Abstract
Study objective:
Despite the increased availability of naloxone, death rates from opioid overdose continue to rise. The goal of this study is to determine the one-year mortality of patients who were treated for a non-fatal opioid overdose in Massachusetts emergency departments.
Methods:
Retrospective observational study of patients from three linked statewide Massachusetts datasets: a master demographics list, an acute care hospital case mix database, and death records. Patients discharged from the emergency department (ED) with a final diagnosis of opioid overdose were included. The primary outcome measure was death from any cause within one year of overdose treatment.
Results:
During the study period, 17,241 patients treated for opioid overdose. Of the 11,557 who met study criteria, 635 (5.5%) died within one year, 130 (1.1%) died within one month and 29 (0.25%) died within 2 days. Of the 635 deaths at 1 year, 130 (20.5%) occurred within 1 month and 29 (4.6%) occurred within 2 days.
Conclusion:
he short-term and one-year mortality of patients treated in the ED for non-fatal opioid overdose is high. The first month, and particularly the first two days after overdose, is the highest risk period. Patients who survive opioid overdose should be considered high risk and receive interventions such as offering buprenorphine, counseling and referral to treatment prior to ED discharge.
Introduction
Background
The opioid overdose epidemic continues, with an estimated 49,000 deaths in the U.S. involving an opioid overdose in 2017 (1). The emergency department (ED) is at the front line of caring for patients who overdose and the large number of patients treated in the ED who survive to be discharged does not receive significant attention. Data indicate that there were 92,000 ED visits for unintentional, nonfatal overdose in 2014 in the United States (2). This number appears to be increasing: a recent report from 45 states indicated that there were 142,557 ED visits for suspected opioid-involved overdoses between July 2016 and September 2017, a staggering average increase of 5.6% per quarter (3).
In Massachusetts, over 2,000 opioid-related deaths occurred in 2016, more than doubling from 2013 (4). These deaths occurred despite the broad distribution and use of the opioid antagonist naloxone as well as laws and regulations designed to increase the safety of opioid prescribing (5). Through Chapter 55 of the Acts of 2015, the Massachusetts state legislature permitted individual linkage of data from several state agencies including the Acute Care Hospital Case Mix file (Case Mix) and the Registry of Vital Records and Statistics (6, 7).
Importance
The care of opioid overdose patients in the ED has been largely unchanged over the past decades. Life-threatening instability or cardiorespiratory arrest is treated with standard advanced cardiac life support techniques. Naloxone is administered to those who suffer respiratory depression. Then, the patient who survives is typically observed in the ED for a period of time before being discharged, often with a list of community substance use disorder treatment resources. Despite this common practice, the near and long-term risk of mortality after surviving an ED visit for opioid overdose is understudied.
Goals of This Investigation
We aimed to determine the one-year mortality of patients who were treated in a Massachusetts ED for suspected opioid overdose and subsequently discharged, describing both 30 day and one-year mortality. If mortality after initially surviving an opioid overdose is high, it would support the need for an alternative approach to the treatment of this disease.
Materials and Methods
Study Design, Setting, Data Collection and Processing
As part of Massachusetts’ legislatively mandated epidemiologic study of opioid-related morbidity and mortality, we conducted a population-based retrospective cohort study using a linked dataset combining a master demographics list, an acute care hospital case mix database and state death records. Death data was provided by the Registry of Vital Records and Statistics, which reports information based on death certificates including medical examiner determinations, if applicable. The setting was the entire state of Massachusetts. A conservative matching procedure was used that considered various combinations of name, date of birth, address and social security number to link records. The databases were held by the Massachusetts Department of Public Health (DPH). We programmed statistical analysis at our institution using a dummy data set and sent code to DPH, who ran the code, and returned deidentified study results from actual data. Analysis was done using SAS Studio 3.5 (SAS Institute, Cary, NC). This work was mandated by Massachusetts law using a deidentified dataset and was deemed exempt from review by the Massachusetts DPH Institutional Review Board. Complete information about the state’s initiative, the core datasets, the linking procedure, and privacy protections are described in a state report (7).
Selection of Participants
We included patients who were treated in the ED for opioid overdose based on diagnosis code between July 1, 2011 and September 30, 2015 but did not have an ED visit for opioid overdose in the 6-month period of January 1, 2011 to June 30, 2011. Patients were identified from the state’s Center for Health Information Analysis Case Mix Data indicating an ED visit with International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code of overdose due to prescription opioid (965.00, 965.01, 965.02, 965.09) or heroin (E850.0, E850.1 or E850.2). Death records were analyzed until September 30, 2016 to capture one-year, all-cause mortality. In addition to one-year mortality, we also determined daily mortality for the first 30 days after ED discharge. The date ranges chosen were the maximum time available in the dataset which afforded both a six-month exclusion period (described below) and a one-year look in the future to determine mortality at that time. The sample size was determined by the available data.
Method of Measurement
Index overdose date was defined as having a flagged date for an overdose and no prior record of overdose. Since we only observe individuals from January 1, 2011 onward we cannot know whether an individual had an overdose prior to entry into the database, making our data left-censored. Therefore, we used a 6-month exclusion period helping to ensure that everyone in the study cohort had been overdose-free for a minimum of 6 months, at least within Massachusetts. Although it is possible that individuals had overdoses after the index visit, only the index overdose date was used to count sequentially numbered time periods after overdose. Death records containing date of death were merged with ED data using unique patient identifiers. Deaths were categorized by using the International Classification of Disease 10 (ICD-10) codes for mortality or using a literal search of written cause of death from the medical examiner’s office for records that did not yet have a valid ICD-10 code. The following codes were selected from the underlying cause of death field to identify poisonings/overdoses: X40–X49, X60–X69, X85–X90, Y10–Y19, and Y35.2. All multiple cause of death fields were then used to identify an opioid-related death: T40.0, T40.1, T40.2, T40.3, T40.4, and T40.6. For those with an identified death record, number of days between index opioid overdose and death was computed. Demographic data on each individual was merged from the Case Mix and master demographic files. Age was defined as the age of the patient in years as reported as of December 31, 2015, regardless of age at time of overdose.
Outcome Measures
Our primary outcome measure was one-year mortality rate of patients after a first overdose. Mortality rate was computed conditional on being discharged from the ED.
Primary Data Analysis
The one-year mortality rate was computed by calculating the percentages of individuals who survived the initial overdose and died within one year. Descriptive statistics (means, medians, and percentages) are reported for the demographic characteristics of cohorts, and 95% confidence intervals (CI) were reported for the primary study outcomes.
Results
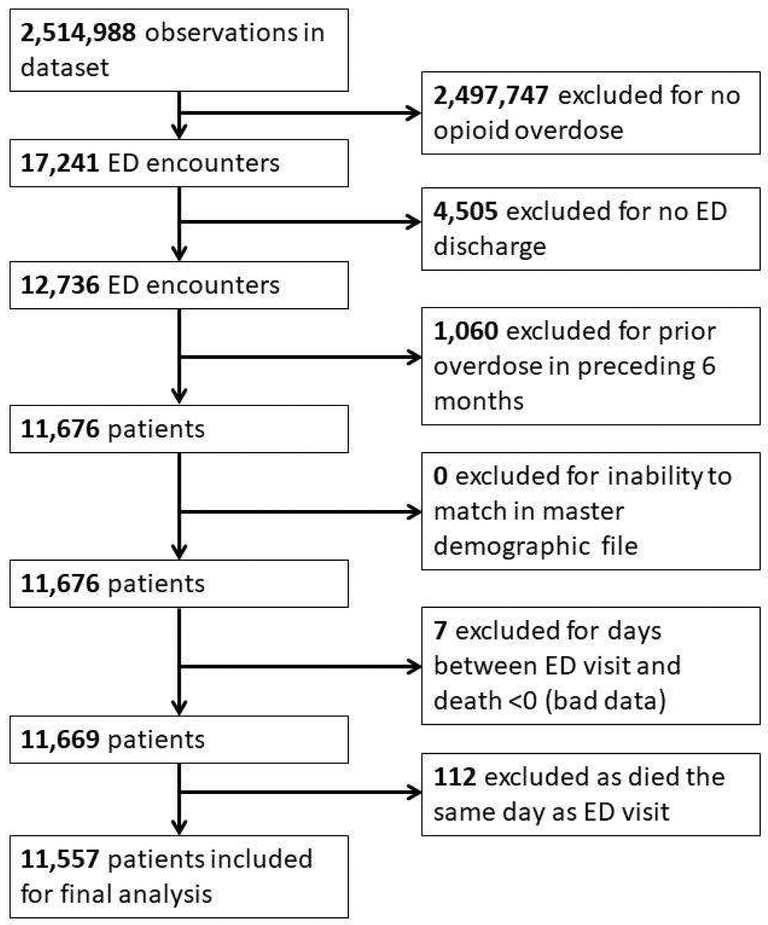
Between July 1, 2011 and September 30, 2015, there were a total of 17,241 patients treated for opioid overdose in Massachusetts EDs. Of these, 11,557 (67.0%) were discharged from the ED and met study inclusion criteria (Figure 1). Of the discharged patients, 635 (5.5% (CI [5.08–5.92])) died within one year, 130 (1.1% (CI [0.94–1.33])) died within one month and 29 (0.25% (CI [0.17–0.36])) died within 2 days. The median age of those who died within one year was 39 (IQR 31–53) years and 451 (71.0%) were male. Race/ethnicity was recorded as white: 557 (87.7%), black: 21 (3.3%) and Hispanic: 47 (7.4%). A total of 125 decedents (19.7%) were recorded to be homeless.
Figure 1:
Flow diagram of included and excluded subjects.
Of the 635 that died after discharge, death records indicated that 428 (67.4%) died of an opioid-related overdose. The manner of death was recorded as 121 (19.1%) natural causes, 460 (72.4%) accidental, 13 (2.0%) suicide and 41 (6.5%) other or pending investigation. The most common location of death was hospital: 310 (48.8%), followed by in a residence: 146 (23.0%), and the remainder nursing home/other/unknown.
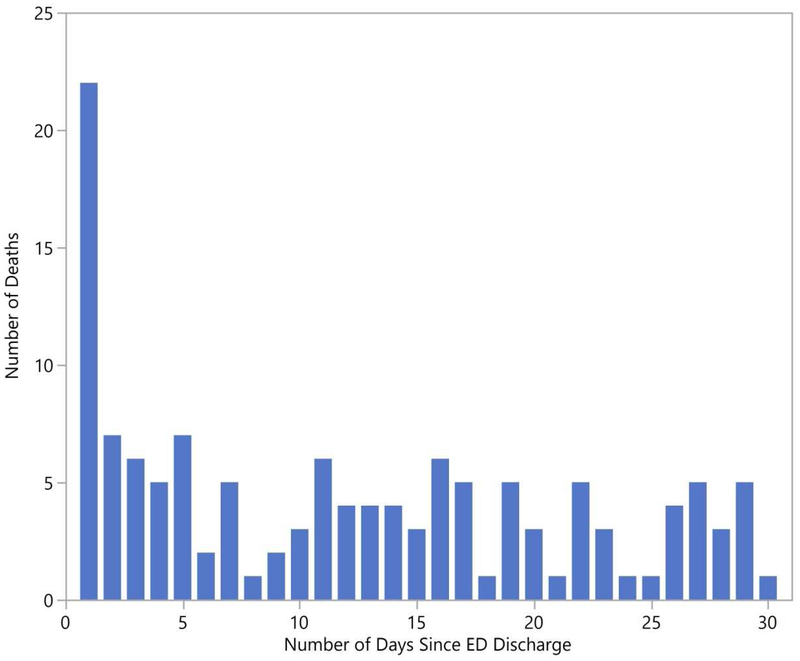
As the data included the date of discharge after overdose, it was possible to evaluate rates of death on a daily basis after ED treatment for overdose, and we did so for the first month after discharge. Of the patients who died, 130 (20.5%) died within the first month. The distribution of deaths for the first 30 days after ED discharge is demonstrated in Figure 2. A large number of patients who died in the first month after ED discharge (n=29, 22.4%) died within the first 2 days.
Figure 2:
Number of deaths after emergency department treatment for non-fatal overdose by number of days after discharge in the first month, by day, n=130.
Limitations
The data in this study was provided by a single state and was reliant on details from large linked datasets that were not originally collected for research purposes. Hence, there may have been misclassification of the outcome variables either through lack of capture or error in linkage between the datasets. Also, if patients were treated for overdose or died in other states, the event would not be included in our analysis.
Discussion
The short-term and one-year mortality of opioid overdose patients who initially survive is high. For patients that were treated in the ED for overdose over 5% were dead within one year. These numbers are particularly tragic given the relatively young age of those who died: the median age of decedents was only 39 years. The loss of life at this young age is responsible for an overall decreased life expectancy seen in the U.S. for the past two years (8), the first decrease in over two decades.
The location of death is also important: in about a quarter of cases, the place of death was a residence, possibly indicating patients who died prior to medical assistance arriving. This finding has implications regarding bystander availability of naloxone, including the Surgeon General’s call for patients at risk for opioid overdose and community members who come into contact with those people to have naloxone available. It is possible that rapid access to naloxone in the community could have saved lives. Conversely, if an individual was using opioids alone, bystander naloxone would not have helped, and the actual lesson is to educate people not to use alone.
A large number of patients discharged from the ED after an opioid overdose die in the first month. About a fifth of patients who died did so in the first month after ED discharge, and about a fifthof those died in the first 2 days. These numbers highlight the importance of early, aggressive intervention for substance use disorder treatment. The initial health care contact in the ED is a critical period for intervention such as buprenorphine initiation (10), naloxone distribution, counselling, and referral to further treatment prior to ED discharge. These findings suggest that hospitals rapidly adopt medication for addiction treatment programs and other interventions for ED patients treated for opioid overdose.
Disclosure:
SGW completed an unrelated research project in 2016 funded by Kaleo Pharma, a company that produces a naloxone autoinjector, and is a former scientific advisory board member of Epidemic Solutions, LLC and General Emergency Medical Supplies Corp, both start-up companies aiming to increase availability of naloxone for bystanders.
Dr. Weiner is supported by NIH grant 1-R01-DA044167.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Scott G. Weiner, Brigham and Women’s Hospital, Boston, MA.
Olesya Baker, Brigham and Women’s Hospital, Boston, MA.
Dana Bernson, Massachusetts Department of Public Health, Boston, MA.
Jeremiah D. Schuur, Alpert Medical School, Brown University, Providence, RI.
References
- 1.National Center for Health Statistics. CDC Wonder. Number of deaths involving opioids. Revised January 2019. Available at: https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. Accessed April 10, 2019.
- 2.CDC. Annual surveillance report of drug-related risks and outcomes—United States, 2017. Atlanta, GA: US Department of Health and Human Services, CDC; 2017. Available at: https://www.cdc.gov/drugoverdose/pdf/pubs/2017-cdc-drug-surveillance-report.pdf. Accessed April 10, 2019. [Google Scholar]
- 3.Vivolo-Kantor AM, Seth P, Gladden RM, Mattson CL, Baldwin GT, Kite-Powell A, Coletta MA. Vital Signs: Trends in Emergency Department Visits for Suspected Opioid Overdoses - United States, July 2016-September 2017. MMWR Morb Mortal Wkly Rep. 2018. March 9;67(9):279–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Massachusetts Department of Public Health. Data Brief: Opioid-Related Overdose Deaths Among Massachusetts Residents. November 2018. Available at: https://www.mass.gov/files/documents/2018/11/16/Opioid-related-Overdose-Deaths-among-MA-Residents-November-2018.pdf. Accessed April 10, 2019.
- 5.Massachusetts Chapter 52 of the Acts of 2016. An act relative to substance use, treatment, education and prevention. Available at: https://malegislature.gov/Laws/SessionLaws/Acts/2016/Chapter52. Accessed April 10, 2019.
- 6.The 190th General Court of the Commonwealth of Massachusetts. Chapter 55: An act requiring certain reports for opiate overdoses. Available at: https://malegislature.gov/Laws/SessionLaws/Acts/2015/Chapter55. Accessed April 10, 2019.
- 7.The Commonwealth of Massachusetts. An assessment of fatal and nonfatal opioid overdoses in Massachusetts (2011–2015). Massachusetts Department of Public Health; 2017. Available at: https://pilot.mass.gov/files/documents/2017/08/31/legislative-report-chapter-55-aug-2017.pdf. Accessed April 10, 2019. [Google Scholar]
- 8.Kochanek KD, Murphy SL, Xu JQ, Arias E. Mortality in the United States, 2016. NCHS Data Brief, no 293. Hyattsville, MD: National Center for Health Statistics; 2017. Available at: https://www.cdc.gov/nchs/data/databriefs/db293.pdf. Accessed April 10, 2019. [Google Scholar]
- 9.Seth P, Scholl L, Rudd RA, Bacon S. Overdose Deaths Involving Opioids, Cocaine, and Psychostimulants - United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018. March 30;67(12):349–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D’Onofrio G, O’Connor PG, Pantalon MV, Chawarski MC, Busch SH, Owens PH, Bernstein SL, Fiellin DA. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015. April 28;313(16):1636–44.5. [DOI] [PMC free article] [PubMed] [Google Scholar]