Abstract
Background
Graduate medical education (GME) has emphasized the assessment of trainee competencies and milestones; however, sufficient in-person assessment is often constrained. Using mobile hands-free devices, such as Google Glass (GG) for telemedicine, allows for remote supervision, education, and assessment of residents.
Objective
We reviewed available literature on the use of GG in GME in the clinical learning environment, its use for resident supervision and education, and its clinical utility and technical limitations.
Methods
We conducted a systematic review in accordance with 2009 PRISMA guidelines. Applicable studies were identified through a review of PubMed, MEDLINE, and Web of Science databases for articles published from January 2013 to August 2018. Two reviewers independently screened titles, abstracts, and full-text articles that reported using GG in GME and assessed the quality of the studies. A systematic review of these studies appraised the literature for descriptions of its utility in GME.
Results
Following our search and review process, 37 studies were included. The majority evaluated GG in surgical specialties (n = 23) for the purpose of surgical/procedural skills training or supervision. GG was predominantly used for video teleconferencing, and photo and video capture. Highlighted positive aspects of GG use included point-of-view broadcasting and capacity for 2-way communication. Most studies cited drawbacks that included suboptimal battery life and HIPAA concerns.
Conclusions
GG shows some promise as a device capable of enhancing GME. Studies evaluating GG in GME are limited by small sample sizes and few quantitative data. Overall experience with use of GG in GME is generally positive.
Introduction
Graduate medical education (GME) has emphasized the importance of assessing resident competencies and milestones so that residency programs throughout the United States will produce physicians demonstrating proficiency across multiple domains.1,2 In order to comply with new requirements, there is renewed emphasis on resident assessment methods. Studies have documented clear associations between level of supervision and educational and patient-related outcomes,3–13 resident autonomy,5,6,9,13 satisfaction,5,9,12 and clinical competence and preparedness after graduation.3,5,9,14–16 Moreover, trainees have identified lack of supervision as a major source of suboptimal patient outcomes.16
Due to scheduling limitations, supervising physicians are not always available to provide in-person oversight, which may be ideal for direct observation and supervision. This is most challenging during time-sensitive emergency consultations and after-hours rotations, such as night float.6 Lefrak and colleagues8 found night float residents encountered lower resident supervision compared with their day rotation colleagues. One strategy to ensure patient safety and quality outcomes while reinforcing resident autonomy and clinical education is adding in-house faculty, which is a costly and resource-limited solution.6,10,11,17
Telemedicine offers a potential medium for enhancing remote supervision, education, and evaluation of residents without necessitating increased physical presence.17–30 A variety of specialties have implemented conventional telemedicine in GME by assessing its feasibility for educating trainees via recorded videos18,27,31 and live video-teleconferencing (VTC) with good feedback.17,19–21,23–30 However, stationary telemedicine end points are not always practical for supervising residents performing hands-on physical examinations or procedures in multiple clinical environments.
Wearable technology has emerged as an alternative to stationary telemedicine and is of recent interest because of its applicability in the clinical setting. Google Glass (GG) in particular is a popular hands-free wearable device with telemedicine capability (Figure 1). Multiple reviews have demonstrated GG's feasibility, usability, and acceptability in surgical settings32–34 and have called for increased research into GG's role in clinical education.
Figure 1.

Google Glass Components
Note: Google Glass (GG) is a lightweight, wearable computing device. It can be mounted over framed glasses or worn with prescription lenses. GG integrates the user's normal visual input into a 640 × 360 pixel digital screen (prism) at the corner of the user's right eye. It does not obstruct a user's view, and the user only needs to look up to view the display. Standard features include a 5-megapixel camera that records in 720p, microphone, mastoid bone conduction–based speaker, touchpad, and wireless and Bluetooth connectivity. In addition to manual control, GG can be operated via voice commands and head gestures.
In this review, we specifically investigate the use of GG in the clinical learning environment and evaluate its use in both surgical and nonsurgical settings. We appraise the literature for experiences with GG used in GME for resident supervision and education, which distinguishes it from previous reviews of clinical uses for GG. We also review the clinical utility and technical limitations of GG, again with a focus on feasibility in the GME clinical learning environment.
Methods
Our systematic review was conducted according to the guidelines in the 2009 PRISMA statement for reporting systematic reviews.35
We established a search strategy after consulting 2 medical librarians. In August 2018, 3 databases (PubMed, MEDLINE, and Web of Science) were independently searched for articles that referenced the use of GG in clinical practice by physicians or trainees for the purpose of GME. To complete the search, we queried articles published in the last 5 years using the key word “Google Glass.” Two reviewers (C.C.W. and W.C.) independently screened titles, abstracts, and full-text articles, selecting only articles pertaining to use of GG in the GME setting. Only articles defined as original research or case reports that had full text available were included for analysis. The findings of original research articles, and particularly those with objective outcome measures, were weighted more heavily in the analysis. Conference proceedings or abstracts with no accompanying full text, editorials, commentaries, or online/news reports were not included. Duplicate records, non-English, and nonhuman studies were also omitted. Table 1 details our full eligibility requirements. Our review focuses on the use of GG due to the paucity of available literature on other wearable devices.36
Table 1.
Specific Eligibility Requirements for Each Criterion
| Inclusion Criteria | Exclusion Criteria |
| 1. Formal articles (defined as original research, review articles, case reports) with full text 2. Google Glass used by physicians or trainees in clinical practice 3. Published between January 1, 2013, and August 1, 2018 | 1. Conference proceedings/abstracts without full text 2. Editorials, commentaries, online/news reports 3. Nonhuman 4. Non-English |
Each article satisfying our search criteria underwent extraction of the following data points: author names, publication year, specific medical specialty described (if any), outcomes assessed, and a summary of findings. We specifically aimed to highlight clinical uses and how GG, as a novel device, might serve as a substitute for conventional telemedicine to augment education and supervision.
Results
Search Results and Study Descriptions
The literature search yielded a total of 349 publications. After excluding duplicates, we performed an initial screening process of scanning the titles (removing 107 articles), then reading the abstracts (removing 25 articles), finally producing 48 unique publications. After reviewing the full texts, we removed 8 additional articles not pertaining to GME, and 3 review articles. A total of 37 articles were included in the final review (Figure 2). The 37 publications included 32 original research articles and 5 case reports. The number of publications for each year is as follows: 2013 (n = 1), 2014 (n = 6), 2015 (n = 11), 2016 (n = 13), 2017 (n = 6), and 2018 (n = 0). The included articles were mostly from surgical or subsurgical specialties (n = 23, 62%), and the remainder were from medical specialties (n = 14, 38%). The most common uses for GG in these articles was surgical/procedural skills teaching or supervision (n = 23, 62%), imaging/study interpretation (n = 10, 27%), and simulation-based exercises (n = 4, 11%). A summary of included articles is presented in Table 2.
Figure 2.
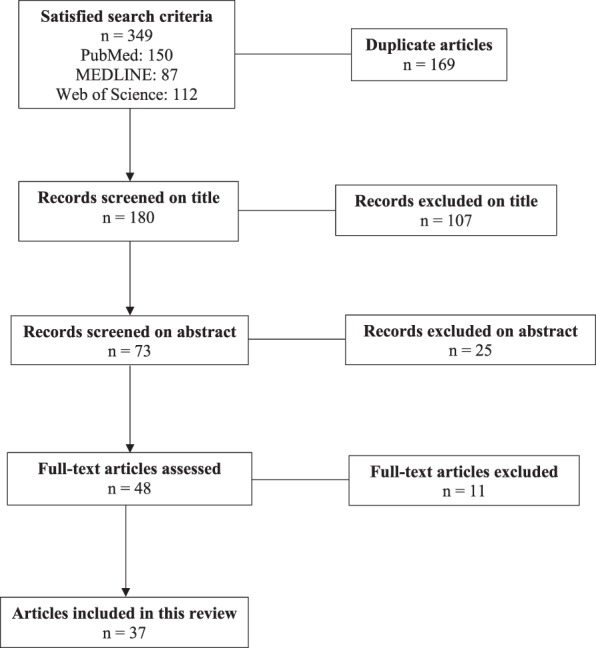
Flowchart of Study Screening Process
Table 2.
Summary of References
| Study, y | Publication Category | Specialty | Outcome(s) Assessed | Summary |
| Lee et al,31 2016 | Article | Spinal surgery | Feasibility, safety, and efficacy of action cameras in spine surgery | This study compared GG to other commercially available action cameras (GoPro Hero 4 Silver and Panasonic HX-A100). GG was the most convenient and lightweight device for long operations, and the only device to allow 2-way communication. However, GG lacked the image quality (HD format) and field of view of GoPro. |
| Moshtaghi et al,36 2015 | Article | Otolaryngology surgery | Utility within ENT surgery and potential for surgical education and enhancement of communication between surgical teams | GG allows otolaryngologists to record surgical videos, communicate between teams, and remotely supervise trainees. However, GG suffers from technical limitations, such as limited visualization of the full depth of anatomy. |
| Sahyouni et al,37 2017 | Article | Neurological surgery | Debriefing and resident education | GG enhanced neurological surgery residents' education, specifically their technical understanding of procedures. |
| Chimenti and Mitten,38 2015a | Article | Surgery | Total time to pin fracture, total number of pin attempts, total number of fluoroscopic images obtained | GG is feasible for assisting in the visualization of fluoroscopic images during percutaneous pinning of hand fractures on cadavers. GG led to decreased time to pin fracture, the number of pin attempts, and the number of fluoroscopic images obtained. |
| Knight et al,39 2015 | Case report | Surgery | Feasibility | GG successfully broadcast a cardiac procedure onto a mobile phone for remote viewing. They report feasibility for medical education, as GG replaces expensive and cumbersome equipment for remote viewing. |
| Sinkin et al,40 2016 | Article | Plastic surgery | Ease of use, image quality, gaze disruption, and distraction during surgery | Plastic surgeons wore GG for image and video capture during operations. The surgeons rated GG as comfortable and easy to wear on a postoperative survey, although one-third rated GG as distracting. |
| Baldwin et al,41 2016 | Article | Surgery | Organ quality assessment measures | GG live VTC function allowed off-site transplant team members to participate in the assessment of donor organ quality. |
| Hamann et al,42 2014 | Article | Dermatology | Communication and collaboration between physicians in multiple departments | GG is an asset for communication between multiple physicians and departments, especially in the setting of Mohs surgery. It can lead to improved patient care and outcomes as the coordination is made more efficient. |
| Brewer et al,43 2016a | Article | General surgery and cardiothoracic surgery | Accuracy of needle placement, time to completion, user satisfaction | GG was assessed as a wearable surgical visualization device for inheriting the first-person perspective of the surgical resident. Results showed improved accuracy of needle placement without significant change in time to task completion. Also, users had favorable reviews of the device. |
| Armstrong et al,44 2014 | Case report | Surgery | Feasibility and resident education | Provided case examples of GG use for diabetic limb salvage surgery. GG enhanced communication among surgeons and has the potential to increase patient safety. |
| Borgmann et al,45 2017 | Article | Urology | Feasibility, safety, and usefulness in urologic surgery | Implementation of GG is feasible and safe in urologic surgery. Urologists rated GG most useful for taking photo/video for training purposes. |
| Garcia-Cruz et al,46 2018 | Article | Urology | Usefulness in the operating room | Urologists found GG more useful in the operating room than outpatient clinic. Live VTC, specifically for educational purposes, was the highest-rated functionality. |
| Chai et al,47 2015 | Article | Dermatology | Feasibility and acceptability | GG is a feasible and acceptable device for real-time ED teledermatology. Patients believed their privacy was protected and preferred GG to standard telephone consults when face-to-face consults were unavailable. |
| Yuan et al,48 2015 | Case report | Neurology | Feasibility for telestroke | The authors described a case of acute evaluation and IV thrombolysis guided by GG VTC between a local physician and remote neurohospitalist. They found GG to be convenient and reliable for teleconsultation. |
| Drummond et al,49 2017a | Article | Pediatrics | Feasibility for remote management of CPR | Pediatric residents were tasked with performing CPR on a mannequin. One group was allowed to utilize GG for live VTC with a remote intensivist and compared to a non-GG control group. GG did not significantly improve pediatric residents' CPR quantity of compressions but did improve quality of compressions. |
| Vallurupalli et al,50 2013 | Article | Cardiology | Fellow education and patient outcomes | This study assessed the effect of GG on the educational experience of cardiology fellows. Trainees enacted scenarios that were livestreamed to a remote device for supervision. Results demonstrated GG's potential to enhance medical education and patient safety. |
| Skolnik et al,51 2016a | Article | Toxicology | Reliability and acceptability between in-person and remote supervisors | Results demonstrated high agreeability between in-person and remote supervisors when toxicology fellows wore GG for livestreaming physical examinations and transmitting still photos of ECGs. Additionally, they showed that users were comfortable with the device. |
| Chai et al,52 2014 | Article | Toxicology | Feasibility of GG VTC for toxicology consults | Toxicology residents in the ED wore GG for VTC with remote fellows and attendings. Video quality was usable in 89% of cases, and the GG consult altered medical management in approximately half of the cases. |
| Hashimoto et al,53 2016 | Article | Surgery | Video quality and safety for telementoring | The authors compared GG and Apple iPhone 5 video quality for a telementoring session during the open cholecystectomy portion of a Whipple procedure. They found current hardware limitations preclude GG's full adoption as a telementoring device for surgery. |
| Liebert et al,54 2016 | Article | Surgery | Usefulness for vital sign monitoring | Vital signs were livestreamed during simulated surgical procedures. GG did not significantly reduce the time it took residents to recognize vitals deterioration. |
| Evans et al,55 2016a | Article | Surgery | First-person (GG) versus third-person videos for visualization of bedside procedural skills assessment in surgical residents | GG first-person vantage point can improve the visualization of bedside procedural skills assessment for surgical residents while maintaining interrater reliability when compared to in-person real-time evaluation. However, GG has several limitations, related to its line of sight and ergonomics. |
| Son et al,56 2017 | Article | Otolaryngology | Resident education | Patients in an ENT clinic wore GG to record residents during a clinic encounter. Residents subsequently reviewed the recordings for training purposes. |
| Rahimy and Garg,57 2015 | Article | Ophthalmology | Utility for surgical education | GG was utilized to record still photos and video clips during a scleral buckling procedure. They found that GG holds promise for surgical teaching, as the recordings were detailed enough to recognize salient steps of the procedure. |
| Nakhla et al,58 2017 | Article | Neurological surgery | Resident education | Senior neurological surgeons captured video segments of critical teaching moments during neurological surgical procedures. Residents found GG easy to use in a postassessment survey. |
| Jeroudi et al,59 2015 | Article | Cardiology | Accuracy of remote ECG interpretation | Interpretation via GG display is less accurate compared with other modalities, and GG will benefit from a higher-resolution camera. There is limited satisfaction and confidence among participants using GG. |
| Spencer et al,60 2014 | Case report | Pediatric anesthesia | Feasibility of GG for airway management | GG is a feasible tool for the documentation of airway assessment and management with minimal disruption to care under standard OR settings (room lighting, etc). |
| Spaedy et al,61 2016 | Article | Cardiology | Accuracy for x-ray interpretation | Physicians interpreted chest x-rays via the GG prism screen, a photo capture taken via GG, and on a traditional computer screen. The majority were uncomfortable interpreting the x-ray on the small prism GG screen, yet many were satisfied with the photo taken via GG. |
| Schaer et al,62 2015 | Article | Surgery | Accuracy of identifying abnormal ECG rhythms from GG | The study shows that GG may be useful for live ECG readings in emergency situations. Six differing ECG rhythms requiring urgent attention were simulated, and GG demonstrated no significant difference from live ECG readings on a laptop. |
| Drake-Brockman et al,63 2016 | Article | Pediatric anesthesia | Satisfaction and ease of use | Pediatric anesthetists used a custom-designed GG software to continuously view patient parameters from the anesthesia work station. They found the custom software acceptable and nondistracting. |
| Wu et al,64 2014a | Article | Emergency medicine | Feasibility of using GG for ultrasound-guided procedures | GG is feasible for use during ultrasound-guided procedures. GG users took longer than their non-GG counterparts to complete the ultrasound-guided procedures and required more needle redirections; however, GG users had decreased unnecessary hand movements compared with the control group. |
| Diaz et al,65 2017 | Case report | Neurological surgery | Feasibility of using GG in neurological surgery | Neurological surgeons mounted GG onto a surgical loupe and integrated the Stealth S7 (Medtronic Inc, Littleton, MA) GG software for an image-guided surgical resection of an intracranial tumor. However, GG is unable to provide the necessary magnification for procedures requiring a microscope. |
| Dickey et al,66 2016 | Article | Urology | User satisfaction and educational outcomes | Utilized a novel application that assisted urology trainees in placing an inflatable penile prosthesis. |
| Muensterer et al,67 2014 | Article | Pediatric surgery | Utility of GG in pediatric surgery | GG has utility in the clinical setting, but several limitations need to be solved, and medical applications need to be developed before it can be recommended universally to physicians and surgeons. |
| Porras et al,68 2016 | Article | Neurological surgery | Ergonomics, media quality, and media sharing | Neurological surgeons compared GG to a Panasonic HX-A500 camera for surgical recording. Both had shortcomings related to ergonomics, while Panasonic had greater media quality and GG had greater media-sharing ability. |
| Duong et al,69 2015 | Article | Cardiology | Accuracy of coronary angiogram interpretation | Ninety percent of surveyed physicians were “somewhat or very satisfied” that GG recordings of coronary angiograms were adequate for interpretation of major findings. |
| Stetler et al,70 2016 | Article | Cardiology | Accuracy of ECG interpretation | A third-party software (VitalCom) provided hands-free zoom and pan capability when viewing images through the GG display. This functionality allowed increased accuracy of ECG interpretation and showed no significant difference from paper or mobile phone ECG interpretation. GG use was also associated with high physician satisfaction. |
Abbreviations: GG, Google Glass; ENT, ear, nose, and throat; VTC, video-teleconferencing; ED, emergency department; IV, intravenous; CPR, cardiopulmonary resuscitation; ECG, electrocardiogram; OR, operating room.
Higher-quality study.
Study Quality Overview
Studies of GG in GME are in the early stages, with most studies (n = 26, 70%) describing feasibility, general use, and feedback on the device's utility. A small subset of these studies (n = 3, 8%) compared GG to other devices with regard to performance in the clinical learning environment on the basis of video quality, technical limitations, and ease of use. Few studies (n = 4, 11%) had objective measures of surgical/procedural performance comparing GG wearers to nonwearers, including time to completion, number of attempts, and need for repositioning/redirection. Only 2 studies (5%) specifically evaluated differences between GG-based assessment and conventional assessment methods (in-person supervision or third-person video assessment). Articles felt to be of particularly high quality are identified in Table 2.
Clinical Uses of GG in GME
Currently available uses of GG broadly include VTC, photo and video capture, and custom prism displays (what can be viewed by the device wearer; Figure 1).
GG's ability to conduct VTC has been demonstrated for surgery,31,36–46 dermatology,42,47 neurology,48 pediatrics,49 cardiology,50 and toxicology.51,52 With VTC, GG also doubles as a telementoring device, allowing trainees to broadcast their point of view to supervising physicians43,44,50,51,53 and vice versa.36 Vallurupalli et al50 found GG could assist trainees in simulated clinical scenarios and allow for improved patient communication. Skolnik et al51 showed high agreeability between in-person and remote supervisors when toxicology fellows wore GG for live-streaming physical examinations and transmitting still photos of electrocardiograms (ECGs). Chai et al52 reported that residents seeing toxicology consults in the emergency room using GG to aid their consultation (VTC with remote supervisors) resulted in a change in medical management in approximately one-half of cases. Thus, trainees were able to gain clinical experience and direct supervisor feedback even in the absence of direct physical oversight.
Beyond person-to-person VTC, existing literature highlights a range of GG uses, including live-streaming vital signs during simulated surgical scenarios,54 recording video for resident assessment purposes,36,37,40,55,56 building a video library to log improvements,26 and capturing point-of-view procedures performed by senior physicians.57,58 Sahyouni et al37 reported that reviewing video clips recorded via GG enhanced neurological surgery residents' technical understanding of procedures, ultimately leading to increased confidence and level of comfort. Multiple studies reported improved trainee techniques following review of recorded surgical videos, with Chimenti and Mitten38 noting that for percutaneous pinning of hand fractures in a cadaveric lab, use of GG led to decreased time to pin fracture, a decrease in the number of pin attempts, and a decrease in the number of fluoroscopic images obtained.38 Lastly, photo capture has been used to obtain intraoperative photos,40,42 obtain photos of electrocardiograms,59 document airway placement in the operating room,60 and photos of chest x-rays.61 Schaer et al62 simulated 6 differing ECG rhythms thought to require urgent attention, and trainees using GG images for interpretation demonstrated no significant difference from live ECG readings on a laptop.
Custom-designed GG applications provide an avenue to enhance basic GG functionality. Custom-designed applications have been developed for pediatric anesthesia63 and cardiac surgery62 to continuously monitor patient parameters. Additionally, custom-designed GG applications have been utilized in image-guided procedures, such as ultrasound-guided central venous access,64 intracranial tumor resection,65 and urologic prosthetics.66
Limitations of GG in GME
In 30% (n = 11) of studies reviewed, the most commonly reported hardware criticism of GG in GME relates to battery life.27,28,37,38,45,57,58,65,67,68,71 Additionally, GG use was affected by incompatibility with select surgical equipment,31,38,57,66,67 inability to follow gaze and correct to the line of sight,31,36,57,66,67 distractibility,38,40,65,67,72 and propensity to overheat.55,64 Use of GG may be limited by room lighting,36–38,57,66,67 a need for additional glasses, or surgical magnification loupes.31,36,37 However, at least 1 study57 found that GG fit with magnifying loupes for scleral buckling surgery, and others utilized strong adhesive tape for loupe attachment.65,68 GG software obstacles include a lack of zoom capability,57,58,61,67 and connectivity issues that hamper VTC and recorded multimedia audiovisual quality.31,36,44,50,52,53,64,67,69 To address zooming, Stetler et al70 disclosed an increased accuracy of remote ECG interpretations on GG with the use of third-party software that enabled hands-free zoom and pan capability, addressing a drawback previously reported by Jeroudi et al.59
Wearer distractibility is also a major concern in the GME setting. One study likened GG voice control features to hands-free communication while driving.67 Another had reservations about inattention blindness,38 but this may be reduced by increasing the emphasis on layout, space, colors, and timing design of the GG software. An additional study found that residents adopted a “listening attitude” during live VTC that negatively impacted performance.49
As with all forms of telemedicine, patient privacy and data security represent a potential concern among medical GG users.36,38,39,44,47,48,55,57,67 Under the Health Insurance Portability and Accountability Act (HIPAA) and the Health Information Technology for Economic and Clinical Health Act (HITECH),73 many commercial wearable devices with GG-like features do not comply with the extensive information technology standards.52 Muensterer et al67 noticed GG automatically syncs with Google servers when charged and connected to a Wi-Fi network, leading to concerns about sensitive information being transmitted outside the medical center firewall.67 To address concerns regarding privacy, many users retain the services of certified partners of GG in order to operationalize them for use in the health care setting.47,51,52 From patient perspectives, use of GG appears to be acceptable.63,67 Patients evaluated with use of GG in teledermatology consults felt comfortable when physicians used third-party HIPAA-compliant GGs.47
Acceptability
A majority of studies expressed striking acceptability among physicians37,40,43,45,46,49,54,56,58,66,67,70 and patients.51,52,56,67 One study found that younger trainees rated GG as more educationally useful and less distracting in the operating room compared with their faculty counterparts.66 Despite results that did not fully support the use of GG in GME, most researchers remained optimistic about future iterations and the potential to improve provision of clinical care and medical education.27,49,53,63,70
Discussion
Our review highlights that much of the literature investigating use of GG in GME has been focused on the feasibility and general use of GG within the clinical learning environment. The literature suggests that the ability to execute VTC, particularly using the wearer's point of view, holds promise as a tool for procedural skills acquisition, remote supervision, and assessment.
Interestingly, we did not encounter any reports of patients wearing GG for point-of-view–recorded encounters with a resident as a tool for self-assessment. This use has been described in both nursing and dental training settings.74,75 As did many of the articles in our review, much of the existing literature regarding use of GG within the medical realm is focused on reporting feasibility. Unfortunately, the literature to date does not include much quantitative or qualitative data reporting the utility of GG from the resident's perspective. Nor are there significant data specifically investigating if this enhanced supervision led to improvement in patient outcomes or resident performance.
Limitations of our review include the relative paucity of literature specific to GG applications in GME, and the published articles primarily include single institution studies or small sample sizes. We chose to exclusively study GG due to its early penetration among wearable devices into the clinical learning environment, although there are other wearable devices commercially available that may offer alternative characteristics for future application. Among the literature describing GG and its acceptance as an educational tool, few objective data exist, and most experience remains observational. Unsurprisingly, much of the current published literature focuses on GG incorporation in surgical settings. More studies of its utility and feasibility in nonsurgical settings will allow for a more complete picture of its future incorporation into medical education and training. Lastly, with the rapid pace of technologic innovation, results may not reflect current advances in wearable mobile health technology.
The body of literature evaluating GG in GME would be bolstered significantly by additional studies more specifically investigating benefits to resident learning and performance as opposed to simply the feasibility of use in the clinical learning environment. A qualitative assessment of the resident perspective when using GG in their education could provide greater insight into trainee experience beyond acceptability, which is what has been published most extensively. Evaluation of patients' attitudes to residents' use of GG in their care would also be informative.
Conclusions
Despite the promise and early experience with GG as a health care and GME tool, further investigation aimed at demonstrating specific educational benefits and feasibility in more diverse settings is needed before it can be fully integrated into the clinical learning environment. This review made evident potentially solvable issues with usability, durability, and acceptance currently seen across specialties. As mobile health technology continues to evolve, GG and other mobile, hands-free devices may serve as effective media for remote supervision and evaluation of medical trainees in the clinical learning environment.
References
- 1.Malik MU, Diaz Voss Varela DA, CM Stewart, Laeeq K, Yenokyan G, Francis HW, et al. Barriers to implementing the ACGME outcome project: a systematic review of program director surveys. J Grad Med Educ. 2012;4(4):425–433. doi: 10.4300/JGME-D-11-00222.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nasca TJ, Philibert I, Brigham T, Flynn TC. The next GME accreditation system—rationale and benefits. N Engl J Med. 2012;366(11):1051–1056. doi: 10.1056/NEJMsr1200117. [DOI] [PubMed] [Google Scholar]
- 3.Bricker DA, Markert RJ. Night float teaching and learning: perceptions of residents and faculty. J Grad Med Educ. 2010;2(2):236–241. doi: 10.4300/JGME-D-10-00005.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fallon WF, Wears RL, Tepas JJ. Resident supervision in the operating room: does this impact on outcome? J Trauma. 1993;35(4):556–560. doi: 10.1097/00005373-199310000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Farnan JM, Petty LA, Georgitis E, Martin S, Chiu E, Prochaska M, et al. A systematic review: the effect of clinical supervision on patient and residency education outcomes. Acad Med. 2012;87(4):428–442. doi: 10.1097/ACM.0b013e31824822cc. [DOI] [PubMed] [Google Scholar]
- 6.Haber LA, Lau CY, Sharpe BA, Arora VM, Farnan JM, Ranji SR. Effects of increased overnight supervision on resident education, decision-making, and autonomy. J Hosp Med. 2012;7(8):606–610. doi: 10.1002/jhm.1959. [DOI] [PubMed] [Google Scholar]
- 7.Jones DL. Residents' perspectives on patient safety in university and community teaching hospitals. J Grad Med Educ. 2014;6(3):603–607. doi: 10.4300/JGME-D-14-00350.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lefrak S, Miller S, Schirmer B, Sanfey H. The night float system: ensuring educational benefit. Am J Surg. 2005;189(6):639–642. doi: 10.1016/j.amjsurg.2004.11.034. [DOI] [PubMed] [Google Scholar]
- 9.Phy MP, Offord KP, Manning DM, Bundrick JB, Huddleston JM. Increased faculty presence on inpatient teaching services. Mayo Clin Proc. 2004;79(3):332–336. doi: 10.4065/79.3.332. [DOI] [PubMed] [Google Scholar]
- 10.Weltz AS, Harris DG, Kidd-Romero S, Kavic SM. Assessing the night float educational experience. Am Surg. 2016;82(1):e6–e8. [PubMed] [Google Scholar]
- 11.Weltz AS, Cimeno A, Kavic SM. Strategies for improving education on night-float rotations: a review. J Surg Educ. 2015;72(2):297–301. doi: 10.1016/j.jsurg.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Baldwin DC, Daugherty SR, Ryan PM. How residents view their clinical supervision: a reanalysis of classic national survey data. J Grad Med Educ. 2010;2(1):37–45. doi: 10.4300/JGME-D-09-00081.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farnan JM, Johnson JK, Meltzer DO, Humphrey HJ, Arora VM. On-call supervision and resident autonomy: from micromanager to absentee attending. Am J Med. 2009;122(8):784–788. doi: 10.1016/j.amjmed.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 14.Mattar SG, Alseidi AA, Jones DB, Jeyarajah DR, Swanstrom LL, Aye RW, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg. 2013;258(3):440–449. doi: 10.1097/SLA.0b013e3182a191ca. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed HM, Gale SC, Tinti MS, Shiroff AM, Macias AC, Rhodes SC, et al. Creation of an emergency surgery service concentrates resident training in general surgical procedures. J Trauma Acute Care Surg. 2012;73(3):599–604. doi: 10.1097/TA.0b013e318265f984. [DOI] [PubMed] [Google Scholar]
- 16.Coleman JJ, Esposito TJ, Rozycki GS, Feliciano DV. Early subspecialization and perceived competence in surgical training: are residents ready? J Am Coll Surg. 2013;216(4):764–771. doi: 10.1016/j.jamcollsurg.2012.12.045. [DOI] [PubMed] [Google Scholar]
- 17.Arriaga M, Nuss D, Arriaga RY. Neurotology telemedicine consultation. Otolaryngol Clin North Am. 2011;44(6):1235–1250. doi: 10.1016/j.otc.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 18.Beard HR, Marquez-Lara AJ, Hamid KS. Using wearable video technology to build a point-of-view surgical education library. JAMA Surg. 2016;151(8):771–772. doi: 10.1001/jamasurg.2016.0976. [DOI] [PubMed] [Google Scholar]
- 19.Burgess LP, Syms MJ, Holtel MR, Birkmire-Peters DP, Johnson RE, Ramsey MJ. Telemedicine: teleproctored endoscopic sinus surgery. Laryngoscope. 2002;112(2):216–219. doi: 10.1097/00005537-200202000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Capampangan DJ, Wellik KE, Bobrow BJ, Aguilar MI, Ingall TJ, Kiernan TE, et al. Telemedicine versus telephone for remote emergency stroke consultations: a critically appraised topic. Neurologist. 2009;15(3):163–166. doi: 10.1097/NRL.0b013e3181a4b79c. [DOI] [PubMed] [Google Scholar]
- 21.Gandsas A, McIntire K, Montgomery K, Bumgardner C, Rice L. The personal digital assistant (PDA) as a tool for telementoring endoscopic procedures. Stud Health Technol Inform. 2004;98:99–103. [PubMed] [Google Scholar]
- 22.Glover JA, Williams E, Hazlett LJ, Campbell N. Connecting to the future: telepsychiatry in postgraduate medical education. Telemed J E Health. 2013;19(6):474–479. doi: 10.1089/tmj.2012.0182. [DOI] [PubMed] [Google Scholar]
- 23.Jagolino AL, Jia J, Gildersleeve K, Ankrom C, Cai C, Rahbar M, et al. A call for formal telemedicine training during stroke fellowship. Neurology. 2016;86(19):1827–1833. doi: 10.1212/WNL.0000000000002568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kramer NM, Demaerschalk BM. A novel application of teleneurology: robotic telepresence in supervision of neurology trainees. Telemed J E Health. 2014;20(12):1087–1092. doi: 10.1089/tmj.2014.0043. [DOI] [PubMed] [Google Scholar]
- 25.McBeth PB, Crawford I, Blaivas M, Hamilton T, Musselwhite K, Panebianco N, et al. Simple, almost anywhere, with almost anyone: remote low-cost telementored resuscitative lung ultrasound. J Trauma. 2011;71(6):1528–1535. doi: 10.1097/TA.0b013e318232cca7. [DOI] [PubMed] [Google Scholar]
- 26.Nagengast ES, Ramos MS, Sarma H, Deshpande G, Hatcher K, Magee WP, Jr, et al. Surgical education through video broadcasting. J Craniofac Surg. 2014;25(5):1619–1621. doi: 10.1097/SCS.0000000000001143. [DOI] [PubMed] [Google Scholar]
- 27.Paro JA, Nazareli R, Gurjala A, Berger A, Lee GK. Video-based self-review: comparing google glass and GoPro technologies. Ann Plast Surg. 2015;74(1 suppl):71–74. doi: 10.1097/SAP.0000000000000423. [DOI] [PubMed] [Google Scholar]
- 28.Ponce BA, Jennings JK, Clay TB, May MB, Huisingh C, Sheppard ED. Telementoring: use of augmented reality in orthopaedic education: AAOS exhibit selection. J Bone Joint Surg Am. 2014;96(10):e84. doi: 10.2106/JBJS.M.00928. [DOI] [PubMed] [Google Scholar]
- 29.Ponsky TA, Schwachter M, Parry J, Rothenberg S, Augestad KM. Telementoring: the surgical tool of the future. Eur J Pediatr Surg. 2014;24(4):287–294. doi: 10.1055/s-0034-1386646. [DOI] [PubMed] [Google Scholar]
- 30.Safir IJ, Shrewsberry AB, Issa IM, Ogan K, Ritenour CW, Sullivan J, et al. Impact of remote monitoring and supervision on resident training using new ACGME milestone criteria. Can J Urol. 2015;22(5):7959–7964. [PubMed] [Google Scholar]
- 31.Lee CK, Kim Y, Lee N, Kim B, Kim D, Yi S. Feasibility study of utilization of action camera, GoPro hero 4, Google Glass, and Panasonic HX-A100 in spine surgery. Spine. 2017;42(4):275–280. doi: 10.1097/BRS.0000000000001719. [DOI] [PubMed] [Google Scholar]
- 32.Chang JY, Tsui LY, Yeung KS, Yip SW, Leung GK. Surgical vision: Google Glass and surgery. Surg Innov. 2016;23(4):422–426. doi: 10.1177/1553350616646477. [DOI] [PubMed] [Google Scholar]
- 33.Davis CR, Rosenfield LK. Looking at plastic surgery through Google Glass, part 1: systematic review of Google Glass evidence and the first plastic surgical procedures. Plast Reconstr Surg. 2015;135(3):918–928. doi: 10.1097/PRS.0000000000001056. [DOI] [PubMed] [Google Scholar]
- 34.Wei NJ, Dougherty B, Myers A, Badawy SM. Using Google Glass in surgical settings: systematic review. JMIR Mhealth Uhealth. 2018;6(3):e54. doi: 10.2196/mhealth.9409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 36.Moshtaghi O, Kelley KS, Armstrong WB, Ghavami Y, Gu J, Djalilian HR. Using Google Glass to solve communication and surgical education challenges in the operating room. Laryngoscope. 2015;125(10):2295–2297. doi: 10.1002/lary.25249. [DOI] [PubMed] [Google Scholar]
- 37.Sahyouni R, Moshtaghi O, Tran DK, Kaloostian S, Rajaii R, Bustillo D, et al. Assessment of Google Glass as an adjunct in neurological surgery. Surg Neurol Int. 2017;8:68. doi: 10.4103/sni.sni_277_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chimenti PC, Mitten DJ. Google Glass as an alternative to standard fluoroscopic visualization for percutaneous fixation of hand fractures: a pilot study. Plast Reconstr Surg. 2015;136(2):328–330. doi: 10.1097/PRS.0000000000001453. [DOI] [PubMed] [Google Scholar]
- 39.Knight HM, Gajendragadkar PR, Bokhari A. Wearable technology: using Google Glass as a teaching tool. BMJ Case Rep. 2015 doi: 10.1136/bcr-2014-208768. pii:bcr2014208768. [DOI] [PMC free article] [PubMed]
- 40.Sinkin JC, Rahman OF, Nahabedian MY. Google Glass in the operating room: the plastic surgeon's perspective. Plast Reconstr Surg. 2016;138(1):298–302. doi: 10.1097/PRS.0000000000002307. [DOI] [PubMed] [Google Scholar]
- 41.Baldwin AC, Mallidi HR, Baldwin JC, Sandoval E, Cohn WE, Frazier OH, et al. Through the looking glass: real-time video using ‘smart' technology provides enhanced intraoperative logistics. World J Surg. 2016;40(1):242–244. doi: 10.1007/s00268-015-3235-x. [DOI] [PubMed] [Google Scholar]
- 42.Hamann D, Mortensen WS, Hamann CR, Smith A, Martino B, Dameff C, et al. Experiences in adoption of teledermatology in Mohs micrographic surgery: using smartglasses for intraoperative consultation and defect triage. Surg Innov. 2014;21(6):653–654. doi: 10.1177/1553350614552735. [DOI] [PubMed] [Google Scholar]
- 43.Brewer ZE, Fann HC, Ogden WD, Burdon TA, Sheikh AY. Inheriting the learner's view: a Google Glass-based wearable computing platform for improving surgical trainee performance. J Surg Educ. 2016;73(4):682–688. doi: 10.1016/j.jsurg.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 44.Armstrong DG, Rankin TM, Giovinco NA, Mills JL, Matsuoka Y. A heads-up display for diabetic limb salvage surgery: a view through the Google looking glass. J Diabetes Sci Technol. 2014;8(5):951–956. doi: 10.1177/1932296814535561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Borgmann H, Rodriguez Socarras M, Salem J, Tsaur I, Gomez Rivas J, Barret E, et al. Feasibility and safety of augmented reality-assisted urological surgery using smartglass. World J Urol. 2017;35(6):967–972. doi: 10.1007/s00345-016-1956-6. [DOI] [PubMed] [Google Scholar]
- 46.Garcia-Cruz E, Bretonnet A, Alcaraz A. Testing smart glasses in urology: clinical and surgical potential applications. Actas Urol Esp. 2018;42(3):207–211. doi: 10.1016/j.acuro.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 47.Chai PR, Wu RY, Ranney ML, Bird J, Chai S, Zink B, et al. Feasibility and acceptability of Google Glass for emergency department dermatology consultations. JAMA Dermatol. 2015;151(7):794–796. doi: 10.1001/jamadermatol.2015.0248. [DOI] [PubMed] [Google Scholar]
- 48.Yuan ZW, Liu ZR, Wei D, Shi M, Wang BJ, Liu YH, et al. Mobile stroke: an experience of intravenous thrombolysis guided by teleconsultation based on Google Glass. CNS Neurosci Ther. 2015;21(7):607–609. doi: 10.1111/cns.12413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Drummond D, Arnaud C, Guedj R, Duguet A, de Suremain N, Petit A. Google Glass for residents dealing with pediatric cardiopulmonary arrest: a randomized, controlled, simulation-based study. Pediatr Crit Care Med. 2017;18(2):120–127. doi: 10.1097/PCC.0000000000000977. [DOI] [PubMed] [Google Scholar]
- 50.Vallurupalli S, Paydak H, Agarwal SK, Argrawal M, Assad-Kottner C. Wearable technology to improve education and patient outcomes in a cardiology fellowship program—a feasibility study. Health Technol (Berl) 2013;3(4):267–268. [Google Scholar]
- 51.Skolnik AB, Chai PR, Dameff C, Gerkin R, Monas J, Padilla-Jones A, et al. Teletoxicology: patient assessment using wearable audiovisual streaming technology. J Med Toxicol. 2016;12(4):358–364. doi: 10.1007/s13181-016-0567-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chai PR, Wu RY, Ranney ML, Porter PS, Babu KM, Boyer EW. The virtual toxicology service: wearable head-mounted devices for medical toxicology. J Med Toxicol. 2014;10(4):382–387. doi: 10.1007/s13181-014-0420-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hashimoto DA, Phitayakorn R. Fernandez-del Castillo C, Meireles O. A blinded assessment of video quality in wearable technology for telementoring in open surgery: the Google Glass experience. Surg Endosc. 2016;30(1):372–378. doi: 10.1007/s00464-015-4178-x. [DOI] [PubMed] [Google Scholar]
- 54.Liebert CA, Zayed MA, Aalami O, Tran J, Lau JN. Novel use of Google Glass for procedural wireless vital sign monitoring. Surg Innov. 2016;23(4):366–373. doi: 10.1177/1553350616630142. [DOI] [PubMed] [Google Scholar]
- 55.Evans HL, O'Shea DJ, Morris AE, Keys KA, Wright AS, Schaad DC, et al. A comparison of Google Glass and traditional video vantage points for bedside procedural skill assessment. Am J Surg. 2016;211(2):336–342. doi: 10.1016/j.amjsurg.2015.07.029. [DOI] [PubMed] [Google Scholar]
- 56.Son E, Halbert A, Abreu S, Hester R, Jefferson G, Jennings K, et al. Role of Google Glass in improving patient satisfaction for otolaryngology residents: a pilot study. Clin Otolaryngol. 2017;42(2):433–438. doi: 10.1111/coa.12810. [DOI] [PubMed] [Google Scholar]
- 57.Rahimy E, Garg SJ. Google Glass for recording scleral buckling surgery. JAMA Ophthalmol. 2015;133(6):710–711. doi: 10.1001/jamaophthalmol.2015.0465. [DOI] [PubMed] [Google Scholar]
- 58.Nakhla J, Kobets A, De la Garza Ramos R, Haranhalli N, Gelfand Y, Ammar A, et al. Use of Google Glass to enhance surgical education of neurosurgery residents: “proof-of-concept” study. World Neurosurg. 2017;98:711–714. doi: 10.1016/j.wneu.2016.11.122. [DOI] [PubMed] [Google Scholar]
- 59.Jeroudi OM, Christakopoulos G, Christopoulos G, Kotsia A, Kypreos MA, Rangan BV, et al. Accuracy of remote electrocardiogram interpretation with the use of Google Glass technology. Am J Cardiol. 2015;115(3):374–377. doi: 10.1016/j.amjcard.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 60.Spencer RJ, Chang PH, Guimaraes AR, Firth PG. The use of Google Glass for airway assessment and management. Paediatr Anaesth. 2014;24(9):1009–1011. doi: 10.1111/pan.12496. [DOI] [PubMed] [Google Scholar]
- 61.Spaedy E, Christakopoulos GE, Tarar MN, Christopoulos G, Rangan BV, Roesle M, et al. Accuracy of remote chest X-ray interpretation using Google Glass technology. Int J Cardiol. 2016;219:38–40. doi: 10.1016/j.ijcard.2016.05.070. [DOI] [PubMed] [Google Scholar]
- 62.Schaer R, Salamin F, Jimenez Del Toro OA, Atzori M, Muller H, Widmer A. Live ECG readings using Google Glass in emergency situations. Conf Proc IEEE Eng Med Biol Soc. 2015;2015:315–318. doi: 10.1109/EMBC.2015.7318363. [DOI] [PubMed] [Google Scholar]
- 63.Drake-Brockman TF, Datta A, von Ungern-Sternberg BS. Patient monitoring with Google Glass: a pilot study of a novel monitoring technology. Paediatr Anaesth. 2016;26(5):539–546. doi: 10.1111/pan.12879. [DOI] [PubMed] [Google Scholar]
- 64.Wu TS, Dameff CJ, Tully JL. Ultrasound-guided central venous access using Google Glass. J Emerg Med. 2014;47(6):668–675. doi: 10.1016/j.jemermed.2014.07.045. [DOI] [PubMed] [Google Scholar]
- 65.Diaz R, Yoon J, Chen R, Quinones-Hinojosa A, Wharen R, Komotar R. Real-time video-streaming to surgical loupe mounted head-up display for navigated meningioma resection. Turk Neurosurg. 2017] doi: 10.5137/1019-5149.JTN.20388-17.1. [published online ahead of print April 30. [DOI] [PubMed]
- 66.Dickey RM, Srikishen N, Lipshultz LI, Spiess PE, Carrion RE, Hakky TS. Augmented reality assisted surgery: a urologic training tool. Asian J Androl. 2016;18(5):732–734. doi: 10.4103/1008-682X.166436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Muensterer OJ, Lacher M, Zoeller C, Bronstein M, Kubler J. Google Glass in pediatric surgery: an exploratory study. Int J Surg. 2014;12(4):281–289. doi: 10.1016/j.ijsu.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 68.Porras JL, Khalid S, Root BK, Khan IS, Singer RJ. Point-of-view recording devices for intraoperative neurosurgical video capture. Front Surg. 2016;3:57. doi: 10.3389/fsurg.2016.00057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Duong T, Wosik J, Christakopoulos GE, Martínez Parachini JR, Karatasakis A, Tarar MN, et al. Interpretation of coronary angiograms recorded using Google Glass: a comparative analysis. J Invasive Cardiol. 2015;27(10):443–446. [PubMed] [Google Scholar]
- 70.Stetler J, Resendes E, Martinez-Parachini JR, Patel K, Amsavelu S, Tarar MN, et al. Hands-free zoom and pan technology improves the accuracy of remote electrocardiogram interpretation using Google Glass. Int J Cardiol. 2016;204:147–148. doi: 10.1016/j.ijcard.2015.11.144. [DOI] [PubMed] [Google Scholar]
- 71.Yoon JW, Chen RE, Kim EJ, Akinduro OO, Kerezoudis P, Han PK, et al. Augmented reality for the surgeon: systematic review. Int J Med Robot. 2018;14(4):e1914. doi: 10.1002/rcs.1914. [DOI] [PubMed] [Google Scholar]
- 72.Golab MR, Breedon PJ, Vloeberghs M. A wearable headset for monitoring electromyography responses within spinal surgery. Eur Spine J. 2016;25(10):3214–3219. doi: 10.1007/s00586-016-4626-x. [DOI] [PubMed] [Google Scholar]
- 73.Modifications to the HIPAA privacy, security, enforcement, and breach notification rules under the health information technology for economic and clinical health act and the genetic information nondiscrimination act; other modifications to the HIPAA rules. Fed Regist. 2013;78(17):5565–5702. [PubMed] [Google Scholar]
- 74.Zahl DA, Schrader SM, Edwards PC. Student perspectives on using egocentric video recorded by smart glasses to assess communicative and clinical skills with standardized patients. Eur J Dent Educ. 2018;22(2):73–79. doi: 10.1111/eje.12217. [DOI] [PubMed] [Google Scholar]
- 75.Marrocco GF, Ginzburg E, Feder SL. Seeing from the eyes of the beholder: a pilot program for learning through reflection in graduate nursing education. Nurs Educ Perspect. 2019;40(2):113–115. doi: 10.1097/01.NEP.0000000000000317. [DOI] [PubMed] [Google Scholar]


