Abstract
Placenta percreta causing uterine rupture is a rare complication of pregnancy. It is most commonly diagnosed after the second trimester and can lead to significant morbidity necessitating abdominal hysterectomy of a gravid or immediately postpartum uterus. We describe a patient who presented with abdominal pain at 13 weeks of gestation and was diagnosed with placenta percreta during laparoscopy for presumed appendicitis. Intraoperatively, placenta was seen perforating the uterine fundus and 1 l of hemoperitoneum was evacuated. However, the uterus was hemostatic and the patient was stable, so the procedure was terminated. The patient was then transferred to a tertiary care center, where she ultimately underwent an uncomplicated laparoscopic gravid hysterectomy. We conclude that placenta percreta can occur in the first trimester even in patients without traditional risk factors. In stable patients, it is appropriate to consider minimally invasive hysterectomy with utilization of specific techniques to minimize intraoperative blood loss.
Keywords: Uterine rupture, Placenta percreta, First trimester, Laparoscopic hysterectomy
Highlights
-
•
Uterine rupture due to placenta percreta can present in the first trimester.
-
•
Minimally invasive laparoscopic hysterectomy can provide definitive treatment with decreased surgical morbidity and shorter convalescence.
-
•
Blood loss and allogenic transfusion can be minimized with appropriate hemostatic techniques and surgical planning.
1. Introduction
Placenta accreta spectrum (PAS) is the pathological adherence of placenta to the myometrium, thought to be due to a defect in the endometrium–myometrium interface, ultimately enabling chorionic villi invasion and trophoblast infiltration into the myometrium. Varying degrees of myometrial invasion – accreta, increta, or percreta – can cause significant morbidity and even mortality from severe hemorrhage. Complete penetration of chorionic villi through the myometrium to serosa (placenta percreta) is the rarest form of PAS and can lead to attachment to neighboring organs, including bladder and bowel. The incidence of PAS has been increasing due to the greater use of cesarean delivery, one of the primary risk factors, and now is as high as 1 in 272 for women with a birth-related hospital discharge diagnosis [1]. Abnormal placentation is often diagnosed on antenatal ultrasound or incidentally discovered at the time of delivery. However, it can also present in the first trimester with uterine rupture and hemoperitoneum, with almost all cases necessitating gravid hysterectomy [[2], [3], [4], [5], [6]].
We report a case of uterine rupture due to placenta percreta at 13 weeks of gestation in the setting of an unscarred uterus. We also describe a novel approach to management, namely laparoscopic hysterectomy. The case shows the safety of minimally invasive surgery in the appropriately selected patient.
2. Case
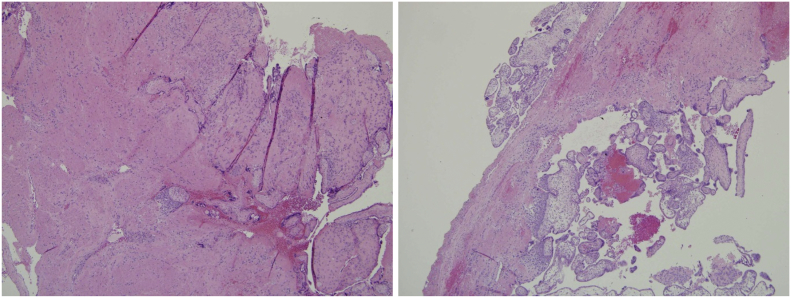
A 28-year-old woman, gravida 2 para 1, at 13 weeks of gestation presented to an emergency department with one week of pain in the right lower quadrant, nausea, and fever. She had had one prior uncomplicated term vaginal delivery but no abdominal or uterine surgery. On examination, she had normal vital signs and diffuse abdominal tenderness without peritoneal signs. Ultrasound revealed a single live intrauterine pregnancy of 13 2/7 weeks, free fluid in the right lower quadrant, and findings that suggested appendicitis. During laparoscopy in general surgery, 1 l of hemoperitoneum was evacuated, revealing a normal appendix and a fundal uterine mass resembling placenta. There was no active bleeding and the procedure was terminated. Postoperative hemoglobin was 5.7 g/dl, so she was transfused 3 units of packed red blood cells and remained hemodynamically stable. Post-operative MRI showed an anterior fundal placenta invading through the myometrium and beyond the serosa, consistent with placenta percreta (Fig. 1). Given concern about uterine rupture, the patient was transferred to a tertiary care center for further management.
Fig. 1.
Anterior placenta. At the fundus, the myometrium is not visualized and the placenta extends beyond the serosa. The bladder is unremarkable.
The patient arrived the next day, hemodynamically stable with repeat hemoglobin of 9.9 g/dl and non-acute abdominal exam. Management options were discussed with the patient and she indicated that she did not desire future fertility and desired gravid hysterectomy rather than a fertility-sparing procedure.
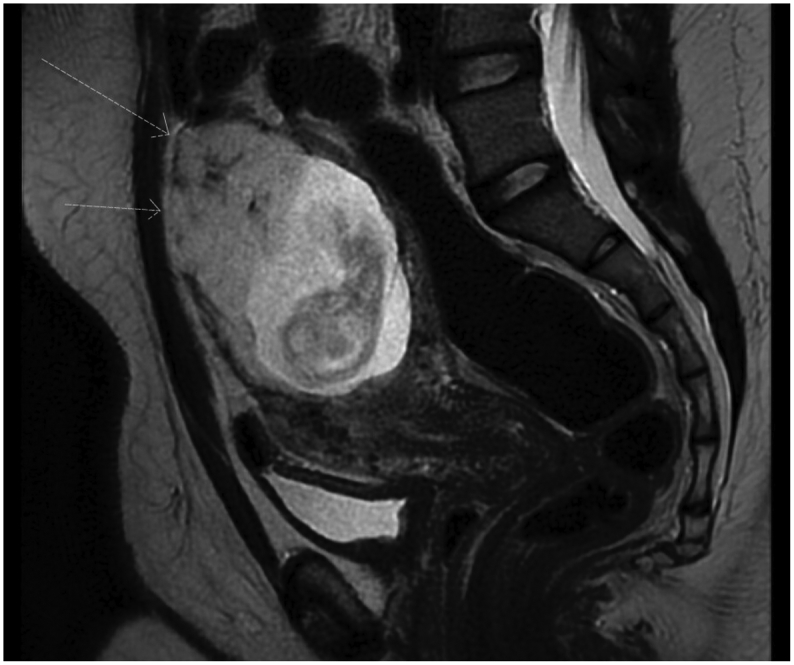
The patient underwent an uncomplicated total laparoscopic hysterectomy and bilateral salpingectomy via four 5 mm abdominal incisions with the minimally invasively gynecologic surgery team. Intraoperative findings included a uterus consistent with gestational age, placenta protruding through the uterine serosa at the fundus, significantly engorged vasculature, and 30 cc of hemoperitoneum with no active bleeding (Fig. 2). Bilateral ovaries and tubes, upper abdomen, and appendix were normal. The intact specimen was too large to be delivered through the vagina and the uterus was placed inside a bag introduced through the vagina. The opening of the bag was brought through the colpotomy and a flexible 12 mm suction cannula was used to remove the amniotic fluid while concurrently applying caudal traction on the specimen bag to decompress the uterus and allow passage through the colpotomy.
Fig. 2.
Intraoperative findings: Placenta protruding through the uterine serosa from the fundus. 30 cc hemoperitoneum.
We took several steps to reduce potential intraoperative hemorrhage. Tranexamic acid 1000 mg was given intravenously during anesthesia induction. Instead of a uterine manipulator, a colpotomy ring around the cervix with a sponge stick in the vagina were used to delineate the vaginal fornices for colpotomy and to manipulate the uterus without disrupting the placenta and risk causing intraoperative hemorrhage. Cell salvage was used to permit autologous blood transfusion. Because the wide gravid uterus increased the risk of occult thermal injury to the ureters, the ureters were identified retroperitoneally and lateralized. The retroperitoneal dissection was carried caudally to the level of the uterine arteries at their origin from the internal iliac artery to allow for uterine artery ligation. Total blood loss was 200 ml and no blood transfusion was required.
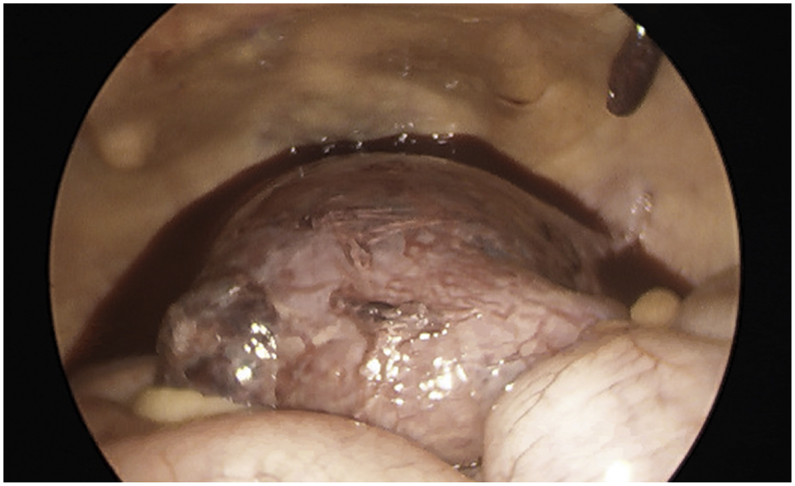
The patient had a routine postoperative course and was discharged on postoperative day 2. She had made a complete recovery by her six-week postoperative visit. Final pathology revealed a uterus distorted at the fundus where placenta was protruding through a 5 cm full-thickness anterior uterine wall defect, consistent with uterine rupture (Fig. 3). Histology revealed placenta with villous maturation consistent with gestational age, no chorioamnionitis, and recognizable myometrium invading through the serosa (Fig. 4), confirming the diagnosis of placenta percreta. Fetus length was consistent with 13 weeks of gestation.
Fig. 3.
Engorged uterus distorted at the fundus where placenta is protruding to the serosa. There is a 5 cm full-thickness defect on the uterine wall, consistent with uterine rupture.
Fig. 4.
A) Immature chorionic villi invading myometrium, consistent with placenta percreta. B) Area of uterine rupture at serosal surface with hemorrhage and fibrin.
3. Discussion and Conclusion
The patient experienced uterine rupture from placenta percreta at 13 weeks. We counseled her about the almost certain risk of further rupture as her pregnancy progressed, and she chose to undergo hysterectomy. She underwent an uncomplicated laparoscopic gravid hysterectomy in a non-emergency setting and specific techniques were utilized to minimize blood loss and morbidity.
Uterine rupture in the first trimester caused by placenta percreta is extremely rare, especially in an unscarred uterus [2]. Besides multiparity, this patient did not have any risk factors associated with abnormal placentation or uterine rupture. Intraperitoneal free fluid in the setting of a gravid uterus can be a common finding on ultrasound and without a high index of suspicion, diagnosis and appropriate management of a uterine rupture can be delayed.
A handful of case studies have described uterine rupture between 13 and 21 weeks [[2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12]]. Patients in these studies presented with severe abdominal pain, hemoperitoneum, and a history of prior cesarean delivery, uterine surgery, manual extraction of placenta, or dilation and curettage. Almost all cases necessitated hysterectomy via laparotomy for life-threatening hemorrhage [[2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12]]. Conservative treatments for placenta percreta remote from delivery have been described, including uterine curettage with packing, primary closure, methotrexate, and uterine vessel occlusion [14,15]. However, there is a four-fold increase in mortality with uterine-sparing treatment compared with hysterectomy [16], with unknown outcomes and potential risks for future pregnancies, and patients often require subsequent hysterectomy for uncontrolled hemorrhage, coagulopathy, or sepsis [18,19,[27], [28], [29], [30]]. Therefore, informed shared-decision making is critical and this patient was counseled on several occasions about management options, including fertility-sparing treatments given her young age and low parity. As she was clinically stable, she had time to fully evaluate the potential short- and long-term sequelae of her treatment decision.
Laparoscopic and robotic-assisted hysterectomy have been described for patients with PAS and interval hysterectomy after delivery of a viable fetus in the third trimester with the placenta left in-situ [16,20,21]. In a PubMed and Google Scholar search using keywords “placenta percreta,” “laparoscopic hysterectomy,” “first/s trimester,” we found no other reports of a minimally invasive gravid hysterectomy for uterine rupture. In the setting of a clinically stable patient, planned laparoscopic hysterectomy provided controlled, definitive treatment with decreased surgical morbidity and shorter convalescence.
Blood loss can be minimized with appropriate hemostatic techniques and surgical planning. We avoided misoprostol, which is routinely given to reduce bleeding during myomectomy [22], due to concerns about uterine contraction leading to uterine rupture or uncontrolled bleeding from the percreta site. Intrauterine vasopressin, routinely used during myomectomy [32], may be used in surgically managed PAS to reduce intraoperative bleeding. We did not use an intrauterine manipulator due to concerns about disrupting the placenta prior to securing the uterine vascular supply, but several other options exist to provide cephalad deviation and delineation of the cervix. Cell salvage was used to decrease risk of allogenic transfusion. Additionally, the surgeon should feel comfortable with retroperitoneal dissection given the potential need for ligation of the uterine blood supply at its origin and to reduce the odds of urinary tract injury due to the wide gravid uterus. The use of temporary internal iliac balloons is controversial; while they might decrease potential blood loss [[23], [24], [25]], serious complications like endothelial damage, thrombosis, inadvertent vessel occlusion, infection, and delay to definitive treatment can occur and routine use is not recommended [12,26].
We also present a novel, minimally invasive approach to hysterectomy with fetus in situ by using a transvaginal suction cannula to decompress the uterus for vaginal extraction. We used a specimen-containment bag which allows for effective caudal traction, prevents tissue dissemination or loss, and permits concurrent laparoscopic guidance to provide counter-traction from above and to observe for perforation during uterine decompression.
In summary, we describe a rare presentation of placenta percreta leading to uterine rupture in the first trimester and demonstrate management with minimally invasive hysterectomy utilizing specific techniques to minimize intraoperative blood loss. Laparoscopic hysterectomy can be successfully performed by experienced surgeons comfortable with advanced laparoscopic and hemostatic techniques and should be considered in the appropriate patient.
Acknowledgments
Contributors
All authors provided medical care for this patient. All authors were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Funding
No funding from an external source supported the publication of this case report.
Patient Consent
Obtained.
Provenance and Peer Review
This case report was peer reviewed.
Acknowledgements
The authors wish to thank the patient of this case report.
References
- 1.Mogos M.F., Salemi J.L., Ashley M., Whiteman V.E., Salihu H.M. Recent trends in placenta accreta in the United States and its impact on maternal–fetal morbidity and healthcare-associated costs, 1998–2011. J. Matern. Fetal Neonatal Med. 2016 Apr 2;29(7):1077–1082. doi: 10.3109/14767058.2015.1034103. [DOI] [PubMed] [Google Scholar]
- 2.Jang D.G., Lee G.S., Yoon J.H., Lee S.J. Placenta percreta-induced uterine rupture diagnosed by laparoscopy in the first trimester. Int. J. Med. Sci. 2011;8(5):424. doi: 10.7150/ijms.8.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Esmans A., Gerris J., Corthout E., Verdonk P., Declercq S. Placenta percreta causing rupture of an unscarred uterus at the end of the first trimester of pregnancy: case report. Hum. Reprod. 2004 Oct 1;19(10):2401–2403. doi: 10.1093/humrep/deh421. [DOI] [PubMed] [Google Scholar]
- 4.Ambrogi G., Ambrogi G., Marchi A.A. Placenta Percreta and uterine rupture in the first trimester of pregnancy. Case Rep. Obstet. Gynecol. 2018;2018 doi: 10.1155/2018/6842892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pont M., Kouadio E., Fernandez M.P., Bottaro M., Augros M., Bechet I., Mathevet P., De J.C., Soler S., Lantheaume S. Placenta percreta at first trimester of pregnancy. Diagnostic and decision-making difficulties: about a case and a review of the literature. J. Gynecol. Obstet. Biol. Reprod. (Paris) 2010 Oct;39(6):498–502. doi: 10.1016/j.jgyn.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 6.Park Y.J., Ryu K.Y., Lee J.I., Park M.I. Spontaneous uterine rupture in the first trimester: a case report. J. Korean Med. Sci. 2005 Dec 1;20(6):1079–1081. doi: 10.3346/jkms.2005.20.6.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.LeMaire W.J., Louisy C., Dalessandri K., Muschenheim F. Placenta percreta with spontaneous rupture of an unscarred uterus in the second trimester. Obstet. Gynecol. 2001 Nov 1;98(5):927–929. doi: 10.1016/s0029-7844(01)01580-0. [DOI] [PubMed] [Google Scholar]
- 8.Fleisch M.C., Lux J., Schoppe M., Grieshaber K., Hampl M. Placenta percreta leading to spontaneous complete uterine rupture in the second trimester. Gynecol. Obstet. Investig. 2008;65(2):81–83. doi: 10.1159/000108288. [DOI] [PubMed] [Google Scholar]
- 9.Topuz S. Spontaneous uterine rupture at an unusual site due to placenta percreta in a 21-week twin pregnancy with previous cesarean section. Clin. Exp. Obstet. Gynecol. 2004;31(3):239–241. [PubMed] [Google Scholar]
- 10.Bernal-Martínez S., Chávez H., Villa F., Guzmán A. Uterine rupture and placenta percreta in the second trimester. Presentation of a case. Ginecol. Obstet. Mexico. 1996 Oct;64:482–483. [PubMed] [Google Scholar]
- 11.Pizzuto K., Ozmiok C., Bozanovic R., Tafler K., Scattolon S., Leyland N.A., Morais M. Hysterectomy with Fetus in situ for uterine rupture at 21-week gestation due to a morbidly adherent placenta. Case Rep. Obstet. Gynecol. 2018;2018 doi: 10.1155/2018/5430591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hornemann A., Bohlmann M.K., Diedrich K., Kavallaris A., Kehl S., Kelling K., Hoellen F. Spontaneous uterine rupture at the 21st week of gestation caused by placenta percreta. Arch. Gynecol. Obstet. 2011 Oct 1;284(4):875–878. doi: 10.1007/s00404-011-1927-5. [DOI] [PubMed] [Google Scholar]
- 14.Legro R.S., Price F.V., Hill L.M., Caritis S.N. Nonsurgical management of placenta percreta: a case report. Obstet. Gynecol. 1994 May;83(5 Pt 2):847–849. [PubMed] [Google Scholar]
- 15.Wang L.M., Wang P.H., Chen C.L., Au H.K., Yen Y.K., Liu W.M. Uterine preservation in a woman with spontaneous uterine rupture secondary to placenta percreta on the posterior wall: a case report. J. Obstet. Gynaecol. Res. 2009 Apr;35(2):379–384. doi: 10.1111/j.1447-0756.2008.00936.x. [DOI] [PubMed] [Google Scholar]
- 16.Lee P.S., Kempner S., Miller M., Dominguez J., Grotegut C., Ehrisman J., Previs R., Havrilesky L.J., Broadwater G., Ellestad S.C., Secord A.A. Multidisciplinary approach to manage antenatally suspected placenta percreta: updated algorithm and patient outcomes. Gynecol. Oncol. Res. Pract. 2017 Dec;4(1) doi: 10.1186/s40661-017-0049-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gupta N., Gupta A., Green M., Kang H.S., Blankstein J. Placenta percreta at 17 weeks with consecutive hysterectomy: a case report and review of the literature. Case Rep. Obstet. Gynecol. 2012;2012 doi: 10.1155/2012/734834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Komiya K., Saitou K., Inoue S., Igarashi T., Hirabayashi Y., Seo N. Massive hemorrhage associated with undiagnosed placenta percreta in a second-trimester pregnancy receiving abortion procedure. Masui. Jpn. J. Anesthesiol. 2009 Aug;58(8):1036–1038. [PubMed] [Google Scholar]
- 20.Allen L., Jauniaux E., Hobson S., Papillon-Smith J., Belfort M.A. FIGO placenta Accreta diagnosis and management expert consensus panel, Duncombe G, Klaritsch P, Chantraine F, Kingdom J, Grønbeck L. FIGO consensus guidelines on placenta accreta spectrum disorders: nonconservative surgical management. Int. J. Gynecol. Obstet. 2018 Mar;140(3):281–290. doi: 10.1002/ijgo.12409. [DOI] [PubMed] [Google Scholar]
- 21.Garibaldi S., Perutelli A., Baldacci C., Gargini A., Basile S., Salerno M.G. Laparoscopic approach for peripartum hysterectomy. J. Minim. Invasive Gynecol. 2013 Jan 1;20(1):112–114. doi: 10.1016/j.jmig.2012.08.779. [DOI] [PubMed] [Google Scholar]
- 22.Frederick S., Frederick J., Fletcher H., Reid M., Hardie M., Gardner W. A trial comparing the use of rectal misoprostol plus perivascular vasopressin with perivascular vasopressin alone to decrease myometrial bleeding at the time of abdominal myomectomy. Fertil. Steril. 2013 Oct 1;100(4):1044–1049. doi: 10.1016/j.fertnstert.2013.06.022. [DOI] [PubMed] [Google Scholar]
- 23.Shih J.C., Liu K.L., Shyu M.K. Temporary balloon occlusion of the common iliac artery: new approach to bleeding control during cesarean hysterectomy for placenta percreta. Am. J. Obstet. Gynecol. 2005 Nov 1;193(5):1756–1758. doi: 10.1016/j.ajog.2005.08.033. [DOI] [PubMed] [Google Scholar]
- 24.Ballas J., Hull A.D., Saenz C., Warshak C.R., Roberts A.C., Resnik R.R., Moore T.R., Ramos G.A. Preoperative intravascular balloon catheters and surgical outcomes in pregnancies complicated by placenta accreta: a management paradox. Am. J. Obstet. Gynecol. 2012 Sep 1;207(3):216–e1. doi: 10.1016/j.ajog.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 25.Cali G., Forlani F., Giambanco L., Amico M.L., Vallone M., Puccio G., Luigi A. Prophylactic use of intravascular balloon catheters in women with placenta accreta, increta and percreta. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014 Aug 1;179:36–41. doi: 10.1016/j.ejogrb.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 26.Shamshirsaz A.A., Fox K.A., Salmanian B., Diaz-Arrastia C.R., Lee W., Baker B.W., Ballas J., Chen Q., Van Veen T.R., Javadian P., Sangi-Haghpeykar H. Maternal morbidity in patients with morbidly adherent placenta treated with and without a standardized multidisciplinary approach. Am. J. Obstet. Gynecol. 2015 Feb 1;212(2):218–e1. doi: 10.1016/j.ajog.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 27.Rashbaum W.K., Gates E.J., Jones J., Goldman B., Morris A., Lyman W.D. Placenta accreta encountered during dilation and evacuation in the second trimester. Obstet. Gynecol. 1995 May 1;85(5):701–703. doi: 10.1016/0029-7844(95)00050-2. [DOI] [PubMed] [Google Scholar]
- 28.Papadakis J.C., Christodoulou N. Placenta percreta presenting in the first trimester: review of the literature. Clin. Exp. Obstet. Gynecol. 2008;35(2):98–102. [PubMed] [Google Scholar]
- 29.Bansal C.L., Gupta J., Asthana D., Kayal A. Placenta Percreta in first trimester leading to disseminated intravascular coagulopathy (DIC): a rare case report. J. Clin. Diagn. Res. 2015 Apr;9(4):QD03. doi: 10.7860/JCDR/2015/9338.5794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Steinauer J.E., Diedrich J.T., Wilson M.W., Darney P.D., Vargas J.E., Drey E.A. Uterine artery embolization in postabortion hemorrhage. Obstet. Gynecol. 2008 Apr 1;111(4):881–889. doi: 10.1097/AOG.0b013e3181685780. [DOI] [PubMed] [Google Scholar]
- 32.Cohen S.L., Senapati S., Gargiulo A.R., Srouji S.S., Tu F.F., Solnik J., Hur H.C., Vitonis A., Jonsdottir G.M., Wang K.C., Einarsson J.I. Dilute versus concentrated vasopressin administration during laparoscopic myomectomy: a randomised controlled trial. BJOG Int. J. Obstet. Gynaecol. 2017 Jan 1;124(2):262–268. doi: 10.1111/1471-0528.14179. [DOI] [PubMed] [Google Scholar]