Abstract
Cognitive-behavioral self-management strategies are recommended for older adults with chronic pain. The goal of this study was to explore how pet ownership promotes use of these strategies in everyday life. We conducted four focus groups (n=25) with dog and cat owners aged ≥ 70 years with persistent pain. Participants described how their pets affect their daily routines and health, including pain and its management. We analyzed transcripts for salient themes, categorizing them according to their alignment with recommended pain self-management strategies: Mood Management (e.g., increases positive affect), Relaxation/Distraction (e.g., soothing presence), Physical Activity (e.g., dog-walking), Behavioral Activation (e.g., motivates activity even when pain present), Social Activation (e.g., facilitates socializing), and Sleep (e.g., encourages routine). Some participants described negative impacts of pet ownership. Having pets can facilitate behaviors and thoughts that may enhance coping with pain. Testing formal ways of leveraging pets’ role may expand non-pharmacological options for chronic pain management.
Keywords: Human-animal interaction, health behavior, qualitative methods
Background and Objectives
Chronic pain is a significant, yet modifiable factor affecting older adults’ quality of life and ability to remain independent in their daily lives. Cognitive and behavioral self-management strategies can help patients with chronic pain improve functioning while avoiding risks associated with opioids and other pharmacological treatments (AGS Panel on Persistent Pain in Older Persons, 2002; Guerriero & Reid, 2017). In practice, however, these strategies are vastly underutilized. Creative approaches are needed to increase the uptake of chronic pain self-management techniques in the everyday lives of older adults.
Leveraging the potential health benefits of companion animals or pets may be one such approach. For many older adults, pet ownership enhances quality of life, physical health, social interaction, and sense of purpose while reducing loneliness (Gee, Mueller, & Curl, 2017). According to socioemotional selectivity theory (Carstensen, 2006), social networks in older age are smaller but selected to optimize emotional needs. The uncomplicated and fulfilling relationships offered by companion animals may explain why many any older pet owners consider these animals an important part of their social networks (Needell & Mehta-Naik, 2016). Pet ownership is common among older adults in the United States: 51% of adults over age 50 report having pets, and approximately one-fifth of people 85 years and older own pets (Mueller, Gee, & Bures, 2018). More women over age 85 own pets than are married (Mueller et al., 2018). The role that pets play in the daily management of persistent pain, however, has received scant research attention.
The biopsychosocial model of chronic pain (Keefe, Caldwell, Tischner, & Aspnes, 2006) suggests mechanisms by which interactions with pets could improve pain-related outcomes. Having pets may reduce psychological distress and pain catastrophizing by promoting distraction, relaxation and pleasant activities (Reid, 2016); they may also facilitate physical and social activity (McNicholas et al., 2005). While at least one study has shown that spending waiting time with a therapy dog in an outpatient pain clinic can decrease pain (Marcus et al., 2012), research is lacking on how pets, who reside with and are cared for by older adults, can enhance chronic pain management over a longer period.
We identified only one prior study addressing the role of pets in chronic pain management. Using data from an online survey of 173 adults with chronic pain conditions, Bradley & Bennett (2015) found that most pet owners (116 of 132) used at least one strategy involving human-animal interaction (HAI) to cope with pain. However, study authors cautioned that pets’ impact on pain management varied with factors such as the pet’s temperament.
In sum, we currently have little information about how pets—a common but often overlooked resource for social support and coping—may play a role in promoting pain self-management among older adults. The overarching goal of this study was to use patient-identified mechanisms to inform a model of HAI for chronic pain self-management support among older adults. To this end, we conducted focus groups with older pet owners who have persistent pain. We gathered detailed descriptions from participants about how pet ownership affects their daily lives and management of health conditions including chronic pain. Once the naturally occurring relationship between HAI and chronic pain management is better understood, we can devise and test more formal ways for older adults to integrate their pets into a chronic pain self-management routine.
Research Design and Methods
This study was approved by the [blinded for review] and designated exempt from ongoing oversight [blinded for review]. All participants completed informed consent including agreement to audio-record the group discussion.
Eligibility criteria:
Participants were adults aged ≥ 70 years who reported pain, from any cause, on at least half of all days over the prior ≥ 6 months. In addition, participants reported at least “sometimes” experiencing restrictions due to pain in ≥ 1 of the following domains: work (around the home or volunteer work), social and recreational activities, and taking care of oneself (dressing, bathing). Participants had to reside full time with a dog and/or cat, and interact with their pet ≥ 4 times/day (defined as petting, talking to, playing with, walking with, sitting with, or feeding/grooming/cleaning up after). Study exclusions were limited to people with significant cognitive impairment (as indicated by a dementia diagnosis) that would interfere with participation in a group discussion.
Sample selection:
Nearly all participants were recruited through a large opt-in registry of adults interested in participating in health research [blinded for review]. Registry members could view information about the study, designate themselves “interested,” and respond to initial screening questions. The database also auto-suggested potentially eligible registrants, who were sent notifications through the website about this study. Those interested were contacted by a staff member for further screening and for scheduling into a focus group, if eligible and willing. Flyers were posted at several community sites; these yielded only two prospective participants, one of whom ended up in the study sample.
Measures:
All participants completed a brief, anonymous survey with items on demographics, chronic health conditions, pain intensity in the last week, and the number and type of their pets.
Focus group question content was informed by two theoretical frameworks: the biopsychosocial model of chronic pain, which posits that a complex interplay of biological, psychological, and social factors shape the chronic pain experience (Gatchel, Peng, Peters, Fuchs, & Turk, 2007) and a model proposing mechanisms linking HAI with health (McNicholas et al., 2005).
At the outset of each discussion, participants were invited to share information about their pet(s). Questions were then asked about how respondents believed their pets affected their health, including psychological functioning, pain, fatigue, and physical and social activity; and facilitators of, barriers to, and concerns about pet care. Discussions were guided by the protocol but were allowed to proceed organically, and moderators adapted question wording and topic order to maintain the feeling of a natural group discussion. (Focus group questions are available in Online Supplement 1.)
Focus groups and setting:
Four focus groups were conducted between November 2017 and May 2018 at an easily accessible building within a university health care system. Groups were moderated by the study’s Principal Investigator [blinded for review] with help from a trained research assistant [blinded for review]. The number of participants in each group ranged from 4 to 9 (total n= 25), and discussions lasted between 60 and 90 minutes. We did not hold a fifth focus group as data saturation (redundancy of information) was achieved by the fourth group (Krueger & Casey, 2000).
Data Analysis:
The lead researcher (moderator) and research assistant (co-moderator) met after each focus group to discuss and record salient themes. The lead researcher developed an a priori list of codes based on these discussions as well as question topics (Miles & Huberman, 1994). Relevant content was transcribed from digital recordings of focus groups. After reviewing all transcripts in detail, the lead researcher applied codes to all meaningful statements in the first transcript, modifying and adding codes to the original list as needed. A second research assistant [blinded for review] applied the modified codes to the second transcript and made further changes to the list of codes and the structure. After agreeing on the new coding scheme, the lead researcher and assistant applied the new list of codes to all four transcripts in an iterative process until consensus was reached.
After finalizing the organizational scheme, we reviewed all segments of coded text within each thematic category to verify the category’s conceptual coherence. In some instances, subthemes were moved or combined. In place of specialized software for qualitative analysis, we used standard word processing and spreadsheet apps. Several emergent themes were judged not pertinent to the present analysis (such as use of non-pet-related pain management therapies, and anecdotes about other people and their pets) and are not discussed here. The Consolidated Criteria for Reporting Qualitative Studies (COREQ) checklist guided reporting of analysis and results (Tong, Sainsbury, & Craig, 2007).
Results
Sample characteristics
A total of 25 adults participated in a focus group discussion. As Table 1 shows, most were female (68%; n=17) and between 70–75 years (76%; n=19). One participant identified as American Indian; the rest were White non-Hispanic. All but one participant had attained education beyond high school. About half (44%; n=11) of participants were currently married/partnered. Using a 1 (no pain) to 10 (worst imaginable pain) numerical rating scale, participants had an average pain level of 4.3 (SD=1.8) in the week prior to screening. Just under half of the sample (48%; n=12) met National Pain Strategy criteria (IPRCC, 2016) for high-impact chronic pain, i.e., “usually” having interference due to pain over the last six months in work, social/recreational activities, and/or self-care activities.
Table 1:
Demographic, health and pet-ownership characteristics of focus group participants (n=25)
| Variable | Percentage (n) or mean (standard deviation) |
|---|---|
| Demographics | |
| Age Group | |
| 70–75 years | 76% (19) |
| 76–80 years | 12% (3) |
| 81–85 years | 12% (3) |
| Female | 68% (17) |
| Race/ethnicity | |
| White non-Hispanic | 96% (24) |
| American Indian | 4% (1) |
| Education | |
| Some college or less | 28% (7) |
| Four-year degree | 24% (6) |
| Beyond four-year degree | 44% (11) |
| Married/long-term partner | 44% (11) |
| Retired | 72% (18) |
| Health | |
| Chronic health conditions (ever diagnosed)a |
|
| Arthritis | 72% (18) |
| High blood pressure | 60% (15) |
| Depression | 36% (9) |
| Average pain intensity in last week (1=no pain to 10=worst imaginable pain) |
4.3 (SD=1.8; observed range 2 – 7.5) |
| Meet criteria for high impact chronic painb | 48% (12) |
| Pet ownership characteristics | |
| Dog(s) | 60% (15) |
| Cat(s) | 40% (7) |
| Both cat(s) and dog(s) | 12% (3) |
Conditions endorsed by less than 30% of the sample: Heart disease (28%), cancer (20%), lung disease (12%), diabetes (8%), asthma (8%), stroke (0%).
Defined as “usually” or “always” having pain interference over the last six months in activities related to work (including housework or volunteering), social and recreational activities, or self-care.
Pets and chronic pain self-management
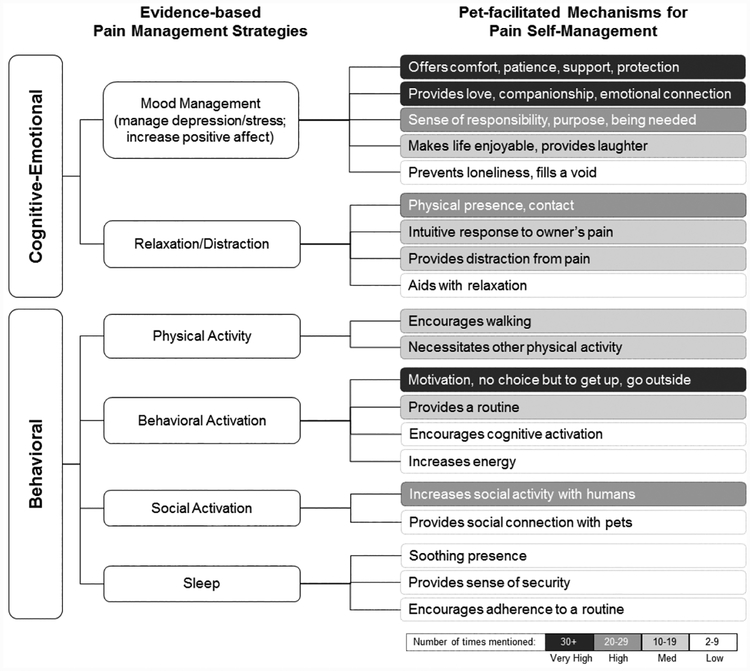
Figure 1 depicts evidence-based pain management and coping strategies (left column) along with associated pet-facilitated mechanisms as identified in focus groups (right column)—regardless of whether or not participants themselves linked these phenomena to pain or its management. A complete list of themes and associated codes is available (Online Supplement 2).
Figure 1:
Pet-facilitated Mechanisms for Chronic Pain Self-Management
Strategy 1: Mood Management
Pets were often described as sources of comfort, patience, support, and protection, especially during challenging times. One person talked about the supportive role her dog played during a period of bereavement:
And my partner died two years ago, and then his children sued me, so it was really a terrible, terrible time. I don’t think I would have gotten out of bed if it wasn’t for the dog. I would have just laid there and not moved because it was so horrible.
A second, adjacent theme is pets’ ability to provide love, companionship, and emotional connection. Whereas the previous theme evokes the role played by pets in lifting mood when it is needed, this second category has more to do with the ongoing positive emotions that pets engender in the pet-owner. These include a feeling that pets make life better, that owners feel close to their pets and sometimes regard them as family members, and—in a phrase used by several participants—that they couldn’t imagine life without them.
They’re such a large part of my life. … [T]hey fill space in my life. They are company, and they have unique personalities, and they’re friendly and affectionate in their own ways, and I love them dearly. I think they add a really big positive aspect to my whole life. (Cat owner)
The third mood management theme is the positive effect of having a sense of responsibility, purpose, and being needed by another living creature:
I think just knowing you’re coming home to something and being greeted and needed is part of it too. Makes you feel alive. (Dog owner)
Respondents said their pets evoked positive affect, in the form of enjoyment and laughter:
They say laughter is a great thing for helping anybody, no matter what’s wrong with them. I can’t look at that dog without smiling and feeling better.
Lastly, a few comments suggested that pets prevent loneliness and fill a void:
To come home to an empty house would be really hard, but there’s a sense of it—even when you don’t even see the animal—you walk in that door and you sense that there’s another living being in that house. (Cat owner)
Strategy 2: Relaxation and Distraction from Pain
Across focus groups, participants talked about how pets’ physical presence or contact was therapeutic for pain.
In our culture [Native American] they say put your animal on your lap and get them to make a noise. The purring animal has a vibration that will help with your pain so you don’t have to take all those high-power things that a lot of doctors want you to take. (Cat owner)
Participants frequently commented that their pets had an intuitive response to pain and would try to provide comfort to their human companion:
I don’t know how he knows, but when I’m having a bad pain day, he’s right there, he’s just right up next to me. He won’t leave me alone. If I move, he is with me. And if I’m having a good day, he’ll spend a lot more time with my wife. (Dog owner)
Participants sometimes referred to the ability of their pets to distract them from pain.
I have to pay attention to them, and I want to pay attention to them, so it takes me out of myself, and I don’t think about how much I hurt. (Cat owner)
I miss my dog right now. My leg is hurting, it’s pulsating, et cetera. I can’t think of anything but that stupid leg. [If she were here,] I’d be more concerned about petting her. She’d roll over, belly up, and say, “Rub my tummy.”
Participants also noted the calming effect of pets and their ability to aid with relaxation.
Just the sense of calmness or whatever, just from having them there, and petting them…I guess relaxation is the best word. It relaxes you. And I think that anyone with chronic pain, you get to the point where you’re like [makes noise] because you’re hurting. So, that really is a substantial benefit. (Dog owner)
Strategy 3: Physical activity
We identified two themes related to the self-management strategy of physical activity: encouraging walking and necessitating other physical activity. As expected, walking dogs (and, occasionally, cats) was the type of physical activity most often described as helping with pain or health more generally.
I have a Fitbit that I walk around with all the time. And I take the dog for a walk. If the dog weren’t there, I probably wouldn’t do it. Especially when the weather is marginal.
Other participants talked about how pet care keeps them active in other ways:
For me it’s the kitty litter box. The box is downstairs in the basement, so when I change it I have to go down two flights of stairs. Hard things for me are standing and walking and stuff so it keeps me moving, even on a bad day.
Strategy 4: Behavioral activation
Distinct from physical activity is the broader notion of behavioral activation. Participants talked about how having pets provided motivation, gave them no choice but to get up or to go outside. In other words, pets compelled participants to perform certain activities, even when in pain or fatigued.
I think it’s kind of mind over matter because it throws me into thinking I have to do this and this and this when I’d rather just lay on the couch and not feel good. It makes you change your mind and have to do that. (Dog owner)
Participants commonly referred to the fact that pet ownership required adherence to a routine:
I mean, you can’t change their routine. They’re used to it and have needs that you gotta meet. So it forces you to get up and take care of them. (Dog owner)
A couple of people alluded to pets’ ability to keep them cognitively active:
I think another thing that helps is sometimes an issue [related to pet health] will come up and next thing you know is you’re joining this younger generation like, “Let’s Google it.” Keeping your brain cells pretty active. (Dog owner)
Some also described their pets as having an energizing effect:
There are days I come home exhausted. But the minute I get upstairs to change and [cat name] is up there and he’s looking at me like, “Please pick me up, please feed me, please make sure I have water.” …. It’s like with a kid, you get that extra burst of energy and you know you’re responsible and come through.
Strategy 5: Social activation
Respondents described two types of social activation related to pets. One is that having pets increased social activity with people, helping them to build or maintain relationships:
Just walking a pet, you not only see your neighbors and say hi, but you stop and talk because they engage you over your pet. (Dog owner)
Less often, participants described the social connection with pets themselves, particularly as conversation partners:
I talk to him all day long. He’s the best conversationalist in the world, because he doesn’t interrupt, because he doesn’t disagree. (Dog owner)
Strategy 7: Sleep
Pets’ soothing presence, ability to provide a sense of security, and encouraging adherence to a sleep routine were all ways in which pets promoted healthy sleep:
She won’t let me sleep beyond a certain time. And … because I’m kind of a night owl, she starts to bug me at a certain time. Because she wants to go to bed so she wants me to go to bed too. (Cat owner)
Negative/null effects of pets
While the vast majority of comments about pets were positive, some participants also mentioned challenges related to pet ownership that may hinder the pain management strategies outlined above. Most often, such comments involved potentially negative effects on mood, including worry related to finding care for their pet if or when the owner is not able to (9 comments), concerns about pet health (5 comments), cost of pet care (3 comments), and anticipatory grief (2 comments). One participant mentioned that the therapeutic effect of having a dog lay at one’s side (relaxation/distraction) can become painful if too much of the dog’s weight rests on the owner’s body. Four comments pertained to potential negative effects of physical activity with pets, such as injury or fear of injury due to walking a rambunctious dog, or strain from picking up a heavy pet. One participant described her pet having a negative impact on social activity with a friend, and six participants mentioned occasional sleep interruptions due to pets.
In a focus group discussion, not every participant responds to every question; therefore, it is impossible to know how often a given benefit is not experienced. Nonetheless, three comments demonstrated that pets do not inevitably affect health in a given domain. For example:
I don’t think he keeps me going, because I’m pretty strong-willed and I get myself going. (Dog owner)
Discussion and Implications
The present study was designed to elucidate the role of pet ownership in helping older adults cope with persistent pain, one of the most common health challenges in older age. Guided by the biopsychosocial model of chronic pain, we conducted a series of focus groups with pet-owners age 70 and over who had long-term, limiting pain. About half of these met National Pain Strategy criteria for high-impact chronic pain, representing a severely affected subgroup of older adults who are at heightened risk of poor health outcomes (Pitcher, VonKorff, Bushnell, & Porter, 2019). We found evidence that pets can play a role in motivating or facilitating six types of evidence-based pain self-management strategies.
Mood management
Depression and anxiety often accompany chronic pain, and these mood disturbances can exacerbate pain’s intensity, duration, and interference with function (Adams & Turk, 2018). Strategies aimed at controlling negative thoughts and emotions are thus a core element of pain self-management training (International Association for the Study of Pain, 2019). Our participants described a variety of ways in which pets can enhance mood—e.g., making owners feel loved and needed, offering companionship and emotional support—benefits that are frequently discussed in the literature on HAI and older adults (Gee et al., 2017). Being able to provide meaningful care, and not just receive it, may also enhance self-efficacy (Pachana, Ford, Andrew, & Dobson, 2005), which may help people cope with pain more effectively.
Pets also offered something positive to our pain-affected participants: joy and laughter. This is noteworthy given that pain researchers have recently begun to explore the value of positive-activity interventions, which promote resilience to chronic pain (Hassett & Finan, 2016). These programs, rooted in positive psychology, encourage people to “upregulate” positive psychosocial factors by, for example, pursuing pleasant activities and honing a sense of purpose, and are hypothesized to improve pain outcomes through both biological and psychosocial pathways (Hassett & Finan, 2016; Hausmann et al., 2017). Our findings suggest that pets may be a natural focus for positively valenced activities, which may be particularly effective with older adults (Carstensen, 2006).
While most discussion of pets and mood centered on their beneficial effects, we also heard from participants that pets can be a source of sadness (e.g., when they die) and stress (e.g., pet health or behavior issues). As with stress and sadness from any other source, it is possible that these negative emotions could exacerbate pain and interfere with pain management.
Relaxation and distraction
Participants repeatedly noted that their pets soothed them and made them forget about their pain; moreover, some claimed that their pets knew precisely when comfort was needed. Relaxation is considered one of the most important and effective coping skills for controlling pain (Keefe et al., 2006). The pleasurable distraction that pets bring to daily life may reduce catastrophic thinking and hypervigilance common among people with chronic pain (Adams & Turk, 2018). While analgesic effects of contact have been found with therapy dogs in a clinical setting (Marcus et al., 2012), our findings demonstrate that pets, who are in a position to provide “as needed” relaxation and distraction, can have a similar effect.
Physical activity
One of the most robust findings in the literature on HAI and health is that dog ownership is associated with increased walking (Christian et al., 2013; Dall et al., 2017). This health benefit is especially salient given that moderate physical activity is considered an essential non-pharmacological treatment for many pain conditions. Most of the dog owners in our focus groups remarked that their dogs motivate or compel them to walk regularly, which some described as beneficial for pain. More surprising, perhaps, is that some cat owners in the group also believed that their cats caused them to be more physically active—either by walking with them outside or through pet-care tasks like feeding them, picking them up, or cleaning litterboxes.
Behavioral activation
Participants spoke bluntly about how their pets forced them to get up off the sofa or out of bed, do things, go outside—even when they were hurting, tired, or would simply prefer to be inactive. This encapsulates the idea of “behavioral activation,” a vital skill taught in cognitive-behavioral approaches to managing pain. The demands of pet ownership thus appear to limit the extent to which people can engage in maladaptive pain behaviors such as “guarding” (restricting movement out of fear), while encouraging more adaptive behaviors such as task persistence (maintaining activity while experiencing pain) (Jensen, Nielson, & Kerns, 2003), and keeping up valued “well” activities like hobbies and socializing (Jensen, 2011).
Social activation
We heard a variety of anecdotes from participants about how pet ownership enhanced their relationships with other people. This is not surprising, given that studies have consistently documented the potential for pets to serve as social catalysts (Wood et al;, 2015). Since persistent, limiting pain can contribute to social isolation, the tendency of pets to promote social contact may be especially important.
While social activation is encouraged for people with chronic pain, it is also true that chronic pain can put a strain on social relationships. For example, people with pain often report feeling stigma and skepticism even from family and close friends (Adams & Turk, 2018). The nonjudgmental relationships that our participants described having with their pets may provide benefits that are not always available in their human relationships—particularly given that people expressed ideas such as their pets were “good listeners” and could intuit the pain-related needs of their human companions. A previous study found that the psychological benefits of social relationships with pets appear to complement, rather than replace, those with other people, and that pet relationships can offset feelings of isolation from other people (McConnell, Brown, Shoda, Stayton, & Martin, 2011). Our data is consistent with these dual pathways, and offers examples of how they are especially helpful in the presence of pain.
Implications:
Findings from this study have potential significance for a large group of older Americans, given that both pet ownership and chronic pain are widespread in this population. In our small sample, both cats and dogs played helpful roles in pain management, and benefits were experienced by both men and women. Although our study was not designed to quantify the extent to which pets improve pain-related outcomes, findings suggest that providers working with pain-affected older adults may want to inquire about the presence of pets. For interested patients, providers could discuss how pet care and companionship might be incorporated into pain management and coping strategies (e.g. dog walking, or playing with a pet to provide distraction during a flare-up). Providers could also point patients to resources that help older adults learn new skills with pets (see https://www.akc.org/) and engage in meaningful activities with their pet and with other pet owners.
Our study also sets the stage for research into formal ways to leverage the power of pet ownership when trying to engage more people in chronic pain self-management regimens (IPRCC, 2016). Jensen and colleagues remind us that people need to be motivated to engage in pain self-management, which often involves difficult behavioral changes (Jensen et al., 2003). Pets might be an effective “hook” in this regard for some older chronic pain patients, given the positive feelings they tend to engender. Specifically, pain self-management educational materials or curricula could feature some of the pet-related strategies that align with core self-management skills, as shown in our model (Figure 1). The effectiveness of “pet-adapted” materials in improving engagement and outcomes related to pain self-management could be assessed.
Despite the potential benefits that pet ownership may bring to older adults experiencing pain, we do not believe that our results suggest that older pain-affected adults without pets should go out and get one. Besides the fact that our study design does not permit such a conclusion, the field of human-animal interaction generally lacks strong evidence that acquiring a pet improves health. Such evidence will continue to be elusive, as research on pets and health is almost always observational in nature (Friedmann & Gee, 2018), due to practical and ethical issues inherent in randomly assigning pet ownership in the context of an experimental study, and is confounded by pre-existing differences between pet owners and non-owners (Saunders, Parast, Babey, & Miles, 2017). Even among pet owners, there is great variability in whether their pet could play a role in chronic pain self-management.
Moreover, the drawbacks of pets identified in a small number of comments are confirmed elsewhere in the literature: for example, a recent, nationally-representative survey revealed that 6% of pet-owners age 50–80 in the United States have experienced a fall or injury due to their pet and 18% report that pet care strains their budget (Janevic et al., 2019). Other documented pet-related risks include depression associated with bereavement, zoonotic infections, and allergic reactions (Matchock, 2015). Therefore, decisions about pet ownership, including among older adults with chronic pain, should be made only after carefully weighing pros and cons (Janevic et al., 2019). The most fruitful direction for research on pets and health in older adults may be to consider how existing pets can be thought of as a resource for managing health conditions which, like chronic pain, are biopsychosocial in nature.
Limitations:
While our results provide novel information on how pet ownership can help older people with daily management of chronic pain, they almost certainly portray a more prominent and more therapeutic role for pets than is the norm. Many of our participants had intensely positive relationships with their pets that may be atypical. The research team is also made up of pet enthusiasts and, although we tried to avoid it, we may have contributed a positive bias to the questions we asked or interpretations we made. Another limitation is that our participants were almost exclusively White non-Hispanic, with education levels indicative of higher SES—characteristics that are associated with pet ownership (Saunders et al., 2017). Our findings may not apply to other population subgroups, who may experience more drawbacks to pet ownership (e.g., cost, housing-related, reduced access to training opportunities) or who may have different cultural beliefs and practices regarding pets.
Pets, too, vary widely in the characteristics that allow them to provide health benefits to their owners, and their ability to be an asset to pain management likely changes over time (e.g., healthy, energetic puppy vs. older dog with chronic health problems). In sum, there are many variables that shape how an individual pet affects a given owner’s health; our results simply signal the possibility of benefits for at least some older adults with chronic pain.
Conclusion:
Older dog- and cat-owners in our study reported that these pets facilitate behaviors and thoughts that are beneficial for managing persistent pain. Older adults should be encouraged to consider how the human-animal interaction provided by pet ownership can help them cope with pain. Testing more formal ways of leveraging pets’ supportive role may result in new, appealing approaches to engaging older adults in chronic pain self-management.
Supplementary Material
Acknowledgement:
We thank Anurima Kumar for her help with data management and manuscript preparation.
Funding: This work was supported by a grant from the Michigan Institute of Clinical & Health Research (MICHR) [grant number UL1TR002240]; and by grants from the National Institute on Aging [K01 AG050706–01A1 to MRJ]; and the National Institute on Drug Abuse [5K23DA038718–03 to JG].
Footnotes
Declaration of Conflicting Interests: The authors declare that there is no conflict of interest.
IRB approval: This study was approved by the University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board (HUM00130644).
Contributor Information
Mary R. Janevic, Department of Health Behavior and Health Education, University of Michigan School of Public Health, 1415 Washington Heights, Ann Arbor, Michigan, 48109-2029.
Varick Shute, Department of Health Behavior and Health Education, University of Michigan School of Public Health, 1415 Washington Heights, Ann Arbor, Michigan, 48109-2029.
Cathleen M Connell, Department of Health Behavior and Health Education, University of Michigan School of Public Health, 1415 Washington Heights, Ann Arbor, Michigan, 48109-2029.
John D. Piette, Department of Health Behavior and Health Education, University of Michigan School of Public Health, 1415 Washington Heights, Ann Arbor, Michigan, 48109-2029.
Jenna Goesling, Department of Physical Medicine and Rehabilitation, University of Michigan Medical School, 325 E Eisenhower Pkwy, Ann Arbor, MI 48108.
Julie Fynke, Wayne State University School of Medicine, Scott Hall (Room: 1102), 540 E. Canfield, Detroit, MI 48201.
Reference List
- Adams LM, & Turk DC (2018). Central sensitization and the biopsychosocial approach to understanding pain. Journal of Applied Biobehavioral Research, e12125. [Google Scholar]
- AGS Panel on Persistent Pain in Older Persons. (2002). The management of persistent pain in older persons. J Am Geriatr Soc, 50(6 Suppl), S205–224. [DOI] [PubMed] [Google Scholar]
- Bradley L, & Bennett PC (2015). Companion-Animals’ Effectiveness in Managing Chronic Pain in Adult Community Members. Anthrozoös, 28(4), 635–647. doi: 10.1080/08927936.2015.1070006 [DOI] [Google Scholar]
- Carstensen LL (2006). The influence of a sense of time on human development. Science, 312(5782), 1913–1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian HE, Westgarth C, Bauman A, Richards EA, Rhodes RE, Evenson KR, … Thorpe RJ Jr (2013). Dog ownership and physical activity: a review of the evidence. Journal of Physical Activity and Health, 10(5), 750–759. [DOI] [PubMed] [Google Scholar]
- Dall PM, Ellis SLH, Ellis BM, Grant PM, Colyer A, Gee NR, … Mills DS (2017). The influence of dog ownership on objective measures of free-living physical activity and sedentary behaviour in community-dwelling older adults: a longitudinal case-controlled study. BMC public health, 17(1), 496. doi: 10.1186/s12889-017-4422-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehde DM, Dillworth TM, & Turner JA (2014). Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol, 69(2), 153–166. doi: 10.1037/a0035747 [DOI] [PubMed] [Google Scholar]
- Friedmann E, & Gee NR (2018). Critical Review of Research Methods Used to Consider the Impact of Human-Animal Interaction on Older Adults’ Health. Gerontologist. doi: 10.1093/geront/gnx150 [DOI] [PubMed] [Google Scholar]
- Gatchel RJ, Peng YB, Peters ML, Fuchs PN, & Turk DC (2007). The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull, 133(4), 581–624. doi: 10.1037/0033-2909.133.4.581 [DOI] [PubMed] [Google Scholar]
- Gee NR, Mueller MK, & Curl AL (2017). Human–Animal Interaction and Older Adults: An Overview. Frontiers in psychology, 8, 1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerriero F, & Reid MC (2017). New opioid prescribing guidelines released in the US: what impact will they have in the care of older patients with persistent pain? Curr Med Res Opin, 33(2), 275–278. doi: 10.1080/03007995.2016.1254603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassett AL, & Finan PH (2016). The role of resilience in the clinical management of chronic pain. Curr Pain Headache Rep, 20(6), 39. [DOI] [PubMed] [Google Scholar]
- Hausmann LR, Youk A, Kwoh CK, Ibrahim SA, Hannon MJ, Weiner DK, … Parks A (2017). Testing a positive psychological intervention for osteoarthritis. Pain Medicine, 18(10), 1908–1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Association for the Study of Pain. (2019). Pain Management for Older Adults: A Self-Help Guide (Hadjistavropoulos T & Hadjistavropolous HD Eds.). Philadelphia, PA: Wolters Kluwer. [Google Scholar]
- IPRCC. (2016). National Pain Strategy, : US Department of Health and Human Services. [Google Scholar]
- Janevic M, Solway E, Malani P, Singer D, Kirch M, Kullgren J, Connell C How pets contribute to healthy aging. University of Michigan National Poll on Healthy Aging. April 2019. Available at: http://hdl.handle.net/2027.42/148428
- Jensen MP (2011). Psychosocial approaches to pain management: an organizational framework. Pain, 152(4), 717–725. doi: 10.1016/j.pain.2010.09.002 [DOI] [PubMed] [Google Scholar]
- Jensen MP, Nielson WR, & Kerns RD (2003). Toward the development of a motivational model of pain self-management. The Journal of Pain, 4(9), 477–492. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Caldwell DS, Tischner J, & Aspnes A (2006). Cognitive-behavioral interventions for arthritis pain management In Bartlett SJ, Bingham CO, Maricic MJ, Iversen MD & Ruffing V (Eds.), Clinical Care in the Rheumatic Diseases (pp. 221–226). Atlanta, GA: Association of Rheumatology Health Professionals. [Google Scholar]
- Krueger RA, & Casey MA (2000). Focus Groups: A Practical Guide for Applied Research (3rd ed.). Thousand Oaks, CA: SAGE Publications, Inc. [Google Scholar]
- Marcus DA, Bernstein CD, Constantin JM, Kunkel FA, Breuer P, & Hanlon RB (2012). Animal-assisted therapy at an outpatient pain management clinic. Pain Med, 13(1), 45–57. doi: 10.1111/j.1526-4637.2011.01294.x [DOI] [PubMed] [Google Scholar]
- Matchock RL (2015). Pet ownership and physical health. Current Opinion in Psychiatry, 28(5), 386–392. [DOI] [PubMed] [Google Scholar]
- McConnell AR, Brown CM, Shoda TM, Stayton LE, & Martin CE (2011). Friends with benefits: on the positive consequences of pet ownership. J Pers Soc Psychol, 101(6), 1239–1252. doi: 10.1037/a0024506 [DOI] [PubMed] [Google Scholar]
- McNicholas J, Gilbey A, Rennie A, Ahmedzai S, Dono JA, & Ormerod E (2005). Pet ownership and human health: a brief review of evidence and issues. BMJ, 331(7527), 1252–1254. doi: 10.1136/bmj.331.7527.1252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles MB, & Huberman AM (1994). Qualitative data analysis: an expanded sourcebook. Thousand Oaks: Sage Publications. [Google Scholar]
- Mueller MK, Gee NR, & Bures RM (2018). Human-animal interaction as a social determinant of health: descriptive findings from the health and retirement study. BMC public health, 18(1), 305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Needell N, & Mehta-Naik N (2016). Is Pet Ownership Helpful in Reducing the Risk and Severity of Geriatric Depression? Geriatrics, 1(4), 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachana NA, Ford JH, Andrew B, & Dobson AJ (2005). Relations between companion animals and self-reported health in older women: cause, effect or artifact? Int J Behav Med, 12(2), 103–110. doi: 10.1207/s15327558ijbm1202_8 [DOI] [PubMed] [Google Scholar]
- Pitcher MH, Von Korff M, Bushnell MC, & Porter L (2019). Prevalence and profile of high-impact chronic pain in the United States. The Journal of Pain, 20(2), 146–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid MC (2016). Expanding Targets for Intervention in Later Life Pain: What Role Can Patient Beliefs, Expectations, and Pleasant Activities Play? Clin Geriatr Med, 32(4), 797–805. doi: 10.1016/j.cger.2016.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders J, Parast L, Babey SH, & Miles JV (2017). Exploring the differences between pet and non-pet owners: Implications for human-animal interaction research and policy. PLoS One, 12(6), e0179494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong A, Sainsbury P, & Craig J (2007). Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care, 19(6), 349–357. doi: 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Whitlock EL, Diaz-Ramirez LG, Glymour MM, Boscardin WJ, Covinsky KE, & Smith AK (2017). Association between persistent pain and memory decline and dementia in a longitudinal cohort of elders. JAMA Intern Med, 177(8), 1146–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood L, Martin K, Christian H, Nathan A, Lauritsen C, Houghton S, … McCune S (2015). The pet factor--companion animals as a conduit for getting to know people, friendship formation and social support. PLoS One, 10(4), e0122085. doi: 10.1371/journal.pone.0122085 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.