Abstract
Objective. To gauge multiple dimensions of pharmacy students’ professionalism, stress, and satisfaction with the Doctor of Pharmacy (PharmD) program.
Methods. An online survey of first- through fourth-year pharmacy students was conducted from 2015-2018 to gauge the degree of students’ professionalism (personal reflection, patient-centric care focus, cultural and interprofessional competencies), program stress (levels, sources, and burnout syndrome), and satisfaction. Multilevel structural equation modeling (SEM) determined the relationship between stress and satisfaction, and the degree to which these impacted levels of professionalism after adjusting for potential correlates (age, sex, financial stress, relationship status, race, and employment status).
Results. Seven hundred sixty-four responses to the survey were received across the four calendar years. Of the students in the sample, 51% were female with a mean (SD) age of 26.6 (3.4) years. The overall response rate to the surveys was 86.2%. Professionalism was most strongly indicated by the measures of community-centeredness, patient-centeredness, and perceived benefits of being part of a team-based environment. The SEM model demonstrated an inverse relationship between the two composite latent constructs of stress and satisfaction. When modeled simultaneously, program satisfaction was found to be the more significant predictor of professionalism than stress after adjusting for associations with age, sex, and relationship status.
Conclusion. Professionalism of pharmacy students is positively associated with students’ satisfaction with the program, but professionalism is not independently significantly predicted by stress. Students who have positive responses to community- and patient-centeredness and who feel they benefit from engaging in a team-based environment are most likely to have greater professionalism.
Keywords: pharmacy education, stress, satisfaction, professionalism, structural equation modeling
INTRODUCTION
Professionalism in healthcare refers to an individual’s embodiment of a set of attitudes and values appropriate for future providers. The more strongly held those professional attitudes are, the greater the likelihood that pharmacists will develop trusting relations with the patients they serve, resulting in improved access and quality of care. The expectancy of a high degree of professionalism is particularly true in the current environment where there is an increasing need for pharmacists to be more “patient-centric.”1 While the importance of professionalism in healthcare is broadly recognized, the literature on the development of healthcare professional attitudes in pharmacy education specifically is sparse.
Furthermore, there is evidence that colleges of pharmacy are not adequately developing students’ professionalism, and that revisions to curricula and teaching methods should be based on systematically gathered evidence.2 Using qualitative grounded theory research, Thompson and colleagues found that both first- and fourth-year pharmacy students and faculty members felt professionalism should be addressed throughout the curriculum.3 Pileggi and colleagues found that the majority of pharmacy residents did not feel “very prepared” for the emotional challenges they encountered.1 Rabi and colleagues found that 16.3% of 300 PharmD students at four US colleges of pharmacy admitted to cheating.4 Many students in this study admitted to activities traditionally defined as dishonest. To inform curricular changes that would better develop professionalism, we need to determine what promotes professionalism in pharmacy students and what may impair its development.
Students’ stress and satisfaction are two factors that may influence their professional behavior, and there is interest in monitoring these feelings as well. The Accreditation Council for Pharmacy Education requested that the University of Utah College of Pharmacy provide a brief description of first professional year (P1) student satisfaction following the rollout of a new curriculum in 2014. Furthermore, colleges of pharmacy have called for development of universal stress assessment.17 Thus, the University of Utah College of Pharmacy was well situated to examine its students’ stress, satisfaction, and professionalism.
Literature about education in other health science professions and about practicing pharmacists provided us with the conceptual foundations for studying the professionalism of pharmacy students and its relation to stress and satisfaction. For instance, studies in medicine, nursing, and dentistry, have provided conceptual models, definitions of relevant constructs (eg, reflective practice to build professionalism), and standardized measures of relevant attitudinal domains.5-15 The authors have previously studied independent and community chain pharmacists nationwide, finding that a workplace with high stress and low satisfaction led to a greater likelihood to search for a new position and of low levels of career advocacy.16 The application of these models and constructs may assist pharmacy educators in fostering the development of student professionalism.
The University of Utah College of Pharmacy developed, piloted, and conducted an annual survey to gauge multiple dimensions of student professionalism (that would be administered across all four years (P1-P4). This survey comprehensively gauged students’ personal reflection, having a patient-centric care focus, cultural competency, and interprofessional competencies (ie, teamwork roles and responsibilities, patient centeredness, interprofessional bias, appreciation of diversity and ethics, and having a focus on community centeredness). Using this data repository, the aim of the present research was to determine the degree of association between students’ perceived levels of stress engendered by the program and their satisfaction with the program’s curricula, modes of teaching, and administration, and to model the degree to which stress and dissatisfaction may impair students’ abilities to manifest professional attitudes and values central to being effective practitioners.
METHODS
The study received approval from the University of Utah Institutional Review Board. All student participants provided informed consent prior to beginning the survey. This annual survey of P1-P4 students enrolled in the Doctor of Pharmacy (PharmD) program at the University Utah College of Pharmacy was conducted in 2015, 2016, 2017, and 2018. The college’s curriculum was fully accredited by the ACPE over the lifetime of the study. The PharmD curriculum consisted of 10 semesters of training over four years. Instruction was divided into didactic learning and pharmacy practice experiences. Didactic learning included coursework in biomedical, pharmaceutical, social/behavioral/administrative, and clinical sciences. Pharmacy practice experiences were divided between introductory pharmacy practice experiences (IPPEs) in the first three years and advanced pharmacy practice experiences (APPEs) in the fourth year. The program emphasized patient-oriented pharmaceutical care and interprofessional health care systems. Additional experiences included literature evaluation skills, clinical application of evidenced-based use of medications, and two formal seminar presentations on predetermined topics. The entire student body (approximately 60 students in each class year) was invited to complete the survey each year.
An online survey tool, Qualtrics Survey Software (Provo, UT), was used by students to complete the survey. Each student received an invitation letter describing the survey goal, estimated time for completion, confidentiality of responses, general details of the type of questions to be asked, timeframe for completion, and compensation for completion. Respondents were assured that participation was voluntary and that whether or not they participated would not affect their standing in the college or university. The survey took approximately 20 to 25 minutes to complete. All respondents received an honorarium (a $25 gift card for a restaurant in the Salt Lake City, UT area) for completing the survey. There were four survey distribution cycles during the four-year data capture period: in fall 2015 for P2, P3, and P4 students reporting on their experiences during the prior year (ie, their P1, P2, and P3 year, respectively); and in spring 2015, spring 2016, and spring 2017, for P1-P4 students reporting on their experiences during the current year. Responses were not linked to individual students, so individual responses across the years were not tracked.
For demographic variables, students indicated their age in years, sex, self-identification of race and ethnicity, current year in the PharmD program, marital status, employment status during the academic year [defined as per questionnaire], and the degree to which they had difficulty supporting themselves or their families financially.
The Maslach Burnout Inventory (MBI) 15-item student version was used to assess the level of student stress and burnout.18-20 Three dimensions were measured: exhaustion, cynicism, and professional efficacy. Exhaustion was rated by how often the stress of the PharmD program had adversely affected the student’s emotional and physical energy during the last academic year. Cynicism was rated by how often during the last academic year students were interested and enthusiastic about their studies. All items on the MBI were measured on a seven-point Likert scale on which 1=never and 7=every day.
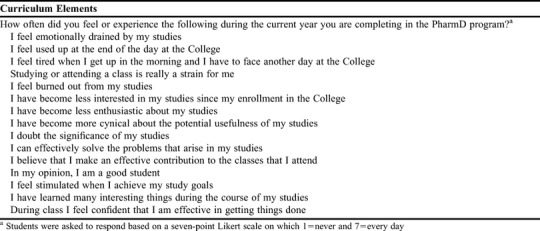
Students also rated the level of perceived stress with 15 curriculum elements (Table 1). The degree to which each of the items contributed to a student’s level of stress experienced in the PharmD program in the academic year was measured using a 10-point scale where 1=not at all and 10=extremely. The items included time available to study, examinations, time with family and friends outside of class, employment (hours working per week), family or other relationships outside of class, health problems, financial issues, and relationships with other students or faculty members in their courses. Following this section, students provided responses in an open-ended question asking if what other elements may have contributed to their program-related stress. As part of the MBI, students were asked to rate their professional efficacy, a measure of students’ confidence and perceived competence in their studies, based on their experience in the previous academic year.
Table 1.
Curriculum Elements that Student Pharmacists Were Asked to Rate Once a Year as Part of a Four-Year Study of Stress and Satisfaction and Their Influence on Professionalism Over Time
Students then indicated their overall satisfaction with the last year they completed in the PharmD program on a Likert scale of 1-10 on which 1=not satisfied at all and 10=extremely satisfied. Students were asked to rate a variety of sources of satisfaction using the same 10-point scale: challenge of the curriculum, logical curriculum progression, engagement in active learning, course loads, provision of knowledge and skills practice at a high level when they graduate, the curriculum as a reasonable value investment, excitement about their future career, development of meaningful relationships with faculty members, satisfaction with college administration, satisfaction with work-life balance, and their academic background being adequate to deal with the challenges of the curriculum. In addition, a six-item Professional Efficacy scale was used to measure students’ feelings of competence and successful achievement in their work and was measured as part of satisfaction.
Students were asked to gauge their loyalty toward and likelihood to recommend the program to friends, relatives, and colleagues using a 10-point scale on which 1=not at all and 10=extremely likely. Students’ individual “likelihood to recommend” scores were used to calculate an aggregated net promoter score (NPS) for the student body. The net promoter score (NPS) is an index ranging from -100 to 100 that is calculated based on the proportion of students that are likely to be promoters compared to the proportion that are likely to be detractors.21-23 Each student was also asked how often they had thought of quitting the PharmD program during their last academic year. The response options were daily, weekly, monthly, every 3 months, every 6 months, yearly, and never.
Professionalism was gauged using three measures: the Groningen Reflective Ability Scale, the Patient-Positive Orientation Scale (PPOS), and the Interprofessional Learning and Cultural Competence (IPAS) measure. The Groningen Reflective Ability Scale24 is a 23-item instrument used to measure personal reflection. The Patient-Positive Orientation Scale (PPOS) 25-28 is an 18-item instrument designed to measure patient-centeredness, interprofessional bias, appreciation of diversity and ethics, and community centeredness. The Interprofessional Learning and Cultural Competence (IPAS) assesses attitudes across five subscales that relate to the 2011 Core Competencies for Interprofessional Collaborative Practice: teamwork roles and responsibilities, patient centeredness, interprofessional bias, diversity and ethics, and community centeredness.29
To examine the relationship between the key constructs of stress, satisfaction, and professionalism, structural equation modeling was used. Structural equation modeling (SEM) refers to a class of statistical models that is an extension of a generalized linear model (eg, ANOVA or regression analysis).29 Structural equation modeling can be used to examine the causal relationships of latent (ie, not directly observed) variables, such as underlying stress, satisfaction, and professionalism.30
The data captured from the scales measuring each domain in the online survey were used to construct the latent variables: stress, satisfaction, and professionalism. Because of the complex and multifactorial nature of stress, satisfaction, and professionalism, using an individual scale would provide a limited and imperfect measure of these variables. However, a major advantage of using SEM is the ability to linearly combine multiple scales, thus allowing the creation of stronger and more robust measures of the underlying variable constructs. The aforementioned observed continuous and categorical scales and questions on stress, satisfaction, and professionalism were used to develop the respective continuous latent variables in this analysis.
The latent professionalism construct was the outcome and was regressed on the stress and satisfaction latent constructs. Stress and satisfaction were allowed to co-vary simultaneously because of their hypothesized inverse relationship.
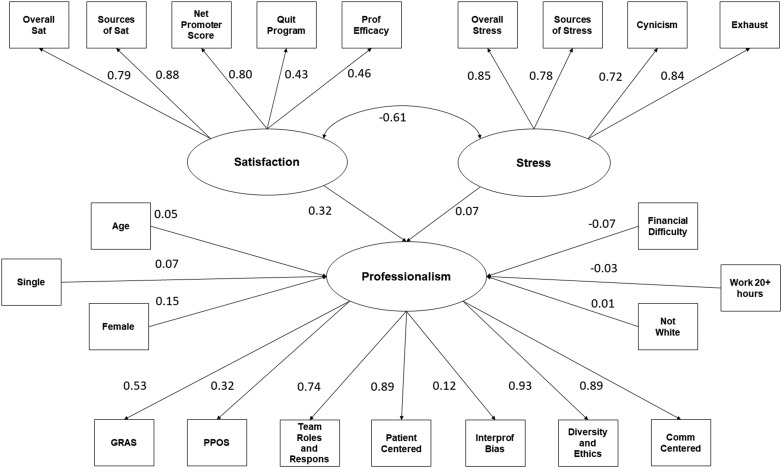
The hypothesized model of the relationships, including the factor-loading variables on the latent constructs, is shown in Figure 1. Multilevel analysis was performed to adjust for cluster-level effects of pharmacy class. Adjusting for a respondent’s pharmacy class was necessary as students within a particular pharmacy class, as occurs in other educational settings, tend to have more similarities than a random sample and therefore cannot be treated as fully independent.
Figure 1.
Structural Equation Model to Determine Statistical Relationship Between Satisfaction and Stress on PharmD Student Professionalism
In addition to the latent variables, professionalism was simultaneously regressed on the following covariates in the model: age (continuous), sex or gender, financial stress (continuous), relationship status (single vs other), race (white vs other), and working status (dichotomized to 20 hours or more per week and less than 20 hours per week). A maximum likelihood estimator with robust standard errors was used. Standardized coefficients of the regression are reported. Standard error of the mean was performed with Mplus, version 8 (Muthén & Muthén, Los Angeles, CA).31
Model fit indices for SEM, including the chi-square test, the Tucker-Lewis Index (TLI), the Bentler’s comparative fit index (CFI), root mean square error of approximation (RMSEA), and the standardized root mean, were examined to assess the model’s comparison to standard measures.32-34
RESULTS
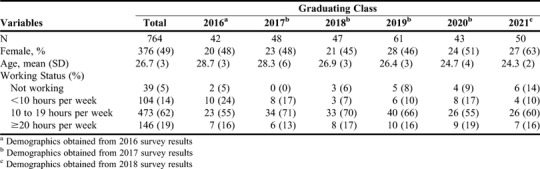
Across the four survey waves (2015, 2016, 2017, and 2018), 764 responses were received. The total population was 51% female with a mean (SD) age of 26.6 (3.4) years (Table 2). The response rate was 81.2% for P1, 89.8% for P2, 93.6% for P3, 78.5% for P4 students, with an overall response rate of 86.2%.
Table 2.
Study Population Characteristics Stratified by Pharmacy Graduating Class
Model fit was evaluated for each latent variable: satisfaction, stress, and professionalism (Table 3) All four loading measures of stress (including level, sources, cynicism, and exhaustion) demonstrated good fit with coefficients above 0.70 and significant p values (<.001). All loading measures on satisfaction were significant (p<.001); however, two measures, quitting the PharmD program and professional efficacy, demonstrated only a moderate magnitude compared to the others. The professionalism model fit showed greater heterogeneity. Nevertheless, three measures, community centeredness, patient centeredness, and team roles and responsibilities, demonstrated a strong and significant fit.
Table 3.
Results of Survey Instrument Measures on Latent Variables in a Study of the Influence of Stress and Satisfaction on Student Pharmacists’ Professionalism
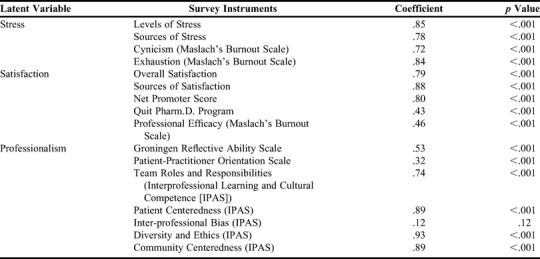
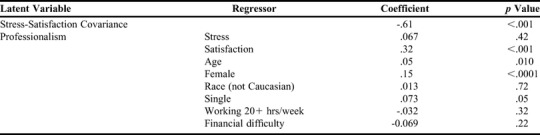
The SEM model results indicated a strong inverse covariance relationship between stress and satisfaction (-.611, p<.001) (Table 4). When modelled simultaneously, satisfaction was shown to be the larger and a more significant predictor of professionalism than stress (after the inverse relationship between stress and satisfaction was taken into account [satisfaction=.32, p<.001; stress=.067, p=.42]). Age (coefficient=.049, p=.01), female gender (coefficient=.15, p <.0001), and single relationship status (coefficient=.073, p=.05) all significantly predicted professionalism in the simultaneous model.
Table 4.
Structured Equation Modeling Regression Analysis Results
Model fit indices were satisfactory. The omnibus chi-square test for goodness of fit (GOF) was significant (indicating poor fit). However, the Tucker-Lewis index was 0.90, the comparative fit index was 0.91, the root mean square error of approximation was 0.08, and the standardized root mean square residual was 0.08, all of which indicated a moderately good fit.
DISCUSSION
To better understand how to develop a professional identity in pharmacy students, we designed this study to understand whether program satisfaction and/or program-related stress impacts the development of professionalism. We found that professionalism was predicted by satisfaction but not independently by stress (after accounting for the finding that students with higher levels of stress had lower levels of satisfaction). Professionalism was also positively associated with age, being female, and being single.
These results have implications for academic pharmacy. Students’ concerns about stress from college workloads is an ongoing issue across higher education.35 Pharmacy education is constantly evolving to keep pace with changing practice guidelines, ACPE standards, and performing modern pharmacy practice. These changes lead to constant levels of stress in faculty members and in students.36,37 However, our results show that stress levels were not directly associated with developing professionalism in pharmacy students after accounting for the relationship between stress and satisfaction and the effect of satisfaction on professionalism. Reasons for the lack of a direct association may be adaption to stress, stress management, or student adjustment over time to maintain life balances despite curricula stress.38
Students who are more satisfied with their education tend to adopt a professional identity. Professional identity is formed at the level of the individual, whereas professionalism is formed at the level of the community, society, and within the pharmacy profession.39 Professionalism is taught and developed through a student pharmacist’s training. However, professional identity is formed by the student’s own deeply held beliefs about what it means to be a professional. A student pharmacist likely develops a strong professional identity when there is alignment among education about professionalism, the social identity of the profession, and the student’s working environment.40 Building greater professional identities is likely to increase advocacy for the profession. However, students across demographic strata and backgrounds may require varying levels of assistance to fully develop their professional identity. Thus, faculty members and school administration should coordinate efforts to understand and address potential barriers to student pharmacists’ development.
Students’ attitudes toward their clinical roles had the strongest connection with their professionalism. The strongest factors of professional identity were students’ view of community and patient centeredness, and team participation. A defined role and responsibility in the healthcare team was also a key component of professionalism. The implications of these findings support an educational emphasis on patient-centered care, population-based care, cultural sensitivity, interprofessional education (including team dynamics, education, and practice), preceptor-student interactions, and team practice facilities. These are critical to the development of professionalism and provide students with a platform from which to continue to build their careers.
The SEM model in this study identified some significant relationships between the latent and indicator variables and the covariates. However, the fit indices demonstrated contradictory satisfaction with the model structure and data. Most indices indicated satisfactory fit; however, the chi-square GOF test showed a significant result, which suggests poor model fit. The chi-square GOF test is sensitive to sample size and is more likely to suggest poor fit when larger sample sizes are used.41 In this analysis, we had a large sample size of 764 responses; therefore, the GOF index, the only index suggesting poor fit in this analysis, may not have been a reliable indicator of the overall model fit.
This study of the interplay of student satisfaction and stress with professionalism over time was limited to one college of pharmacy. Moreover, the design expressly did not allow for a longitudinal analysis nor control for the changes that occurred within an individual student over time. As such, the cross-sections contained many of the same student participants and likely introduced a clustering effect. We attempted to control for this by performing a multi-level analysis. Future efforts should individually track pharmacy students over their course of study and measure each of the domains. The University of Utah College of Pharmacy has a definition of professionalism which may not apply to other colleges of pharmacy. This study was not designed to assess or provide learning experiences that encouraged professionalism. However, these results may provide a better understanding of the drivers of pharmacy student professionalism. The analysis should be replicated at other institutions to determine the generalizability of our findings.
CONCLUSION
Levels of stress and satisfaction in pharmacy students about their educational experience are inversely related. Professionalism of pharmacy students is positively associated with students’ satisfaction with the program, but it is not significantly impacted by stress (after adjusting for its impact on satisfaction). Students who have positive attitudes toward community and patient-centeredness and who feel they benefit from working in a team-based environment are most likely to have greater levels of professionalism.
SURVEY AVAILABILITY
The University of Utah has developed a written agreement with any school or college of pharmacy that would like to use the questionnaire. Please contact Dr. Munger at the University Utah College of Pharmacy for details about the use of the questionnaire.
REFERENCES
- 1.Pileggi DJ, Fugit A, Romanelli F, et al. Pharmacy residents’ preparedness for emotional challenges of patient care. Am J Health-Syst Pharm. 2015;72:1475-1480. [DOI] [PubMed] [Google Scholar]
- 2.Jungnickel PW, Kelley KW, Hammer DP, Haines ST, Marlowe KF. Addressing competencies in the future in the professional curriculum. Am J Pharm Educ . 2009;73(3):Article 156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3..Thompson DF, Farmer KC, Beall DG, et al. Identifying perceptions of professionalism in pharmacy using four-frame leadership model. Am J Pharm Educ . 2008;72(4):Article 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rabi SM, Patton LR, Fjortoft N, Zgarrick DP. Characteristics, prevalence, attitudes, and perceptions of academic dishonesty among pharmacy students. Am J Pharm Educ. 2006;70(4):Article 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cruess SR, Johnson S, Cruess RL. Professionalism for medicine: opportunities and obligations. MJA 2002;177:208-211. [DOI] [PubMed] [Google Scholar]
- 6.Cruess RL. Teaching professionalism: theory, principles, and practices. Clin Orthop Relat Res . 2006;449:177-185. [DOI] [PubMed] [Google Scholar]
- 7.Cruess RL, Cruess SR, Boudreau JD, Snell I, Steinert Y. Reframing medical education to support professional identity formation. Acad Med . 2014;89:1446-1451. [DOI] [PubMed] [Google Scholar]
- 8.Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. A schematic representation of the professional identity formation and socialization of medical students and residents: a guide for medical educators. Acad Med . 2015;90(6):715-725. Doi: 10.1097/ACM.0000000000000700. [DOI] [PubMed] [Google Scholar]
- 9.Robertson K. Reflection in professional practice and education. Aust Fam Physician 2005;34(9):781-783. [PubMed] [Google Scholar]
- 10.Jha V, Bekker HL, Duffy SR, Roberts TE. A systematic review of studies assessing and facilitating attitudes towards professionalism in medicine. Med Educ . 2007;41(8):822-829. [DOI] [PubMed] [Google Scholar]
- 11.Bullen C, Neuwelt P. Educating public health physicians for the future: a current perspective from Aotearoa New Zealand. Australia and New Zealand Health Policy. 2009;6:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Connor SJ. Developing professional habitus: a Bernsteinain analysis of the modern nurse apprenticeship. Nurse Educ Today . 2007;27(7):748-754. [DOI] [PubMed] [Google Scholar]
- 13.Mann K, Gordon J, MacLeod A. Reflection and reflective practice in health professions education: a systematic review. Adv Health Sci Educ Theory Pract. 2009;14(4):595-621. [DOI] [PubMed] [Google Scholar]
- 14.DiLullo C, McGee P, Kriebel RM. Demystifying the millennial student: a reassessment in measures of character and engagement in professional education. Anat Sci Educ . 2011;4(4):214-226. Doi: 10.1002/ase.240. [DOI] [PubMed] [Google Scholar]
- 15.Parandeh A, Khaghanizade M, Mohammadi E, Mokhtari JN. Factors influencing development of professional values among nursing students and instructors: a systematic review. Glob J Health Sci . 2014;7(2):284-293. Doi: 10.5539/gjhs.v7n2p284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Munger MA, Gordon E, Hartman J, Vincent K, Feehan M. Community pharmacists’ occupational satisfaction and stress: a profession in jeopardy? J Am Pharm Assoc . 2013;53:282-296. [DOI] [PubMed] [Google Scholar]
- 17.Frick LJ, Frick JL, Coffman RE, Dey S. Student stress in a three-year doctor of pharmacy program using a mastery learning educational model. Am J Pharm Educ. 2011;75(4):Article 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galán F, Sanmartin A, Polo J, Giner L. Burnout risk in medical students in Spain using the Maslach Burnout Inventory-Student Survey. Int Arch Occup Environ Health . 2011;84(4):453-9. Doi: 10.1007/s00420-011-0623-x. [DOI] [PubMed] [Google Scholar]
- 19.Seeleman C, Hermans J, Lamkaddem M, Surrmond J, Stronks K, Essink-Bot M-L. A students’ survey of cultural competence as a basis for identifying gaps in the medical curriculum. BMC Med Educ . 2014;14:216 Doi: 10.11286/1472-6920-14-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aukes LC, Geertsma J, Cohen-Schotanus J, Zwierstra RP, Slaets JP. The development of a scale to measure personal reflection in medical practice and education. Med Teach . 2007;29(2-3):177-182. [DOI] [PubMed] [Google Scholar]
- 21.Net Promotor Score. https://www.medallia.com/net-promoter-score/. Accessed September 5, 2018.
- 22.Feehan M, Ilangakoon C, Mesure P. Three steps to clarity: a structured approach for qualitative verbatim analysis. Quirk’s Marketing Res Rev. 2010. (a);Oct:48-55. [Google Scholar]
- 23.Feehan M, Ilangakoon C, Mesure P. Keeping score: is the net promoter score a reliable tool in the global recessionary environment? Marketing Res . 2010. (b):Winter:6-10. [Google Scholar]
- 24.Campos JA, Jordani PC, Zucoloto ML, Bonafé FS, Maroco J. Burnout syndrome among dental students. Rev Bras Epidemiol . 2012;15(1):155-165. [DOI] [PubMed] [Google Scholar]
- 25.Krupat E, Putnam SM, Yeager C. The fit between doctors and patients, can it be measured? J Gen Intern Med . 1996;1(Suppl):134. [Google Scholar]
- 26.Tsimtsiou Z, Kerasidou O, Efstathiou N, Papaharitou S, Hatzimouratidis K, Hatzichristou D. Medical students’ attitudes toward patient-centered care: a longitudinal survey. Med Educ . 2007;41(2):146-153. [DOI] [PubMed] [Google Scholar]
- 27.Ross EF, Haidet P. Attitudes of physical therapy students toward patient-centered care, before and after a course in psychosocial aspects of care. Patient Educ Cons . 2011;85(3):529-532. [DOI] [PubMed] [Google Scholar]
- 28.Beattie A, Durham J, Harvey J, Steele J, McHanwell S. Does empathy change in first-year dental students? Eur J Dent Educ . 2012;16(1):e111-6. Doi: 10.1111/j.1600-0579.2011.00683.x. [DOI] [PubMed] [Google Scholar]
- 29.Norris J, Lassche M, Joan C, et al. The development and validation of the interprofessional attitudes scale: assessing the interprofessional attitudes of students in the health professions. Acad Med . 2015: 90:1394-1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lei P-W, Wu Q. Introduction to structural equation modeling: issues and practical considerations. Educ Meas Issues Pract. 2007;26(3):33-43. [Google Scholar]
- 31.Muthén LK, Muthén BO. Mplus User's Guide (1998-2017). Eighth ed. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- 32.Hu L-t and Bentler PM. Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol Meth. 1998;3(4):424-453. [Google Scholar]
- 33.Hu L-t and Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Modeling Multidisc J . 1999;6(1):1-55. [Google Scholar]
- 34.Heinen I, Bullinger M, Kocalevent R-D, et al. Perceived stress in first year medical students - associations with personal resources and emotional distress. BMC Med Educ. 2017;17(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sarson K. Medical education needs to adapt to learning styles. STAT . August 31, 2017. https://www.statnews.com/2017/08/31/medical-education-students-learning-styles/. Accessed September 5, 2018. [Google Scholar]
- 36.Marshall LL, Allison A, Nykamp D, Lanke S. Perceived stress and quality of life among doctor of pharmacy students. Am J Pharm Educ . 2008;72(6):Article 137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Desselle SP, Peirce GL, Crabtree BL, et al. Pharmacy faculty workplace issues: findings from the 2009-2010 COD-COF Joint task force on faculty workforce. Am J Pharm Educ. 2011;75(4):Article 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fight or Flight: Managing Stress in Pharmacy School https://www.pharmacist.com/article/fight-or-flight-managing-stress-pharmacy-school Accessed September 5, 2018.
- 39.Burke P. Identities and social structure: the 2003 Cooley-Mead Award Address. Soc Psychol Q . 2004;67:5-15. [Google Scholar]
- 40.Lane S. Professionalism and professional identity: what are they, and what are they to you? Australian Med Stud J. 2018;8(2):10-15 [Google Scholar]
- 41.Iacobucci D. Structural equations modeling: fit indices, sample size, and advanced topics. J Consum Psych. 2010;20:90-98. [Google Scholar]