Abstract
This study tried to investigate the effects of number of medications and age on antihypertensive medication adherence in a real-world setting using a nationwide representative cohort.
We obtained data from the National Health Insurance Service-National Sample Cohort (NHIS-NSC) of Korea, which is a sample of 2.2% (N = 1,048,061) of total population (N = 46,605,433). Patients aged 20 years or older (N = 150,550) who took antihypertensive medications for at least 1 year were selected. Medication possession ratio (MPR) was used for measuring adherence. The subjects were divided into 5 subgroups according to total number of medications: 1–2, 3–4, 5–6, 7–8, and 9 or more. The mean age and the mean number of medications were 60.3 ± 12.6 years and 4.1 ± 2.2, respectively. The mean MPR was 80.4 ± 23.9%, and 66.9% (N = 100,645) of total subjects were adherent (MPR ≥ 80%). The overall tendency of antihypertensive medication adherence according to the total number of medications displayed an inverted U-shape with a peak at 3–4 drugs. Adherence consistently increased as the age increased until age 69 and started to decrease from age 70. The proportion of adherent patients (MPR ≥ 80%) according to the total number of medications also showed an inverted U-shape with a peak at 3–4 drugs. When the same number of drugs was taken, the proportion of adherent patients according to age featured an inverted U- shape with a peak at 60 to 69 years. Patients taking 9 or more total drugs had the overall odds ratio (95% CI) of non-adherence (MPR < 80%) with 1.17 (1.11–1.24) compared with those taking 1 to 8 total drugs and the odds ratios in the age subgroups of 40 to 49, 50 to 59, 60 to 69 years were 1.57 (1.31–1.87), 1.21 (1.08–1.36), and 1.14 (1.04–1.25), respectively (P < .05).
Association between age, total number of medications, and antihypertensive adherence displayed an inverted U-shape with a peak at 3 to 4 total medications and at age 60 to 69 years. When the total number of drugs was 9 or more, adherence decreased prominently, regardless of age.
Keywords: age, hypertension, medication adherence, number of medications
1. Introduction
Medication adherence refers to the patient's active, voluntary, and collaborative participatory behavior to achieve a therapeutic effect.[1,2] Non-adherence can be considered a medical illness state because it leads to increased harmful health consequences such as complications and increased medical cost.[2–5] In chronic diseases such as hypertension, proper medication adherence is especially important because it requires long-term administration of medication.[6] Prolonged non-adherence to antihypertensive medication leads to complications such as cardiovascular and renal diseases which adversely affect the lifespan and the quality of life.[2,7] In fact, in a Korean population study, the effect of antihypertensive medication adherence on hospitalization due to cardiovascular diseases and all-cause mortality was found to be 1.25 and 1.48 times higher, respectively.[8] Nevertheless, according to the World Health Organization (WHO), approximately 50% to 70% of hypertensive patients are reported to be non-adherent to medication.[2]
Medication adherence is affected by various elements such as factors related to the patient, medication/disease, socioeconomic status, and the healthcare system.[2,6,9,10] There have been continuous studies on the effect of the type and number of antihypertensive drugs on adherence to these medications. However, the results of studies on the relationship between the total number of prescribed drugs and adherence were inconsistent, despite the common belief that adherence will decrease when the number of medications taken simultaneously increases. Some previous studies have reported that adherence decreased as patients took more drugs at the same time,[11–14] whereas others reported that medication adherence rather increased when there were more prescribed medications; so the controversy still remains.[15–18] A possible reason for the inconsistent results in these studies is that most were conducted under specific conditions in certain centers with a relatively small number of subjects for a short observation period. The purpose of this study was to investigate the effect of the total number of prescribed medications on the adherence to antihypertensive medication through a field study of a real-world setting using a large-scale representative data.
2. Methods
2.1. Data source
Our study used the National Health Insurance Service-National Sample Cohort (NHIS-NSC) of Korea, which represents the entire nation's health information quoted by sex, age, income quintiles, etc. NHIS-NSC was formed in 2002 as a cohort sample of 1,048,061 individuals, which accounts for approximately 2.2% of the total population (N = 46,605,433). NHIS-NSC data are obtained through observation every year and include qualification data (birth, death, sex, family relation, address, property, income, type of insurance, etc) and medical service use data (billing statements, medical history, prescription and treatment records, etc) (Fig. 1).[19]
Figure 1.
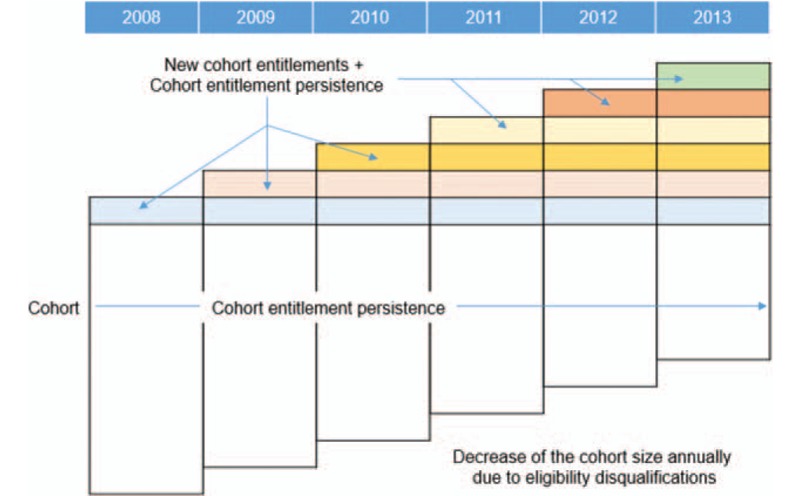
Dynamic cohort design. Cohort size: about 1 million/Y (2.2% of total population) Cohort data include qualification data (birth, death, sex, family relationship, address, property, income, insurance type) and medical service use data (billing statement, medical records, diagnosis record, prescription record, etc).
2.2. Study population
We first selected hypertensive patients taking antihypertensive drugs (N = 193,104) from the NHIS-NSC (1,048,061 cases, total outpatient prescriptions 221,750,977 cases) and examined the data from 2008 to 2013. Hypertensive patients were defined as all subjects with International Classification of Diseases Tenth Revision (ICD-10) codes that included hypertension (I10, I11, I12, I13, I15). The type of antihypertensive drugs included in this study were angiotensin-converting enzyme inhibitors (ACEi), angiotensin II receptor blockers (ARB), beta-blockers (BB), calcium channel blockers (CCB), and diuretics. We included all single and compound drugs (ACEi/CCB, ACEi/diuretics, ARB/CCB, ARB/CCB/diuretics, ARB/diuretics, BB/CCB, BB/diuretics) of these types sold domestically until December 31, 2013, resulting in a total of 239 kinds of antihypertensive drugs under the Anatomical Therapeutic Chemical (ATC) classification.[20] Among the chosen hypertensive patients, those aged 20 years or older were further selected (N = 192,131), and in order to prevent statistical deviations by extreme values, subjects with the upper 0.01% value for the number of total medications and diagnoses were excluded (N = 1759). Subjects who took more than 7 types of antihypertensive drugs simultaneously (1637 patients) were also excluded, because they were considered as exceptional cases that were taking almost all kinds of available antihypertensive drugs. Finally, only the subjects (N = 150,550) who were prescribed antihypertensive drugs for at least 1 year were selected to achieve a more objective and stable measurement and comparison of medication adherence (Fig. 2). The extracted subjects were divided into 5 groups according to the total number of drugs taken: 1–2, 3–4, 5–6, 7–8, and 9 or more. The Seoul National University Hospital institutional review board (IRB) approved this study (IRB No. E-15-5-079-673), and written informed consent was waived because NHIS-NSC was anonymized under strict guidelines of confidentiality. This study was approved by the NHIS review committee for research support (NHIS-2017-2-610).
Figure 2.
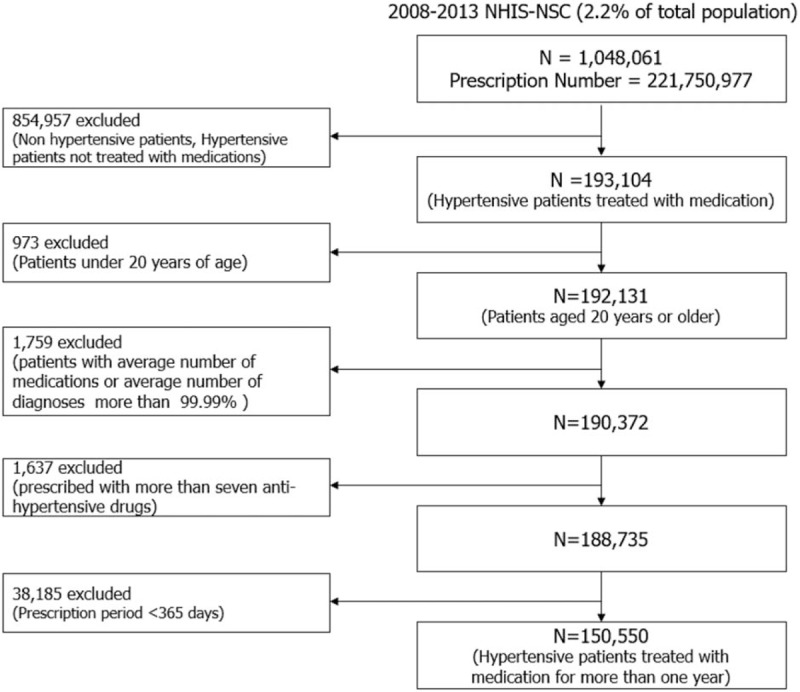
Study population and data collection. NHIS-NSC = National Health Insurance Service-National Sample Cohort.
2.3. Method of measuring medication adherence
Medication adherence was measured using the Medication Possession Ratio (MPR), which is one of the most commonly used indirect measurement indices.[6,9,21] MPR is calculated by dividing the total days supplied (excluding supplied days for the last clinic visit) of medication by the number of days between the first and last refills.[9] If the MPR is less than 80%, it is considered as non-adherence.[9] In this study we defined MPRs calculated over 100% as 100%.
MPR = total days supplied /number of days between the first and last refills (prescription period)
2.4. Factors associated to medication adherence
Medication adherence is known to be determined by factors related to the patient, medication/disease, socioeconomic status, the healthcare system, etc.[2,6,9,10] In our study, factors related to the patient (age, sex, severity of disability), social/economic status (income level, residential area), medication/disease (cost of antihypertensive drugs, prescription period, total days supplied of antihypertensive drugs), and healthcare system (insurance coverage) were obtained as confounders and analyzed. The income level was evaluated on a scale of 0 to 10 and divided into tertiles. Other factors such as education level, occupation, associated symptoms, side effects of treatment, accompanying family/caregiver status, and physician factors are also known to affect adherence, but these factors were not included as variables in the study since they were not available in the NHIS-NSC data (Fig. 3). As a result, we adjusted the confounders for age, sex, severity of disability, income, residential area, health insurance coverage, average cost of antihypertensive medication, and prescription period. Total number of drugs prescribed was determined as the average number of drugs prescribed to the subjects during the study period.
Figure 3.
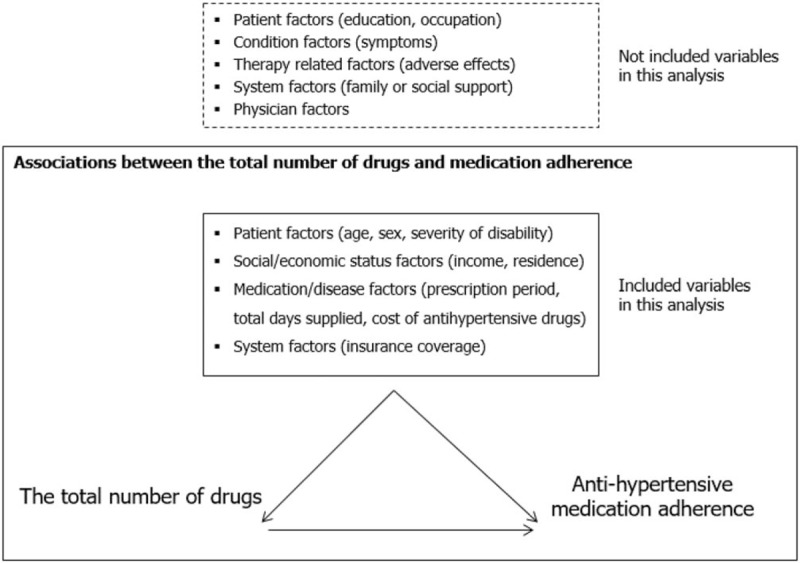
Analysis scheme for investigating associations between the total number of drugs and anti-hypertensive medication adherence.
2.5. Statistical analysis
The subjects were divided into 5 groups according to the total number of medications; 1–2, 3–4, 5–6, 7–8, and 9 or more. We measured and compared the prevalence of medication adherence among the 5 groups before and after adjustment for confounding factors via analysis of covariance (ANCOVA). We performed a subgroup analysis to determine changes and trends of adherence according to age (20–39, 40–49, 50–59, 60–69, 70–79, ≥80 years) before and after correcting the confounding factors. In order to confirm the relationship between the number of medications and adherence to antihypertensive medications, the odds ratio of non-adherence according to the number of medications was estimated through logistic regression analysis. All analyses were performed using STATA version 14.0 (Stata Corp., College Station, TX) and statistical significance was defined as P values <.05.
3. Results
3.1. Basic characteristics of the subjects
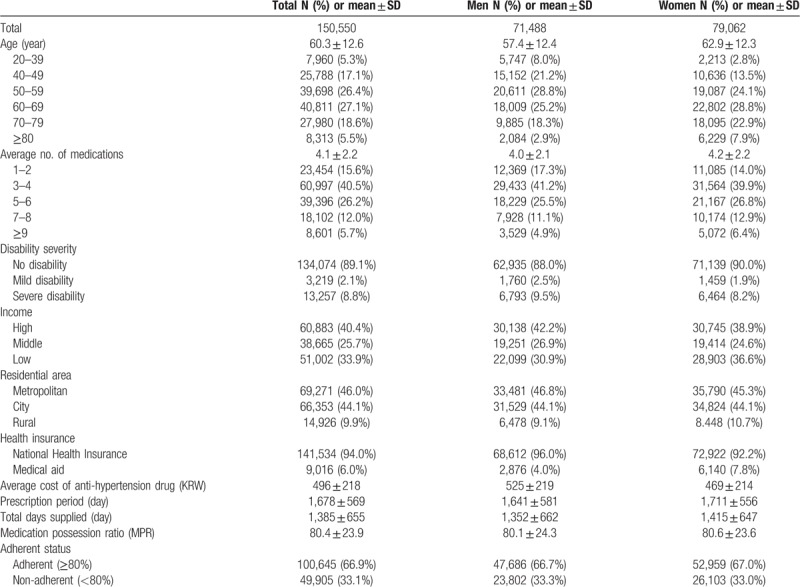
Of the 150,550 subjects, 71,488 (47.5%) were male and 79,062 (52.5%) were female. The mean age of the subjects was 60.3 ± 12.6 years. Of the total subjects, 5.3% were aged 20 to 39 years, 17.1% were aged 40 to 49 years, 26.4% were aged 50 to 59 years, 27.1% were aged 60 to 69 years, 18.6% were aged 70 to 79 years and 5.5% were aged 80 years or older. The median number of total medications taken by the subjects was 4.1 ± 2.2. There were 23,454 patients (15.6%) with 1–2 total medications, 60,997 (40.5%) with 3–4, 39,396 (26.2%) with 5–6, 18,102 (12.0%) with 7–8, and 8601 (5.7%) with 9 or more. In terms of disability, 134,074 patients (89.1%) were non-disabled, 3219 (2.1%) were mildly disabled, and 13,527 patients (8.8%) were severely disabled. After examining the social/economic (income, residential area) and healthcare system factors (insurance coverage) of the subjects, 40.4% were found in the high-income class, 25.7% were in the middle-income class, and 33.9% were in the low-income class. By residence, 46.0% resided in metropolitan areas, 44.1% in cities, and 9.9% in rural areas. Of the subjects, 94.0% were beneficiaries of the National Health Insurance, and 6.0% were covered by medical aid. The average unit price of antihypertensive drugs was 496 Korean won (equivalent to about 0.5 US dollar), and the average prescription period was 1678 ± 569 days (Table 1).
Table 1.
Baseline characteristics (n = 150,550).
3.2. Adherence to antihypertensive medication according to sex and age
The mean MPR (crude mean) of all subjects was 80.4 ± 23.9%, 80.1 ± 24.3% for men and 80.6 ± 23.6% for women (Table 1). The crude mean (adjusted mean) of MPR of the groups according to the total number of medications was 78.6% (79.5%) for 1–2 drugs group, 81.3% (80.7%) for 3–4 drugs group, 81.1% (80.6%) for 5–6 drugs group, 80.3% (80.8%) for 7–8 drugs group, and 75.5% (78.6%) for 9 or more drugs group. The overall tendency of antihypertensive medication adherence according to the total number of drugs demonstrated an inverted U-shape with a peak at 3–4 total prescribed drugs (Table 2). The results of the subgroup analysis according to sex were also similar in trends with the results of the whole subjects (data were not shown).
Table 2.
Anti-hypertensive medication adherence according to the total number of drugs and age.
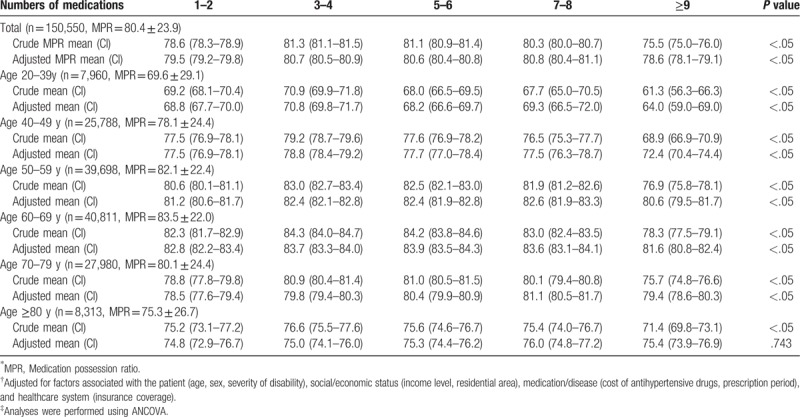
By age group, adherence in the 20 to 39 group was the lowest with 69.6%, and it gradually increased as the age increased with the adherence being at 78.1% and 82.1% in the 40 to 49 and 50 to 59 age group, respectively. Adherence peaked at 60 to 69 age group with 83.5%, after which it decreased progressively as the age increased with adherence being 80.1% and 75.3% in the 70 to 79 age group and 80 years or older group, respectively (Table 2). When the total number of medications was increased, the adherence tendency to antihypertensive agents displayed an inverted U-shape peaking at 3–4 total drugs in all age groups, although there were some level of differences (Table 2, Fig. 4). Adherence consistently increased from 20 to 69 years of age and tended to decrease starting from 70 years of age (Table 2, Fig. 4). This tendency still remained similar even after adjusting for confounding variables (Table 2).
Figure 4.
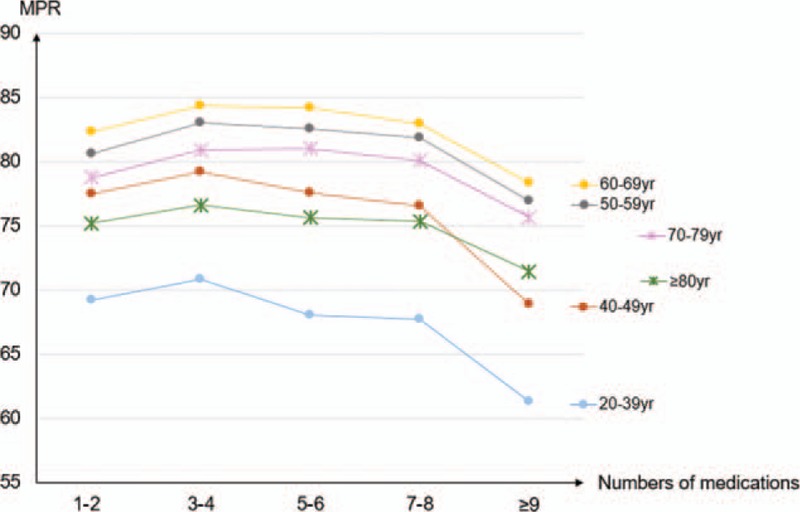
Trends for anti-hypertensive medication adherence according to the total number of drugs and age. MPR = Medication possession ratio, yr = years.
Of the total subjects, 100,645 (66.9%) were adherent patients (MPR ≥ 80%), of which 47,686 (66.7%) were men and 52,959 (67.0%) were women (Table 1). The proportion of adherent patients according to the total number of medications also featured an inverted U-shape with a peak at 3–4 total drugs, regardless of the age group, similar to how the overall MPR tendency based on total medications was displayed. After peaking at 3–4 total prescribed drugs, the proportion of adherent patients gradually decreased as the total number of drugs increased and decreased significantly when 9 or more total drugs were taken in all age groups. The proportion of adherent patients in the 20 to 39 age group was below 50.7%, regardless of the total number of drugs. Patients in the 60 to 69 age group demonstrated the highest proportion of adherent patients with more than 63.7% being adherent regardless of the total number of medications. The proportion of adherent patients tended to decrease again in the 70 years or older group. When the same number of drugs was taken, the proportion of adherent patients according to the age group showed an inverted U-shape with a peak at 60 to 69 years (Fig. 5).
Figure 5.
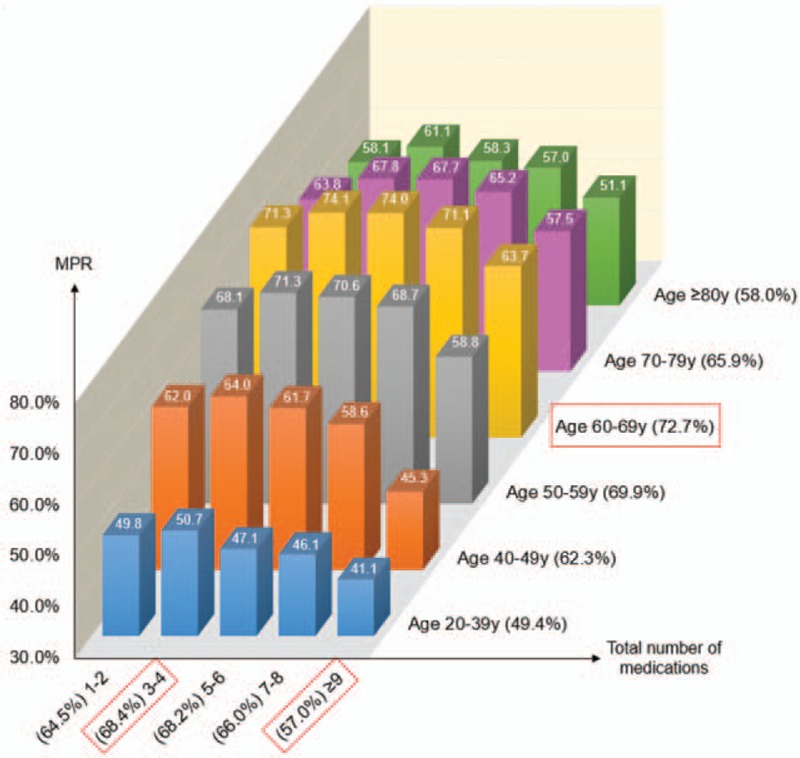
Proportion of adherent patients according to the total number of drugs and age. MPR = Medication possession ratio, y = years. Definition of adherent patient: patient with anti-hypertensive medication possession ratio ≥8.
3.3. Relationship between the number of medications and adherence of antihypertensive agents
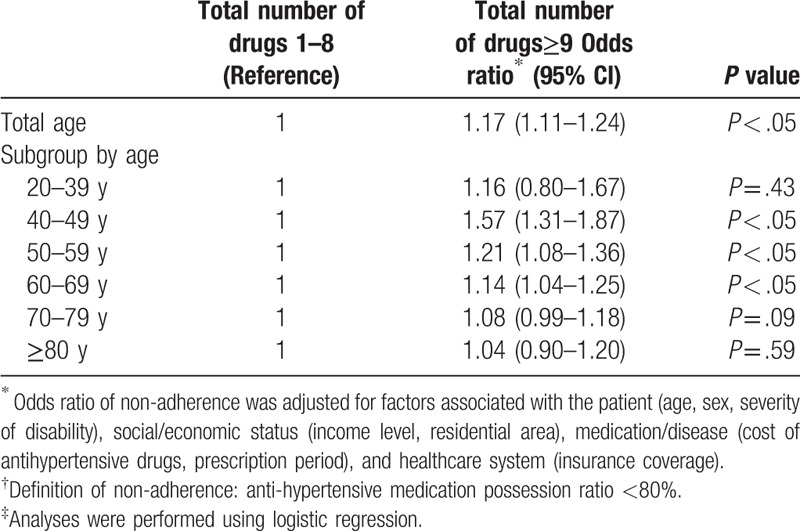
To confirm the relationship between the number of total medications and the adherence to antihypertensive drugs, the relative odds ratio of non-adherence (MPR < 80%) according to the total drug numbers was compared after adjusting for confounding variables. Overall, when 9 or more total drugs were taken, the odds ratio (95% confidence interval, [CI]) of non-adherence was 1.17 (1.11–1.24) compared with those taking 1–8 total drugs and the result was statistically significant (P < .05). In the age subgroups of 20 to 39, 40 to 49, 50 to 59, 60 to 69, 70 to 79 and 80 years or older, the odds ratios (95% CI) of non-adherence when taking 9 or more drugs were 1.16 (0.80–1.67), 1.57 (1.31–1.87), 1.21 (1.08–1.36), 1.14 (1.04–1.25), 1.08 (0.99–1.18), and 1.04 (0.90–1.20), respectively, compared with those taking 1–8 total drugs. These results were statistically significant (P < .05) in the 40 to 49, 50 to 59, and 60 to 69 age groups, borderline significant in the 70 to 79 age group, and non-significant in the 20 to 39 and 80 years or older age groups (Table 3).
Table 3.
Relationship between the total number of drugs and non-adherent patient.
4. Discussion
This study used large-scale data of NHIS-NSC to analyze the relationship between the number of prescribed drugs and adherence to antihypertensive agents. After observing the cohort subjects who continued to take antihypertensive agents for more than one year and a maximum of 6 years, the mean MPR was found to be 80.4%. In addition, the age distribution of patients taking antihypertensive drugs was 0.7% in their 20s, 4.6% in their 30s, 17.1% in their 40s, 26.4% in their 50s, 27.1% in their 60s, and 5.5% in those aged 80 years or older, respectively. These results are not much different from the results of a 1 year study of antihypertensive medication compliance using large-scale claims and qualification data of the National Health Insurance of Korea conducted by Park et al.[22] Moreover, the prevalence of age specific hypertension reported by the Korean National Health and Nutrition Survey (KNHANES) from 2007 to 2013 was also similar. Thus, the NHIS-NSC data used in this study can be considered to represent the characteristics of the whole population in a balanced manner.
Interestingly, our results of antihypertensive adherence in relation to the number of total prescribed drugs for all subjects revealed the tendency of an inverted U-shape with a peak at 3–4 total medications regardless of age (Fig. 4). In contrast to the general belief that medication adherence will decrease as the number of medications increases, the adherence was higher when the number of prescribed drugs was 3–4 than that of 1–2 in our study. The reason for this can be interpreted by the health belief model. Those who believe that they are sick will be more alert to their general health status, and as a result they will make extra efforts to maintain their well-being.[23,24] Therefore, patients who are taking 3–4 total drugs believe they are more ill than patients prescribed with 1–2 drugs and they will make additional efforts to take the drugs as prescribed by the physician, which will ultimately lead to higher adherence.[15,25] This trend is consistent with other previous studies.[15,26]
On the other hand, when the number of prescribed medications exceeds 3–4, the adherence started to decrease again. This can be explained by the result of regimen complexity due to increased prescribed drugs. Also, the more multiple- drug therapy patients receive, the greater likelihood of incidence of adverse effects occurring due to multi-drug interactions, which leads to increase in non-adherence.[27]
When analyzed by age group, adherence increased with increase in age up to 69 years, and started to decrease after that point. (Table 2, Fig. 4). In a study that analyzed the persistence with antihypertensive agents for 10 years, the persistence was higher in the elderly population (aged ≥60 years) than in the 20 to 59 age group.[28] Some other studies also reported that medication adherence increases with age.[29–32] The reason for this tendency is that older patients generally have greater severity of illness than younger ones, which increases their awareness about their health status, and this seems to have a positive effect on adherence.[33]
Meanwhile, there were also previous studies that reported that medication adherence decreased with increasing age in the elderly population.[34,35] In our study, adherence to antihypertensive agents started to decrease when subjects were aged 70 years or more. This suggests that impairment of cognitive and physical function in the elderly population may lead to more frequent cases of omitted drug use. In fact, there were reports that chronically ill patients aged 75 years or older had a higher medication error rate than patients who were younger than 75 years.[36] Therefore, cognitive impairment in elderly patients is an independent risk factor that increases non-adherence to medication,[37,38] and physical dysfunction can work as a barrier to taking prescribed drugs adequately.[39]
The above discussion is more evident in the analysis of the percentage of adherent patients (MPR ≥ 80%) according to the total number of drugs and age. In this study, the proportion of adherent patients displayed an inverted U-shape pattern with increasing number of drugs, regardless of age, and peaked when the number of drug was 3–4. In addition, the proportion of adherent patients was the lowest in 20 to 39 age group and gradually increased with age, peaked in the 60 to 69 age group and decreased again in the 70 or older age group. It is known that hypertensive patients in their 20s and 30s are 10 to 12 times more likely to have non-persistence with antihypertensive agents compared with those in their 50s or older.[40,41] In this regard, young hypertensive patients are relatively reluctant to take medications, so the proportion of adherent patients is low. The percentage of adherent patients increased until the age 60 to 69 years and started to decrease after age 70. This can be explained by the health belief model[23,24] and the cognitive impairment[37,38] and physical dysfunctions[39] in extremely old patients mentioned in previous paragraphs.
Finally, the degree of non-adherence (MPR < 80%) was compared using odds ratio when the total prescribed drugs were 9 or more and 1–8. When the total number of drugs was 9 or more, the odds ratio of non-adherence was 1.17 compared with those taking 1–8 total drugs. This tendency was more pronounced when analyzed according to age groups, with the odds ratio of non-adherence being highest in the 40 to 49 age group and the level of non-adherence improving gradually as age increased. In particular, the odds ratio was borderline significant in 70 to 79 age group, and non-significant in the 80 years or older group (Table 3). The difference in degree of non-adherence according to age groups can be explained in relation to the initiation time of treatment for hypertension. The adherence to antihypertensive medication is generally known to be relatively low in the early hypertension treatment phase when hypertensive medication is initiated.[42] In fact, according to another Korean study using claims data, Korean patients who started antihypertensive medication had MPRs less than 60% in the first year, and the rate of good adherence (MPR ≥ 80%) was less than 40%.[43] Hypertensive patients in their 40s are more likely to have been in the early phase of treatment than those in their 50s or older, and this might have resulted in the higher odds ratio of non-adherence in the 40 to 49 age group when the total drugs were 9 or more.
In contrast, subjects in their 20sand 30s who have the highest possibility of being at the early phase of hypertension treatment, had a 1.16 odds ratio of non-adherence, which is smaller than the odds ratio of that in their 40s; but this result was not statistically significant. Generally, few patients take antihypertensive agents in their 20s and 30s,[22,44] and subjects who take 9 or more total drugs in the 20 to 39 age group were also relatively rare in this study (about 1.6%, N = 129 out of 7960). In addition, the overall proportion of adherent patients in their 20s and 30s was low (49.4%) in the first place, so it would be difficult to discuss the cause of the above result, which is presently non-significant. Further analysis of the factors related to antihypertensive medication adherence in young adults with 20 to 39 years of age would be needed in the near future.
The strength of this study is that we measured the adherence to antihypertensive medications according to the total number of prescribed drugs and age by observing subjects who were continuously taking antihypertensive agents for more than year for a long period with a large-scale sample which is approximately 2.2% of the Korean population. There were some similar studies in the past, but they were mostly analyzed either with smaller sample of subjects,[11–13,15–18] or for shorter periods of observation.[11,12,14–18] Moreover, this study has the strength of analyzing various confounding variables through qualification and medical utilization data of subjects in the NHIS-NSC. We attempted to improve the objectivity of the results by adjusting the factors that can affect medication adherence, such as age, sex, income level, health insurance type, price of the antihypertensive agents, and prescription period.
On the other hand, this study also has some limitations. First of all, our study calculated the adherence using MPR, which is one of the widely used indirect methods for measuring drug compliance.[9] In practice, however, patients can also seek medication from sources that do not appear in the NHIS-NSC (eg, drug samples, sharing drugs with other people, receiving drugs from someone else).[45] Furthermore, some patients visit the clinic and receive medication prescription regularly but do not actually take the drugs; this kind of behavior cannot be reflected in the MPR calculation. Therefore, adherence can be sometimes underestimated or overestimated when using MPR.[21,46,47] Moreover, MPR can be over 100% theoretically, if the patient gets early refills before the drug completely runs out and this can also lead to an overestimation of adherence. Nonetheless, MPR is one of the most commonly used methods for measuring medication adherence due to its relatively high objectivity and accessibility, and is especially known as the best tool for assessing the compliance to antihypertensive medication using retrospective data.[6,46] Also, we capped MPR at 100% for MPRs over 100% to neutralize the possible overestimation as many studies do. Another limitation of this study is that we could not include other factors that can potentially affect medication adherence such as the patient's conditions (eg, self-efficacy, understanding of purpose of medication, specific comorbidities), relationship between the patient and healthcare provider, and other social/economic factors (eg, education level, occupation). In fact, we did include comorbidities as confounding factors in our initial analysis and the overall tendency of results were similar as the final analysis. However, the degree of collinearity between the total number of drugs and the diagnoses were too strong. Furthermore, the subjects can be diagnosed with new diseases at any point of the observation period but these new diagnoses at a certain point cannot be regarded as having influenced the medication adherence during the whole observation period. Therefore, we ultimately excluded the comorbidities in the final analysis.
Lastly, our study did not distinguish the specific type of drugs that were prescribed along with antihypertensive agents. Even if the patients take the same number of drugs, adherence may vary depending on the components of the medications being taken. However, it is nearly impossible to identify every single drug that was prescribed to the subjects during the whole observation period when analyzing with real-world data such as the NHIS-NSC. Thus, we settled to reflect polypharmacy status of the subjects by presenting average number of total drugs of the observation period. The analysis would have been more complete if the class of concurrent medications was adjusted as a confounding factor. If further analysis is conducted by reflecting these limitations in the near future, more objective and meaningful results will be obtained.
5. Conclusions
In conclusion, the relation between the patient's age and total number of prescribed drugs and antihypertensive medication adherence demonstrated an inverted U-shape with a peak at 3–4 total drugs and at age 60 to 69 years. In particular, when 9 or more total drugs were taken, adherence decreased significantly, regardless of age. Therefore, clinicians need to take a more strategic approach to improve adherence to antihypertensive medications, depending on the total number of prescribed drugs and the age of the patient.
Author contributions
Conceptualization: Seung Jae Kim, Ho Chun Choi.
Data curation: Seung Jae Kim, Oh Deog Kwon, Ho Chun Choi.
Formal analysis: Seung Jae Kim, Oh Deog Kwon, Ho Chun Choi.
Methodology: Seung Jae Kim, Ho Chun Choi.
Project administration: Ho Chun Choi.
Supervision: Ho Chun Choi.
Writing – original draft: Seung Jae Kim.
Writing – review & editing: Seung Jae Kim, Eunice Bormee Han, Cheol Min Lee, Seung-Won Oh, Hee-Kyung Joh, Bumjo Oh, Hyuktae Kwon, BeLong Cho, Ho Chun Choi.
Seung Jae Kim orcid: 0000-0001-8885-7137.
Footnotes
Abbreviations: MPR = medication possession ratio, NHIS-NSC = National Health Insurance Service-National Sample Cohort.
How to cite this article: Kim SJ, Kwon OD, Han EB, Lee CM, Oh SW, Joh HK, Oh B, Kwon H, Cho B, Choi HC. Impact of number of medications and age on adherence to antihypertensive medications: A nationwide population-based study. Medicine. 2019;98:49(e17825).
The authors have no conflicts of interests to disclose.
References
- [1].AM D Improving medication adherence. Clin Diabetes 2006;2006:71–7. [Google Scholar]
- [2].Sabaté E. Adherence to Long-term Therapies: Evidence for Action. Geneva, Switzerland:World Health Organization; 2003. [Google Scholar]
- [3].Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005;353:487–97. [DOI] [PubMed] [Google Scholar]
- [4].Mennini FS, Marcellusi A, von der Schulenburg JM, et al. Cost of poor adherence to anti-hypertensive therapy in five European countries. Eur J Health Econ 2015;16:65–72. [DOI] [PubMed] [Google Scholar]
- [5].Chisholm-Burns MA, Spivey CA. The ’cost’ of medication nonadherence: consequences we cannot afford to accept. J Am Pharm Assoc (2003) 2012;52:823–6. [DOI] [PubMed] [Google Scholar]
- [6].Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation 2009;119:3028–35. [DOI] [PubMed] [Google Scholar]
- [7].Law M, Morris J, Wald N. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009;338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Shin S, Song H, Oh S-K, et al. Effect of antihypertensive medication adherence on hospitalization for cardiovascular disease and mortality in hypertensive patients. Hypertens Res 2013;36:1000. [DOI] [PubMed] [Google Scholar]
- [9].Iuga AO, McGuire MJ. Adherence and health care costs. Risk Manag Healthc Policy 2014;7:35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Tajouri TH, Driver SL, Holmes DR., Jr ’Take as directed’—strategies to improve adherence to cardiac medication. Nat Rev Cardiol 2014;11:304–7. [DOI] [PubMed] [Google Scholar]
- [11].Chapman RH, Petrilla AA, Benner JS, et al. Predictors of adherence to concomitant antihypertensive and lipid-lowering medications in older adults. Drugs Aging 2008;25:885–92. [DOI] [PubMed] [Google Scholar]
- [12].Gazmararian JA, Kripalani S, Miller MJ, et al. Factors associated with medication refill adherence in cardiovascular-related diseases. J Gen Intern Med 2006;21:1215–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ghembaza MA, Senoussaoui Y, Tani MK, et al. Impact of patient knowledge of hypertension complications on adherence to antihypertensive therapy. Curr Hypertens Rev 2014;10:41–8. [DOI] [PubMed] [Google Scholar]
- [14].Holmes HM, Luo R, Hanlon JT, et al. Ethnic disparities in adherence to antihypertensive medications of medicare part D beneficiaries. J Am Geriatr Soc 2012;60:1298–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Shalansky SJ, Levy AR. Effect of number of medications on cardiovascular therapy adherence. Ann Pharmacother 2002;36:1532–9. [DOI] [PubMed] [Google Scholar]
- [16].Grégoire J-P, Moisan J, Guibert R, et al. Predictors of self-reported noncompliance with antihypertensive drug treatment: a prospective cohort study. Can J Cardiol 2006;22:323–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Natarajan N, Putnam W, Van Aarsen K, et al. Adherence to antihypertensive medications among family practice patients with diabetes mellitus and hypertension. Can Fam Physician 2013;59:e93–100. [PMC free article] [PubMed] [Google Scholar]
- [18].Siegel D, Lopez J, Meier J. Antihypertensive medication adherence in the Department of Veterans Affairs. Am Jf Med 2007;120:26–32. [DOI] [PubMed] [Google Scholar]
- [19].Lee J, Lee JS, Park S-H, et al. Cohort profile: the national health insurance service–national sample cohort (NHIS-NSC), South Korea. Int J Epidemiol 2016;46:e15–15. [DOI] [PubMed] [Google Scholar]
- [20].Organization WH. The Anatomical Therapeutic Chemical Classification System with Defined Daily Doses (ATC/DDD). Oslo:WHO; 2006. [Google Scholar]
- [21].Andrade SE, Kahler KH, Frech F, et al. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf 2006;15:565–74. [DOI] [PubMed] [Google Scholar]
- [22].Park JH, Shin Y, Lee SY, et al. Antihypertensive drug medication adherence and its affecting factors in South Korea. Int J Cardiol 2008;128:392–8. [DOI] [PubMed] [Google Scholar]
- [23].Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q 1988;15:175–83. [DOI] [PubMed] [Google Scholar]
- [24].Rosenstock IM. Why people use health services. Milbank Q 2005;83:1–32. Online-only-Online-only. [Google Scholar]
- [25].Billups SJ, Malone DC, Carter BL. The relationship between drug therapy noncompliance and patient characteristics, health-related quality of life, and health care costs. Pharmacotherapy 2000;20:941–9. [DOI] [PubMed] [Google Scholar]
- [26].Grant RW, O’Leary KM, Weilburg JB, et al. Impact of concurrent medication use on statin adherence and refill persistence. Arch Intern Med 2004;164:2343–8. [DOI] [PubMed] [Google Scholar]
- [27].Munger MA, Van Tassell BW, LaFleur J. Medication nonadherence: an unrecognized cardiovascular risk factor. MedGenMed 2007;9:58. [PMC free article] [PubMed] [Google Scholar]
- [28].Van Wijk BL, Klungel OH, Heerdink ER, et al. Rate and determinants of 10-year persistence with antihypertensive drugs. J Hypertens 2005;23:2101–7. [DOI] [PubMed] [Google Scholar]
- [29].Monane M, Bohn RL, Gurwitz JH, et al. Compliance with antihypertensive therapy among elderly Medicaid enrollees: the roles of age, gender, and race. Am J Public Health 1996;86:1805–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hashmi SK, Afridi MB, Abbas K, et al. Factors associated with adherence to anti-hypertensive treatment in Pakistan. PLoS One 2007;2:e280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Marentette MA, Gerth WC, Billings DK, et al. Antihypertensive persistence and drug class. Can J Cardiol 2002;18:649–56. [PubMed] [Google Scholar]
- [32].Shaya FT, Du D, Gbarayor CM, et al. Predictors of compliance with antihypertensive therapy in a high-risk medicaid population. J Natl Med Assoc 2009;101:34–9. [DOI] [PubMed] [Google Scholar]
- [33].Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q 1984;11:1–47. [DOI] [PubMed] [Google Scholar]
- [34].B G How can we improve the effectiveness of treatment in elderly hypertensives? Blood Press 2005;2:46–9. [DOI] [PubMed] [Google Scholar]
- [35].Cárdenas-Valladolid J, Martín-Madrazo C, Salinero-Fort MA, et al. Prevalence of adherence to treatment in homebound elderly people in primary health care. Drugs Aging 2010;27:641–51. [DOI] [PubMed] [Google Scholar]
- [36].Schwartz D, Wang M, Zeitz L, et al. Medication errors made by elderly, chronically ill patients. Am J Public Health Nations Health 1962;52:2018–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Salas M, In’t Veld BA, van der Linden PD, et al. Impaired cognitive function and compliance with antihypertensive drugs in elderly: the Rotterdam Study. Clin Pharmacol Ther 2001;70:561–6. [DOI] [PubMed] [Google Scholar]
- [38].Alosco ML, Spitznagel MB, van Dulmen M, et al. Cognitive function and treatment adherence in older adults with heart failure. Psychosom Med 2012;74:965–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Turner A, Hochschild A, Burnett J, et al. High prevalence of medication non-adherence in a sample of community-dwelling older adults with adult protective services-validated self-neglect. Drugs Aging 2012;29:741–9. [DOI] [PubMed] [Google Scholar]
- [40].Bautista LE. Predictors of persistence with antihypertensive therapy: results from the NHANES. Am J Hypertens 2008;21:183–8. [DOI] [PubMed] [Google Scholar]
- [41].Elliott WJ. Improving outcomes in hypertensive patients: focus on adherence and persistence with antihypertensive therapy. J Clin Hypertens 2009;11:376–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Payne KA, Esmonde-White S. Observational studies of antihypertensive medication use and compliance: is drug choice a factor in treatment adherence? Curr Hypertens Rep 2000;2:515–24. [DOI] [PubMed] [Google Scholar]
- [43].Sung S-K, Lee S-G, Lee K-S, et al. First-year treatment adherence among outpatients initiating antihypertensive medication in Korea: results of a retrospective claims review. Clin Ther 2009;31:1309–20. [DOI] [PubMed] [Google Scholar]
- [44].Hales CM, Carroll MD, Simon PA, et al. Hypertension prevalence, awareness, treatment, and control among adults aged ≥18 years—Los Angeles county, 1999–2006 and 2007–2014. MMWR Morb Mortal Wkly Rep 2017;66:846–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Shin DW, Park JH, Park JH, et al. Antihypertensive medication adherence in cancer survivors and its affecting factors: results of a Korean population-based study 2011;19:211–20. [DOI] [PubMed] [Google Scholar]
- [46].Halpern MT, Khan ZM, Schmier JK, et al. Recommendations for evaluating compliance and persistence with hypertension therapy using retrospective data. Hypertension 2006;47:1039–48. [DOI] [PubMed] [Google Scholar]
- [47].Arnet I, Abraham I, Messerli M, et al. A method for calculating adherence to polypharmacy from dispensing data records 2014;36:192–201. [DOI] [PMC free article] [PubMed] [Google Scholar]


