in randomly selected households (Survey of the Health of Wisconsin (SHOW) 2019). Since 2008, SHOW has collected information on a broad range of demographics, socioeconomic status, health history and health behaviors among Wisconsin residents. Informed consent was obtained prior to data collection via in-home interview, questionnaire and physical exam, and collection of biological samples (Nieto et al., 2010).
All SHOW protocols are approved and regulated by the University of Wisconsin, Madison Health Sciences Institutional Review Board (IRB). The University of Michigan Medical School IRB determined that secondary analysis of SHOW data for this study did not require IRB approval. Among the 1,758 adults who participated in SHOW 2014-2016, 1,616 (92%) had complete case data for all variables of interest.
2.2. Measures
Smoking—
To identify current smokers, two self-report survey items were used. Respondents were asked ‘Have you smoked 100 or more cigarettes in your entire life?’ and ‘Do you smoke cigarettes now?’ Those who responded ‘yes’ to both of these items were considered current smokers, those who did not respond ‘yes’ were considered either former or never smokers and served as the reference group.
Heavy Alcohol Use—
Men who reported consuming >14 drinks/week and women who reported consuming >7 drinks/week were considered to meet criteria for heavy alcohol use, which is consistent with gender-specific risk of developing alcohol use disorder as defined by the National Institute for Alcohol Abuse and Alcoholism (“Drinking Levels Defined ∣ National Institute on Alcohol Abuse and Alcoholism (NIAAA)” n.d.). Those who drank less than these cut points were not considered to meet criteria for heavy alcohol use and served as the reference group.
Dual Substance Use—
Those who were both current smokers and met criteria for heavy alcohol use were considered to meet criteria for dual substance use. All others were considered to have none or single substance use and served as the reference group.
Food Insecurity—
Three survey items were used to create a binary indicator of food insecurity, (1) “(I We worried whether (my our) food would run out before (I/We) got money to buy more”, (2) “The food that (I/we) bought just didn't last, and (I/we) didn't have money to get more” and (3) “(I/We) could not afford to eat balanced meals”. Those who responded that any of these statements was “often true” or “sometimes true” over the previous 12 months were considered food insecure. Those who responded that all three statements were “never true” over the previous 12 months were considered not food insecure and served as the reference group. This criterion was based on the United States Department of Agriculture 6-item Short Form Food Security Module (“U.S. Household Food Security Survey Module: Six-Item Short Form” 2012), which is an international standard for identifying food insecurity.
Covariates—
A number of demographic and socioeconomic covariates were included in analyses due to their potential to confound associations between food insecurity and substance use. Demographic covariates included age group (18 to <35 [reference group], 35 to <50, 50 to <65, ≥65), race/ethnicity (non-Hispanic White [reference group], non-Hispanic Black, other race/ethnicity or multiracial), marital status (married [reference group], single or living with partner, divorced or separated or widowed) and gender (male [reference group], female). Socioeconomic covariates included income-to-poverty ratio (continuous measure) estimated based on total household income and number of individuals in the home compared to federal poverty estimates provided by the Wisconsin Department of Health Services (Levy 2008), educational attainment (treated as a continuous measure across 5 categories: <high school degree, high school degree or equivalent, some college, associate’s degree, bachelor’s degree or above), and employment status (employed [reference group], unemployed, other).
2.3. Statistical Analysis
All analyses were conducted using SAS version 9.4 (SAS Institute Inc. 2013, 4). Survey procedures were employed to account for SHOW’S complex sampling design. First, χ2 and F tests compared sample characteristics by food insecurity status. Next three separate logistic regression models were used to examine associations of food insecurity with current smoking status, heavy alcohol consumption and dual use. Fully adjusted models accounted for age category, gender, race, marital status, education attainment, household income-to-poverty ratio and employment status. Finally, moderation by demographic factors (i.e. marital status, age group and gender) with food insecurity were tested separately as interactions in fully adjusted models.
3. Results
There were 1,616 adults age 18 and over in the analytic sample. Of these, 24% were food insecure (n=382), 13% currently smoked cigarettes (n=216), 14% reported heavy consumption of alcohol (n=220), and 3% reported dual substance use (n=45). Table 1 shows sample characteristics by food insecurity status. A larger proportion of self-identified non-Hispanic Blacks were food insecure compared to non-Hispanic Whites (14% vs 4%). People who were food insecure were also more likely to be single or living with a partner than married (40% vs. 17%). Those who were food insecure also had lower socioeconomic status. Household income-to-poverty ratio (PIR) was 2.0 (95% confidence interval (CI)= 1.7, 2.3) among those who were food insecure compared to 4.4 (95% CI=4.0, 4.7) among those who were food secure. Additionally, food insecurity was more common among those with less than a high school degree (9% vs. 4% of those food secure) and those who were unemployed (10% vs. 3% of those food secure).
Table 1.
| Food Insecure | |||
|---|---|---|---|
| No | Yes | ||
| Characteristics | n= 1,234 | n= 382 | P valuec |
| Age Category | <0.001 | ||
| 18 to <35 years | 188 (19.5) | 136 (42.1) | |
| 35 to <50 | 251 (24.2) | 109 (28.8) | |
| 50 to <65 | 394 (33.1) | 89 (21.5) | |
| ≥65 | 401 (23.3) | 48 (7.6) | |
| Female | 665 (48.4) | 235 (55.9) | 0.082 |
| Race/Ethnicity | <0.001 | ||
| Non-Hispanic White | 1,103 (89.3) | 273 (72.9) | |
| Non-Hispanic Black | 37 (2.9) | 59 (13.8) | |
| Other Race or Multiracial | 94 (7.8) | 50 (13.3) | |
| Marital Status | <0.001 | ||
| Married | 863 (68.2) | 158 (40.8) | |
| Divorced, Separated or Widowed | 205 (14.3) | 85 (19.3) | |
| Single or Living with Partner | 166 (17.4) | 139 (39.9) | |
| Educational Attainment | <0.001 | ||
| <High School Degree | 50 (4.1) | 38 (9.1) | |
| High School Degree or Equivalent | 202 (16.5) | 98 (27.2) | |
| Some College | 212 (17.3) | 92 (26.2) | |
| Associates Degree | 202 (16.9) | 77 (18.2) | |
| Bachelor's Degree or Above | 568 (45.2) | 77 (19.4) | |
| Household income-to-poverty ratio, mean (95% CI) | 4.4 (4.0, 4.7) | 2.0 (1.7, 2.3) | <0.001 |
| Employment Status | <0.001 | ||
| Employed | 712 (63.7) | 221 (61.5) | |
| Unemployed | 28 (3.0) | 37 (10.0) | |
| Not Working and Not Seeking Employment | 494 (33.3) | 124 (28.5) | |
| Currently Smoke Cigarettes | 94 (8.4) | 122 (33.6) | <0.001 |
| Heavy Alcohol Consumptiond | 161 (12.9) | 59 (16.8) | 0.133 |
| Dual Substance Usee | 19 (1.6) | 26 (8.0) | 0.007 |
Survey of the Health of Wisconsin
Cell values represent column percentages
X2 or F test
Men who reported consuming >14 drinks/week and women who reported consuming >7 drinks/week were considered to meet criteria for heavy alcohol use
Currently Smoke Cigarettes and Heavy Alcohol Consumption
Table 2 shows odds ratios (OR’s) and 95% CI’s for the association of food insecurity with current smoking status. Smoking was more common among individuals who were food insecure. Those who were food insecure had a 5.5 (95% CI=4.2, 7.3) times higher odds of currently smoking cigarettes. In fully adjusted models this association remained but was diminished (OR=3.0; 95% CI=2.1, 4.4). A number of covariates were also associated with current smoking status. Those who were ≥65 had a 0.4 (95% CI=0.2, 0.9) times lower odds of currently smoking cigarettes than those 18 to <35. Women had a 0.6 (95% CI=0.5, 0.9) times lower odds of currently smoking cigarettes. The odds of current smoking was greater for those who were divorced, separated, or widowed (OR=2.5; 95% CI=1.8, 3.4) than those who were married. Greater educational attainment (OR=0.6; 95% CI=0.5, 0.7) and household income (OR=0.8; 95% CI=0.7, 0.9) were inversely associated with current smoking status.
Table 2.
Odds ratios (OR's) and 95% confidence intervals (CI's) for currently smoking cigarettes among Wisconsin adults, SHOWa 2014-2016-b.
| Crude | Adjusted | |||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Food Insecure (ref=no) | 5.5 (4.2, 7.3) | <0.001 | 3.0 (2.1, 4.4) | <0.001 |
| Age Category (ref=18 to <35) | <0.001 | |||
| 35 to <50 | -- | 1.5 (1.0, 2.3) | ||
| 50 to <65 | -- | 1.9 (1.0, 3.6) | ||
| ≥65 | -- | 0.4 (0.2, 0.9) | ||
| Female (ref=male) | -- | 0.6 (0.5, 0.9) | 0.016 | |
| Race/Ethnicity (ref=non-Hispanic White) | 0.31 | |||
| Non-Hispanic Black | -- | 1.0 (0.4, 2.3) | ||
| Other Race or Multiracial | -- | 1.6 (0.9, 2.9) | ||
| Marital Status (ref=married) | <0.001 | |||
| Divorced, Separated or Widowed | -- | 2.5 (1.8, 3.4) | ||
| Single or Living with Partner | -- | 1.4 (0.7, 2.9) | ||
| Educational Attainment | -- | 0.6 (0.5, 0.7) | <0.001 | |
| Household income-to-poverty ratio, mean (95% CI) | -- | 0.8 (0.7, 0.9) | 0.005 | |
| Employment Status (ref=employed) | 0.12 | |||
| Unemployed | -- | 1.2 (0.7, 2.1) | ||
| Not Working and Not Seeking Employment | -- | 0.7 (0.5, 1.0) | ||
Survey of the Health of Wisconsin
n=1,616
Table 3 shows ORs and 95% CIs for the association of food insecurity with heavy alcohol use. In the adjusted model, food insecurity was not associated with heavy alcohol consumption (OR=1.3; 95% CI=0.9, 1.8). However, a number of covariates were associated with heavy alcohol consumption, including age, gender, marital status and employment. Those who were 35 to <50 years of age had a 1.4 (95% CI=1.0, 2.1) times higher odds of heavy alcohol consumption than those 18 to <35. Women had a 1.5 (95% CI=1.1, 2.1) times higher odds of heavy alcohol consumption compared to men. The odds of currently smoking was greater for those who were single or living with a partner (OR=1.8; 95% CI=1.3, 2.6) than those who were married.
Table 3.
Odds ratios (OR's) and 95% confidence intervals (CI's) for heavy alcohol consumptiona among Wisconsin adults, SHOWb 2014-2016c.
| Crude | Adjusted | |||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Food Insecure (ref=no) | 1.4 (1.0, 2.0) | 0.09 | 1.3 (0.9, 1.8) | 0.16 |
| Age Category (ref=18 to <35) | 0.024 | |||
| 35 to <50 | -- | 1.4 (1.0, 2.1) | ||
| 50 to <65 | -- | 1.3 (0.9, 2.0) | ||
| ≥65 | -- | 0.9 (0.4, 1.8) | ||
| Female (ref=male) | -- | 1.5 (1.1, 2.1) | 0.014 | |
| Race/Ethnicity (ref=non-Hispanic White) | 0.30 | |||
| Non-Hispanic Black | -- | 0.7 (0.3, 1.3) | ||
| Other Race or Multiracial | -- | 1.1 (0.4, 2.6) | ||
| Marital Status (ref=married) | 0.004 | |||
| Divorced, Separated or Widowed | -- | 1.2 (0.6, 2.3) | ||
| Single or Living with Partner | -- | 1.8 (1.3, 2.6) | ||
| Educational Attainment | -- | 1.0 (1.0, 1.1) | 0.35 | |
| Household income-to-poverty ratio, mean (95% CI) | -- | 1.0 (0.9, 1.1) | 0.52 | |
| Employment Status (ref=employed) | 0.047 | |||
| Unemployed | -- | 1.5 (1.0, 2.3) | ||
| Not Working and Not Seeking Employment | -- | 0.9 (0.5, 1.6) | ||
Men who reported consuming >14 drinks/week and women who reported consuming >7 drinks/week were considered to meet criteria for heavy alcohol use
Survey of the Health of Wisconsin
n=1,616
Table 4 shows ORs and 95% CIs for the association of food insecurity with dual substance use. Dual substance use was more common among those who were food insecure. In adjusted analyses, food insecure individuals had a 5.4 (95% CI=2.1, 13.7) times higher odds of dual substance use compared to those who were food secure. Significant associations remained in fully adjusted models but was attenuated (OR=2.8; 95% CI=1.3, 6.1). Age and educational attainment were also associated with dual substance use after adjusting for all other covariates. Those who were 35 to <50 had a 3.6 (95% CI=2.0, 6.4) times higher odds of dual substance use than those 18 to <35 in adjusted models and dual substance use was lower among individuals with greater educational attainment (OR=0.8; 95% CI=0.7, 1.0).
Table 4.
Odds ratios (OR's) and 95% confidence intervals (CI's) for dual substance usea among Wisconsin adults, SHOWb 2014-2016c.
| Crude | Adjusted | |||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Food Insecure (ref=no) | 5.4 (2.1, 13.7) | 0.001 | 2.8 (1.3, 6.1) | 0.011 |
| Age Category (ref=18 to <35) | <0.001 | |||
| 35 to <50 | -- | 3.6 (2.0, 6.4) | ||
| 50 to <65 | -- | 1.2 (0.4, 4.0) | ||
| ≥65 | -- | 1.3 (0.3, 5.6) | ||
| Female (ref=male) | -- | 1.0 (0.6, 1.8) | 0.99 | |
| Race/Ethnicity (ref=non-Hispanic White) | 0.94 | |||
| Non-Hispanic Black | -- | 1.1 (0.3, 4.0) | ||
| Other Race or Multiracial | -- | 1.3 (0.3, 4.6) | ||
| Marital Status (ref=married) | 0.46 | |||
| Divorced, Separated or Widowed | -- | 2.5 (0.5, 11.3) | ||
| Single or Living with Partner | -- | 2.1 (0.4, 11.8) | ||
| Educational Attainment | -- | 0.8 (0.7, 1.0) | 0.018 | |
| Household income-to-poverty ratio, mean (95% CI) | -- | 0.9 (0.6, 1.1) | 0.26 | |
| Employment Status (ref=employed) | 0.13 | |||
| Unemployed | 1.2 (0.5, 3.1) | |||
| Not Working and Not Seeking Employment | -- | 0.6 (0.3, 1.1) | ||
Those who reported that they currently smoked cigarettes and had heavy alcohol consumption (i.e. men who reported consuming >14 drinks/week and women who reported consuming >7 drinks/week were considered to meet criteria for heavy alcohol use)
Survey of the Health of Wisconsin
n=1,616
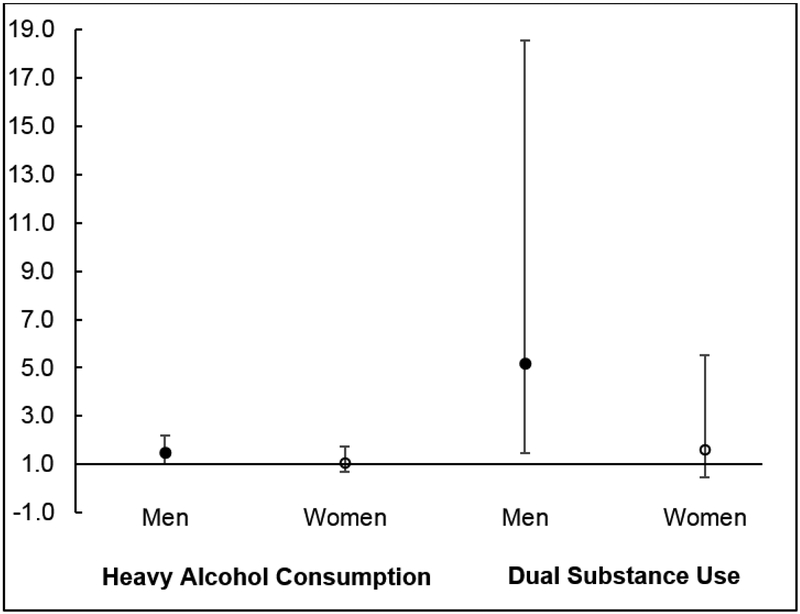
When testing moderation of associations by demographic factors, interactions with food insecurity were not observed for marital status or age (α=0.05; data not shown). However, gender did moderate the relationship of food insecurity with heavy alcohol consumption (p-value=0.012) and dual substance use (p-value=0.001). Figure 1 shows associations of food insecurity with heavy alcohol consumption and dual substance use, stratified by gender. Among men, food insecurity was associated with a 1.5 (95% CI=1.0, 2.2) times higher odds of heavy alcohol consumption; however, food insecurity was not associated with heavy alcohol consumption among women (OR=1.1; 95% CI=0.7, 1.8). Similarly, food insecurity was associated with a higher odds of dual substance use among men (OR=5.2; 95% CI=1.5, 18.6); however, this was not the case for women (OR=1.6; 95% CI=0.5, 5.5).
Figure 1.
Odds ratios and 95% confidence intervals for the association of food insecurity with heavy alcohol consumptiona and dual substance useb, stratified by genderc-e.
aMen who reported consuming >14 drinks/week and women who reported consuming >7 drinks/week were considered to meet criteria for heavy alcohol use
bCurrently Smoke Cigarettes and Heavy Alcohol Consumption
cData come from the Survey of the Health of Wisconsin (SHOW), 2014-2015; n=1,616.
dOdds ratios are adjusted for age group, race/ethnicity, marital status, educational attainment, household income-to-poverty ratio and employment status.
ep-value for interaction of gender and food insecurity when modeling odds of heavy alcohol consumption = 0.012; p-value for interaction of gender and food insecurity when modeling odds of dual substance use = 0.001
4. Discussion
This study determined associations of food insecurity with smoking cigarettes and heavy alcohol use among Wisconsin adults, independent of other socioeconomic factors. Findings demonstrated that smoking cigarettes was more common among those who were food insecure. Additionally, food insecurity was associated with heavy alcohol use and dual substance use among men, but not among women. These findings, when taken into consideration with prior evidence, demonstrate that food insecurity and substance use are highly correlated. Observed differences in the associations by gender suggest another layer of complexity. More work is needed to disentangle the temporality of these associations and identify strategies that best address their co-occurrence.
Our observation that smoking cigarettes is more common among Wisconsin adults who are food insecure replicates previous findings in diverse cross-sectional data sources. This includes a nationally-representative sample of U.S. adults (Farrelly and Shafer 2017) and within U.S. Latinos (Iglesias-Rios et al., 2015). Associations of food insecurity and smoking has also been observed in communities outside the U.S. (Semba et al., 2011).
Longitudinal analyses are necessary to test temporality of associations between food insecurity and cigarette smoking. Work thus far is inconsistent but demonstrates a reciprocal relationship. One longitudinal study spanning the Great Recession observed that those who did not smoke in 2003 and became food insecure in 2015 were more likely to initiate cigarette use than those who did not become food insecure and; those who smoked at baseline were less likely to stop smoking if they became food insecure (Kim-Mozeleski et al., 2019). Conversely, longitudinal data following the Great Recession in a cohort of older Americans indicated that becoming food insecure was associated with greater smoking cessation—potentially as a coping strategy in response to financial constraint (Bergmans 2019). When testing the influence of cigarette consumption on food insecurity, longitudinal analysis of U.S. data suggested that the added expense associated with smoking cigarettes may prolong recovery from food insecurity (Hernandez et al., 2017). In sum, future analyses testing associations of food insecurity with smoking behavior should consider potential moderation by macroeconomic factors. Additionally, the underlying pathways by which food insecurity would increase cigarette consumption are not well established and require further investigation.
Our finding that the association of food insecurity with cigarette smoking was consistent, regardless of age, gender or marital status is a novel contribution. Moderation of associations between food insecurity and tobacco use is largely understudied. A study by Mayer and colleagues (2019) also observed a lack of moderation by age, gender or marital status using data from a nationally representative sample of U.S. adults. A lack of moderation by demographic factors would suggest that the pathways connecting food insecurity and cigarette use are similar across demographic factors and could be leveraged to benefit multiple subgroups simultaneously. In contrast, post hoc analyses by Bergmans (2019) demonstrated that becoming food insecure was associated with an increase in daily cigarette consumption among women but not among men, which indicates more research using longitudinal data is needed.
The observation that food insecurity was associated with heavy alcohol consumption and dual use among men, but not women, is another novel contribution of this study. Perhaps the experience of food insecurity is unique among men such that it increases the risk of heavy alcohol consumption and dual substance use. For example, some evidence suggests that men are more sensitive to the broader social implications of food insecurity than women (Perkins et al., 2018). However, associations of food insecurity with alcohol use and dual use among men may be bidirectional, and reverse causation cannot be ruled out. For example, men have a greater shared genetic vulnerability to alcohol use disorder and disordered gambling than women, which was not accounted for in our analyses (Slutske et al., 2013). Therefore, it is possible that there are behaviors unique to men who excessively consume alcohol, such as disordered gambling, that also increase the risk of food insecurity. Overall associations of food insecurity with alcohol use are not well understood and require further study.
Findings demonstrated that food insecurity was associated with prevalence of smoking cigarettes among both men and women, and heavy alcohol use and dual use among men. Regardless of directionality, these associations could inform public health interventions. For example, it is possible that addressing both food insecurity and substance use concurrently is more effective that trying to ameliorate either alone. Additionally, failing to acknowledge food insecurity within the context of substance use interventions could render them less effective for participants who are food insecure, or vice versa.
4.1. Strengths and Limitations
This study determined associations of food insecurity with smoking cigarettes, heavy alcohol consumption and dual use. Additionally, we tested moderation by age, gender and marital status. Data came from a large, statewide representative sample of adults living in Wisconsin—an upper Midwestern state with both urban and rural residents with diverse socioeconomic status. However, findings should be considered in light of several limitations.
First, the use of cross-sectional data prevents drawing causal conclusions or testing temporality of associations. Second, tobacco use was restricted to cigarette smoking, thus; future analyses should consider the changing landscape of nicotine use as e-cigarettes become increasingly common. Finally, future research should determine whether analyses concerning heavy alcohol use, dual use and moderation by gender can be replicated in other data sources.
5. Conclusions
This study extends current understanding regarding the relationship of food insecurity with substance use—particularly linkages of food insecurity with heavy alcohol use and dual use among men. Findings indicated that smoking cigarettes was more common among those who were food insecure than those who were not food insecure. Additionally, when testing moderation by gender, heavy alcohol consumption and dual use were positively correlated with food insecurity among men, but not among women. Longitudinal analyses are needed to disentangle temporality and underlying pathways of observed associations. Additionally, future work should determine whether interventions and policies targeting food insecurity can simultaneously reduce cigarette and alcohol use.
Highlights.
Associations of food insecurity with smoking, heavy alcohol use, dual use tested.
Effect modification by gender, marital status and age group were also examined.
Data came from a cross-sectional, representative sample of Wisconsin adults.
Food insecurity was associated with smoking.
Food insecurity associated with heavy alcohol use and dual use in men but not women.
Acknowledgements
RSB and TW are supported by the National Institute of Mental Health (T32-MH73553). LC is supported by the National Institute on Alcohol Abuse and Alcoholism (T32-AA007477).
Footnotes
Role of Funding Source
Nothing declared.
Conflict of Interest
None declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adler Nancy E., Maria Glymour M, and Fielding Jonathan. 2016. “Addressing Social Determinants of Health and Health Inequalities.” JAMA 316 (16): 1641–42. 10.1001/jama.2016.14058. [DOI] [PubMed] [Google Scholar]
- Ayer Lynsay A., Harder Valerie S., Rose Gail L., and Helzer John E.. 2011. “Drinking and Stress: An Examination of Sex and Stressor Differences Using IVR-Based Daily Data.” Drug and Alcohol Dependence 115 (3): 205–12. 10.1016/j.drugalcdep.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmans Rachel S. 2019. “Food Insecurity Transitions and Smoking Behavior among Older Adults Who Smoke.” Preventive Medicine 126 (July): 105784 10.1016/j.ypmed.2019.105784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmans Rachel S., Berger Lawrence M., Palta Mari, Robert Stephanie A., Ehrenthal Deborah B., and Malecki Kristen. 2018. “Participation in the Supplemental Nutrition Assistance Program and Maternal Depressive Symptoms: Moderation by Program Perception.” Social Science & Medicine 197 (January): 1–8. 10.1016/j.socscimed.2017.11.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmans Rachel S., Palta Mari, Robert Stephanie A., Berger Lawrence M., Ehrenthal Deborah B., and Malecki Kristen. 2018. “Associations between Food Security Status and Dietary Inflammatory Potential within Lower-Income Adults from the United States National Health and Nutrition Examination Survey (NHANES), Cycles 2007 to 2014.” Journal of the Academy of Nutrition and Dietetics 118 (6): 994–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmans Rachel S., Zivin Kara, and Mezuk Briana. 2019. “Depression, Food Insecurity and Diabetic Morbidity: Evidence from the Health and Retirement Study.” Journal of Psychosomatic Research 117 (February): 22–29. 10.1016/j.jpsychores.2018.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carim-Todd Laura, Mitchell Suzanne H., and Oken Barry S.. 2016. “Impulsivity and Stress Response in Nondependent Smokers (Tobacco Chippers) in Comparison to Heavy Smokers and Nonsmokers.” Nicotine & Tobacco Research 18 (5): 547–56. 10.1093/ntr/ntv210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman-Jensen A, Rabbitt Matthew P, Gregory Christian A, and Singh Anita. 2018. “Household Food Security in the United States in 2017.” ERR-256. U.S. Department of Agriculture, Economic Research Service. [Google Scholar]
- Committee on Economic, Social and Cultural Rights. 1999. “General Comment 12 (Twentieth Session, 1999): The Right to Adequate Food (Art. 11).” Substantive Issues Arising in the Implementation of the International Covenant on Economic, Social and Cultural Rights. Geneva, Switzerland: United Nations, Economic and Social Council. [Google Scholar]
- Corbin William R., Farmer Nicole M., and Nolen-Hoekesma Susan. 2013. “Relations among Stress, Coping Strategies, Coping Motives, Alcohol Consumption and Related Problems: A Mediated Moderation Model.” Addictive Behaviors 38 (4): 1912–19. 10.1016/j.addbeh.2012.12.005. [DOI] [PubMed] [Google Scholar]
- DHHS, US. 2014. “The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General.” Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 17. [Google Scholar]
- “Drinking Levels Defined ∣ National Institute on Alcohol Abuse and Alcoholism (NIAAA).” n.d. Accessed March 22, 2019 https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking. [Google Scholar]
- Drope Jeffrey, Liber Alex C., Cahn Zachary, Stoklosa Michal, Kennedy Rosemary, Douglas Clifford E., Henson Rosemarie, and Drope Jacqui. 2018. “Who’s Still Smoking? Disparities in Adult Cigarette Smoking Prevalence in the United States.” CA: A Cancer Journal for Clinicians 68 (2): 106–15. 10.3322/caac.21444. [DOI] [PubMed] [Google Scholar]
- Farrelly Matthew C., and Shafer Paul R.. 2017. “Comparing Trends Between Food Insecurity and Cigarette Smoking Among Adults in the United States, 1998 to 2011.” American Journal of Health Promotion 31 (5): 413–416. [DOI] [PubMed] [Google Scholar]
- Federal Trade Commission (FTC). 2019. “Federal Trade Commission Cigarette Report for 2017 and Federal Trade Commission Smokeless Tobacco Report for 2017.”
- Frongillo Edward A, and Wolfe Wendy S. 2010. “Impact of Participation in Home-Delivered Meals on Nutrient Intake, Dietary Patterns, and Food Insecurity of Older Persons in New York State.” Journal of Nutrition For the Elderly 29 (3): 293–310. 10.1080/01639366.2010.499094. [DOI] [PubMed] [Google Scholar]
- Hashibe Mia, Brennan Paul, Benhamou Simone, Castellsague Xavier, Chen Chu, Maria Paula Curado Luigino Dal Maso, Daudt Alexander W., Fabianova Eleonora, and Wünsch-Filho Victor. 2007. “Alcohol Drinking in Never Users of Tobacco, Cigarette Smoking in Never Drinkers, and the Risk of Head and Neck Cancer: Pooled Analysis in the International Head and Neck Cancer Epidemiology Consortium.” Journal of the National Cancer Institute 99 (10): 777–789. [DOI] [PubMed] [Google Scholar]
- Hernandez Daphne C., Reesor Layton, Reitzel Lorraine R., Businelle Michael S., Wetter David W., and Kendzor Darla E.. 2017. “Smoking, Financial Strain, and Food Insecurity.” Health Behavior and Policy Review 4 (2): 182–188. [Google Scholar]
- Hobkirk Andréa L., Krebs Nicolle M., and Muscat Joshua E.. 2018. “Income as a Moderator of Psychological Stress and Nicotine Dependence among Adult Smokers.” Addictive Behaviors 84: 215–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iglesias-Rios Lisbeth, Bromberg Julie E., Moser Richard P., and Augustson Erik M.. 2015. “Food Insecurity, Cigarette Smoking, and Acculturation among Latinos: Data from NHANES 1999–2008.” Journal of Immigrant and Minority Health 17 (2): 349–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Monetary Fund. 2019. “World Economic Outlook, July 2019” World Economic Outlook Reports. Washington, D.C. [Google Scholar]
- Jamal Ahmed. 2016. “Current Cigarette Smoking among Adults—United States, 2005–2015.” MMWR. Morbidity and Mortality Weekly Report 65. [DOI] [PubMed] [Google Scholar]
- Jo Young-Hwan, Talmage David A., and Role Lorna W.. 2002. “Nicotinic Receptor-Mediated Effects on Appetite and Food Intake.” Journal of Neurobiology 53 (4): 618–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Mozeleski Jin E., Seligman Hilary K., Yen Irene H., Shaw Susan J., Buchanan David R., and Tsoh Janice Y.. 2019. “Changes in Food Insecurity and Smoking Status over Time: Analysis of the 2003 and 2015 Panel Study of Income Dynamics.” American Journal of Health Promotion 33 (5): 698–707. 10.1177/0890117118814397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy Christopher J. 2008. “Federal Poverty Level” In Encyclopedia of Aging and Public Health, edited by Loue Sana JD and Sajatovic Martha, 356–358. http://link.springer.com/content/pdf/10.1007/978-0-387-33754-8_176.pdf. [Google Scholar]
- Linden-Carmichael Ashley N., Lanza Stephanie T., Dziak John J., and Bray Bethany C.. 2017. “Contemporary Alcohol Use Patterns among a National Sample of U.S. Adult Drinkers.” Journal of Addictive Diseases 36 (4): 222–26. 10.1080/10550887.2017.1338816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer Margaret, Gueorguieva Ralitza, Ma Xiaomei, and White Marney A.. 2019. “Tobacco Use Increases Risk of Food Insecurity: An Analysis of Continuous NHANES Data from 1999 to 2014.” Preventive Medicine 126 (September): 105765 10.1016/j.ypmed.2019.105765. [DOI] [PubMed] [Google Scholar]
- McKee Sherry A., and Weinberger Andrea H.. 2013. “How Can We Use Our Knowledge of Alcohol-Tobacco Interactions to Reduce Alcohol Use?” Annual Review of Clinical Psychology 9: 649–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieto F. Javier, Peppard Paul E., Engelman Corinne D., McElroy Jane A., Galvao Loren W., Friedman Elliot M., Bersch Andrew J., and Malecki Kristen C.. 2010. “The Survey of the Health of Wisconsin (SHOW), a Novel Infrastructure for Population Health Research: Rationale and Methods.” BMC Public Health 10: 785 10.1186/1471-2458-10-785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nord Mark. 2010. Does SNAP Decrease Food Insecurity?: Untangling the Self-Selection Effect. DIANE Publishing. [Google Scholar]
- Östergren Olof, Martikainen Pekka, Tarkiainen Lasse, Elstad Jon Ivar, and Brønnum-Hansen Henrik. 2019. “Contribution of Smoking and Alcohol Consumption to Income Differences in Life Expectancy: Evidence Using Danish, Finnish, Norwegian and Swedish Register Data.” J Epidemiol Community Health 73 (4): 334–39. 10.1136/jech-2018-211640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peretti-Watel Patrick, and Constance Jean. 2009. “It’s All We Got Left’. Why Poor Smokers Are Less Sensitive to Cigarette Price Increases.” International Journal of Environmental Research and Public Health 6 (2): 608–21. 10.3390/ijerph6020608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins Jessica M., Nyakato Viola N., Kakuhikire Bernard, Tsai Alexander C., Subramanian SV, Bangsberg David R., and Christakis Nicholas A.. 2018. “Food Insecurity, Social Networks and Symptoms of Depression among Men and Women in Rural Uganda: A Cross-Sectional, Population-Based Study.” Public Health Nutrition 21 (5): 838–48. 10.1017/S1368980017002154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmusson Grace, Lydecker Janet A., Coffino Jaime A., White Marney A., and Grilo Carlos M.. 2019. “Household Food Insecurity Is Associated with Binge-Eating Disorder and Obesity.” International Journal of Eating Disorders 52 (1): 28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reczek Corinne, and Umberson Debra. 2012. “Gender, Health Behavior, and Intimate Relationships: Lesbian, Gay, and Straight Contexts.” Social Science & Medicine (1982) 74 (11): 1783–90. 10.1016/j.socscimed.2011.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm Jürgen, Dawson Deborah, Frick Ulrich, Gmel Gerrit, Roerecke Michael, Shield Kevin D., and Grant Bridget. 2014. “Burden of Disease Associated with Alcohol Use Disorders in the United States.” Alcoholism: Clinical and Experimental Research 38 (4): 1068–77. 10.1111/acer.12331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks Jeffrey J., Gonzales Katherine R., Bouchery Ellen E., Tomedi Laura E., and Brewer Robert D.. 2015. “2010 National and State Costs of Excessive Alcohol Consumption.” American Journal of Preventive Medicine 49 (5): e73–e79. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. 2013. “SAS Software Verrsion 9.4.” Cary, NC, USA: SAS Institute Inc. [Google Scholar]
- Semba Richard D., Campbell Ashley A., Sun Kai, Saskia de Pee Nasima Akhter, Regina Moench-Pfanner Jee Hyun Rah, Badham Jane, Kraemer Klaus, and Bloem Martin W.. 2011. “Paternal Smoking Is Associated with Greater Food Insecurity among Poor Families in Rural Indonesia.” Asia Pacific Journal of Clinical Nutrition 20 (4): 618–23. [PubMed] [Google Scholar]
- Slutske Wendy S., Ellingson Jarrod M., Richmond-Rakerd Leah S., Zhu Gu, and Martin Nicholas G.. 2013. “Shared Genetic Vulnerability for Disordered Gambling and Alcohol Use Disorder in Men and Women: Evidence from a National Community-Based Australian Twin Study.” Twin Research and Human Genetics 16 (2): 525–34. 10.1017/thg.2013.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Survey of the Health of Wisconsin (SHOW). 2019. “Survey Overview: Sampling Strategy and Recruitment.” UW School of Medicine and Public Health. 2019. https://www.med.wisc.edu/show/survey-overview/. [Google Scholar]
- Umberson Debra, Crosnoe Robert, and Reczek Corinne. 2010. “Social Relationships and Health Behavior Across Life Course.” Annual Review of Sociology 36 (August): 139–57. 10.1146/annurev-soc-070308-120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- “U.S. Household Food Security Survey Module: Six-Item Short Form.” 2012. Economic Research Service, USDA. http://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/survey-tools/. [Google Scholar]
- Weinberger Andrea H., Gbedemah Misato, and Goodwin Renee D.. 2017. “Cigarette Smoking Quit Rates among Adults with and without Alcohol Use Disorders and Heavy Alcohol Use, 2002–2015: A Representative Sample of the United States Population.” Drug and Alcohol Dependence 180 (November): 204–7. 10.1016/j.drugalcdep.2017.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger Andrea H., Platt Jonathan, Jiang Bianca, and Goodwin Renee D.. 2015. “Cigarette Smoking and Risk of Alcohol Use Relapse Among Adults in Recovery from Alcohol Use Disorders.” Alcoholism: Clinical and Experimental Research 39 (10): 1989–96. 10.1111/acer.12840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiltshire Susan, Bancroft Angus, Parry Odette, and Amos Amanda. 2003. “I Came Back Here and Started Smoking Again’: Perceptions and Experiences of Quitting among Disadvantaged Smokers.” Health Education Research 18 (3): 292–303. 10.1093/her/cyf031. [DOI] [PubMed] [Google Scholar]
- Xu Xin, Bishop Ellen E., Kennedy Sara M., Simpson Sean A., and Pechacek Terry F.. 2015. “Annual Healthcare Spending Attributable to Cigarette Smoking: An Update.” American Journal of Preventive Medicine 48 (3): 326–333. [DOI] [PMC free article] [PubMed] [Google Scholar]