Abstract
The number of annual THA's, TKA's, and TSA's is set to increase significantly by the year 2030, making it imperative to understand the risks for negative outcomes in these procedures. While research has studied the patient risk factors for perioperative and postoperative complications, there has been relatively little research for intraoperative complications. After a thorough literature review, the most supported finding was that patients with a BMI >30 had significantly more intraoperative blood loss than those with a BMI <30. All other relationships between patient risk factors and intraoperative complications of interest were inadequately studied.
Keywords: Intraoperative, Complications, Total arthroplasty, Risk factors
Highlights
-
•
There has been little research comparing patient risk factors to intraoperative complications in primary THA, TKA, and TSA.
-
•
Most relationships between risk factors and intraoperative complications were inadequately studied, except for blood loss.
-
•
Patients with a BMI >30 had more intraoperative blood loss than those with a BMI <30.
-
•
Researchers should discriminate complications into discrete time categories including the intraoperative period.
1. Introduction
The number of total hip arthroplasties (THA), total knee arthroplasties (TKA), and total shoulder arthroplasties (TSA) is expected to rise significantly by the year 2030.1,2 Due to the increased demand for these procedures, it is of great importance to understand the link between intraoperative complications and patient risk factors. Doing so will help avoid increased costs and negative health outcomes. Birkmeyer et al.3 found that THA's at hospitals that ranked in the top 20% for general surgical complications cost patients on average $2436 more. Nichols et al.4 found that patients who had complications in the perioperative period of a TKA or THA were both more likely to be discharged with home health services, and that discharge with home health services increased incidence of readmission.
While there has been much research comparing patient risk factors, such as age, sex, and body mass index (BMI), to complications within the perioperative and 30-day postoperative periods,5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 there has been relatively little research done comparing patient risk factors to intraoperative complications such as mortality, absolute hypotension and hypertension, and pulmonary embolism. By addressing this gap in the current literature, the health outcomes of patients, and the financial outcomes of patients and providers, can be improved. In this article, the current literature will be reviewed for patient characteristics and comorbidities that both alter the incidence of intraoperative complications and have not yet been studied thoroughly, thereby maximizing the effectiveness and precision of future studies.
2. Methods
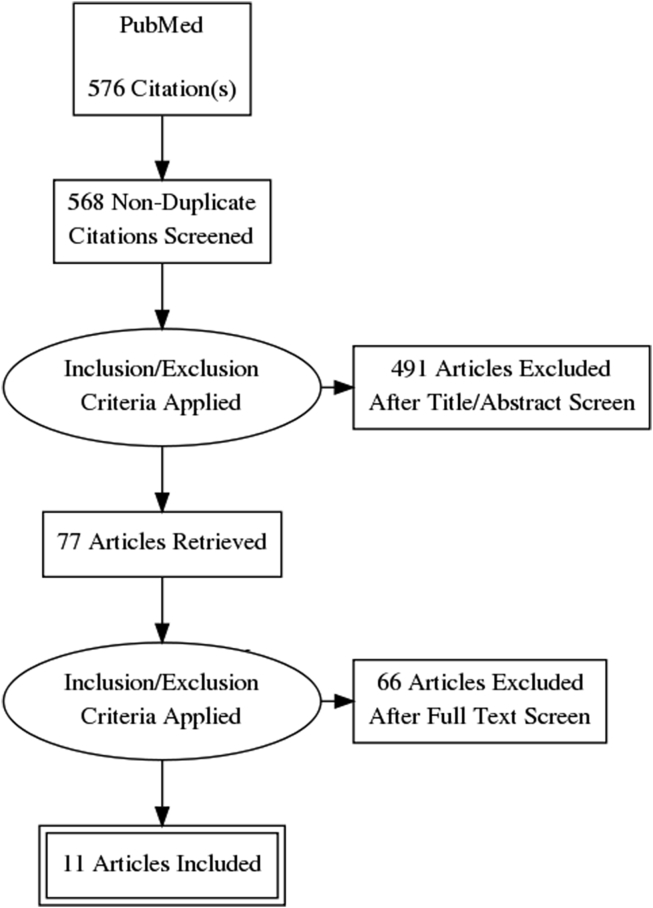
Relevant articles were found through the PubMed database using the PRISMA guidelines. Table 1 provides a list of the search terminology used for this review. The date range of the articles retrieved was from 1976 to 2018. Articles studying populations outside of the United States were included. 576 articles were retrieved from PubMed. After removing 8 duplicates, 568 articles were left to be screened via title and abstract review.
Table 1.
Record of all search terms used on PubMed.
| Search Terms Used for Literature Review |
|---|
| “Risk Factors Intraoperative Complications Arthroplasty” |
| “Preoperative Risk Factors Intraoperative Complications Arthroplasty” |
| “Patient Characteristics Intraoperative Complications Arthroplasty” |
| “Risk Factors Intraoperative Events Arthroplasty” |
| “Patient Characteristics Intraoperative Mortality Arthroplasty” |
| “Risk Factors Intraoperative Mortality Arthroplasty” |
| “Sudden Death Intraoperative Mortality” |
| “Perioperative Risk Factors Intraoperative Complications Arthroplasty” |
| “Perioperative Risk Factors Intraoperative Hypothermia Arthroplasty” |
| “Risk Factors Intraoperative Hypoxia Arthroplasty” |
| “Intraoperative Thromboembolism Risk Factors Arthroplasty” |
Following abstract review, 491 articles were excluded using our exclusion criteria. Exclusion criteria included irrelevant comparisons defined as articles that did not specifically compare patient characteristics to intraoperative complications, such as articles that measured comparisons to perioperative or postoperative complications. Irrelevant comparisons also included measurements of the efficacy of different procedure techniques, as well as articles that studied patient risk factors for intraoperative fractures, as this topic is thoroughly represented in the literature.16, 17, 18, 19, 20 Notably, an irrelevant comparison consistently found was the utility of Transexamic acid in decreasing perioperative blood loss. This is an antifibrinolytic drug that prevents plasmin formation. In addition, tourniquet times were similarly omitted as irrelevant comparisons. Although both Transexamic acid and tourniquets play an important role in limiting perioperative blood loss, the goal of this review was to compare patient characteristics to intraoperative complications, not procedure techniques and the use of certain drugs to intraoperative complications.
Exclusion criteria further included irrelevant populations defined as surgical patients who did not specifically undergo elective, primary, or revision TSA, TKA, or THA. These three procedures were included together as the article retrieval count was low for each one, however excluded groups included hemiarthroplasty patients in order to limit surgical variables. There were no exclusions based on the location of studies, surgeon laterality, surgical approach, type of material for implant fixation, or prosthesis types. The composition of the 491 articles excluded was 467 irrelevant comparisons and 24 irrelevant populations.
The full content of the remaining 77 articles was then thoroughly reviewed. 66 of these articles were excluded, the composition of which was 62 irrelevant comparisons as defined above, 3 that were not in the English language, and 1 article that had an insignificant patient population of 7. The total articles included in the results section of this review was therefore 11. Please see Fig. 1 for a graphical diagram of this process.
Fig. 1.
PRISMA Flow Chart. Depicts a step-by-step analysis of the literature review.
These final 11 articles included some, but not all, of the patient characteristics and intraoperative complications of interest in our study. Patient characteristics of interest were: age, sex, BMI, blood type, rheumatoid arthritis (RA), osteoarthritis (OA), coronary artery disease, congestive heart failure (CHF), chronic obstructive pulmonary disease, asthma, presence of a patent foramen ovale (PFO), diabetes mellitus type I and II, and ASA score. Intraoperative complications of interest were: blood loss, mortality, intraoperative absolute hypotension and hypertension, bone cement implantation syndrome, pulmonary embolism, changes in heart rate, hypoxia, and hypothermia.
Independent statistical analysis was not possible for this review as the data required was unavailable. Statistical significance was represented by p-values less than 0.05. Both significant and insignificant p-values are reported in the results section. Some authors chose not to include p-values with their results.
3. Results
3.1. Blood loss
Throughout the literature review, intraoperative blood loss was found to be the most represented intraoperative complication.21, 22, 23, 24, 25, 26 Studies often attempted to assess the risk for blood transfusion by measuring blood loss among patients with varying comorbidities. However, many of these articles did not discriminate blood loss into discrete categories of “intraoperative” and “postoperative” blood loss. When blood loss was discriminated into discrete categories, there was often no statistical analysis conducted that compared the patient characteristics listed in the methods section with intraoperative blood loss.
Multiple studies found that a higher BMI was correlated with higher intraoperative blood loss (Table 2). In a prospective study of 80 THA's, Bowditch et al.21 found that patients with a BMI over 30 lost on average 213 mL more blood intraoperatively than patients with a BMI under 30 (p = 0.003). In 2013, Naziri et al.22 conducted a retrospective study of 190 TKA's, the results of which agreed with Bowditch's findings. Naziri et al. compared “super obese” patients, defined as those with a BMI >50, to patients with a BMI <30. They found that the “super obese” patients lost on average 121 mL more blood intraoperatively (p = 0.001). Gupta et al.23 supported this finding with their retrospective analysis of 119 TSA's. They found that patients with a BMI >35 lost on average 62 mL more blood intraoperatively than patients with a BMI <35 (p = 0.050).
Table 2.
Pertinent findings of each study regarding intraoperative blood loss and related patient risk factors. The risk factor column lists the case group followed by the control group for each study. (+) represents a positive, or larger, amount of blood lost from the perspective of the case group to the control group. Statistically significant p-values are denoted by an asterisk*. The significance level was p < 0.05.
| Studies Comparing Patient Characteristics and Intraoperative Blood Loss | |||||
|---|---|---|---|---|---|
| Author(s) | Number of Arthroplasties (n) | Type of Arthroplasty | Risk Factor (Case vs Control) | Mean Blood Loss (Case vs Control) | P Value |
| Bowditch et al. (21) | 80 | THA | BMI > 30 vs BMI < 30 |
+213 mL | P = 0.003* |
| Naziri et al. (22) | 190 | TKA | BMI > 50 vs BMI < 30 |
+121 mL | P = 0.001* |
| Gupta et al. (23) | 119 | TSA | BMI > 35 vs BMI < 35 |
+62 mL | P = 0.050* |
| Alberth et al. (24) | 540 | THA | Blood Type O vs. Blood Types A, B, and AB | No significant difference, per author. | Unavailable |
| Prasad et al. (25) | 66 | TKA | Sex: Male vs. Female |
+61.2 mL | P = 0.139 |
| Prasad et al. (25) | 66 | TKA | RA vs OA | +19 mL | P = 0.78 |
BMI was not the only patient characteristic compared to intraoperative blood loss. Alberth et al.,24 through a retrospective study of 540 THA's, found that patients with blood types A, B, and AB did not have increased intraoperative blood loss when compared to patients with blood type O. No p-value was provided by the author. Sex was considered by Prasad et al.25 in a prospective study of 66 TKA's. It was found that the sex of the patient played no role in intraoperative blood loss, with male patients losing an average of 265 mL and female patients losing an average of 203.8 mL intraoperatively (p = 0.139). Prasad et al. also found that there was no significant difference in intraoperative blood loss between patients with RA compared to patients with OA. RA patients had a mean intraoperative blood loss of 235 mL while OA patients had a mean loss of 216 mL (p = 0.78).
Of note, a review article considering the risk of blood loss and transfusion in TKA and THA was conducted by Sizer et al.26 While their abstract suggests a key point that age, ASA grade over III, and a Charlson Index greater than three are indicative of greater intraoperative blood loss, the articles they cite to support this27, 28, 29, 30 do not differentiate intraoperative blood loss from total blood loss.
3.2. Mortality and microemboli
Although the safety of TSA's, THA's, and TKA's is well documented, there continues to be a risk for intraoperative death. Bone cement implantation syndrome (BCS) is a cause of this terrible outcome. Although BCS is not well understood, according to Donaldson et al.31 the common definition includes a variety of the following: hypoxia, hypotension, cardiac arrhythmias, increased pulmonary vascular resistance, and cardiac arrest. According to a retrospective analysis of 38,488 THA's by Parvizi et al.,32 female elderly patients with an underlying cardiovascular disease, fracture diagnosis (p < 0.05), and undergoing a cemented arthroplasty were most at risk for BCS (Table 3). “Elderly” was not defined in the review, however the mean age of females in the study population was 80.9 years. No additional p-values were included in the study for these findings.
Table 3.
Significance of certain patient characteristics for certain intraoperative complications in total arthroplasty. (+)'s represent the determination by a study author that the risk factor considered significantly increases the risk of the intraoperative complication considered. (-)'s represent the determination by a study author that the risk factor considered does not increase risk for the intraoperative complication considered. P-values are provided when available and significance is denoted by an asterisk*. The significance level was p < 0.05.
| Studies Comparing Intraoperative Complications with Patient Characteristics | ||||||
|---|---|---|---|---|---|---|
| Author | Number of Arthroplasties (n) | Type of Arthroplasty | Outcome Considered | Risk Factor | Significa-nce | P Value |
| Parvizi et al. (32) | 38,488 | THA | Death | Age | (+) | Unavail-able |
| Parvizi et al. (32) | 38,488 | THA | Death | Fracture Diagnosis | (+) | P < 0.05* |
| Parvizi et al. (32) | 38,488 | THA | Death | Sex | (+) | Unavail-able |
| Patel et al. (37) | 45 | THA | Microemboli Incidence | Age | (-) | P = 0.60 |
| Patel et al. (37) | 45 | THA | Microemboli Incidence |
PFO | (-) | P = 0.23 |
| Perka et al. (38) | 237 | TKA | Change in Intraoperative Blood Pressure | BMI | (-) | Unavail-able |
| Saltzman et al. (39) | 136 | TSA | All Intraoperative Complications | Age | (-) | P = 0.071 |
| Saltzman et al. (39) | 136 | TSA | All Intraoperative Complications | Sex | (-) | P = 0.950 |
| Saltzman et al. (39) | 136 | TSA | All Intraoperative Complications | Charlson's Comorbidity Index | (-) | P = 0.670 |
Most studies considering mortality focus on postoperative deaths.5,33, 34, 35 This is expected, as Parvizi et al.32 found only 23 intraoperative deaths in his review sample. Moreover, another retrospective study by Dobbs et al.36 found there were only three intraoperative deaths out of the 85 patients who died in their study population of 37,304 patients. It is worth mentioning that this study included both internal fixation and THA, with 31,086 patients undergoing the arthroplasty. The three intraoperative deaths are not discriminated into internal fixation or THA groups, leading to the possibility that the number of deaths related to THA may be lower.
When considering microemboli separately from intraoperative deaths, one article sheds light on the subject. Patel et al.37 prospectively studied 45 THA's. They found that neither age (p = 0.60) nor the presence of a PFO (p = 0.23) increased the likelihood of intraoperative microemboli (Table 3).
3.3. Intraoperative changes in blood pressure: absolute hypotension and hypertension
While many articles have studied the events of intraoperative absolute hypotension and hypertension, only one has taken the time to compare intraoperative blood pressure with a patient characteristic of interest to this review (Table 3). This was a prospective study conducted by Perka et al.38 that assessed 237 cementless TKA's. They found there was no statistically significant relationship between BMI and intraoperative blood pressure. No p-value was provided by the authors.
3.4. General intraoperative complications
Several studies measured the incidence of all complications compared to patient characteristics of interest. However, only one of these studies measured the incidence of intraoperative complications in this regard (Table 3). In their comparative retrospective cohort study, Saltzman et al.39 found that neither age (p = 0.071), sex (p = 0.950), BMI (p = 0.670), or the Charlson's comorbidity Index (p = 0.601) were predictive of any of the intraoperative complications recorded in their sample of 136 TSA's. Intraoperative complications in this study were defined as any event that deviated from the normal intraoperative course.
4. Discussion
Intraoperative complications continue to result in increased costs and suboptimal patient outcomes,3,4 including death.32 This review found that blood loss was the only intraoperative complication adequately compared to a patient characteristic. While there were studies that compared other patient characteristics to other intraoperative complications, these studies were few, and most times did not solely focus on intraoperative complications. The studies reported in the results section offer few conclusive findings besides the need for more research. Fortunately, this review highlights subjects of interest for future studies concerning intraoperative complications and their risk factors.
The most well-supported conclusion of this review was that patients with a BMI >30 had a statistically significant increase in intraoperative blood loss.21, 22, 23, 24 Understanding the preventative measures that can be taken to limit blood loss in these patients can result in better health outcomes, especially given the secondary complications that include the adverse effects of some blood transfusions.40 Examples of preventative measures include optimizing the use of tourniquets during surgery or developing a formula that predicts the need for perioperative Transexamic acid administration, both on the basis of BMI. Likewise, these techniques to limit blood loss can be tailored to other patient characteristics once their relationship with intraoperative blood loss is more thoroughly understood.
This review found only one study that compared absolute intraoperative hypotension to a patient characteristic, which in the case of Perka et al.'s38 study was BMI. Although they found no link, it is important to explore the relationships of other patient characteristics, such as CHF, with absolute hypotension during total arthroplasty. Especially given that absolute hypotension may occur in bone cement implantation syndrome. According to Dobbs et al. patients with serious intraoperative hypotension had a higher chance of death in the hospital as well as a protracted postoperative course.36
When comparing TSA, TKA, and THA this review found that they were all represented in considering BMI versus blood loss, however the other intraoperative complications were studied by only one patient population each. Intraoperative mortality, absolute hypotension, and general complications were each only represented by THA, TKA, and TSA patients respectively, highlighting the limitations of this review article. Additionally, another limitation of this review arises from the low number of articles retrieved, forcing this review to consider all three major total arthroplasties. This introduced unnecessary variables, making conclusions less reliable. Moreover, while it would have been beneficial to the orthopaedics community for this review to evaluate the effects of Transexamic acid, tourniquet times, surgeon laterality, and a variety of other excluded items, these were not considered to be patient characteristics, and would have diluted the conclusions written here due to the addition of unnecessary complexity.
The following are a few suggestions to improve relevant future studies regarding the topic of this review. First, researchers should differentiate complications temporally. For example, instead of only reporting perioperative complications, researchers should differentiate their complications into discrete categories of intraoperative, early postoperative, 30 days postoperative, and so on. Second, researchers should not only collect data on age, sex, BMI, and other relevant patient characteristics, but make the effort to compare these to complications in both the intraoperative and postoperative periods. Third, full reporting of data should be included in future studies to allow other researchers the ability to conduct their own statistical analyses on important relationships. We believe applying these suggestions, as well as targeting areas of interest outlined in this review, will lead to better patient health outcomes and reduced costs.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Contributor Information
Adel Hijazi, Email: adel.eddie.hijazi@gmail.com.
Muhammad Talha Padela, Email: tpadela@gmail.com.
Zain Sayeed, Email: zainsayeed@gmail.com.
Aws Hammad, Email: awshammad@gmail.com.
Kamela Devole, Email: kdevole4@yahoo.com.
Todd Frush, Email: frushtod@hotmail.com.
Gamal Mostafa, Email: gamal.mostafa@va.gov.
Walid K. Yassir, Email: wyassir@gmail.com.
Khaled J. Saleh, Email: kjsaleh@gmail.com.
References
- 1.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Padegimas M.E., Maltenfort M., Lazarus D.M., Ramsey L.M., Williams R.G., Namdari S. Future patient demand for shoulder arthroplasty by younger patients: national projections. Clin Orthop. 2015 Jun;473(6):1860–1867. doi: 10.1007/s11999-015-4231-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birkmeyer D.J., Gust C., Dimick B.J., Birkmeyer O.N.J., Skinner S.J. Hospital quality and the cost of inpatient surgery in the United States. Ann Surg. 2012 Jan;255(1):1–5. doi: 10.1097/SLA.0b013e3182402c17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nichols I.C., Vose G.J. Clinical outcomes and costs within 90 Days of primary or revision total joint arthroplasty. J Arthroplast. 2016 Jul;31(7):1400–1406.e3. doi: 10.1016/j.arth.2016.01.022. [DOI] [PubMed] [Google Scholar]
- 5.Parvizi J., Ereth H.M., Lewallen G.D. Thirty-day mortality following hip arthroplasty for acute fracture. J Bone Joint Surg Am. 2004 Sep;86-A(9):1983–1988. doi: 10.2106/00004623-200409000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Ondeck T.N., Bohl D.D., Bovonratwet P. Predicting adverse outcomes after total hip arthroplasty: a comparison of demographics, the American society of anesthesiologists class, the modified Charlson comorbidity index, and the modified frailty index. J Am Acad Orthop Surg. 2018 Oct;26(20):735–743. doi: 10.5435/JAAOS-D-17-00009. [DOI] [PubMed] [Google Scholar]
- 7.Naqvi Y.S., Rabiei H.A., Maltenfort G.M. Perioperative complications in patients with sleep apnea undergoing total joint arthroplasty. J Arthroplast. 2017 Sep;32(9):2680–2683. doi: 10.1016/j.arth.2017.04.040. [DOI] [PubMed] [Google Scholar]
- 8.Mahure S., Mollon B., Quien M., Karia R., Zuckerman J., Kwon Y. Impact of diabetes on perioperative complications in patients undergoing elective total shoulder arthroplasty. Bull Hosp Jt Dis. 2017 May;75(3):173–179. 2013. [PubMed] [Google Scholar]
- 9.Buller T.L., Rosas S., Sabeh G.K., Roche W.M., McLawhorn S.A., Barsoum K.W. Hypothyroidism increases 90-day complications and costs following primary total knee arthroplasty. J Arthroplast. 2018 Apr;33(4):1003–1007. doi: 10.1016/j.arth.2017.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newman M.J., Sultan A.A., Khlopas A. What are the short-term outcomes in multiple sclerosis patients after total knee arthroplasty? J Knee Surg. 2019 Feb;32(2):165–170. doi: 10.1055/s-0038-1636836. [DOI] [PubMed] [Google Scholar]
- 11.Ward M.M. 2018 Apr. Complications of Total Hip Arthroplasty in Patients with Ankylosing Spondylitis. Arthritis Care Res [Internet]http://www.ncbi.nlm.nih.gov/pubmed/29669197 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newman M.J., Stroud G.S., Yang A. Total shoulder arthroplasty in octogenarians: is there a higher risk of adverse outcomes? J Orthop. 2018 Jun;15(2):671–675. doi: 10.1016/j.jor.2018.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gurunathan U., Anderson C., Berry E.K., Whitehouse L.S., Crawford W.R. Body mass index and in-hospital postoperative complications following primary total hip arthroplasty. Hip Int J Clin Exp Res Hip Pathol Ther. 2018 Nov;28(6):613–621. doi: 10.1177/1120700017754058. [DOI] [PubMed] [Google Scholar]
- 14.Scholten R., Leijtens B., Kremers K., Snoeck M., Koëter S. The incidence of mild hypothermia after total knee or hip arthroplasty: a study of 2600 patients. J Orthop. 2018 Jun;15(2):408–411. doi: 10.1016/j.jor.2018.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ondeck T.N., Bohl D.D., Bovonratwet P., McLynn P.R., Cui J.J., Grauer N.J. Discriminative ability of elixhauser's comorbidity measure is superior to other comorbidity scores for inpatient Adverse outcomes after total hip arthroplasty. J Arthroplast. 2018 Jan;33(1):250–257. doi: 10.1016/j.arth.2017.08.032. [DOI] [PubMed] [Google Scholar]
- 16.Lindberg-Larsen M., Jørgensen C.C., Solgaard S. Increased risk of intraoperative and early postoperative periprosthetic femoral fracture with uncemented stems. Acta Orthop. 2017 Aug;88(4):390–394. doi: 10.1080/17453674.2017.1302908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhao R., Cai H., Liu Y., Tian H., Zhang K., Liu Z. Risk factors for intraoperative proximal femoral fracture during primary cementless THA. Orthopedics. 2017 Mar;40(2):e281–e287. doi: 10.3928/01477447-20161116-06. [DOI] [PubMed] [Google Scholar]
- 18.Miettinen A.S.S., Mäkinen J.T., Kostensalo I. Risk factors for intraoperative calcar fracture in cementless total hip arthroplasty. Acta Orthop. 2016 Nov;87(2):113–119. doi: 10.3109/17453674.2015.1112712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ponzio Y.D., Shahi A., Park G.A., Purtill J.J. Intraoperative proximal femoral fracture in primary cementless total hip arthroplasty. J Arthroplast. 2015 Aug;30(8):1418–1422. doi: 10.1016/j.arth.2015.02.043. [DOI] [PubMed] [Google Scholar]
- 20.Nowak M., Kusz D., Wojciechowski P., Wilk R. Risk factors for intraoperative periprosthetic femoral fractures during the total hip arthroplasty. Pol Orthop Traumatol. 2012 Sep;77:59–64. [PubMed] [Google Scholar]
- 21.Bowditch G.M., Villar N.R. Do obese patients bleed more? A prospective study of blood loss at total hip replacement. Ann R Coll Surg Engl. 1999 May;81(3):198–200. [PMC free article] [PubMed] [Google Scholar]
- 22.Naziri Q., Issa K., Malkani L.A., Bonutti M.P., Harwin F.S., Mont A.M. Bariatric orthopaedics: total knee arthroplasty in super-obese patients (BMI > 50 kg/m2). Survivorship and complications. Clin Orthop. 2013 Nov;471(11):3523–3530. doi: 10.1007/s11999-013-3154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta K.A., Chalmers N.P., Rahman Z. Reverse total shoulder arthroplasty in patients of varying body mass index. J Shoulder Elb Surg. 2014 Jan;23(1):35–42. doi: 10.1016/j.jse.2013.07.043. [DOI] [PubMed] [Google Scholar]
- 24.Alberth G., Kettisen J., Lisander B. Blood loss in prosthetic hip replacement is not influenced by the AB0 blood group. Eur J Surg Acta Chir. 2001 Sep;167(9):652–655. doi: 10.1080/11024150152619264. [DOI] [PubMed] [Google Scholar]
- 25.Prasad N., Padmanabhan V., Mullaji A. Blood loss in total knee arthroplasty: an analysis of risk factors. Int Orthop. 2007 Feb;31(1):39–44. doi: 10.1007/s00264-006-0096-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sizer C.S., Cherian J.J., Elmallah K.R.D., Pierce P.T., Beaver B.W., Mont A.M. Predicting blood loss in total knee and hip arthroplasty. Orthop Clin N Am. 2015 Oct;46(4):445–459. doi: 10.1016/j.ocl.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 27.Guerin S., Collins C., Kapoor H., McClean I., Collins D. Blood transfusion requirement prediction in patients undergoing primary total hip and knee arthroplasty. Transfus Med Oxf Engl. 2007 Feb;17(1):37–43. doi: 10.1111/j.1365-3148.2006.00698.x. [DOI] [PubMed] [Google Scholar]
- 28.Mesa-Ramos F., Mesa-Ramos M., Maquieira-Canosa C., Carpintero P. Predictors for blood transfusion following total knee arthroplasty: a prospective randomised study. Acta Orthop Belg. 2008 Feb;74(1):83–89. [PubMed] [Google Scholar]
- 29.Pola E., Papaleo P., Santoliquido A., Gasparini G., Aulisa L., De Santis E. Clinical factors associated with an increased risk of perioperative blood transfusion in nonanemic patients undergoing total hip arthroplasty. J Bone Joint Surg Am. 2004 Jan;86-A(1):57–61. doi: 10.2106/00004623-200401000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Grosflam M.J., Wright A.E., Cleary D.P., Katz N.J. Predictors of blood loss during total hip replacement surgery. Arthritis Care Res Off J Arthritis Health Prof Assoc. 1995 Sep;8(3):167–173. doi: 10.1002/art.1790080309. [DOI] [PubMed] [Google Scholar]
- 31.Donaldson J.A., Thomson E.H., Harper J.N., Kenny W.N. Bone cement implantation syndrome. Br J Anaesth. 2009 Jan;102(1):12–22. doi: 10.1093/bja/aen328. [DOI] [PubMed] [Google Scholar]
- 32.Parvizi J., Holiday D.A., Ereth H.M., Lewallen G.D. The Frank Stinchfield Award. Sudden death during primary hip arthroplasty. Clin Orthop. 1999 Dec;(369):39–48. doi: 10.1097/00003086-199912000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Rhee C., Lethbridge L., Richardson G., Dunbar M. Risk factors for infection, revision, death, blood transfusion and longer hospital stay 3?months and 1?year after primary total hip or knee arthroplasty. Can J Surg J Can Chir. 2018 Jun;61(3):165–176. doi: 10.1503/cjs.007117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lin C.-F.J., Liang W.-M. Mortality, readmission, and reoperation after hip fracture in nonagenarians. BMC Muscoskelet Disord. 2017 Apr;18(1) doi: 10.1186/s12891-017-1493-5. http://www.ncbi.nlm.nih.gov/pubmed/28376876 [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Amundsen A., Rasmussen V.J., Olsen S.B., Brorson S. Mortality after shoulder arthroplasty: 30-day, 90-day, and 1-year mortality after shoulder replacement–5853 primary operations reported to the Danish Shoulder Arthroplasty Registry. J Shoulder Elb Surg. 2016 May;25(5):756–762. doi: 10.1016/j.jse.2015.09.020. [DOI] [PubMed] [Google Scholar]
- 36.Dobbs E.R., Parvizi J., Lewallen G.D. Perioperative morbidity and 30-day mortality after intertrochanteric hip fractures treated by internal fixation or arthroplasty. J Arthroplast. 2005 Dec;20(8):963–966. doi: 10.1016/j.arth.2005.04.035. [DOI] [PubMed] [Google Scholar]
- 37.Patel V.R., Stygall J., Harrington J., Newman P.S., Haddad S.F. Cerebral microembolization during primary total hip arthroplasty and neuropsychologic outcome: a pilot study. Clin Orthop. 2010 Jun;468(6):1621–1629. doi: 10.1007/s11999-009-1140-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Perka C., Arnold U., Buttgereit F. Influencing factors on perioperative morbidity in knee arthroplasty. Clin Orthop. 2000 Sep;(378):183–191. doi: 10.1097/00003086-200009000-00028. [DOI] [PubMed] [Google Scholar]
- 39.Saltzman M.B., Chalmers N.P., Gupta K.A., Romeo A.A., Nicholson P.G. Complication rates comparing primary with revision reverse total shoulder arthroplasty. J Shoulder Elb Surg. 2014 Nov;23(11):1647–1654. doi: 10.1016/j.jse.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 40.Gu A., Maybee C.M., Wei C., Probasco W.V., Ast M.P., Sculco P.K. Preoperative blood transfusion associated with increased length of stay and increased postoperative complications after revision total knee arthroplasty. J Orthop. 2019 Jun;16(3):265–268. doi: 10.1016/j.jor.2019.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]