Abstract
Background:
Lung ultrasound is a useful tool in the assessment of pulmonary congestion in heart failure that is typically performed and interpreted by physicians at the point-of-care.
Aims:
To investigate the ability of nurses, students, and paramedics to accurately identify B-lines and pleural effusions for the detection of pulmonary congestion in heart failure and to examine the training necessary.
Methods and results:
We conducted a systematic review and searched online databases for studies that investigated the ability of nurses, students, and paramedics to perform lung ultrasound and detect B-lines and pleural effusions. Of 979 studies identified, 14 met our inclusion criteria: five in nurses, eight in students, and one in paramedics. After 0–12 h of didactic training and 58–62 practice lung ultrasound examinations, nurses were able to identify B-lines and pleural effusions with a sensitivity of 79–98% and a specificity of 70–99%. In image adequacy studies, medical students with 2–9 h of training were able to acquire adequate images for B-lines and pleural effusions in 50–100%. Only one eligible study investigated paramedic-performed lung ultrasound which did not support the ability of paramedics to adequately acquire and interpret lung ultrasound images after 2 h of training.
Conclusions:
Our findings suggest that nurses and students can accurately acquire and interpret lung ultrasound images after a brief training period in a majority of cases. The examination of heart failure patients with lung ultrasound by non-clinicians appears feasible and warrants further investigation.
Keywords: Heart failure, lung ultrasound, nurse, ultrasound education
Introduction
The careful assessment and management of congestion is an important yet difficult challenge in patients with heart failure.1,2 Lung ultrasound (LUS) enables detection of pulmonary congestion in heart failure with higher sensitivity than auscultation or chest X-ray, and an increased number of LUS findings are associated with worse prognosis in heart failure patients.3–5 In the current European Society of Cardiology heart failure guidelines LUS is mentioned as a class IIb, level C recommendation in the diagnostic evaluation of patients with acute heart failure.6 The technique involves examining the chest wall to identify vertical artifacts originating at the pleural line (B-lines). Ultrasound can also be utilized to detect pleural effusions. Currently, LUS is used primarily by physicians at the point-of-care, and this rapid technique is relatively easy to learn.7,8 Both in the US and Europe, nurses are managing heart failure patients in conjunction with physicians.9–12 Furthermore, in resource-limited settings, nurses and community health workers may represent the primary providers for both acute and chronic heart failure patients. LUS performed by these providers may allow for lower-cost and more effective management of these patients.
The goal of this systematic review was to investigate the ability of nurses, students, and paramedics to accurately identify B-lines and pleural effusions, and to determine the extent of training necessary. By examining the ability of these providers to learn LUS, including medical students who have limited clinical experience, we aimed to investigate the feasibility of task-shifting towards LUS performed by non-physician providers in heart failure patients. Our hypothesis was that nurses, students, and paramedics can learn LUS within a relatively short training period.
Methods
Literature search strategy
A medical librarian searched PubMed, EMBASE, and Web of Science on 2 February 2018 and removed duplicates. The search strategy includes both MeSH and free-text terms in the title and abstract, such as “Ultrasound”, “Heart Failure”, “Medical Student”, “Nurse”, and “Emergency Medical Technician” (see Supplementary Material online). Two investigators (VS and PB) independently reviewed the search results, with discrepancies resolved by a third researcher with extensive LUS experience (EP).
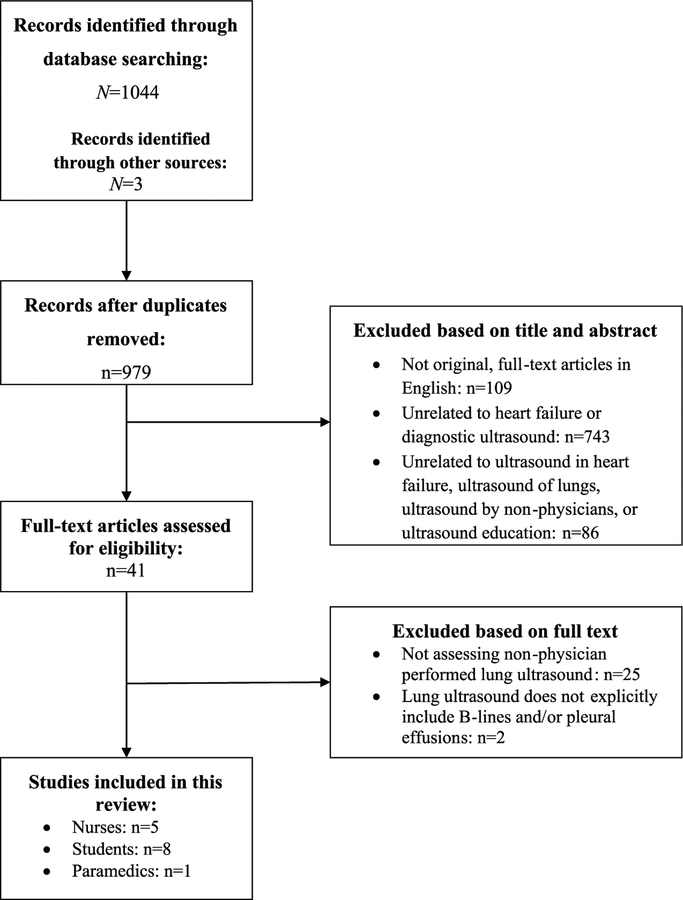
We included full-text articles that involved nurses, medical students, and paramedics with none or only minimal ultrasound experience performing LUS to identify B-lines and pleural effusions. We excluded studies in which LUS was solely utilized for hemothorax or pneumothorax detection, and studies that did not assess image adequacy and/or diagnostic accuracy of LUS examinations. Search results were initially screened based on title and abstract (Figure 1). Abstracts, literature reviews, case reports, editorials, poster presentations, and letters to the editor were excluded. We employed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Flow Diagram 2009 checklist to describe our methodology and findings (Supplementary Material Table 1).13 The protocol for this systematic review was registered on PROSPERO (CRD42018087857).
Figure 1.
PRISMA Flow Diagram.
Eligible studies were divided into three groups: training and performance of LUS by nurses (n=5), students (n=8), and paramedics (n=1). We utilized an NIH Quality Assessment tool to assess study methodology in regard to the appropriateness of the study sample, clarity of objectives and methodology, and results reporting. Two investigators (VS and PB) independently rated each of the 12 questions for each study, in addition to an overall score, with discrepancies in the overall score resolved by a third reviewer (EP) (Supplementary Material Tables 3.1–3.4).14
Data extraction and statistical analyses
Data from each study were extracted by one investigator (VS), verified by a second investigator (PB), and reported in Tables 1–3 and in the Supplementary Material. We collected information regarding the study design, objectives, ultrasound and training methodologies, and diagnostic accuracy. Where necessary, we contacted corresponding authors to clarify information (n=3). Included studies were reviewed for potential sources of bias that may have impacted upon the main results.
Table 1.
Nurse-performed lung ultrasound.
| First author Year Country | Patients n | Patient population | Nurses n | LUS goal | # Zones | Positive zone Positive overall | Didactic training; hands-on training | Reference standard | Diagnostic accuracy Sensitivity (95% CI) Specificity (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| Ünlüer 201419 Turkey | 90 | ED, dyspnea | 2 | B-lines | Six? | B-lines in four zones based on predefined protocol20 | 3 h; 60 scans | Expert medical record review (blinded to nurse LUS) | Nurse 1: Sens. 95% (84.2–99.4) Spec. 96% (85.5–99.5) Nurse 2: Sens. 100% (9I.8–100.0) Spec. 100% (92.5–100.0) |
| Dalen 201515 Norway | 62 | Outpatient HF clinic, routine follow-up care | 2 | Pleural effusion | Six | Three categories: ‘0’ ‘5 mm’b ‘>5 mm’ |
0 h; 15–20 scansd | Expert LUS | Sens. 92% Spec. 99% |
| Graven 201516 Norway | 59 | Inpatient, median 5 days postcardiac surgery | 2 | Pleural effusion | Eight | Four categories: Not present Insignificantb Moderate Largec |
0 h; three months’ bedside education with 58 and 62 scans each | Expert LUS | Sens. 98% Spec. 70% |
| Gustafsson 201517 Sweden | 104 | Outpatient HF clinic, routine follow-up care | 4 | B-lines, pleural effusion | Seven | ≥ 3 B-lines in one zone Evidence of pleural effusion | 3 h (extra material given); 1 h | Expert image review (blinded to other clinical findings) | B-lines: Sens. 79% (59–91) Spec. 9I% (81–96) Pleural effusion: Sens. 88% (50–99) Spec. 93% (85–97) |
| Mumoli 201618 Italy | 226 | ED, acute dyspneaa | 5 | B-lines | Eight | ≥ 3 B-lines in one zone B-lines in ≥ 2 zones bilaterally | 12 h; 20 h | Expert medical record review (blinded to nurse LUS) | Sens. 95% (93–98) Spec. 88% (84–92) |
Shortness of breath with RR >24 breaths per minute, or O2 saturation < 92%, or had been started on O2 therapy.
If seen in costodiaphragmatic angle only.
Moderate: if pleural effusion separated the diaphragm and the lung with a maximum distance of < 30 mm; large: if maximum distance <30 mm.
Nurses had each completed ~200 ultrasound scans prior to the study period.
LUS: lung ultrasound; CI: confidence interval; ED: Emergency Department; HF: heart failure; Sens.: sensitivity; Spec.: specificity.
Table 3.
Student-performed LUS on patients.
| First author Year Country | Patients n (# of LUS exams) | Patient population | Students n (school year) | LUS aim | # zones | Positive one Positive overall | Didactic training; hands-on training | Reference standard | Image adequacy and diagnostic accuracy |
|---|---|---|---|---|---|---|---|---|---|
| Mai 201324 United States | 27 (5) | Outpatient cardiology and healthy volunteers who were asymptomatic | 3 (not reported) | B-lines | Two | ≥ 3 B-lines B-lines in ≥ 1 lung apices | 0 h; < 1 h brief device orientation | Expert LUS and image review | Image adequacy: 100% Diagnostic accuracy: Sens. 40%, Spec. 100% |
| Andersen 201421 Norway | 211 (59) | Inpatients and outpatients | 30 (5) | B-lines, pleural effusion | Two | Not reported | < 1 h; ~8 h (including all POC techniques) | Expert image review | Image adequacy: 93% (95% CI: 84.3–98.2) Diagnostic accuracy: Sens. 90.5% (95% CI: 68.8–97.6), Spec. 94.7% (95% CI: 82.2–99.4) |
| Udrea 201726 United States | 482 (47) | ED, patients requiring lung exam, and healthy volunteers | 5 (1) | B-lines, pleural effusion | Six | ≥ 3 B-lines Evidence of pleural effusion | 18 h; ~13 h (including all POC techniques) | Expert image review | Agreement with expert diagnosis: 95.7% |
LUS: lung ultrasound; CI: confidence interval; POC: point of care; ED: Emergency Department; Sens.: sensitivity; Spec.: specificity
Authors used mainly descriptive statistics to summarize their findings. Image adequacy and agreement with physician interpretation as the reference standard are reported as percentages, diagnostic accuracy is reported as sensitivity and specificity with 95% confidence intervals, and written examination results are reported as mean test scores and standard deviations as reported in the studies. Where possible, outcomes in each subcategory (nurses, students, paramedics) are aggregated as percentage ranges. p values <0.05 were considered statistically significant.
Results
Our search yielded 979 unduplicated publications, 14 of which were included in this review. These studies were conducted between 2011 and 2015, and took place across North America, Europe, Asia, and Africa. The number of participants ranged from N=2 to N=195 and the number of patients ranged from N=5 to N=226. The number of lung zones examined and definitions of a positive lung zone, positive exam, and degree of pleural effusion varied (Tables 1–4). A list of inclusion and exclusion criteria for each study is provided (see Supplementary Material).
Table 4.
Paramedic-performed LUS.
| First author Year Country | Patients n | Patient population | Paramedics n | LUS aim | # zones | Positive zone Positive overall | Didactic training; hands-on training | Reference standard | Image adequacy and Diagnostic accuracy |
|---|---|---|---|---|---|---|---|---|---|
| Becker 201829 United States | 25 | Ambulance, undifferentiated respiratory distressa | 17 | B-lines | Four (continuous clips of anterior and lateral chest) | Predominance of B-lines based on predefined protocol28 |
0.5 hours plus extra material and refresher-training offered; 1.5 hours | Expert image review | Image adequacy: 41.2% Agreement with expert diagnosis: 62.5% |
Complaints of shortness of breath, or objective signs of respiratory distress, or non-invasively measured SpO2 < 92%. LUS: lung ultrasound; SpO2: oxygen saturation.
Nurses
Five studies investigated the feasibility of nurse-performed LUS15–19 (Table 120). The number of nurses ranged from n=2 to n=5. The duration of didactic training ranged from 0 to 12 h, and hands-on training ranged from 58 to 62 practice LUS examinations.
Two studies involved specialized nurse-led outpatient heart failure clinics.15,17 Nurses in one of these studies had prior experience performing ultrasound of the pleural space prior to study start.15 When compared with LUS performed by an expert or with expert review of the nurses’ images, the studies reported a sensitivity ranging from 88% to 92% and specificity from 93% to 99% for nurses to detect pleural effusions. Heart failure nurses detected B-lines with a sensitivity of 79% and specificity of 91% based on the expert review of nurses’ images.17 In another study, cardiology nurses were able to identify clinically significant pleural effusions in hospitalized patients following cardiac surgery with 98% sensitivity and 70% specificity when compared with expert-performed LUS.16 Two studies, using physician medical record review as the reference standard, found that internal medicine and emergency medicine nurses could use LUS to identify a cardiac etiology in patients presenting with undifferentiated dyspnea by detecting B-lines with sensitivities ranging from 95% to 100% and specificities ranging from 88% to 100%.18,19 One of these studies also examined the diagnostic accuracy of combining nurse-performed LUS with brain natriuretic peptide levels (suspected cardiogenic dyspnea cut-off levels ≥ 400 pg/mL), reporting a sensitivity of 99% and specificity of 92% for detecting B-lines as compared with physician medical record review.18
Several methodological aspects should be considered with respect to these studies. The time required to perform LUS was specified in two studies, and ranged from <2 to 4 min.18,19 The number of lung zones examined ranged from six to eight. One study characterized an examination as positive for pulmonary congestion if three or more B-lines were found in two or more zones.18 In another study, three or more B-lines total indicated pulmonary congestion.17 One study utilized the LUS findings based on a comprehensive, pre-defined protocol.19,20 Pleural effusions were categorized as “not present” or “insignificant” or “significant”.15,16 In one study, pleural effusions were considered present if found bilaterally.17
Students
Eight studies explored whether ultrasound-inexperienced students in the medical field could identify and interpret B-lines and pleural effusions.21–28 We categorized these studies to differentiate whether LUS was performed on (1) standardized patients (i.e. actors), healthy volunteers, and training simulators, or (2) actual patients. The number of participating students ranged from n=3 to n=195, and their years in medical school ranged from first to fifth (of six) year of education. Assessment was based on either expert imaging or expert evaluation of students’ skills and/or images. In two studies, the experts were unblinded to the diagnoses.21,26 Where reported, the number of lung zones examined ranged from two to six.21–26
Five of the eight studies involved students acquiring LUS clips on standardized patients, healthy volunteers, and simulators (Table 2).22,23,25,27,28 Where reported, didactic training time ranged from 1 to 8 h.22,23,27,28 The mean duration of hands-on training was 1.25 h (range 1–2 h). Three of these reported average image acquisition adequacy rates ranging from 87% to 100%.22,25,28 Using clips of both normal and pathological lung findings, one study used a test to assess the students’ ability to interpret LUS. Students demonstrated a significant improvement in the percentage of correct answers on the test (pre-training: 42.1%, post-training: 82.6%, p<0.001).23 When the post-test scores of medical students were compared with those of Emergency Medicine residents, no significant difference was found (p=0.33).
Table 2.
Student-performed LUS on healthy volunteers or simulators.
| First author Year Country | Models | Students n | School year | LUS goal | # zones | Didactic training; hands-on training | Reference standard | Image adequacy and clinical knowledge test scores |
|---|---|---|---|---|---|---|---|---|
| Connolly 201 527 United States | Simulation | 22 | Not reported | B-lines, pleural effusion | ? | 4 h of online didactic material; 1 h | Expert image review | Image adequacy: pre-training 23%, post-training 51%; improved by 2.6 (1.1–4.2) points (p=0.003*) Test scores: pre-training 8.4, post-training 18.5 of 21 points (p<0.001*) |
| Eissa 201528 United States | Simulation | 70 | 3 | B-lines, pleural effusion | ? | 1 h; 1 h | Not reported | Image adequacy: pre-training 52.1% ± 18.5, post-training 87.3% ± 13.9 (p<0.001*) |
| Heiberg 201522 South Africa | Healthy volunteers | 16 | 3–5 | Pleural effusion | Two | 5–8 h of e-learning (including all POC modules);1 h | Expert image review | Image adequacy: right: pretraining 31%, post-training 100% (p<0.01*). Left: pretraining 13%, post-training 50% (p<0.02, not significant) |
| Steinmetz 201625 Canada | Standardized patients | 195 | 1 | B-lines | Three | Text and video; 1 h | Expert image review | Image adequacy: 100% |
| Lim 201723 South Korea | Healthy volunteers | 40 | 4 | B-lines, pleural effusion | Six | 1 h; 2 h | Expert image review | Image adequacy: 96% Test scores: pre-training 42.1 ± 13.7%, post-training 82.6 ± 10.7% (p<0.001*) |
Statistically significant.
LUS: lung ultrasound; POC: point of care.
Another study reported that, after training, there was a significant improvement in the number of students who attained interpretable images of the right pleural view (baseline: 51%, e-learning: 56%, e-learning and hands-on training: 100%), but not the left (p<0.01).22 A third study found that, for medical and physician assistant students utilizing an ultrasound simulator, clinical knowledge improved from a mean of 8.4 out of 21 possible points at baseline to a mean of 18.5 points (p<0.001) after training.27 While there was a significant improvement in image adequacy, 48% of the images were still considered inadequate after training (p=0.003).
Methodologies across these studied varied. One study did not differentiate the training time dedicated to the identification of B-lines and pleural effusion from that of focused transthoracic echocardiography training.27 The teacher–student ratio was reported in two studies as 1:4 and in one study as 1:5.22,25,27 Time required to perform LUS was not reported in these studies.
Students performed LUS on patients in three studies (Table 3).21,24,26 Two explored whether students could learn to identify B-lines and pleural effusions as part of a larger point-of-care ultrasound training program.21,26 Since only the overall training time was reported, the time dedicated to LUS training is unclear. One of these studies noted that students were able to detect pleural effusion and B-lines in inpatients and outpatients with a sensitivity of 91% and a specificity of 95%, using expert sonographers as the gold standard.21 The other study, including patients in the Emergency Department (ED), patients who required lung examinations, and healthy volunteers, reported a 96% physician agreement with students’ image interpretation based on LUS findings.26 These studies did not report the time required to perform LUS.
The third study assessed the ability of a medical student, pharmacy resident, and medical intern to perform a limited cardiac ultrasound on asymptomatic outpatient cardiology patients and healthy volunteers with remote, real-time guidance and without formal training. Using pocket-sized ultrasound devices, the trainees acquired lung images with a technical adequacy of 100%. Their images yielded interpretable results for the detection of B-lines with a sensitivity of 40% and specificity of 100% as compared with images acquired by sonographers with high-end ultrasound systems.24 The total time required to acquire the series of cardiac views, in addition to lung views, was 5 min. The results reported for the medical student were reported in aggregate with those of the pharmacy resident and medical intern.
Teacher–student ratios were not reported for these studies. Only two studies reported specific LUS interpretation methods. A positive zone was defined as three or more B-lines, and one study further specified that LUS was positive for pulmonary congestion if at least one (of two total) zones was positive.24,26 Pleural effusions were categorized as either present or absent on each side.26
Paramedics
One study investigated whether paramedics could perform LUS in patients with shortness of breath or objective signs of respiratory distress during transport in an urban setting29 (Table 4). Participants (n=17) attended a 30-min lecture followed by 1.5 h of hands-on training. They were also offered a refresher course and supplementary material. Four lung zones of the anterior and lateral chest were examined. Time required to perform LUS was not reported. Among 25 patients, 59% of paramedic-performed examinations were deemed uninterpretable by expert sonographers, many due to over-gained images. Sixty-three percent of the interpretable examinations correlated with the final ED diagnosis of patients in the study. Paramedics were also asked to provide an overall impression of the lung (“dry” vs. “wet”) based on a pre-specified ultrasound protocol.30 Their interpretation was compared with the final ED diagnosis of a subset (n=15) of patients (Cohen’s kappa = 0.74). This study did not meet its pre-defined endpoint of a >80% rate of interpretable paramedic-performed LUS images.
Discussion
To our knowledge, this is the first systematic review investigating the ability of nurses, students, and paramedics to identify B-lines and pleural effusions on ultrasound. We found that nurses and – in a majority of cases – students can correctly identify B-lines and pleural effusions following 0–12 h of didactic training and 58–62 practice examinations and approximately 2–9 h of training, respectively. Only one study investigated paramedic-performed LUS, in which paramedics were struggling to identify B-lines and pleural effusions after 2 h of training.
We did not note any obvious differences in the abilities of participants to perform LUS across inpatient, outpatient, ED, and simulation settings. Apart from one study, all study participants had little to no background in ultrasound and varied in knowledge and experience related to heart failure.13 These findings suggest that, after a relatively short training period, nurses, students, and paramedics can accurately learn to detect B-lines and pleural effusions by LUS.
Nurses
Nurse-performed LUS has the potential to improve outcomes in patients with heart failure by enhancing both the detection of subclinical pulmonary congestion and resultant management of congestion across a variety of settings.
Prior research has demonstrated that nurses can learn to perform and interpret inferior vena cava (IVC) ultrasound examinations with moderate to good agreement with expert sonographers.31–33 One study in this current review found that nurse–expert correlation was greater for detecting B-lines and pleural effusions than for measuring the IVC diameter, suggesting that identifying B-lines and pleural effusions may be easier to learn than other ultrasound examinations.17
One study demonstrated that the diagnostic accuracy of nurse-performed LUS had higher sensitivity and negative predictive value when combined with brain natriuretic peptide levels in patients presenting to the ED with acute dyspnea.18 Thus, the utility of nurse-performed LUS may prove to be even greater in the clinical context, wherein imaging results do not stand alone but rather serve as an additional data point in the patient assessment.
Prior research has demonstrated that nurse-led heart failure clinics can contribute to the reduction of unplanned heart failure hospitalizations.10,15,17,34,35 Coupling this strategy with nurse-performed ultrasound of the pleural space and lungs to monitor pulmonary congestion has the potential to further improve outcomes and possibly decrease costs.
In resource-limited settings, nurses may screen for and manage common illnesses to allow patients to receive timely care.36–38 Nurse-performed LUS could contribute to improved access to care in areas where, for instance, local health centers are significantly closer than the nearest hospital.
Students
The ability of students to perform and interpret LUS suggests that, after a short training period, LUS can be learned even with minimal clinical experience. In fact, two studies in this review involved first-year medical students, in the context of basic anatomy and physiology didactics. In studies that included other point-of-care ultrasound examinations, students performed better in LUS compared with cardiac and gallbladder ultrasound examinations, suggesting that LUS might be relatively easier to learn.21,26 Given that medical students with little to no clinical experience are able to perform and interpret LUS, shifting this task to other healthcare professionals, including nurses, could prove to be a feasible intervention.
One study examined changes in patient management that occurred before and after physician review of students’ ultrasound images.26 However, the impact on diagnosis and management was reported for only combined student-performed point-of-care ultrasound examinations rather than LUS alone. Future research is needed to investigate how student-performed LUS may impact the assessment and management of patients with known or suspected heart failure.
Paramedics
As the first point-of-contact for 15% of patients who visit the ED in the US, paramedics seem to be ideally suited to learn LUS for improved pre-hospital management of acutely dyspneic patients.39 In the study identified in this review, the low paramedic–patient ratio suggests that each paramedic performed few examinations. Perhaps with a greater number of patients and longer training, paramedic-performed LUS could be feasible as other paramedic-performed ultrasound examinations have been previously shown.40–47 Heegaard et al. detail a one-year training period consisting of didactic and hands-on instruction in which paramedics were able to perform adequate Focused Assessment with Sonography in Trauma (FAST) and abdominal aortic (AAA) examinations.42 LUS is a simple technique, and implementing a training method similar to that utilized in this study may yield more promising results.
Furthermore, paramedic-performed LUS might be even more useful in non-urban settings in which transportation times are longer and pre-hospital assessment has a greater impact on patient management. Further research is needed to investigate the feasibility of paramedic-performed LUS, ideally with more extensive training.
Implications
While the studies included in this review are small and should be supported by future larger investigations, they suggest that training non-physicians in ultrasound of the lungs and pleural space is feasible.
Based on the findings of the reviewed studies, nurses are able to record B-lines and pleural effusions with a minimum of ~4 h of training and students with a minimum of ~2 h of training.17,28 The sensitivity of nurse-performed LUS was highest for instruction that involved longer hands-on training time as compared with didactic time. For student studies involving healthy volunteers, overall image adequacy was also highest in the study with longer hands-on than didactic training time.23 In clinical practice, lung and pleural ultrasound training for non-physicians could employ brief training sessions with an emphasis on hands-on instruction.
Nurses already play an important role in the care of heart failure patients in a variety of settings and incorporating point-of-care ultrasound in the management of these patients could improve and expedite care and potentially reduce costs. For example, studies in heart failure clinics suggest that nurse-performed ultrasound examinations may provide prognostic information in patients with chronic heart failure and have the potential to improve patients’ quality of life.45–47 Other venues include resource-limited settings, especially in regions with long transport times where heart failure therapy could be initiated by pre-hospital providers.48 Despite the findings of one study discussed in this systematic review, paramedic-performed lung and pleural ultrasound could be feasible, with adequate training, as prior studies have shown that paramedics are able to perform other, more complex, point-of-care ultrasound examinations.29,42–46
Limitations and future considerations
This systematic review is limited by the small number and sample sizes of relevant studies. Due to supplementary learning material or unreported training times, we could not always quantify the training that was required for participants to learn LUS. Ultrasound methodology and reference standards varied across the studies. In two studies, a subset of participants may have been performing a greater number of the total reported examinations than others.15,24 Selection bias may have impacted findings in one study in which students selected examinations to log for review. In the same study, the assessment of diagnostic accuracy included only images deemed acceptable by the expert sonographer.19 The findings of only one study in our review did not support the hypothesis that paramedics can successfully learn and interpret LUS, which may be attributable to publication bias. Nevertheless, we believe that this systematic review provides hypothesis-generating data that may inform future research.
Based on our findings there are several knowledge gaps that could be addressed by future investigations. It is unclear which training methods and duration would be most effective and sufficient to train nurses and paramedics in LUS for the assessment of patients with heart failure. Additionally, the determination of clinical settings in which these interventions would provide the greatest benefit to patients and clinical workflow warrants further research. Finally, cost-effectiveness should be evaluated in the context of longer term outcomes across various clinical settings.
Conclusion
Our findings suggest that nurses and students in the medical field can learn to perform and interpret B-lines and pleural effusions using LUS with limited training. The examination of heart failure patients with LUS by non-clinicians appears feasible and warrants further investigation.
Supplementary Material
Implications for practice.
Lung ultrasound can be performed and interpreted by non-physicians, including nurses.
Lung ultrasound may be learned despite minimal clinical experience.
Non-physicians can learn lung ultrasound with short training periods.
Acknowledgements
VS, PB and EP had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. TBS contributed substantially to the data interpretation, and the writing of the manuscript. The authors thank David Osterbur, PhD from the Countway Library of Medicine, Harvard Medical School, in Boston for his assistance with the literature search.
Funding
This work was supported by the National Heart, Lung and Blood Institute (grant number K23HL123533) (EP) and Gangsted, Lundbeck, Reinholdt W. Jorck and Wife, Julie von Müllen and Augustinus (PB). The sponsors had no input in the development of the research and manuscript.
Footnotes
Declaration of conflicting interests
The authors declare that there is no conflict of interest.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics - 2017 update: A report from the American Heart Association. Circulation 2017; 135: e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Metra M and Teerlink JR. Heart failure. Lancet 2017; 390: 1981–1995. [DOI] [PubMed] [Google Scholar]
- 3.Al Deeb M, Barbic S, Featherstone R, et al. Point-of-care ultrasonography for the diagnosis of acute cardiogenic pulmonary edema in patients presenting with acute dyspnea: A systematic review and meta-analysis. Acad Emerg Med 2014; 21: 843–852. [DOI] [PubMed] [Google Scholar]
- 4.Martindale JL, Wakai A, Collins SP, et al. Diagnosing acute heart failure in the Emergency Department: A systematic review and meta-analysis. Acad Emerg Med 2016; 23: 223–242. [DOI] [PubMed] [Google Scholar]
- 5.Pivetta E, Goffi A, Lupia E, et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED: A SIMEU multicenter study. Chest 2015; 148: 202–210. [DOI] [PubMed] [Google Scholar]
- 6.Ponikowski P, Voors A, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Eur Heart J 2016; 37: 2129–2200. [DOI] [PubMed] [Google Scholar]
- 7.Chiem AT, Chan CH, Ander DS, et al. Comparison of expert and novice sonographers’ performance in focused lung ultrasonography in dyspnea (FLUID) to diagnose patients with acute heart failure syndrome. Acad Emerg Med 2015; 22: 564–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gargani L, Sicari R, Raciti M, et al. Efficacy of a remote web-based lung ultrasound training for nephrologists and cardiologists: A LUST trial sub-project. Nephrol Dial Transplant 2016; 31: 1982–1988. [DOI] [PubMed] [Google Scholar]
- 9.Coen J and Curry K. Improving heart failure outcomes: The role of the clinical nurse specialist. Crit Care Nurse Q 2016; 39: 335–344. [DOI] [PubMed] [Google Scholar]
- 10.Osleng MW, Olsen BF, Hetland A, et al. Quality of life improves in patients with chronic heart failure and Cheyne–Stokes respiration treated with adaptive servo-ventilation in a nurse-led heart failure clinic. J Clin Nurs 2017; 9: 1226–1233. [DOI] [PubMed] [Google Scholar]
- 11.Albert NM, Barnason S, Deswal A, et al. Transitions of care in heart failure: A scientific statement from the American Heart Association. Circ Hear Fail 2015; 8: 384–409. [DOI] [PubMed] [Google Scholar]
- 12.Rice H, Say R and Betihavas V. The effect of nurse-led education on hospitalisation, readmission, quality of life and cost in adults with heart failure: a systematic review. Patient Educ Couns 2018; 101: 363–374. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Alessandro L, Tetzlaff J, et al. ; The Prisma Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Heart, Lung, and Blood Institute. Quality assessment tool for before–after (pre–post) studies with no control group, https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/before-after (2014, accessed 15 October 2018).
- 15.Dalen H, Gundersen GH, Skjetne K, et al. Feasibility and reliability of pocket-size ultrasound examinations of the pleural cavities and vena cava inferior performed by nurses in an outpatient heart failure clinic. Eur J Cardiovasc Nurs 2015; 14: 286–293. [DOI] [PubMed] [Google Scholar]
- 16.Graven T, Wahba A, Hammer AM, et al. Focused ultrasound of the pleural cavities and the pericardium by nurses after cardiac surgery. Scand Cardiovasc J 2015; 49: 56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gustafsson M, Alehagen U and Johansson P. Pocket-sized ultrasound examination of fluid imbalance in patients with heart failure: A pilot and feasibility study of heart failure nurses without prior experience of ultrasonography. Eur J Cardiovasc Nurs 2015; 14: 294–302. [DOI] [PubMed] [Google Scholar]
- 18.Mumoli N, Vitale J, Giorgi-Pierfranceschi M, et al. Accuracy of nurse-performed lung ultrasound in patients with acute dyspnea: A prospective observational study. Medicine (Baltimore) 2016; 95: e2925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Unluer EE, Karagoz A, Oyar O, et al. Lung ultrasound by emergency nursing as an aid for rapid triage of dyspneic patients: A pilot study. Int Emerg Nurs 2014; 22: 226–231. [DOI] [PubMed] [Google Scholar]
- 20.Lichtenstein DA. Lung and interstitial syndrome. In: Whole body ultrasonography in the critically ill. Berlin; Heidelberg: Springer, 2010: pp.151–162. [Google Scholar]
- 21.Andersen GN, Viset A, Mjolstad OC, et al. Feasibility and accuracy of point-of-care pocket-size ultrasonography performed by medical students. BMC Med Educ 2014; 14: 156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heiberg J, Hansen LS, Wemmelund K, et al. Point-of-care clinical ultrasound for medical students. Ultrasound Int Open 2015; 1: E58–E66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lim JS, Lee S, Do HH, et al. Can limited education of lung ultrasound be conducted to medical students properly? A pilot study. Biomed Res Int 2017; 2017: 8147075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mai TV, Ahn DT, Phillips CT, et al. Feasibility of remote real-time guidance of a cardiac examination performed by novices using a pocket-sized ultrasound device. Emerg Med Int 2013; 2013: 627230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Steinmetz P, Oleskevich S and Lewis J. Acquisition and long-term retention of bedside ultrasound skills in first-year medical students. J Ultrasound Med 2016; 35: 1967–1975. [DOI] [PubMed] [Google Scholar]
- 26.Udrea DS, Sumnicht A, Lo D, et al. Effects of student-performed point-of-care ultrasound on physician diagnosis and management of patients in the Emergency Department. J Emerg Med 2017; 53: 102–109. [DOI] [PubMed] [Google Scholar]
- 27.Connolly K, Beier L, Langdorf MI, et al. Ultrafest: A novel approach to ultrasound in medical education leads to improvement in written and clinical examinations. West J Emerg Med 2015; 16: 143–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eissa K, Alokla K, Assasa O, et al. Using simulation-based training to incorporate thoracic ultrasound into physical examination. J La State Med Soc 2015; 167: 264–267. [PubMed] [Google Scholar]
- 29.Becker TK, Martin-Gill C, Callaway CW, et al. Feasibility of paramedic performed prehospital lung ultrasound in medical patients with respiratory distress. Prehosp Emerg Care 2018; 22: 175–179. [DOI] [PubMed] [Google Scholar]
- 30.Lichtenstein DA and Meziere GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: The BLUE protocol. Chest 2008; 134: 117–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Steinwandel U, Gibson N, Towell A, et al. Can a renal nurse assess fluid status using ultrasound on the inferior vena cava? A cross-sectional interrater study. Hemodial Int 2018; 22: 261–269. [DOI] [PubMed] [Google Scholar]
- 32.De Lorenzo RA and Holbrook-Emmons VL. Ultrasound measurement of inferior vena cava diameters by emergency department nurses. Adv Emerg Nurs J 2014; 36: 271–278. [DOI] [PubMed] [Google Scholar]
- 33.Modi P, Glavis-Bloom J, Nasrin S, et al. Accuracy of inferior vena cava ultrasound for predicting dehydration in children with acute diarrhea in resource-limited settings. PLoS One 2016; 11: e0146859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cheng HY, Chair SY, Wang Q, et al. Effects of a nurse-led heart failure clinic on hospital readmission and mortality in Hong Kong. J Geriatr Cardiol 2016; 13: 415–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stromberg A, Martensson J, Fridlund B, et al. Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failure: Results from a prospective, randomised trial. Eur Heart J 2003; 24: 1014–1023. [DOI] [PubMed] [Google Scholar]
- 36.Lulebo AM, Kaba DK, Atake SE, et al. Task shifting in the management of hypertension in Kinshasa, Democratic Republic of Congo: A cross-sectional study. BMC Health Serv Res 2017; 17(Suppl. 2): 698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Joshi R, Alim M, Kengne AP, et al. Task shifting for noncommunicable disease management in low and middle income countries – a systematic review. PLoS One 2014; 9: e103754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Callaghan M, Ford N and Schneider H. A systematic review of task-shifting for HIV treatment and care in Africa. Hum Resour Health 2010; 8: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meisel ZF, Pines JM, Polsky D, et al. Variations in ambulance use in the United States: The role of health insurance. Acad Emerg Med 2011; 18: 1036–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brooke M, Walton J, Scutt D, et al. Acquisition and interpretation of focused diagnostic ultrasound images by ultrasound-naive advanced paramedics: Trialling a PHUS education programme. Emerg Med J 2012; 29: 322–326. [DOI] [PubMed] [Google Scholar]
- 41.Walcher F, Kirschning T, Muller MP, et al. Accuracy of prehospital focused abdominal sonography for trauma after a 1-day hands-on training course. Emerg Med J 2010; 27: 345–349. [DOI] [PubMed] [Google Scholar]
- 42.Heegaard W, Hildebrandt D, Spear D, et al. Prehospital ultrasound by paramedics: Results of field trial. Acad Emerg Med 2010; 17: 624–630. [DOI] [PubMed] [Google Scholar]
- 43.Chin EJ, Chan CH, Mortazavi R, et al. A pilot study examining the viability of a Prehospital Assessment with UltraSound for Emergencies (PAUSE) protocol. J Emerg Med 2013; 44: 142–149. [DOI] [PubMed] [Google Scholar]
- 44.Rooney KP, Lahham S, Lahham S, et al. Pre-hospital assessment with ultrasound in emergencies: implementation in the field. World J Emerg Med 2016; 7: 117–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gundersen GH, Norekval TM, Haug HH, et al. Adding point of care ultrasound to assess volume status in heart failure patients in a nurse-led outpatient clinic. A randomised study. Heart 2016; 102: 29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gundersen GH, Norekvål TM, Graven T, et al. Patient-reported outcomes and associations with pleural effusion in outpatients with heart failure: An observational cohort study. BMJ Open 2017; 7: e013734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gustafsson M, Alehagen U and Johansson P. Imaging congestion with a pocket ultrasound device: Prognostic implications in patients with chronic heart failure. J Card Fail 2015; 21: 548–554. [DOI] [PubMed] [Google Scholar]
- 48.Shah SP, Shah SP, Fils-Aime R, et al. Focused cardiopulmonary ultrasound for assessment of dyspnea in a resource-limited setting. Crit Ultrasound J 2016; 8: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.