Abstract
The role of Porphyromonas gingivalis (P. gingivalis) or its virulence factors, including lipopolysaccharide (LPS) not only has been related with periodontitis but also with endothelial dysfunction, a key mechanism involved in the genesis of atherosclerosis and hypertension that involving systemic inflammatory markers as angiotensin II (Ang II) and cytokines. This study compares the effect of repeated and unique exposures of P. gingivalis W83 LPS and live bacteria on the production and expression of inflammatory mediators and vasoconstrictor molecules with Ang II. Human coronary artery endothelial cells (HCAEC) were stimulated with purified LPS of P. gingivalis (1.0, 3.5 or 7.0 μg/mL) or serial dilutions of live bacteria (MOI 1: 100 - 1:0,1) at a single or repeated exposure for a time of 24 h. mRNA expression levels of AGTR1, AGTR2, IL-8, IL-1β and MCP-1 were determined by RT-qPCR, and IL-6, MCP-1, IL-8, IL-1β and GM-CSF levels were measured by flow cytometry, ELISA determined Ang II levels. Live bacteria in a single dose increased mRNA levels of AGTR1, and repeated doses increased mRNA levels of IL-8 and IL-1β (p < 0.05). Repeated exposure of live-P. gingivalis induced significant production IL-6, MCP-1 and GM-CSF (p < 0.05). Moreover, these MCP-1, IL-6 and GM-CSF levels were greater than in cells treated with single exposure (p < 0.05), The expression of AGTR1 and production of Ang II induced by live-P. gingivalis W83 showed a vasomotor effect of whole bacteria in HCAEC more than LPS. In conclusion, the findings of this study suggest that repeated exposure of P. gingivalis in HCAEC induces the activation of proinflammatory and vasoconstrictor molecules that lead to endothelial dysfunction being a key mechanism of the onset and progression of arterial hypertension and atherosclerosis.
Subject terms: Hypertension, Periodontitis, Infection
Introduction
Inflammation has received much attention as an determining factor in hypertension and atherosclerosis progression1,2. Although the effect of inflammation on endothelial dysfunction has been widely studied, the mechanisms of inflammation in hypertension have not been completely elucidated2.
Chronic systemic inflammation induced by periodontitis is linked to endothelial dysfunction due to the entry of Gram-negative anaerobes into the bloodstream after various stimuli, such as tooth brushing and chewing3 and periodontal treatment3–5 likewise, DNA6,7 of periodontal pathogens (e.g., Porphyromonas gingivalis) and live bacteria8,9 have been demonstrated in atherosclerotic coronary lesions10,11, and increased systemic inflammatory markers induced by endotoxemia have been associated with hypertension/early atherosclerosis and periodontal disease12,13. Hence, there is a potential association between vascular inflammation and cardiovascular disease (CVD), since endothelial cells are the primary targets of immunological attack in inflammatory responses14.
The endothelium has been described as a secretory unit of pathogen-associated molecular patterns (PAMPs) that generates secreting soluble mediators. Cytokines and chemokines, as well as other products such as reactive oxygen species and metalloproteinases (MMPs) have been correlated with greater atheromatous lipid core increases in the presence of monocytes-macrophages and in the levels of IL-8, MCP-1, MMP-8 and MMP-9 in atherosclerotic plaques15,16. P. gingivalis, a major periodontal pathogen in periodontitis, has been shown to stimulate cytokine/chemokine production, which induces expression of cell adhesion molecules, including intercellular adhesion molecule (ICAM-1), vascular cell adhesion molecule (VCAM-1) and p-selectin, which are considered key steps in the onset of endothelial dysfunction17,18. P. gingivalis also activates endothelial cells, triggers smooth muscle cell proliferation and therefore impairs vasomotor function19,20.
The evolving role of Ang II as a regulator of endothelial cell function and its action by stimulating various receptors, specifically angiotensin II type 1 receptor (AGTR1) stimulates oxidative stress, fibrosis, cell proliferation and a release of cytokines and chemokines which in turn mediates tissue inflammation21,22. Recently, the evidence has indicated that low-grade inflammation may be involved in the development of hypertension23. In fact, the initiation or progression of periodontitis might involve a local renin-angiotensin system (RAS) activation21,22, that could lead to an increase in blood pressure, a decrease in nitric oxide, inflammation and development of atherosclerosis and endothelial dysfunction22,24,25.
Several bacteraemia episodes occur continuously in patients with periodontitis and are even induced by daily dental-care activities (i.e., brushing, flossing and chewing)26,27. Repeated episodes are also generated during intensive periodontal treatments that could induce an inflammatory acute response in the endothelium28,29. Although many reports examining P. gingivalis have demonstrated vascular endothelium activation through the selective recruitment of leukocytes to inflammatory foci in HCAEC via Toll-like receptor 2 (TLR2) after a single exposure to endotoxin16,30,31, it has been not studied in an in-vitro approach using repeated exposure in endothelial models of inflammatory responses. Therefore, these in-vitro cell models do not represent or mimic the vascular pathophysiology in patients with periodontitis, since the endothelium is exposed to repeated and accumulative doses of transient endotoxemia that could represent changes in the response, compared to the single exposure models. The purpose of this study was to compare the inflammatory and vasoactive response of Ang II of HCAEC stimulated with single and repeated exposure of lipopolysaccharide (P. gingivalis-LPS) and live-P. gingivalis W83.
Results
Effect of P. gingivalis on the expression of AGTR1, AGTR2, IL-8, IL-1β, MCP-1 in HCAEC
The biochemical characterization to confirm the degree of purity of LPS of P. gingivalis W83 showed a semi-rough LPS chemotype with bands of low molecular weight free of contaminants such as nucleic acids and proteins high endotoxic activity at very low concentrations similar to observed by commercial LPS (P. gingivalis ATCC 33277, InvivoGen)32. In relation to cell viability, our results demonstrated that LPS and live bacteria did not affect HCAECs (Fig. 1).
Figure 1.
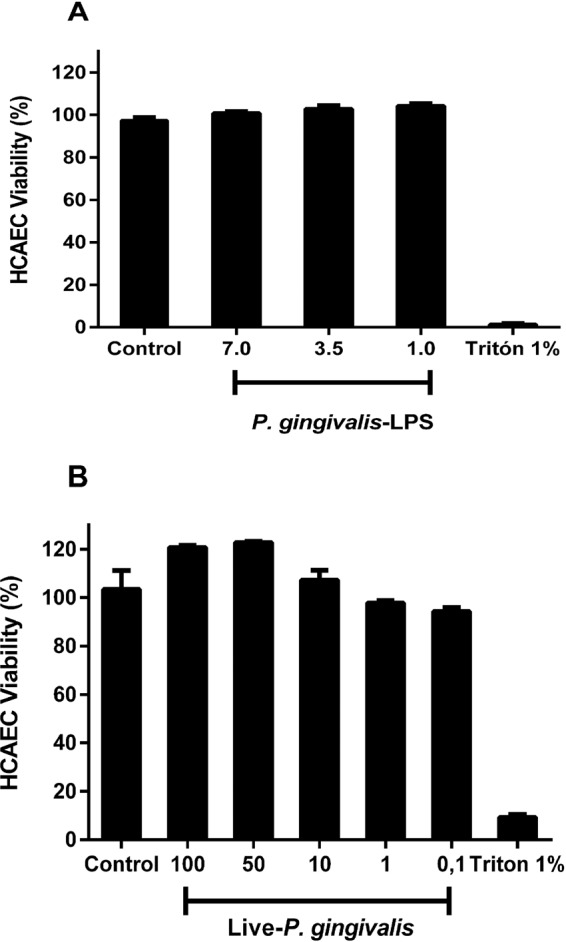
Viability of HCAECs after repeated treatments with live-P. gingivalis (A) and P. gingivalis-LPS (B). The HCAECs were stimulated to repeated live-P. gingivalis (MOI 1:100 - 1:0,1) and P. gingivalis-LPS (1.0, 3.5 and 7.0 µg/mL) exposures, during 24 h. Cell viability was determined according to the fluorometric detection after reduction of resazurin in the resorufin product using AlamarBlue. 1% was considered our positive control of cell death. Percentage of cell viability with respect to the control. *Represents the statistical difference with respect to the control or without stimulus. (p < 0.05). Three independent experiments were performed; the results are presented as the means ± SEM (n = 3).
In this study, we evaluated the expression of proinflammatory cytokine mRNA and AGTR genes in HCAEC stimulated with P. gingivalis-LPS and live-P. gingivalis W83. The cells stimulated at single and repeated exposure with the different concentrations of P. gingivalis-LPS did not show significant changes for any of the pro-inflammatory markers even in comparison with the control group (Fig. 2), while repeated exposure of MOI 1:100 live-P. gingivalis compared to single exposure to the same MOI 1:100, significantly affects the expression of IL-8 and IL-1β (p < 0.05). In contrast, the expression of MCP-1 was not significantly affected by the treatments; however, an apparent reduction in its mRNA was observed after single exposure to LPS and live bacteria. (Fig. 2A–E). On the other hand, a single exposure to live-P. gingivalis increased the AGTR1 expression (Fig. 2A) compared to unchallenged HCAEC and challenged with live bacteria to a repeated exposure (p < 0.05), whereas AGTR2 (Fig. 2B) It was not because of the results of the treatments evaluated.
Figure 2.
mRNA expression levels in HCAEC stimulated with P. gingivalis-LPS or live-P. gingivalis. Monolayers of HCAEC cultured in 12-well plates were stimulated with P. gingivalis-LPS (1.0, 3.5, 7.0 µg/mL) or serial dilutions of P. gingivalis (MOI 1:100- 1:0,1) for 24 h under repeated exposure (+++) or single exposure (+). After stimulation, (A) AGTR1, (B) AGTR2, (C) IL-8, (D) IL-1β, (E) MCP-1, mRNA levels were measured by are expressed as the means by RT-qPCR. Results are expressed as the means ± SEM (n=3). Statiscal significance is represented as *p < 0.05, and (ns) for not significant.
P. gingivalis induces IL-1β, IL-8, IL-6, MCP-1, and GM-CSF production in HCAEC
In a pilot test, HCAEC cells were stimulated at day 1, day 3, and day 5; the supernatant was removed each 48 h to reaching a total of 7 days under repeated exposure. In general, we found similar results in a longer time frame and shorter time frame to induce the production of IL8 in the majority of LPS concentrations assessed (Supplementary Fig. 1). However, in a short period of time an overproduction of IL8 was achieved, suggesting greater endothelial activation than with a long period of time in which endothelial activation appears to decrease. This model could be used to study endotoxin tolerance of periodontal pathogens, an aspect that requires further research. Similarly, when comparing IL6 and IL1, there were also no modifications between the 24 h and 7 day in repeated exposure models (Supplementary Fig. 2).
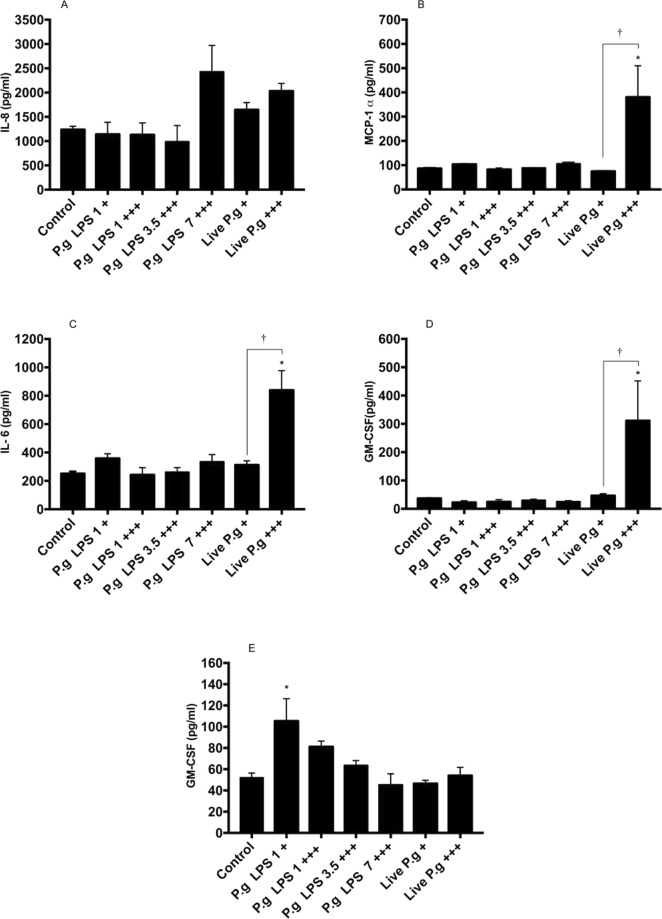
The HCAECs were stimulated with P. gingivalis-LPS or live-P. gingivalis for 24 h by repeated or single exposures to evaluate the levels of IL-8, MCP-1, IL-6, IL-1β and GM-CSF in culture supernatants. Repeated exposure to live-P. gingivalis induced a significant increase in the production of IL-6, MCP-1 and GM-CSF, compared to the control group (p < 0.05), while the P. gingivalis-LPS is a single exposure only induced change in IL-1β (Fig. 3). The chemokine IL-8 was increased mainly in HCAEC challenged with live-P. gingivalis and P. gingivalis-LPS at 7 μg/mL at repeated expositions, but not significantly compared to the control (Fig. 3A). After considering the results so far, endothelial responses differed between approaches. HCAEC to repeated exhibitions with live-P. gingivalis achieved a significantly higher production of MCP-1, IL-6 and GM-CSF than treated endothelial cells at a single exposure of bacteria (Fig. 3B–D), while producing IL-1β (Fig. 3E) was higher in HCAEC challenged with LPS at a single exposure of 1μg/mL (p < 0.05).
Figure 3.
Chemokines and cytokines secreted in HCAEC stimulated with P. gingivalis-LPS or live-P. gingivalis. Monolayers of HCAEC cultured in 12-well plates were stimulated with P. gingivalis-LPS (1.0, 3.5, 7.0 µg/mL) or P. gingivalis (MOI 1:100 - 1:0,1) for 24 h under repeated exposure (+++) or single exposure (+). After stimulation, levels of the following chemokines were measured in cell culture supernatants using a cytometric bead array: (A) IL-8, (B) MCP-1, (C) IL-6, (D) GM-CSF, (E) IL-1β. Symbol (*) means p < 0.05 vs control cells; (**) means p < 0.01 vs control cells; †p < 0.05 compared vs cells treated by single exposure; ††p < 0.01 compared vs cells treated by single exposure; (ns) for not significant. Three independent experiments were performed; the results are presented as the means ± SEM (n = 3).
P. gingivalis increases angiotensin II levels in HCAEC
Ang II concentration was evaluated in HCAEC supernatants after P. gingivalis-LPS stimulation and live-P. gingivalis in single and repeated expositions. Only live-P. gingivalis (MOI 1:100) at repeated exposure significantly increased the concentration of Ang II, compared to the live bacteria single exposure (1.9 times) and the control cells (2.1 times) (Fig. 4).
Figure 4.
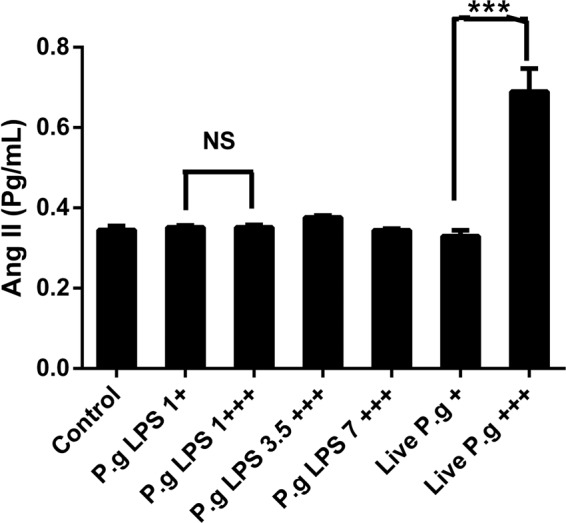
Angiotensin II levels are determined in the HCAEC cell culture supernatant stimulated to single (+) or repetitive (+++) exposures of P. gingivalis-LPS or live-P. gingivalis by the ELISA kit. The results are expressed as the means ± SEM (n=3) with a statistical significance represented as (*)p < 0.05 vs. control, (†)p < 0.05 compared vs cells treated by single exposure; (ns) for not significant.
Discussion
Oral pathogens associated with periodontitis, such as P. gingivalis, have been of particular interest due to the high levels of bacteraemia and endotoxemia after routine dental procedures and everyday oral activities, such as tooth brushing7. The biological mechanisms underlying the potential link between periodontitis and atherosclerosis or hypertension remain unclear, mainly in terms of inflammatory and vasoactive endothelial responses to P. gingivalis with repeated exposures. In this study, we evaluated the effects of single versus repeated administration of P. gingivalis-LPS and whole bacteria on the pro-inflammatory mediators and vasoactive markers involved in HCAEC atherosclerotic response.
In relation to cell viability, there are no reports in the literature that demonstrate the in vitro effect of periodontopathogens such as P. gingivalis on HCAEC cells at repeated exposures and at concentrations greater than 2 mg/mL with LPS33,34. Our results demonstrated that of P. gingivalis-LPS and the bacteria did not affect the cellular viability of HCAEC at the concentrations evaluated; data similar to those reported by Chou et al.35 where even 100 µg/mL of P. gingivalis-LPS W83 on leukocytes as PMN did not affect its viability36. However, depending on the type of cell line differences may occur, in this way have been described in esophageal cell lines as OE19 (adenocarcinoma), OE21 (squamous cell carcinoma), a sensitivity different from that reported in oral tumor cells (HN30), where the esophageal cancer cells were only sensitive to LPS P. gingivalis W83 concentrations of 20, 50 and 100 μg/mL (24,48 and 72 h), unlike oral cells (HN30) where the LPS increases the viability in relation to the control after 72 h of stimulus37.
P. gingivalis W83 strains have been known to adhere, invade and persist in bacteria-infected HCAEC33; however, its ability to activate endothelial cells by chemokine and cytokine production seems to exhibit slight activation to IL-8, IL-6, and MCP-1 compared to cells infected with other strains, such as 381 or 3327733. On the other hand, this study demonstrated inflammatory effect of W83 strain on endothelial cells, since HCAEC exposed to repeated exposure of live-P. gingivalis induced significant increases in chemokine levels, such as IL-8 and MCP-1, and in cytokines, such as IL-6, compared with the control group, while HCAEC cells challenged with a single exposure of P. gingivalis W83 showed similar production of IL-8, IL-6 and MCP-1, compared with uninfected cells.
Increases in IL-8 are involved in the firm adhesion of rolling monocytes in the early stages of atherogenesis38. Similarly, IL-6 and MCP-1 increases have been implicated in the adhesion of leukocytes (mainly monocytes) to activated endothelium, which contributes to cellular migration39. Experimental findings suggest differential efficacy of P. gingivalis to activate HCAEC cells. P. gingivalis 381 also enhanced IL-6, IL-8 and MCP-1 production and even the adhesion of immune cells with bacteria-infected HCAEC, while other P. gingivalis strains, such as W83, induced slight activation33,40,41.
P. gingivalis-LPS was a poor inducer of IL-6, MCP-1, GM-CSF and IL-8 from HCAECs supernatants, similar results has been shown in immune cells as dendritic cell (DCs)42. In contrast, several authors have shown that endotoxin of P. gingivalis strain 33277 induces an important pro-inflammatory effect, increasing the production of IL-8, soluble E-selectin and MCP-1 in HCAEC43, while 381 strains only exerted a weak stimulatory effect on HCAEC41. These results have been previously described and can be attributed to the presence of the K1 capsule or the characteristics of thechemotype of P. gingivalis-LPS W83 that may present differences in the O antigen region44–46, which leads to the structural variations of the LPS that can be related with attenuation of the immune system of the host. Therefore, the low inflammatory response in HCAEC cells challenged with LPS could not be generalized to all strains of P. gingivalis16,33.
It has been described that P. gingivalis-LPS is an inducer of tolerance in macrophages, mainly by the suppression of the endothelial recognition receptor (TLR-4)47,48; however, our results showed that LPS (7.0 µg/mL) induced an increase in the release of IL-8 at repeated exposures, which may be related to the type of endothelial recognition receptor to which P. gingivalis-LPS W83 binds (TLR-2) or other factors that may be involved by positively regulating the release of IL-849,50. However, new studies are required to elucidate the mechanism of action.
Regarding the relationship between mRNA and proteins levels, cytokines as MCP-1 and IL-8 which were significantly detected in supernatants of HCAEC exposed to live-P. gingivalis, while MCP-1 mRNA levels were not upregulated. These discrepancies between mRNA and protein levels may involve the degradation rate of mRNA, which falls within a much tighter range (2–7 h for mammalian mRNAs vs 48 h for proteins)51. In fact, a previous report in aortic smooth muscle cells has determined that in vitro half-life of MCP-1 mRNA is approximately 45 min52, however, further verification using transcriptome analysis or RT-qPCR are required.
On the other hand, Ang II has been implied in atherogenesis promoting the oxidative stress in the vasculature, endothelial dysfunction and induction of an inflammatory response in the vessel wall53. Regardless endothelial cells are not considered a dominant source of AngII and AGTR54; previous studies have shown that classic LPS from enterobacterias stimulate local and circulatory Ang II levels55–57. However, knowledge regarding the in vitro vasoactive effects of periodontopathogens as P. gingivalis-LPS on HCAECs, the cell type that has typically been used in studies of atherosclerotic diseases, is unclear yet. Contrariwise, our data showed P. gingivalis-LPS as a poor gene inducer to Ang II, AGTR1, AGTR2 and all chemokine/cytokine measured. It also suggests a weak vasoactive and inflammatory effect of endotoxin isolated from P. gingivalis W83.
Interestingly, repeated exposure of live bacteria P. gingivalis induces a greatest effect in HCAEC, suggesting that Ang II can modulate signaling cascades associated with the release of pro-inflammatory cytokines through calcium mobilization, arachidonic acid production, kinases activation (MAPKs, PKC, JAK, PI3K) or the activation of transcription factors as cAMP and NF-Kβ17,58–60, which may explain the possible effects presented by the stimulation with live-P. gingivalis on endothelial cells21,55. However, further research is required to clarify possible mechanism.
Regarding the association between Ang II and the release of proinflammatory molecules such as IL8, IL6 and MCP1, there is no evidence with periodontopathogens, while some evidence have been reported Escheriria coli-LPS (E. coli-LPS)48,58,59, suggesting a synergistic effect between live-P. gingivalis stimulus and Ang II.
In contrast to the high concentration of Ang II at repeated dose of live bacteria, we found a down regulation of AGTR1 and AGTR2 at the mRNA level. Similar results with human saphenous vein cells (VSMC) and rat aortic smooth muscle (HASMC) suggest that high concentrations of Ang II can induce in vitro gen downregulation or desensitization/internationalization of AGTR148,58,59 or AGTR257. However, additional studies are required to identify the role of these receptors in endothelial dysfunction at repeated dose of periodontopathogens.
This work represents an alternative to the traditional in-vitro approach to evaluate P. gingivalis effects on endothelial cells, since transient and frequent bacteremia or endotoxemia episodes have been clearly described in patients with periodontitis. However, the classic stimulation model performed at a single dose up to 24 h did not expose the endothelium to these immunological challenges. Therefore, in-vitro exposure to more than one (repeated) exposure of P. gingivalis on the endothelium could lead to a better understanding for the study of endothelial dysfunction and pro-inflammatory activation.
Materials and Methods
Bacterial culture and inoculum standardization
P. gingivalis (BAA-308/W83) strain was obtained from the American Type Culture Collection (ATCC) and cultured using standard methods. This strain was originally isolated from humans with oral infections (i.e., periodontitis) and has been shown to be highly virulent compared with other P. gingivalis strains60. Bacteria were grown in supplemented Brucella agar (0.3% Bacto agar, 0.2% yeast extract, 5% defibrinated sheep blood, 0.2% haemolyzed blood, 0.0005% hemin, and 0.00005% menadione) and incubated at 37 °C for 4 days in anaerobic conditions (Anaerogen, Oxoid, Hampshire, UK)61. Bacterial inoculums were prepared and standardized for P. gingivalis in RPMI-1640 (Thermo Scientific, Waltham, MA, USA) and were quantified by spectrophotometry (Thermo Scientific, Waltham, MA, USA) at specific optical densities (OD) of 0.900–0.908 at a wavelength of 620 nm, corresponding to 2,6 × 109 bacteria/mL. The count of colony forming units (CFU) was confirmed in triplicate under incubation conditions. Viable bacteria experiments were performed in a maximum time of two hours after having counted them, in order to avoid bacterial mortality.
LPS extraction and purification
LPS extraction was performed using hot phenol-water, as previously reported32, with 1.1 g of wetted P. gingivalis W83; the purification was accomplished using an enzymatic treatment with nucleases and protease, followed by size-exclusion chromatography (Sephacryl S-200 HR) with sodium deoxycholate as the mobile phase62. The characterization of the LPS was determined by SDS-PAGE electrophoresis, purpald assay and chromogenic LAL test, compared to the commercial LPS of P. gingivalis ATCC 33277 (InvivoGen)32.
Stimulation of HCAEC with LPS and viable bacteria in a single and repeated exposure model
HCAEC cells (LONZA, Walkersville USA) were cultured in supplemented EGM2 MV medium (LONZA, Walkersville, USA). The cells were used at passage 7 in growth medium (2 × 105 cells/well) using 12-well culture plates (CytoOne, USA Scientific, Orlando FL, USA) and pre-incubated at 37 °C in a water-saturated atmosphere of 95% air and 5% CO2 until reaching confluence at 20 h. Subsequently, the cells were exposed to two treatment models at different concentrations of purified LPS (1.0, 3.5 and 7.0 µg/mL) and serial dilutions of live bacteria (MOI 1:100 - 1:0,1). A pilot study was conducted using longer exposure times where HCAEC cells were stimulated with P. gingivalis LPS on days 1, day 3 and day 5; the supernatant is removed every 48 hours to reach a total of 7 days under repeated exposure. The supernatant was stored at −80 C, for subsequent cytokine analysis.
In the first model the cells were stimulated for 6 h, after that, the stimulus was removed between each stimulus and replaced with a next exposure for another 6 h and for the last stimulation HCAEC the cells were exposed to another 12 h, for a total exposure time from 24 h. The supernatant was collected and storage for soluble factors measuring.
For the second treatment model, the conventional stimulus was referenced by literature in which HCAECs were stimulated with LPS at 1 µg/mL and serial dilutions of live bacteria MOI (1:100 - 1:0,1) at a single exposure for 24 h43.
Cell viability assay
The cells were cultured in 96-well plates and stimulated according to the model described above with P. gingvalis-LPS (1.0, 3.5 and 7.0 µg/mL) and the live bacterium MOI 1:100. Subsequently to determine the cell viability was determined according to the fluorometric detection after the reduction of resazurin in the resorufin product using AlamarBlue (Biosource, Camarillo, CA, USA)63, the cells were placed in the medium containing 10% Alamar blue, after 10 h of incubation, 100 μL of the medium was transferred to the wells of a 96-well plate and the changes in the fluorescence with a microplate fluorometer equipped with an excitation filter set of 560 nm/590 nm emission (Infinite 200 PRO, Tecan, Männedorf, Switzerland). The unstimulated samples were considered our survival control, while those treated with 1% triton for 10 minutes were defined as positive control of death.
RNA extraction and RT-qPCR
The mRNA expression levels of AGTR1, AGTR2, IL-8, IL-1β, MCP-1 and GAPDH were obtained from HCAEC cell stimulated to single or repeated exposures with LPS or live bacteria by qPCR. Total RNA was obtained from HCAEC using the QuickPrep MicroPrep isolation kit (Zymo Research, Irvine, CA, USA). The total amount of RNA was quantified using a Nanodrop (Thermo Scientific, Waltham, MA, USA). RT-qPCR was performed using 40 ng of total RNA and a RT-qPCR Luna Universal One-Step kit (New England Biolabs, Ipswich, MA, USA). Primers were designed using Beacon Designer software and are listed in Table 1. The reaction mixture consisted of 4,1 µL of template [10 ng/µL], 5 µL of Luna Universal One-Step Reaction Mix [2x], 0,5 µL of Luna WarmStart RT Enzyme Mix [20x], and 0,2 µL of primers [10 µM], in a final reaction volume of 10 µL. The temperature profile used was as follows: 55 °C for 10 min, 1 cycle at 95 °C for 1 min, followed by 40 cycles of amplification at 95 °C for 10 s and 60 °C for 30 min. Expression levels were calculated from the qPCR results based on the modified 2−ΔΔCt method suggested by Pfaffl64. For these calculations, GAPDH and unstimulated cells were used as controls.
Table 1.
Primer sequences used for gene expression analysis by qPCR.
| Gene | Primer Forward | Primer Reverse |
|---|---|---|
| AGTR1 | 5′-TCAGCCAGCGTCAGTTTCAA-3′ | 5′-GCCAGCAGCCAAATGATGATG-3′ |
| AGTR2 | 5′-GACAGACCAAACATATAAGAAGGA-3′ | 5′-TCAGCTTGCTTAGTGCCTA-3′ |
| COX-2 | 5′-GATGATGTATGCCACAATCT-3′ | 5′-AGTCTCTCCTATCAGTATTAGC-3′ |
| IL-8 | 5′-TGTGAAGGTGCAGTTTTGCCAAGG-3′ | 5′-GTTGGCGCAGTGTGGTCCACTC-3′ |
| IL-1β | 5′-CTTTGAAGCTGATGGCCCTAAA-3′ | 5′-AGTGGTGGTCGGAGATTCGT-3′ |
| MCP-1 | 5′-GAAAGTCTCTGCCGCCCTT-3′ | 5′- TTGATTGCATCTGGCTGAGCG-3′ |
| GAPDH | 5′-GGTGGTCTCCTCTGACTTCAACA-3′ | 5′-GTTGCTGTAGCCAAATTCGTTGT-3′ |
Determination of chemokine and cytokine levels by flow cytometry
IL-6, MCP-1, IL-8, IL-1β, and GM-CSF levels were measured in culture supernatants from HCAEC stimulated with LPS or live bacteria by flow cytometry using a Human Proinflammatory Chemokine Panel (BioLegend, San Diego, CA, USA), according to the manufacturer’s instructions. The minimal detectable concentrations of IL-8, MCP-1, IL-6, IL-1β and GM-CSF were 1.9, 2.2, 3.6, 2.6 and 2.0 pg/mL, respectively. Flow cytometry was performed using the BD Accuri C6 flow cytometer (Becton Dickinson Biosciences, San Jose, CA, USA), and the data were processed using BD Accuri C6 Software.
Angiotensin II concentration
Ang II levels were determined from the supernatants of the cultured HCAEC stimulated with LPS or live bacteria, using the EIA ELISA Kit (Cayman Chemical, Ann Arbor, MI, USA). To detect Ang II in the supernatants, sample extraction and ELISA were performed according to the manufacturer’s instructions65.
Statistical analysis
All experiments were repeated at least 3 times for qPCR and flow cytometry. All data were expressed as the mean ± SEM. ELISA results were performed at least 3 times in duplicate. One-way variance analysis (ANOVA) and Tukey’s post hoc tests were performed for all analyses. A p-value < 0.05 was considered statistically significant.
Conclusions
Repeated exposure live-P. gingivalis induces a greater pro-inflammatory response than single exposure, described by IL-8, IL-6, MCP-1 and GM-CS in HCAEC. The expression of AGTR1 and production of Ang II induced by live-P. gingivalis W83 showed the vasomotor effect of whole bacteria in HCAEC more than LPS. The findings of this study suggest that repeated exposure of P. gingivalis in HCAEC induces the activation of proinflammatory and vasoconstrictor molecules that lead to endothelial dysfunction as a key mechanism of the onset and progression of arterial hypertension (HT) and atherosclerosis, which requires more research.
Supplementary information
Acknowledgements
This study was supported by the Administrative Department of Science, Technology, and Innovation COLCIENCIAS (Grant: No. 130865740864) and by Universidad El Bosque, Research vice-rectory, Bogota, Colombia. The authors thank Juliette de Avila (Immunology laboratory, UIBO, El Bosque University, Bogota) for his assistance with flow cytometry and Oral Microbiology Laboratory, UIBO for their assistance in the culture of bacterium P. gingivalis.
Author contributions
D.M.B. and G.I.L. designed the original idea of the project; D.M.C. standardized the obtaining of the bacterial extract and the methodology of extraction and purification the LPS of P. gingivalis. S.V.G. and S.J.M. performed the mRNA and cytokine expression assays and the analysis of the results, Y.CH.Q., performed the assays for the quantification of Ang II, D.M.B. performed the cytotoxicity assays, D.M.B. directed the execution of the project and with Y.CH.Q. and G.I.L. they were in charge of the analysis of the results. All authors participated in the writing-original draft. S.V.G., D.M.B. and G.I.L. drafted the final manuscript, which was critically reviewed by all the authors.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
is available for this paper at 10.1038/s41598-019-54259-y.
References
- 1.Dinh Quynh N., Drummond Grant R., Sobey Christopher G., Chrissobolis Sophocles. Roles of Inflammation, Oxidative Stress, and Vascular Dysfunction in Hypertension. BioMed Research International. 2014;2014:1–11. doi: 10.1155/2014/406960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geovanini Glaucylara Reis, Libby Peter. Atherosclerosis and inflammation: overview and updates. Clinical Science. 2018;132(12):1243–1252. doi: 10.1042/CS20180306. [DOI] [PubMed] [Google Scholar]
- 3.Forner Lone, Larsen Tove, Kilian Mogens, Holmstrup Palle. Incidence of bacteremia after chewing, tooth brushing and scaling in individuals with periodontal inflammation. Journal of Clinical Periodontology. 2006;33(6):401–407. doi: 10.1111/j.1600-051X.2006.00924.x. [DOI] [PubMed] [Google Scholar]
- 4.Horliana Anna Carolina Ratto Tempestini, Chambrone Leandro, Foz Adriana Moura, Artese Hilana Paula Carillo, Rabelo Mariana de Sousa, Pannuti Cláudio Mendes, Romito Giuseppe Alexandre. Dissemination of Periodontal Pathogens in the Bloodstream after Periodontal Procedures: A Systematic Review. PLoS ONE. 2014;9(5):e98271. doi: 10.1371/journal.pone.0098271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lafaurie Gloria Inés, Mayorga-Fayad Isabel, Torres María Fernanda, Castillo Diana Marcela, Aya Maria Rosario, Barón Alexandra, Hurtado Paola Andrea. Periodontopathic microorganisms in peripheric blood after scaling and root planing. Journal of Clinical Periodontology. 2007;34(10):873–879. doi: 10.1111/j.1600-051X.2007.01125.x. [DOI] [PubMed] [Google Scholar]
- 6.Kurihara N., Inoue Y., Iwai T., Umeda M., Huang Y., Ishikawa I. Detection and Localization of Periodontopathic Bacteria in Abdominal Aortic Aneurysms. European Journal of Vascular and Endovascular Surgery. 2004;28(5):553–558. doi: 10.1016/j.ejvs.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Figuero Elena, Sánchez-Beltrán María, Cuesta-Frechoso Susana, Tejerina Jose María, del Castro Jose Antonio, Gutiérrez Jose María, Herrera David, Sanz Mariano. Detection of Periodontal Bacteria in Atheromatous Plaque by Nested Polymerase Chain Reaction. Journal of Periodontology. 2011;82(10):1469–1477. doi: 10.1902/jop.2011.100719. [DOI] [PubMed] [Google Scholar]
- 8.Kozarov, E. V., Dorn, B. R., Shelburne, C. E., Dunn, W. A. & Progulske-Fox, A. Human Atherosclerotic Plaque Contains Viable Invasive Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis. Arterioscler. Thromb. Vasc. Biol., 10.1161/01.atv.0000155018.67835.1a (2005). [DOI] [PubMed]
- 9.Rafferty B., Jönsson D., Kalachikov S., Demmer R. T., Nowygrod R., Elkind M. S. V., Bush H., Kozarov E. Impact of monocytic cells on recovery of uncultivable bacteria from atherosclerotic lesions. Journal of Internal Medicine. 2011;270(3):273–280. doi: 10.1111/j.1365-2796.2011.02373.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pucar Ana, Milasin Jelena, Lekovic Vojislav, Vukadinovic Miroslav, Ristic Miljko, Putnik Svetozar, Kenney E. Barrie. Correlation Between Atherosclerosis and Periodontal Putative Pathogenic Bacterial Infections in Coronary and Internal Mammary Arteries. Journal of Periodontology. 2007;78(4):677–682. doi: 10.1902/jop.2007.060062. [DOI] [PubMed] [Google Scholar]
- 11.Gaetti-Jardim E., Marcelino S. L., Feitosa A. C. R., Romito G. A., Avila-Campos M. J. Quantitative detection of periodontopathic bacteria in atherosclerotic plaques from coronary arteries. Journal of Medical Microbiology. 2009;58(12):1568–1575. doi: 10.1099/jmm.0.013383-0. [DOI] [PubMed] [Google Scholar]
- 12.Mustapha Indra Z., Debrey Sarah, Oladubu Michael, Ugarte Richard. Markers of Systemic Bacterial Exposure in Periodontal Disease and Cardiovascular Disease Risk: A Systematic Review and Meta-Analysis. Journal of Periodontology. 2007;78(12):2289–2302. doi: 10.1902/jop.2007.070140. [DOI] [PubMed] [Google Scholar]
- 13.Türkoğlu Oya, Barış Nezihi, Tervahartiala Taina, Şenarslan Ömer, Sorsa Timo, Atilla Gül. Evaluation of Systemic Levels of Neutrophilic Enzymes in Patients With Hypertension and Chronic Periodontitis. Journal of Periodontology. 2014;85(7):908–916. doi: 10.1902/jop.2013.130346. [DOI] [PubMed] [Google Scholar]
- 14.Harrison David G., Guzik Tomasz J., Lob Heinrich E., Madhur Meena S., Marvar Paul J., Thabet Salim R., Vinh Antony, Weyand Cornelia M. Inflammation, Immunity, and Hypertension. Hypertension. 2011;57(2):132–140. doi: 10.1161/HYPERTENSIONAHA.110.163576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Szekanecz Zoltán, Koch Alisa E. Vascular endothelium and immune responses: implications for inflammation and angiogenesis. Rheumatic Disease Clinics of North America. 2004;30(1):97–114. doi: 10.1016/S0889-857X(03)00116-9. [DOI] [PubMed] [Google Scholar]
- 16.Al-Soudi A., Kaaij M.H., Tas S.W. Endothelial cells: From innocent bystanders to active participants in immune responses. Autoimmunity Reviews. 2017;16(9):951–962. doi: 10.1016/j.autrev.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 17.Andrukhov Oleh, Steiner Ilse, Liu Shutai, Bantleon Hans Peter, Moritz Andreas, Rausch-Fan Xiaohui. Different effects of Porphyromonas gingivalis lipopolysaccharide and TLR2 agonist Pam3CSK4 on the adhesion molecules expression in endothelial cells. Odontology. 2013;103(1):19–26. doi: 10.1007/s10266-013-0146-x. [DOI] [PubMed] [Google Scholar]
- 18.Assinger Alice, Buchberger Elisabeth, Laky Markus, Esfandeyari Azadeh, Brostjan Christine, Volf Ivo. Periodontopathogens induce soluble P-selectin release by endothelial cells and platelets. Thrombosis Research. 2011;127(1):e20–e26. doi: 10.1016/j.thromres.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 19.Wada Koichiro, Kamisaki Yoshinori. Roles of Oral Bacteria in Cardiovascular Diseases — From Molecular Mechanisms to Clinical Cases: Involvement of Porphyromonas gingivalis in the Development of Human Aortic Aneurysm. Journal of Pharmacological Sciences. 2010;113(2):115–119. doi: 10.1254/jphs.09R22FM. [DOI] [PubMed] [Google Scholar]
- 20.Nakano K, Wada K, Nomura R, Nemoto H, Inaba H, Kojima A, Naka S, Hokamura K, Mukai T, Nakajima A, Umemura K, Kamisaki Y, Yoshioka H, Taniguchi K, Amano A, Ooshima T. Characterization of aortic aneurysms in cardiovascular disease patients harboring Porphyromonas gingivalis. Oral Diseases. 2010;17(4):370–378. doi: 10.1111/j.1601-0825.2010.01759.x. [DOI] [PubMed] [Google Scholar]
- 21.Santos C.F., Akashi A.E., Dionísio T.J., Sipert C.R., Didier D.N., Greene A.S., Oliveira S.H.P., Pereira H.J.V., Becari C., Oliveira E.B., Salgado M.C.O. Characterization of a Local Renin-Angiotensin System in Rat Gingival Tissue. Journal of Periodontology. 2009;80(1):130–139. doi: 10.1902/jop.2009.080264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Santos Carlos F., Morandini Ana C., Dionísio Thiago J., Faria Flávio A., Lima Marta C., Figueiredo Caio M., Colombini-Ishikiriama Bella L., Sipert Carla R., Maciel Rubens P., Akashi Ana P., Souza Gabriela P., Garlet Gustavo P., Rodini Camila O., Amaral Sandra L., Becari Christiane, Salgado Maria C., Oliveira Eduardo B., Matus Isaac, Didier Daniela N., Greene Andrew S. Functional Local Renin-Angiotensin System in Human and Rat Periodontal Tissue. PLOS ONE. 2015;10(8):e0134601. doi: 10.1371/journal.pone.0134601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin-Cabezas Rodrigo, Seelam Narendra, Petit Catherine, Agossa Kévimy, Gaertner Sébastien, Tenenbaum Henri, Davideau Jean-Luc, Huck Olivier. Association between periodontitis and arterial hypertension: A systematic review and meta-analysis. American Heart Journal. 2016;180:98–112. doi: 10.1016/j.ahj.2016.07.018. [DOI] [PubMed] [Google Scholar]
- 24.Gürkan Ali, Emingil Gülnur, Saygan Buket Han, Atilla Gül, Köse Timur, Baylas Haluk, Berdeli Afig. Renin-angiotensin gene polymorphisms in relation to severe chronic periodontitis. Journal of Clinical Periodontology. 2009;36(3):204–211. doi: 10.1111/j.1600-051X.2008.01379.x. [DOI] [PubMed] [Google Scholar]
- 25.Paizan Mara, Vilela-Martin Jose. Is There an Association between Periodontitis and Hypertension? Current Cardiology Reviews. 2014;10(4):355–361. doi: 10.2174/1573403X10666140416094901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Geerts Sabine O., Nys Monique, Mol Patrick De, Charpentier Joseph, Albert Adelin, Legrand Victor, Rompen Eric H. Systemic Release of Endotoxins Induced by Gentle Mastication: Association With Periodontitis Severity. Journal of Periodontology. 2002;73(1):73–78. doi: 10.1902/jop.2002.73.1.73. [DOI] [PubMed] [Google Scholar]
- 27.Tomás Inmaculada, Diz Pedro, Tobías Aurelio, Scully Crispian, Donos Nikolaos. Periodontal health status and bacteraemia from daily oral activities: systematic review/meta-analysis. Journal of Clinical Periodontology. 2011;39(3):213–228. doi: 10.1111/j.1600-051X.2011.01784.x. [DOI] [PubMed] [Google Scholar]
- 28.D'Aiuto F., Nibali L., Mohamed-Ali V., Vallance P., Tonetti M. S. Periodontal therapy: a novel non-drug-induced experimental model to study human inflammation. Journal of Periodontal Research. 2004;39(5):294–299. doi: 10.1111/j.1600-0765.2004.00741.x. [DOI] [PubMed] [Google Scholar]
- 29.Tonetti Maurizio S., D'Aiuto Francesco, Nibali Luigi, Donald Ann, Storry Clare, Parkar Mohamed, Suvan Jean, Hingorani Aroon D., Vallance Patrick, Deanfield John. Treatment of Periodontitis and Endothelial Function. New England Journal of Medicine. 2007;356(9):911–920. doi: 10.1056/NEJMoa063186. [DOI] [PubMed] [Google Scholar]
- 30.Bainbridge Brian W., Darveau Richard P. Porphyromonas gingivalislipopolysaccharide: an unusual pattern recognition receptor ligand for the innate host defense system. Acta Odontologica Scandinavica. 2001;59(3):131–138. doi: 10.1080/000163501750266710. [DOI] [PubMed] [Google Scholar]
- 31.Hajishengallis George, Tapping Richard I., Harokopakis Evlambia, Nishiyama So-ichiro, Ratti Pukar, Schifferle Robert E., Lyle Elizabeth A., Triantafilou Martha, Triantafilou Kathy, Yoshimura Fuminobu. Differential interactions of fimbriae and lipopolysaccharide from Porphyromonas gingivalis with the Toll-like receptor 2-centred pattern recognition apparatus. Cellular Microbiology. 2006;8(10):1557–1570. doi: 10.1111/j.1462-5822.2006.00730.x. [DOI] [PubMed] [Google Scholar]
- 32.Gualtero Escobar Diego Fernando, Porras Gaviria Jeimy Paola, Bernau Gutierrez Sebastian, Buitrago Ramírez Diana Marcela, Castillo Perdomo Diana Marcela, Lafaurie Villamil Gloria Ines. Purificación y caracterización de lipopolisacáridos de Eikenella corrodens 23834 y Porphyromonas gingivalis W83. Revista Colombiana de Biotecnología. 2014;16(1):34. doi: 10.15446/rev.colomb.biote.v16n1.44224. [DOI] [Google Scholar]
- 33.Rodrigues Paulo H., Reyes Leticia, Chadda Amandeep S., Bélanger Myriam, Wallet Shannon M., Akin Debra, Dunn William, Progulske-Fox Ann. Porphyromonas gingivalis Strain Specific Interactions with Human Coronary Artery Endothelial Cells: A Comparative Study. PLoS ONE. 2012;7(12):e52606. doi: 10.1371/journal.pone.0052606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Deng, H. et al. Invasion of four common periodontal pathogens into vascular endothelial cells in vitro. Zhonghua Kou Qiang Yi Xue Za Zhi (2010). [PubMed]
- 35.Chou H.-H., Yumoto H., Davey M., Takahashi Y., Miyamoto T., Gibson F. C., Genco C. A. Porphyromonas gingivalis Fimbria-Dependent Activation of Inflammatory Genes in Human Aortic Endothelial Cells. Infection and Immunity. 2005;73(9):5367–5378. doi: 10.1128/IAI.73.9.5367-5378.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jones Katy J., Ekhlassi Sanaz, Montufar-Solis Dina, Klein John R., Schaefer Jeremy S. Differential Cytokine Patterns in Mouse Macrophages and Gingival Fibroblasts After Stimulation WithPorphyromonas gingivalisorEscherichia coliLipopolysaccharide. Journal of Periodontology. 2010;81(12):1850–1857. doi: 10.1902/jop.2010.100226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gonçalves, M. et al. Effect of LPS on the viability and proliferation of human oral and esophageal cancer cell lines. Brazilian Arch. Biol. Technol., 10.1590/1678-4324-2016150485 (2016).
- 38.Zernecke Alma, Shagdarsuren Erdenechimeg, Weber Christian. Chemokines in Atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology. 2008;28(11):1897–1908. doi: 10.1161/ATVBAHA.107.161174. [DOI] [PubMed] [Google Scholar]
- 39.Zohlnhöfer Dietlind, Brand Korbinian, Schipek Katharina, Pogatsa-Murray Gisela, Schömig Albert, Neumann Franz-Josef. Adhesion of Monocyte Very Late Antigen-4 to Endothelial Vascular Cell Adhesion Molecule-1 Induces Interleukin-1β–Dependent Expression of Interleukin-6 in Endothelial Cells. Arteriosclerosis, Thrombosis, and Vascular Biology. 2000;20(2):353–359. doi: 10.1161/01.ATV.20.2.353. [DOI] [PubMed] [Google Scholar]
- 40.Honda T., Oda T., Yoshie H., Yamazaki K. Effects of Porphyromonas gingivalis antigens and proinflammatory cytokines on human coronary artery endothelial cells. Oral Microbiology and Immunology. 2005;20(2):82–88. doi: 10.1111/j.1399-302X.2004.00193.x. [DOI] [PubMed] [Google Scholar]
- 41.Roth Georg A., Moser Bernhard, Roth-Walter Franziska, Giacona Mary Beth, Harja Evis, Papapanou Panos N., Schmidt Ann Marie, Lalla Evanthia. Infection with a periodontal pathogen increases mononuclear cell adhesion to human aortic endothelial cells. Atherosclerosis. 2007;190(2):271–281. doi: 10.1016/j.atherosclerosis.2006.03.018. [DOI] [PubMed] [Google Scholar]
- 42.Pulendran, B. et al. Lipopolysaccharides from distinct pathogens induce different classes of immune responses in vivo. J. Immunol. (2001). [DOI] [PMC free article] [PubMed]
- 43.Nakamura Naokazu, Yoshida Masayuki, Umeda Makoto, Huang Yi, Kitajima Shigetaka, Inoue Yoshinori, Ishikawa Isao, Iwai Takehisa. Extended exposure of lipopolysaccharide fraction from Porphyromonas gingivalis facilitates mononuclear cell adhesion to vascular endothelium via Toll-like receptor-2 dependent mechanism. Atherosclerosis. 2008;196(1):59–67. doi: 10.1016/j.atherosclerosis.2007.01.039. [DOI] [PubMed] [Google Scholar]
- 44.Brunner Jorg, Scheres Nina, El Idrissi Nawal B, Deng Dong M, Laine Marja L, van Winkelhoff Arie J, Crielaard Wim. The capsule of Porphyromonas gingivalis reduces the immune response of human gingival fibroblasts. BMC Microbiology. 2010;10(1):5. doi: 10.1186/1471-2180-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rangarajan M., Aduse-Opoku J., Paramonov N., Hashim A., Bostanci N., Fraser O. P., Tarelli E., Curtis M. A. Identification of a Second Lipopolysaccharide in Porphyromonas gingivalis W50. Journal of Bacteriology. 2008;190(8):2920–2932. doi: 10.1128/JB.01868-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.How, K. Y., Song, K. P. & Chan, K. G. Porphyromonas gingivalis: An overview of periodontopathic pathogen below the gum line. Frontiers in Microbiology, 10.3389/fmicb.2016.00053 (2016). [DOI] [PMC free article] [PubMed]
- 47.Verstrepen L, et al. TLR-4, IL-1R and TNF-R signaling to NF-κB: Variations on a common theme. Cellular and Molecular Life Sciences. 2008 doi: 10.1007/s00018-008-8064-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Outzen Emilie M., Zaki Marina, Mehryar Rahila, Abdolalizadeh Bahareh, Sajid Waseem, Boonen Harrie C. M., Sams Anette, Sheykhzade Majid. Lipopolysaccharides, but not Angiotensin ll, lnduces Direct Pro-lnflammatory Effects in Cultured Mouse Arteries and Human Endothelial and Vascular Smooth Muscle Cells. Basic & Clinical Pharmacology & Toxicology. 2017;120(4):335–347. doi: 10.1111/bcpt.12697. [DOI] [PubMed] [Google Scholar]
- 49.Zhang Tao, Kurita-Ochiai Tomoko, Hashizume Tomomi, Du Yuan, Oguchi Sumito, Yamamoto Masafumi. Aggregatibacter actinomycetemcomitansaccelerates atherosclerosis with an increase in atherogenic factors in spontaneously hyperlipidemic mice. FEMS Immunology & Medical Microbiology. 2010;59(2):143–151. doi: 10.1111/j.1574-695X.2010.00674.x. [DOI] [PubMed] [Google Scholar]
- 50.Kurita-Ochiai Tomoko, Yamamoto Masafumi. Periodontal Pathogens and Atherosclerosis: Implications of Inflammation and Oxidative Modification of LDL. BioMed Research International. 2014;2014:1–7. doi: 10.1155/2014/595981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vogel Christine, Marcotte Edward M. Insights into the regulation of protein abundance from proteomic and transcriptomic analyses. Nature Reviews Genetics. 2012;13(4):227–232. doi: 10.1038/nrg3185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu Bin, Poon Michael, Taubman Mark B. PDGF-BB enhances monocyte chemoattractant protein-1 mRNA stability in smooth muscle cells by downregulating ribonuclease activity. Journal of Molecular and Cellular Cardiology. 2006;41(1):160–169. doi: 10.1016/j.yjmcc.2006.03.426. [DOI] [PubMed] [Google Scholar]
- 53.Schmidt-Ott Kai M, Kagiyama Shuntaro, Phillips M.Ian. The multiple actions of angiotensin II in atherosclerosis. Regulatory Peptides. 2000;93(1-3):65–77. doi: 10.1016/S0167-0115(00)00178-6. [DOI] [PubMed] [Google Scholar]
- 54.Matsusaka Taiji, Niimura Fumio, Shimizu Akihiro, Pastan Ira, Saito Akihiko, Kobori Hiroyuki, Nishiyama Akira, Ichikawa Iekuni. Liver Angiotensinogen Is the Primary Source of Renal Angiotensin II. Journal of the American Society of Nephrology. 2012;23(7):1181–1189. doi: 10.1681/ASN.2011121159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ruiz-Ortega Marta, Ruperez Monica, Esteban Vanesa, Egido Jesús. Molecular mechanisms of angiotensin II-induced vascular injury. Current Hypertension Reports. 2003;5(1):73–79. doi: 10.1007/s11906-003-0014-0. [DOI] [PubMed] [Google Scholar]
- 56.Sanchez-Lemus Enrique, Murakami Yuki, Larrayoz-Roldan Ignacio M., Moughamian Armen J., Pavel Jaroslav, Nishioku Tsuyoshi, Saavedra Juan M. Angiotensin II AT1Receptor Blockade Decreases Lipopolysaccharide-Induced Inflammation in the Rat Adrenal Gland. Endocrinology. 2008;149(10):5177–5188. doi: 10.1210/en.2008-0242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang Fei, Xia Zhao-Fan, Chen Xu-Lin, Jia Yi-Tao, Wang Yong-Jie, Ma Bing. Angiotensin II type-1 receptor antagonist attenuates LPS-induced acute lung injury. Cytokine. 2009;48(3):246–253. doi: 10.1016/j.cyto.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 58.Bkaily, G. et al. Angiotensin II AT 1 receptor internalization, translocation and de novo synthesis modulate cytosolic and nuclear calcium in human vascular smooth muscle cells. Can. J. Physiol. Pharmacol., 10.1139/y03-007 (2003). [DOI] [PubMed]
- 59.Kranzhöfer Roger, Schmidt Joachim, Pfeiffer Carolein A. H., Hagl Siegfried, Libby Peter, Kübler Wolfgang. Angiotensin Induces Inflammatory Activation of Human Vascular Smooth Muscle Cells. Arteriosclerosis, Thrombosis, and Vascular Biology. 1999;19(7):1623–1629. doi: 10.1161/01.ATV.19.7.1623. [DOI] [PubMed] [Google Scholar]
- 60.Nelson K. E., Fleischmann R. D., DeBoy R. T., Paulsen I. T., Fouts D. E., Eisen J. A., Daugherty S. C., Dodson R. J., Durkin A. S., Gwinn M., Haft D. H., Kolonay J. F., Nelson W. C., Mason T., Tallon L., Gray J., Granger D., Tettelin H., Dong H., Galvin J. L., Duncan M. J., Dewhirst F. E., Fraser C. M. Complete Genome Sequence of the Oral Pathogenic Bacterium Porphyromonas gingivalis Strain W83. Journal of Bacteriology. 2003;185(18):5591–5601. doi: 10.1128/JB.185.18.5591-5601.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Castillo Diana Marcela, Castillo Yormaris, Delgadillo Nathaly Andrea, Neuta Yineth, Jola Johana, Calderón Justo Leonardo, Lafaurie Gloria Inés. Viability and Effects on Bacterial Proteins by Oral Rinses with Hypochlorous Acid as Active Ingredient. Brazilian Dental Journal. 2015;26(5):519–524. doi: 10.1590/0103-6440201300388. [DOI] [PubMed] [Google Scholar]
- 62.Hirschfeld Matthew, Ma Ying, Weis John H., Vogel Stefanie N., Weis Janis J. Cutting Edge: Repurification of Lipopolysaccharide Eliminates Signaling Through Both Human and Murine Toll-Like Receptor 2. The Journal of Immunology. 2000;165(2):618–622. doi: 10.4049/jimmunol.165.2.618. [DOI] [PubMed] [Google Scholar]
- 63.Oroszlán Melinda, Herczenik Eszter, Rugonfalvi-Kiss Szabolcs, Roos Anja, Nauta Alma J, Daha Mohamed R, Gombos Imre, Karádi István, Romics László, Prohászka Zoltán, Füst George, Cervenak László. Proinflammatory changes in human umbilical cord vein endothelial cells can be induced neither by native nor by modified CRP. International Immunology. 2006;18(6):871–878. doi: 10.1093/intimm/dxl023. [DOI] [PubMed] [Google Scholar]
- 64.Pfaffl M. W. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Research. 2001;29(9):45e–45. doi: 10.1093/nar/29.9.e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Miceli I, et al. Stretch reduces nephrin expression via an angiotensin II-AT 1 -dependent mechanism in human podocytes: effect of rosiglitazone. Am. J. Physiol. Physiol. 2009 doi: 10.1152/ajprenal.90423.2008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.