Abstract
The greatest proportion of new HIV infections among men who have sex with men (MSM) is occurring among young Black MSM (YBMSM) ages 13–24. Consequently, research is needed to understand the psychosocial pathways that influence HIV risk and resilience in YBMSM. Minority Stress Theory proposes that the stigma, prejudice, and discrimination facing sexual and racial minorities are chronic stressors that lead to increased engagement in risk behaviors. The present study examined whether minority stress is associated with stimulant use and sexual risk behaviors by depleting psychosocial resilience. We recruited 1817 YBMSM, ages 18–29, from multiple venues in two major cities in Texas for participation in a brief survey. Results from structural equation modeling indicated that decreased resilience partially mediated the association of minority stress with sexual risk behavior. Resilience was also negatively associated with stimulant use. Interventions focused on cultivating psychosocial resilience could mitigate the deleterious consequences of minority stress and reduce stimulant use in YBMSM.
Keywords: Stimulant use, Resilience, Minority stress, Sexual risk, YBMSM
Introduction
The greatest proportion of all new HIV diagnoses among men who have sex with men (MSM) is occurring among young Black MSM (YBMSM) ages 13–24 [1, 2]. Numerous studies have demonstrated a strong association between stimulant drug use (e.g., powder cocaine, crack cocaine, ecstasy, and methamphetamine) and sexual risk behaviors that can lead to the acquisition of HIV among MSM [3–8]. Stimulants impair judgment, increase impulsivity, lower risk-aversion, and increase one’s arousal and desire to engage in sexual behavior. Use of these substances can increase the likelihood of engaging in condomless sex, increase the frequency and duration of sex, and potentially increase the number of one’s sex partners [9–11]. The contribution of stimulants to HIV risk has also been documented among Black MSM who engage in high-risk sexual behavior [12, 13]. However, less is known about the risk and protective factors for stimulant use and high-risk sexual behavior among YBMSM.
There is a robust body of literature showing that experiences of discrimination and victimization, as well as the negative psychosocial states that are associated with experiences of racism and homophobia, are associated with stimulant and other illicit drug use among MSM [11, 14–17]. Substance use disparities and HIV disparities may be viewed as socially-produced ills, in part explained by discrimination and victimization these men have experienced [18–25]. These ills experienced by YBMSM both predispose them to, and may exacerbate the formation of, maladaptive behaviors including stimulant use and risky sexual behavior. For YBMSM, the intersectionality of multiple stigmatized identities (i.e., minority race, and minority sexual orientation) may have layered or additive effects [25–27]. For example, risk for substance use disorders has been shown to be greatest when individuals report multiple types of discrimination [28], suggesting the need to account for multiple, overlapping identities or experiences of discrimination.
Minority stress theory [20] provides a lens through which one can examine the cumulative effects of discriminatory experiences on the well-being of YBMSM. Minority Stress Theory maintains that individuals who have non-majority identities, such as gay men and racial/ethnic minorities, experience disproportionately burdensome degrees of stigma, prejudice, and discrimination, and as a result, are at risk for increased levels of depression, substance use and sexual behaviors that may put the individual at risk for HIV [19, 20]. Additionally, homophobia, discrimination, and victimization may be internalized, and this internalized homophobia itself is a minority stressor [19, 20, 29]. The combined effects of these discriminatory experiences and their internalization may increase risk for HIV infection or transmission by influencing individual-level risk factors such as stimulant use and risky sexual behavior among YBMSM [15, 16, 30].
While the associations between mental health problems, substance abuse, and sexual risk behavior have been documented among young MSM [5, 29, 31, 32], these seminal approaches to understanding HIV disparities have focused largely on the measurement of risk-factors and have contributed to the risk-reduction literature while providing little attention to the vitality of protective factors in YBMSM health. In the broader literature focused on MSM, resilience has been defined as a process of adaption and readjustment including psychological, social, and behavioral characteristics that occur despite multiple personal and social losses [33–37]. HIV prevention researchers have also suggested that sources of resilience have been largely untapped resources in behavioral interventions and that they may be associated with reductions in substance abuse and HIV-related risk behaviors among MSM [29, 35, 36, 38]. Further, sources of resilience such as higher levels of self-esteem and social support have been specifically linked to reduced HIV-risk behavior and increased HIV-related health behaviors such as HIV testing, specifically among Black MSM [24, 39]. Herrick et al. [36] suggested that HIV prevention work would be more efficacious if it were designed to draw upon these sources of resilience.
In order for behavioral interventions to be maximally effective among YBMSM, they must focus directly on the potential mediating and moderating factors for problematic substance use and sexual risk behavior that result from minority stress. More specifically, combating stimulant use will likely be ineffective unless the discrimination experienced as the result of multiple stigmatized identities is addressed. It is paramount that HIV-prevention interventions focus not only on preventing and addressing the deleterious effects of minority stress, but also on fully understanding and capitalizing on the potentially mediating and or moderating factors that influence substance use among YBMSM. The influence of resilience assets and resources (i.e., individual factors such as gay and bisexual pride and self-esteem, and social factors such as support from peers) on YBMSM need to be examined as potential protective factors against minority stress and its associated risks [37–41].
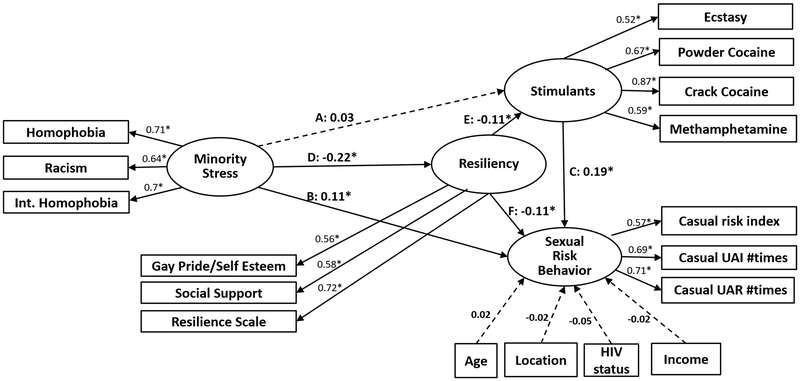
In the resilience literature there has been some debate as to whether resilience serves a mediator or a moderator. This study sought to examine sources of resilience as a potential mediator of the relationship between stressful discriminatory experiences, stimulant use, and sexual risk taking among an understudied population of YBMSM from the U.S. South (two cities in Texas) who are at high-risk for HIV infection. Based on the existing literature, we examined three specific sources of resilience among YBMSM: sexual identity pride (e.g., pride in being gay or bisexual), (2) availability and receipt of social support, and (3) traits and attitudes conceptualized as resilience, such as the belief that one’s life has meaning, or the belief that one can get through difficult times [42]. This study is the first to elucidate the potentially mediating effects of gay pride/self-esteem, resilience, and social support on the relationship between stressful experiences of racism and homophobia, stimulant use, and sexual risk behavior among YBMSM. Specifically, we hypothesized that the effect of minority stress on sexual risk behavior would have a direct pathway, as well as indirect pathways, where the relationship between minority stress and sexual risk behavior would be mediated by sources of resilience and stimulant use. We also hypothesized that sources of resilience would have an effect on stimulant use, which in turn we hypothesized would affect sexual risk behavior. A simplified path diagram of our hypotheses, without the measurement component, is depicted in Fig. 1. Understanding the important role of these potential protective factors is vital to the development of innovative resilience-based substance abuse and HIV-prevention interventions for YBMSM.
Fig. 1.
Path model of hypothesized structural relationships
Methods
Participants
Participants were Black and/or African American men between ages of 18–29. Participants were recruited as part of a large community-based HIV prevention study of YBMSM in the Dallas and Houston metropolitan areas. Data for these analyses were obtained from three waves of independent, cross-sectional samples (N = 1817) surveyed 1 year apart in each community after implementation of Mpowerment, a multi-level intervention designed to promote sense of community, increase HIV testing, and reduce sexual risk behavior among YBMSM [43]. Data from the three waves collected in the summer and fall of 2013, 2014, and 2015 were combined for this study. Eligibility requirements were that participants were Black or African American, were 18–29 years old, lived in the Dallas or Houston metropolitan areas, reported having had receptive and/or insertive anal sex with another man in the past 12 months, and spoke English.
Recruitment and Procedures
The methods have been previously described in more detail in Vincent et al. [44] Briefly, participants were recruited using modified venue-based time-location sampling, adapted from the National HIV Behavioral Surveillance Survey [45]. Venues and sampling periods were identified in 4-h blocks. In order to proceed with data collection, at least eight YBMSM needed to be present at each sampling event. A maximum of 20 surveys were collected in a given sampling event. The majority of recruitment took place at bars and clubs (93%), with an additional 7% taking place at the project offices at a major university and 0.4% at a community-based youth organization.
Nearly all participants who were approached agreed to undertake the study eligibility screening (92%); nearly all eligible participants opted to participate (94%). The site recruiters from the University of Texas, Southwestern Medical Center in Dallas and the University of Texas Health Sciences Center in Houston introduced the study and obtained verbal informed consent from each participant. Self-administered surveys were completed privately on personal digital assistants (PDAs). Autonomous PDAs were used to encourage honest responses and reduce social desirability bias for sensitive behaviors such as sexual behavior and drug use [46]. Participants were asked to provide partial information on unique characteristics (e.g., first letter of their mother’s first name) in order to construct post hoc a unique alphanumeric identifier which was used to identify respondents who participated in multiple waves so we could exclude them from these analyses. Surveys took less than 30 min on average to complete (Mean = 24 min; IQR = 17–29 min). Participants were compensated $30. The study procedures were reviewed and approved by several institutional review boards (IRBs), including the IRB at the home institution of the principal investigator as well as the IRBs of the data collection subcontractors in Dallas and Houston.
Measures
Sociodemographic
Age, self-reported HIV status, city of residence, education attained, sexual identity, and income were assessed to describe the sample, and those variables found to be significantly associated with the outcome variables at the bivariate level were used as control variables for analyses.
Minority Stress
Three separate measures of minority stress were administered including experienced homophobia, experienced racism, and internalized homophobia. Correlations among these measures were moderate (r’s = 0.46–0.51), suggesting that they assess relatively distinct facets of minority stress.
Experienced Homophobia
We used seven items adapted from Díaz et al.’s longer scale to assess men’s experiences of homophobia in the past year [47]. Participants rated how often in the past year they: (1) were made fun of or called names; (2) were hit or beaten up; (3) heard that gay people are sinners, (4) heard that gay people will be alone when they grow old; (5) felt that their attraction to other men (or being gay or bisexual) hurt and embarrassed their family; (6) had to pretend that they were totally straight or heterosexual in order to be accepted; and (7) were treated unfairly at their job for being effeminate (girly) or for being attracted to other men (or gay or bisexual). Items were rated on five-point Likert-type scales from never [1] to very often [5]. The items displayed adequate internal consistency (Cronbach’s alpha = 0.86; M = 15.64, SD = 6.68) and were used as a composite score.
Experienced Racism
We used eleven items adapted from Díaz et al.’s longer scale to assess men’s experiences of racism in the past year [47]. Sample items assessed how often “your civil rights been violated (i.e., job or housing discrimination due to racism, racial discrimination, or racial prejudice),” how often “you witnessed prejudice or discrimination directed at someone else because of their race/ethnic group,” and how often “you were treated as if you were ‘stupid’ or ‘talked down to’ because of your race/ethnic group?” Items were rated on a Likert-type scale from never [1] to very often [5]. The items displayed excellent internal consistency (Cronbach’s alpha = 0.95; M = 23.25, SD = 10.36) and were used as a composite score.
Internalized Homophobia
We used three items from our previous research [48], originally adapted from Nungesser’s [49] work to reflect the current vernacular when speaking about homosexuality, to assess this construct: “Do your religious beliefs make you feel any guilt about having sex with other men?” “Does having sex with other men make you dislike yourself?” and “Do you ever wish that you were attracted only to women?” Items were rated on a Likert-type scale from not at all [1] to a great deal [5]. The items displayed adequate internal consistency (Cronbach’s alpha = 0.79; M = 5.99, SD = 3.23) and were used as a composite score.
Sources of Resilience
Three separate measures of sources of resilience were administered including a measure of pride/self-esteem, social support and perceived resilience. Correlations among these measures were moderate (r’s = 0.34–0.47), suggesting that they assess relatively distinct facets of minority resilience.
Pride and Self-Esteem
We used three items developed from our previous research [48] to assess this construct. We asked how happy and how much pride men felt in being gay or bisexual. We also asked how comfortable they were with their sexual attraction to other men. Items were reworded to fit an interval scale response set (i.e., the degree to which they endorsed the item). These items were rated on a five-point Likert-type scale from not at all to a great deal. The items displayed adequate internal consistency (Cronbach’s alpha = 0.84; M = 11.41, SD = 3.43) and were used as a composite score.
Social Support
We assessed how much social support respondents received from their African American gay and bisexual male friends using four items adapted from our previous research [48] that were originally adapted from Procidano and Heller [50]. The decision to assess support from other gay and bisexual friends was based on previous research suggesting that support from these peers is uniquely important for MSM and YBMSM when they are facing HIV-related concerns or challenges [51–53]. The four items include (1) being with these friends helps them feel good about themselves; (2) these friends provide them with helpful information or advice; (3) these friends help solve problems; and (4) they have a deep sharing relationship with these friends. Items were rated on a six-point Likert-type scale from disagree strongly to agree strongly. The items had good internal consistency (Cronbach’s alpha = 0.89; M = 18.37, SD = 5.36) and were used in a composite score.
Resilience
We used the 14-item Wagnild & Young Resilience Scale [42] to measure respondents’ overall resilience that is not specific to their identity. Example items are “I feel that I can handle many things at a time,” and “I can get through difficult times because I’ve experienced difficulty before.” Items were rated on a six-point Likert-type scale from disagree strongly to agree strongly. The items had excellent internal consistency (Cronbach’s alpha = 0.97; M = 73.53, SD = 15.29) and were used as a composite score.
Stimulant Use
Participants reported the number of days in the past 2 months where they used ecstasy, powder cocaine, crack-cocaine or methamphetamine. Each of these substances was collapsed into a binary variable (e.g., use of any ecstasy in the prior 2 months) and then these four variables were used to model the stimulant use latent variable.
Sexual Risk Behavior
Participants were first asked if they had a current boyfriend or lover (i.e., primary partner) and then were asked to report their sexual risk behavior with other sex partners (i.e., not their boyfriend or lover). Such behaviors were measured by three indicators: (1) a 7-point indicator of levels of sexual risk with other men that ranged from: “1 = no sex in past 2 months, 2 = no anal sex in past 2 months, 3 = anal sex with condom only past 2 months, 4 = had condomless anal sex past 2 months with sero-concordant partners only, 5 = had condomless anal sex past 2 months with risk to the insertive partner, 6 = had condomless anal sex past 2 months with risk to the receptive partner, 7 = had condomless anal sex past 2 months with risk to both partners”; (2) and (3) are the numbers of casual condomless anal sex episodes in the past 60 days, insertive and receptive, respectively. Pre-exposure prophylaxis (PrEP) was not factored into our operationalization of sexual risk as it was not available in either Dallas or Houston at the time of data collection.
Statistical Analyses
We used structural equation modeling (SEM) to assess the relationship between the four constructs: minority stress, resilience, stimulant use and sexual risk behavior. The measurement model estimated the latent variables, which are defined by the indicators. The structural model estimated the relationships between the latent constructs. Again, we hypothesized that the effect of minority stress on sexual risk behavior would have a direct pathway, as well as indirect pathways where the relationship is mediated by sources of resilience and stimulant use. We also hypothesized that sources of resilience would have an effect on stimulant use, which in turn affects sexual risk behavior. These mediating effects are tested through three indirect pathways in Fig. 1, which are explained in more detail in the results section.
We conducted SEM using Mplus 8 with maximum likelihood estimation with robust standard errors (i.e. robust to non-normality) of model parameters. For each estimated regression parameter, we report the standardized solution, including the standardized estimate (β), its standard error (SE), and the p value based on the Z-statistic. Age, city, HIV status and income were included as covariates in the models. To evaluate model fit, we report the Root Mean Square Error of Approximation (RMSEA; [54]), Comparative Fit Index (CFI; [55, 56]), and the standardized root mean square residual (SRMR). Satisfactory global model fit is attained when two of the following three conditions are met: CFI ≥ 0.95, RMSEA ≤ 0.06, and SRMR ≤ 0.08 [57].
Results
Participants are described in Table 1. The analytic sample was split evenly across Dallas and Houston and the majority of participants self-identified as gay (78%). Mean age was 24.86 and most had graduated from high school or obtained a GED (86%) and were currently employed part- or full-time (83%). Almost three-quarters of the participants made less than $40,000 annually. One in six participants self-reported an HIV-positive serostatus. More than one in five participants (23%) reported stimulant use in the past 2 months. The two most common stimulants used in the prior 60 days were ecstasy (18%) and powder cocaine (17%). The use of crack cocaine (14%) and methamphetamine (13%) were slightly less common.
Table 1.
Participants’ characteristics (n = 1817)
| % | n | |
|---|---|---|
| Age | ||
| M = 24.86, SD = 2.85 | ||
| City | ||
| Dallas | 50.25 | 913 |
| Houston | 49.75 | 904 |
| Sexual orientation identity | ||
| Gay, homosexual | 77.58 | 1407 |
| Bisexual | 20.29 | 368 |
| Heterosexual | 1.49 | 27 |
| Other | 0.66 | 12 |
| Educational attainment | ||
| Did not complete high school or GED | 14.47 | 258 |
| High school or GED | 23.56 | 420 |
| Some college/associate’s/technical degree | 41.05 | 732 |
| Bachelor’s degree | 16.10 | 287 |
| Any graduate studies | 4.82 | 86 |
| Employment status | ||
| Employed full-time | 64.58 | 1154 |
| Employed part-time | 18.02 | 322 |
| Unemployed | 14.89 | 266 |
| Disability | 2.52 | 45 |
| Income | ||
| < $10,000 | 23.61 | 419 |
| $10,000–$19,999 | 18.54 | 329 |
| $20,000–$39,999 | 31.27 | 555 |
| $40,000–$59,999 | 14.99 | 266 |
| $60,000–$79,999 | 5.75 | 102 |
| $80,000–$99,999 | 2.99 | 53 |
| ≥ $100,000 | 2.87 | 51 |
| HIV serostatus | ||
| HIV-negative | 78.30 | 1407 |
| HIV-positive | 13.24 | 238 |
| Unknown (includes tested, never tested) | 8.46 | 152 |
| Stimulant use in past 60 days | ||
| Ecstasy | 18.36 | 325 |
| Powered cocaine | 16.70 | 294 |
| Crack | 14.23 | 252 |
| Methamphetamine | 13.10 | 232 |
| Sexual risk behavior | ||
| Casual sex risk index in past 60 days | ||
| No sex | 53.36 | 945 |
| No anal sex | 8.81 | 156 |
| Anal with condom only | 15.08 | 267 |
| UAI sero-concordant only | 14.29 | 253 |
| UAI insertive risk | 2.99 | 53 |
| UAI receptive risk | 5.42 | 96 |
| UAI mutual risk | 0.06 | 1 |
| Mean (SD) | n | |
| Casual UAI # times (past 60 days) | 0.64 (3.41) | 1817 |
| Among men with any casual UAI insertive | 2.03 (6.38) | 832 |
| Casual UAR # times (past 60 days) | 0.93 (4.43) | 1817 |
| Among men with any casual UAI receptive | 1.40 (4.94) | 829 |
Overall model fit of the structural equation model was acceptable (χ2 (107) = 450, p < 0.001; CFI = 0.91, RMSEA = 0.05 and SRMR = 0.04). Associations between the control variables and sexual risk behavior were not statistically significant. Figure 2 depicts the estimated paths in Model 1. Paths with solid lines in Fig. 2 indicate statistically significant effects with p < 0.05 and those with dashed lines represent effects that are not statistically significant (p > 0.05). The factor loadings for the measurement model (the latent variables) and the regression coefficients for the structural model are reported in Table 2. For the measurement model, indicator loadings were of moderate to high magnitude (0.52–0.87) and were statistically significant, which together indicate a strong relationship with their respective hypothesized latent constructs. For the structural model, the reported estimates represent the standardized regression coefficients.
Fig. 2.
Measurement and structural model of minority stress, resilience, stimulant use, and sexual risk behavior
Table 2.
Standardized SEM results
| Standardized estimate | SE | P | |
|---|---|---|---|
| Measurement model | |||
| Minority stress | |||
| Homophobia | 0.71 | 0.02 | < 0.001 |
| Racism | 0.64 | 0.02 | < 0.001 |
| Internalized homophobia | 0.70 | 0.02 | < 0.001 |
| Sources of resilience | |||
| Gay/bisexual pride and self-esteem | 0.56 | 0.03 | < 0.001 |
| Social support | 0.58 | 0.03 | < 0.001 |
| Resilience scale | 0.72 | 0.03 | < 0.001 |
| Stimulant use | |||
| Ecstasy | 0.52 | 0.02 | < 0.001 |
| Powder cocaine | 0.67 | 0.02 | < 0.001 |
| Crack cocaine | 0.87 | 0.02 | < 0.001 |
| Methamphetamine | 0.59 | 0.02 | < 0.001 |
| Sexual risk behavior | |||
| Casual sex risk index | 0.57 | 0.04 | < 0.001 |
| Casual UAI # times | 0.69 | 0.04 | < 0.001 |
| Casual UAR # times | 0.71 | 0.04 | < 0.001 |
| Structural model | |||
| Sources of resilience regressed on | |||
| Minority stress (Path D) | − 0.22 | 0.04 | < 0.001 |
| Stimulant use regressed on | |||
| Minority stress (Path A) | 0.03 | 0.03 | 0.37 |
| Sources of resilience (Path E) | − 0.11 | 0.04 | 0.00 |
| Sexual risk behavior regressed on | |||
| Stimulant use (Path C) | 0.19 | 0.04 | < 0.001 |
| Minority stress (Path B) | 0.11 | 0.04 | 0.01 |
| Sources of resilience (Path F) | − 0.11 | 0.05 | 0.02 |
Direct Effects
Sexual risk behavior was associated with each of the three latent predictor variables (stimulant use, minority stress, and resilience). Stimulant use had the largest association with sexual risk behavior (β = 0.19, p < 0.001), followed by the association between minority stress and sexual risk behavior (β = 0.11, p = 0.01). Sources of resilience was negatively associated with sexual risk behavior (β = − 0.11, p = 0.02).
Total Effects
The total indirect effect of minority stress on sexual risk behavior included three unique pathways. These included a path where sources of resilience mediated the association between minority stress on sexual risk behavior, a path where stimulant use mediated the association between minority stress on sexual risk behavior, and a path that included both sources of resilience and stimulant use as mediators between minority stress and sexual risk behavior. Table 3 summarizes the total effects of minority stress on sexual risk behavior. The combined total effect (direct and indirect) is statistically significant (estimated total effect = 0.14, p < 0.05). The indirect effects are shown as three unique pathways in Table 3 (through stimulant use, through sources of resilience, through stimulant use and sources of resilience). The indirect effects summarize the lags that constitute each pathway; each of these lags were also reported independently as β estimates in Table 2.
Table 3.
Total standardized effect of minority stress on sexual risk behavior
| Standardized estimate | SE | P | |
|---|---|---|---|
| Total effect of minority stress on sexual risk behavior | 0.14 | 0.04 | < 0.001 |
| Direct effect (path B) | 0.11 | 0.04 | 0.01 |
| Total indirect effects | 0.04 | 0.01 | 0.01 |
| Through stimulants (paths A and C) | 0.01 | 0.01 | 0.38 |
| Through sources of resilience (paths D and F) | 0.03 | 0.01 | 0.02 |
| Through sources of resilience and stimulant use (paths D, E, and C) | 0.01 | 0.00 | 0.01 |
The first pathway represents the indirect effect of minority stress on sexual risk behavior through stimulant use (paths A and C with βA = 0.03 and βC = 0.19 from Table 1). Although the second lag βC is statistically significant (p < 0.001) suggesting that stimulant use is associated with more sexual risk behavior, the first lag is not statistically significant (p = 0.37). As a result, our testing of the combined indirect effect of minority stress on sexual risk behavior mediated by stimulant use (specifically pathway A and C) shows that this particular indirect effect is not statistically significant (total estimate = 0.01, p = 0.38 from Table 3), and that sources of resilience likely plays a more important role in explaining the significant total indirect effect (estimate = 0.04, p < 0.05) given its influence on the second and the third pathways.
The second pathway consists of paths D and F. This represents the mediating effect of sources of resilience on the path between minority stress and sexual risk behavior. These paths were estimated as βD = − 0.22 and βF = − 0.11 respectively, from Table 2. The combined effect is statistically significant (total indirect effect estimated as 0.03, p < 0.05 from Table 3). This pathway suggests that greater minority stress is associated with lower sources of resilience; lower sources of resilience is associated with increased sexual risk behavior.
The third pathway consists of paths D, E, and C. This combined effect suggests that higher minority stress is associated with less resilience (βD = − 0.22, p < 0.05). Less resilience is associated with more stimulant use (βE = − 0.11, p < 0.05), which in turn is associated with more sexual risk behavior (βC = 0.19, p < 0.05). The total indirect effect of this pathway is estimated as 0.01 with p < 0.05 and is shown at the bottom of Table 3. This pathway suggests that greater minority stress is associated with less resilience, which is associated with more stimulant use; higher levels of stimulant use are associated with higher levels of sexual risk behavior. Pathway (D, E, and C) provides additional sources of influence on stimulant use and sexual risk behavior beyond the direct effect of minority stress on sexual risk behavior (path B) and indirect effect (paths D and F representing effect of minority stress on sexual risk behavior mediated by resilience).
Discussion
Using structural equation modeling, we examined the effect of minority stress on sexual risk behavior, while accounting for the role of resilience sources and stimulant use among YBMSM. Our findings controlled for differences across sociodemographic variables including age, city, income, and HIV status; none of these covariates were significantly associated with sexual risk behavior among these YBMSM. Minority stress was found to be negatively associated with resilience, and resilience was found to be negatively associated with stimulant use and sexual risk behavior. Essentially, these findings suggest that minority stress makes men less resilient, and less resilient men have more sexual risk.
Minority stress was significantly and directly associated with sexual risk behavior among these YBMSM. This finding is consistent with existing research that has demonstrated that minority stress (experiences of homophobia and/or racism, and internalized homophobia) is associated with sexual risk behavior among MSM [30, 58, 59] and that Black MSM may experience multiple layers of stigma [25–27, 60]. We also found that stimulant use was associated with sexual risk behavior. The direct effect of stimulant use on sexual risk behavior was nearly twofold greater than the direct effect of minority stress on sexual risk behavior. This finding may represent the more proximal psychosocial and physiological effects of stimulant use. For example, methamphetamine has well-documented associations with sexual risk behavior among MSM and this relationship is partly attributed to its perceived or actual effects on libido [9, 11, 61]. As a similar but distinct point, we also note the association between stimulant use and sexual risk behavior may also represent the context of use for these substances. That is, YBMSM may be using stimulants in social environments where they meet sexual partners, or using stimulants more proximally in association with sexual behavior itself (i.e., using the drug immediately before or during sex) [13, 15, 62, 63].
We did not find evidence for an association between minority stress and stimulant use among these YBMSM, either before or after accounting for the potential role of sources of resilience in the model. This is in contrast to prior research indicating that minority stress, such as experiences of victimization and discrimination, and internalized homophobia are associated with substance use [11, 14–17]. For example, data from the National epidemiology survey on alcohol and related conditions (NESARC) suggest that sexual minorities who experience multiple forms of discrimination (e.g., homophobia, racism) are at increased risk for substance use disorders [28]. We also did not find evidence for an indirect association, where minority stress would lead to greater stimulant use, which in turn would increase sexual risk behavior. The lack of a direct or indirect effect suggests that in the context of sources of resilience and sexual risk behavior among YBMSM, stimulant use may be a phenomenon distinct from minority stress. While our findings represent one model and are preliminary, they may indicate that overly simplistic models for antecedents of sexual risk taking (e.g., stimulants are used to cope with minority stress, and thus have the secondary effect of increasing sexual risk behavior) are not always sufficient explanations for sexual risk behavior among YBMSM.
Finally, our model suggests several interesting findings related to sources of resilience as a compensatory function [37]. The indicators we incorporated into this latent construct are theoretically informed, with existing evidence for their inclusion as markers of resilience [37, 38, 64]. Indicators included both resilience assets (e.g., individual traits) and resources (e.g., social support) [37]. Importantly, we found that these sources of resilience potentially reduced stimulant use and sexual risk behavior. Sources of resilience was negatively associated with stimulant use, and also negatively associated with sexual risk behavior. The magnitude of its effect on these two risk behaviors was virtually equivalent. This finding aligns with prior research that has shown that sources of resilience such as sexual identity pride, individuals’ resilient traits, and social support are associated with positive outcomes such as better psychosocial health indicators, reduced sexual risk behavior, or increased HIV testing [37–39, 65].
Minority stress was found to be negatively associated with sources of resilience among the YBMSM in this sample. This finding is important because it suggests that minority stress may deplete sources of resilience, and that this depletion is partially responsible for stimulant use and sexual risk behavior among these men. In fact, of all the significant effects in the model, this association had the largest magnitude. In other words, YBMSM who experience more minority stress will have lower levels of protective resilience (in this case, sexual identity pride, social support, and resilient traits). Interventions to increase resilience (again, operationalized as both individual-level assets as well as resources) may have the dual-purpose function of increasing resilience and reducing minority stress, in order to address these interrelated risk factors of stimulant use and sexual risk among YBMSM.
Our findings have caveats related to the directionality and temporality of the associations we tested and identified. With cross-sectional data, is not possible to assess temporality of the associations. Relatedly, it is also not possible to determine the direction of the effects we identified. The model that we tested was empirically informed by the existing body of cross-sectional research in this area; however, other explanations are plausible. It is possible that rather than (or in addition to, in the case of heterogeneous effects) minority stress contributing to stimulant use and/or sexual risk behavior, stimulant use and/or sexual risk behavior might actually exacerbate the risk for experiencing or perceiving minority stress (e.g., homophobia, racism). For example, research has found that methamphetamine use is stigmatized among HIV-positive men [66]. If behaviors such as methamphetamine use or sexual risk behavior violate predominant social norms, men may be socially marginalized, resulting in fewer social supports (in our model, a facet of resilience). Stimulant use may also increase men’s exposure to environments or circumstances where they are at increased risk of homophobia or racism (e.g., incarceration, homelessness). Finally, we also note that the sources of resilience that we incorporated as indicators (sexual identity pride, social support, and resilience) may be factors that either promote resilience, or they may be markers of resilience. For example, peer social support may engender resilience (e.g., peer support is protective against risk); however, peer social support may also be an outcome of resilience (e.g., other resilient traits engender strong social relationships, and thus social support). Future research, especially longitudinal research, should seek to delineate the temporality and direction of associations between minority stress, resilience, substance use, and sexual risk behavior.
Limitations
Our findings should be considered in light of several more general limitations. Our latent variables inherently cannot be observed, and instead consist of proxy indicators of the underlying latent construct. Other observed or unobserved indicators may be more robust indicators of the underlying constructs. Our selection of indicators was empirically and theoretically informed, and the indicators loaded sufficiently (in terms of magnitude and statistical significance) on their respective latent variables. With regard to minority stress, we did not assess internalized racism in the study and therefore we were unable to include it as a variable in our model. Future studies assessing minority stress among YBMSM should include measures of internalized racism. There are also potential limitations in terms of sampling and the data obtained. Data were collected after Mpowerment, a multi-level intervention designed to promote sense of community, empower identity, and reduce sexual risk behavior among YBMSM, had been fully implemented in both cities, potentially limiting the generalizability of these findings to all YBMSM. However, Mpowerment was intended to influence the levels of these variables rather than change the associations between variables. Participants were recruited from two cities in Texas, and from a variety of pre-specified venues. However, venue-based time-location sampling was used to increase the representativeness of the sample with regard to the venues for recruitment. Finally, data were self-reported and subject to social desirability bias. However, participants completed the surveys autonomously on electronic devices to encourage honest responses [46].
Conclusions
Minority stress has been shown to be higher among YMBSM because of the intersectionality of multiple oppressions due to their race and sexual orientation. We found that minority stress and stimulant use are independently and directly associated with sexual risk behavior among YBMSM. However, sources of resilience also have protective effects against stimulant use and sexual risk behavior. Our findings show that minority stressors may deplete resilience. Our findings suggest several areas for future research and intervention development. Minority stress has well-documented and multifaceted effects on the health of YBMSM. Therefore, interventions should focus on addressing discrimination and homophobia at the community-level in order to reduce the structural inequalities that contribute to these socially-produced ills and reductions in resilience among YBMSM. Second, the resilience factors linked to reduced substance use need to be better understood among this population. In order to design future resilience-based interventions for this sub-population of MSM most burdened by HIV, it is vital that research efforts aimed at understanding the risk and protective factors for both substance use and sexual risk behavior are applied to YBMSM. Strengths-based interventions, such as Strengths-Based Case Management [67], have been shown to be effective in reducing problematic substance use. Researchers have also suggested that interventions that seek to increase supportive relationships and a sense of community among YBMSM may be particularly useful for reducing substance use and sexual risk behavior [35, 38, 43].
Acknowledgements
The authors would like to thank Anne Freeman, Douglas Sheehan, and Stephen Brown from the University of Texas Southwestern; and Jan Risser and Paige Padgett from the University of Texas, Houston.
Funding These analyses were supported by National Institutes of Health awards R03DA042660 (PI: Storholm), and R01MH096690 (PI: Kegeles). Dr. Storholm was also supported by R03DA043402, and P30MH058107, and Dr. Vincent was also supported by the National Institute of Mental Health K23MH111402.
Footnotes
Conflict of interest All authors declare that no conflicts of interest exist.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.US Centers for Disease Control and Prevention. HIV among Gay and Bisexual Men: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, 2017. https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/cdc-msm-508.pdf. Accessed 15 Aug 2018. [Google Scholar]
- 2.US Centers for Disease Control and Prevention. HIV Among African American Gay and Bisexual Men: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, 2018. https://www.cdc.gov/hiv/group/msm/bmsm.html. Accessed 15 Aug 2018. [Google Scholar]
- 3.Colfax G, Coates TJ, Husnik MJ, Huang Y, Buchbinder S, Koblin B, et al. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. J Urban Health. 2005;82(1):62–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mattison AM, Ross MW, Wolfson T, Franklin D. Circuit party attendance, club drug use, and unsafe sex in gay men. J Subst Abuse. 2001;13(1–2):119–26. [DOI] [PubMed] [Google Scholar]
- 5.Halkitis PN, Moeller RW, Siconolfi DE, Storholm ED, Solomon TM, Bub KL. Measurement model exploring a syndemic in emerging adult gay and bisexual men. AIDS Behav. 2013;17(2):662–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halkitis PN, Parsons JT, Stirratt MJ. A double epidemic: crystal methamphetamine drug use in relation to HIV transmission among gay men. J Homosex. 2001;41(2):17–35. [DOI] [PubMed] [Google Scholar]
- 7.Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, et al. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20(5):731–9. [DOI] [PubMed] [Google Scholar]
- 8.Storholm ED, Fisher DG, Napper LE, Reynolds GL, Halkitis PN. A psychometric analysis of the compulsive sexual behavior inventory. Sex Addict Compuls. 2011;18(2):86–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shoptaw S, Reback CJ. Methamphetamine use and infectious disease-related behaviors in men who have sex with men: implications for interventions. Addiction. 2007;102(s1):130–5. [DOI] [PubMed] [Google Scholar]
- 10.Woolf SE, Maisto SA. Alcohol use and risk of HIV infection among men who have sex with men. AIDS Behav. 2009;13(4):757–82. [DOI] [PubMed] [Google Scholar]
- 11.Halkitis PN, Levy MD, Moreira AD, Ferrusi CN. Crystal methamphetamine use and HIV transmission among gay and bisexual men. Curr Addict Rep. 2014;1(3):206–13. [Google Scholar]
- 12.Kelly JA, St Lawrence JS, Tarima SS, DiFranceisco WJ, Amirkhanian YA. Correlates of sexual HIV risk among African American men who have sex with men. Am J Public Health. 2016;106(1):96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mimiaga MJ, Reisner SL, Fontaine YM, Bland SE, Driscoll MA, Isenberg D, et al. Walking the line: stimulant use during sex and HIV risk behavior among Black urban MSM. Drug Alcohol Depend. 2010;110(1–2):30–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wong CF, Weiss G, Ayala G, Kipke MD. Harassment, discrimination, violence, and illicit drug use among young men who have sex with men. AIDS Educ Prev. 2010;22(4):286–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harawa NT, Williams JK, Ramamurthi HC, Manago C, Avina S, Jones M. Sexual behavior, sexual identity, and substance abuse among low-income bisexual and non-gay-identifying African American men who have sex with men. Arch Sex Behav. 2008;37(5):748–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jerome RC, Halkitis PN. Stigmatization, stress, and the search for belonging in Black men who have sex with men who use methamphetamine. J Black Psychol. 2009;35(3):343–65. [Google Scholar]
- 17.Kecojevic A, Wong CF, Corliss HL, Lankenau SE. Risk factors for high levels of prescription drug misuse and illicit drug use among substance-using young men who have sex with men (YMSM). Drug Alcohol Depend. 2015;150:156–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alessi EJ. Changing directions in HIV prevention: the move toward a psychosocial model. J Gay Lesbian Soc Serv. 2008;20(4):273–87. [Google Scholar]
- 19.Meyer IH. Minority stress and mental health in gay men. J Health Soc Behav. 1995;36(1):38–56. [PubMed] [Google Scholar]
- 20.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vincke J, Bolton R. Social support, depression, and self-acceptance among gay men. Hum Relat. 1994;47:1049–62. [Google Scholar]
- 22.Herek GM. The psychology of sexual prejudice In: Garnets LD, Kimmel DC, editors. Psychological perspectives on lesbian, gay, and bisexual experiences. 2nd ed. New York: Columbia University Press; 2003. p. 157–64. [Google Scholar]
- 23.Cochran SD, Mays VM. Depressive distress among homosexually active African American men and women. Am J Psychiatry. 1994;151(4):524–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peterson JL, Jones KT. HIV prevention for Black men who have sex with men in the United States. Am J Public Health. 2009;99(6):976–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilson PA, Valera P, Martos AJ, Wittlin NM, Munoz-Laboy MA, Parker RG. Contributions of qualitative research in informing HIV/AIDS interventions targeting Black MSM in the United States. J Sex Res. 2016;53(6):642–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Storholm ED, Halkitis PN, Kupprat SA, Hampton MC, Palamar JJ, Brennan-Ing M, et al. HIV-related stigma as a mediator of the relation between multiple-minority status and mental health burden in an aging HIV-positive population. J HIV AIDS Soc Serv. 2013;12(1):9–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quinn K, Dickson-Gomez J, DiFranceisco W, Kelly JA, St Lawrence JS, Amirkhanian YA, et al. Correlates of internalized homonegativity among black men who have sex with men. AIDS Educ Prev. 2015;27(3):212–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCabe SE, Bostwick WB, Hughes TL, West BT, Boyd CJ. The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. Am J Public Health. 2010;100(10):1946–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stall R, Friedman M, Catania JA. Interacting epidemics and gay men’s health: a theory of syndemic production among urban gay men. Unequal Oppor. 2008;1:251–74. [Google Scholar]
- 30.Amola O, Grimmett MA. Sexual identity, mental health, HIV risk behaviors, and internalized homophobia among Black men who have sex with men. J Couns Dev. 2015;93(2):236–46. [Google Scholar]
- 31.Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34(1):37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Storholm ED, Halkitis PN, Siconolfi DE, Moeller RW. Cigarette smoking as part of a syndemic among young men who have sex with men ages 13–29 in New York City. J Urban Health. 2011;88(4):663–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kurtz SP, Buttram ME, Surratt HL, Stall RD. Resilience, syndemic factors, and serosorting behaviors among HIV-positive and HIV-negative substance-using MSM. AIDS Educ Prev. 2012;24(3):193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rabkin JG, Remien R, Williams JB, Katoff L. Resilience in adversity among long-term survivors of AIDS. Psychiatr Serv. 1993;44(2):162–7. [DOI] [PubMed] [Google Scholar]
- 35.Herrick AL, Lim SH, Wei C, Smith H, Guadamuz T, Friedman MS, et al. Resilience as an untapped resource in behavioral intervention design for gay men. AIDS Behav. 2011;15(Suppl 1):S25–9. [DOI] [PubMed] [Google Scholar]
- 36.Herrick AL, Stall R, Goldhammer H, Egan JE, Mayer KH. Resilience as a research framework and as a cornerstone of prevention research for gay and bisexual men: theory and evidence. AIDS Behav. 2014;18(1):1–9. [DOI] [PubMed] [Google Scholar]
- 37.Wilson PA, Meyer IH, Antebi-Gruszka N, Boone MR, Cook SH, Cherenack EM. Profiles of resilience and psychosocial outcomes among young Black gay and bisexual men. Am J Commun Psychol. 2016;57(1–2):144–57. [DOI] [PubMed] [Google Scholar]
- 38.Reed SJ, Miller RL. Thriving and adapting: resilience, sense of community, and syndemics among young Black Gay and bisexual men. Am J Commun Psychol. 2016;57(1–2):129–43. [DOI] [PubMed] [Google Scholar]
- 39.Scott HM, Pollack L, Rebchook GM, Huebner DM, Peterson J, Kegeles SM. Peer social support is associated with recent HIV testing among young black men who have sex with men. AIDS Behav. 2014;18(5):913–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilson PA, Nanin J, Amesty S, Wallace S, Cherenack EM, Fullilove R. Using syndemic theory to understand vulnerability to HIV infection among Black and Latino men in New York City. J Urban Health. 2014;91(5):983–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wong CF, Schrager SM, Holloway IW, Meyer IH, Kipke MD. Minority stress experiences and psychological well-being: the impact of support from and connection to social networks within the Los Angeles house and ball communities. Prev Sci. 2014;15(1):44–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wagnild GM, Young HM. Development and psychometric evaluation of the resilience scale. J Nurs Meas. 1993;1(2):165–78. [PubMed] [Google Scholar]
- 43.Hays RB, Rebchook GM, Kegeles SM. The Mpowerment Project: community-building with young gay and bisexual men to prevent HIV. Am J Commun Psychol. 2003;31(3–4):301–12. [DOI] [PubMed] [Google Scholar]
- 44.Vincent W, Pollack LM, Huebner DM, Peterson JL, Steward WT, Rebchook GM, et al. HIV risk and multiple sources of heterosexism among young Black men who have sex with men. J Consult Clin Psychol. 2017;85(12):1122–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men–a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(Suppl 1):39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gorbach PM, Mensch BS, Husnik M, Coly A, Masse B, Makanani B, et al. Effect of computer-assisted interviewing on self-reported sexual behavior data in a microbicide clinical trial. AIDS Behav. 2013;17(2):790–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Díaz RM, Ayala G, Bein E. Sexual risk as an outcome of social oppression: data from a probability sample of Latino gay men in three U.S. cities. Cultur Divers Ethnic Minor Psychol. 2004;10(3):255–67. [DOI] [PubMed] [Google Scholar]
- 48.Kegeles SM, Hays RB, Coates TJ. The Mpowerment project: a community-level HIV prevention intervention for young gay men. Am J Public Health. 1996;86(8_Pt_1):1129–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nungesser LG. Homosexual acts, actors, and identities. Westport: Praeger Publishers; 1983. [Google Scholar]
- 50.Procidano ME, Heller K. Measures of perceived social support from friends and from family: three validation studies. Am J Commun Psychol. 1983;11(1):1–24. [DOI] [PubMed] [Google Scholar]
- 51.Brady SS, Dolcini MM, Harper GW, Pollack LM. Supportive friendships moderate the association between stressful life events and sexual risk taking among African American adolescents. Health Psychol. 2009;28(2):238–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hays RB, Catania JA, McKusick L, Coates TJ. Help-seeking for AIDS-related concerns: a comparison of gay men with various HIV diagnoses. Am J Commun Psychol. 1990;18(5):743–55. [DOI] [PubMed] [Google Scholar]
- 53.Peterson JL, Coates TJ, Catania JA, Hilliard B, Middleton L, Hearst N. Help-seeking for AIDS high-risk sexual behavior among gay and bisexual African-American men. AIDS Educ Prev. 1995;7(1):1–9. [PubMed] [Google Scholar]
- 54.Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociol Methods Res. 1992;21(2):230–58. [Google Scholar]
- 55.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238–46. [DOI] [PubMed] [Google Scholar]
- 56.Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88(3):588–606. [Google Scholar]
- 57.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. [Google Scholar]
- 58.Jeffries WLT, Marks G, Lauby J, Murrill CS, Millett GA. Homophobia is associated with sexual behavior that increases risk of acquiring and transmitting HIV infection among black men who have sex with men. AIDS Behav. 2013;17(4):1442–53. [DOI] [PubMed] [Google Scholar]
- 59.Frye V, Nandi V, Egan J, Cerda M, Greene E, Van Tieu H, et al. Sexual orientation- and race-based discrimination and sexual HIV risk behavior among urban MSM. AIDS Behav. 2015;19(2):257–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, et al. HIV among black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav. 2014;18(1):10–25. [DOI] [PubMed] [Google Scholar]
- 61.Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16(6):1394–410. [DOI] [PubMed] [Google Scholar]
- 62.Jerome RC, Halkitis PN, Siconolfi DE. Club drug use, sexual behavior, and HIV seroconversion: a qualitative study of motivations. Subst Use Misuse. 2009;44(3):431–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Palamar JJ, Kiang MV, Storholm ED, Halkitis PN. A qualitative descriptive study of perceived sexual effects of club drug use in gay and bisexual men. Psychol Sex. 2014;5(2):143–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Buttram ME. The social environmental elements of resilience among vulnerable African American/Black men who have sex with men. J Hum Behav Soc Environ. 2015;25(8):923–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.McNair OS, Gipson JA, Denson D, Thompson DV, Sutton MY, Hickson DA. The associations of resilience and HIV risk behaviors among Black gay, bisexual, other men who gave sex with men (MSM) in the deep South: the MARI Study. AIDS Behav. 2018;22(5):1679–87. [DOI] [PubMed] [Google Scholar]
- 66.Semple SJ, Strathdee SA, Zians J, Patterson TL. Factors associated with experiences of stigma in a sample of HIV-positive, methamphetamine-using men who have sex with men. Drug Alcohol Depend. 2012;125(1–2):154–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Brun C, Rapp RC. Strengths-based case management: individuals’ perspectives on strengths and the case manager relationship. Soc Work. 2001;46(3):278–88. [DOI] [PubMed] [Google Scholar]