Abstract
The ubiquitously expressed family of inward rectifier potassium (KIR) channels, encoded by KCNJ genes, is primarily involved in cell excitability and potassium homeostasis. Channel mutations associate with a variety of severe human diseases and syndromes, affecting many organ systems including the central and peripheral neural system, heart, kidney, pancreas, and skeletal muscle. A number of mutations associate with altered ion channel expression at the plasma membrane, which might result from defective channel trafficking. Trafficking involves cellular processes that transport ion channels to and from their place of function. By alignment of all KIR channels, and depicting the trafficking associated mutations, three mutational hotspots were identified. One localized in the transmembrane-domain 1 and immediately adjacent sequences, one was found in the G-loop and Golgi-export domain, and the third one was detected at the immunoglobulin-like domain. Surprisingly, only few mutations were observed in experimentally determined Endoplasmic Reticulum (ER)exit-, export-, or ER-retention motifs. Structural mapping of the trafficking defect causing mutations provided a 3D framework, which indicates that trafficking deficient mutations form clusters. These “mutation clusters” affect trafficking by different mechanisms, including protein stability.
Keywords: inward rectifier channel, trafficking, alignment, mutation, KCNJ, KIR, disease, structure
1. Introduction
Seventy years ago, Katz detected the inward rectification phenomenon for the first time [1]. Its unexpected property of conducting larger inward than outward potassium currents at similar deviations from the potassium equilibrium potential was unprecedented at that time. During the following decades, the understanding of inward rectifier channels was established further, stimulated by biophysical analysis and cloning of KIR genes. Inward rectifying channels—unlike voltage-gated potassium channels (Kv) which open in response to alterations in transmembrane electrostatic potential [2,3]—are primarily gated by intracellular substances (e.g., polyamines and Mg2+). Spermine and spermidine—two polyamines for which micromolar concentrations are sufficient to reach physiological effective levels—cause stronger block of the outward current than Mg2+. The underlying molecular mechanism of rectification was first explained by Lopatin in 1994 [3]. Polyamines enter the channel pore from the cytoplasmic side and subsequently interact with six specific residues (i.e., KIR2.1 E224, D259, E299, F254, D255 and D172) [4] in the transmembrane pore domain and its cytosolic pore extension. A similar mechanism of pore-blocking is caused by Mg2+, but weaker.
The inward rectifier channel family consists of strong and weak rectifiers. Strong rectifiers, e.g., KIR2 and KIR3, are often expressed in excitable cells such as neuronal or muscle cells. Their rectifying properties enable cells to conserve K+ during action potential formation and facilitate K+ entry upon cell hyperpolarization. In addition, they contribute to repolarization and stabilization of the resting membrane potential. For example, application of 10 µM barium, at that concentration rather specific for KIR2 channel inhibition, lengthened the action potential of guinea-pig papillary muscle preparations by 20 ms [5]. In the heart, KIR2 is strongly expressed in the ventricles and less in the atrioventricular node (AVN) [6]; KIR3 is mainly expressed in the atrium with much lower levels in the ventricle. Weak rectifier channels, e.g., KIR1, KIR4, and KIR5, are mainly associated with potassium homeostasis and often regulate extracellular potassium concentrations to allow functioning of several ion (co)transporters.
KIR channels are encoded by KCNJ genes. Various diseases associate with mutations in KCNJ genes. The aim of this review is to correlate disease associated mutations causing aberrant inward rectifier channel trafficking with protein domains important for trafficking by means of channel alignment, and finally to put mutational changes in a structural framework.
2. Classification, Structure, and Expression
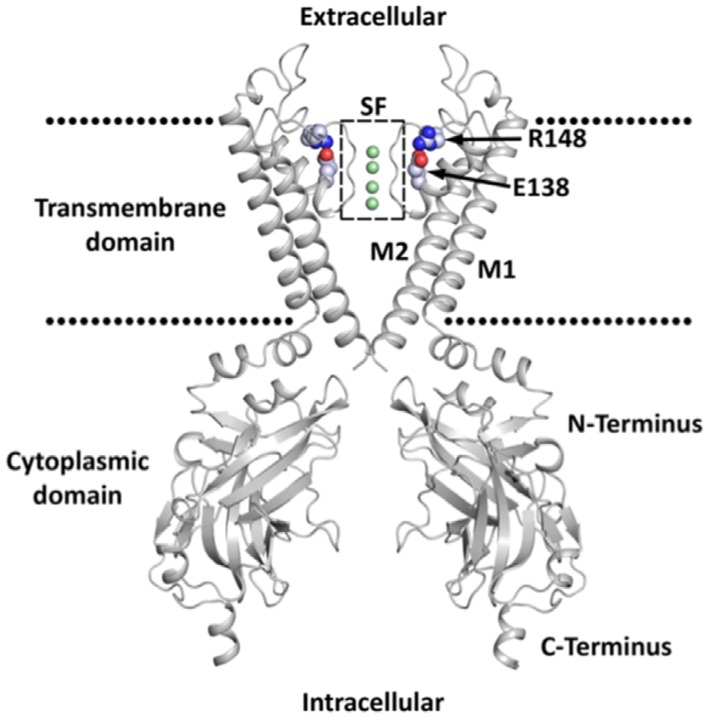
The KIR family is divided into seven subfamilies (KIR1-7) according to their amino-acid homology [4]. The sequence homology is 40% between subfamilies and rises to 70% within some subfamilies. The structural common features of these channels are that the channel pore is formed by a tetramer of subunits, most often homotetramers (Figure 1). Each subunit has two transmembrane domains (M1 and M2) which are separated by a pore-loop that contains the GYG (or GFG) potassium selectivity filter motif located close to the extracellular side of the membrane. Pore-loop stability depends strongly on one negatively and one positively charged residue, E138 and R148 respectively in KIR2.1 [7]. There is a relatively short N-terminus linked to M1 and a longer C-terminus linked to M2 which form the characteristic cytoplasmic extended pore domain (CTD). Despite their structural similarities, the KIR subfamilies also display divergent properties, e.g., sensitivity to extracellular Ba2+ or the response to regulatory signals.
Figure 1.
Two opposing domains of the KIR channel with structural common features highlighted. The membrane is indicated by dotted lines. The selectivity filter (SF) is highlighted by a dotted box. Ions inside the SF are shown as green spheres. Residues E138 and R148 (KIR2.1) are shown as spheres.
All KIR family members have a widespread expression pattern [4]. Neural tissues strongly express KIR2, KIR3, KIR4, and KIR5. Kidneys show high expression of KIR4, KIR5, and KIR6, whereas pancreatic tissue highly expresses KIR5 and KIR6. The retina shows profound expression of KIR7. The heart displays strong expression of KIR2, KIR3 and KIR6. KIR2 subfamily-members form the classical IK1 current in working ventricular and atrial cardiomyocytes, where they contribute to repolarization and resting membrane potential stability. KIR3 (IKAch) members are strongly expressed in the nodal tissues of the heart, where they are involved in heart rate regulation [8]. Further, they are widely expressed in the brain where they have numerous neurological functions [9]. KIR6 channels form octamers with the ATP/ADP sensing SUR subunits and couple cellular metabolic status to cardiac repolarization strength.
3. Channel Trafficking
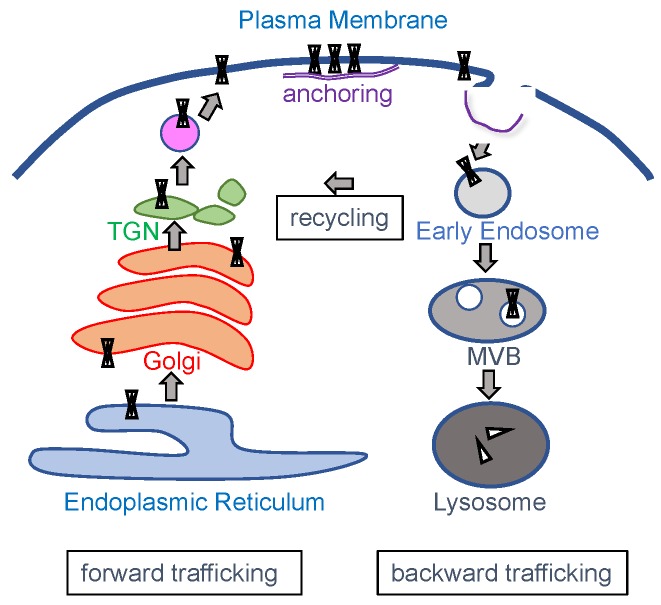
Following their translation in the endoplasmic reticulum (ER), correctly folded KIR channels are transported to the plasma membrane, a process known as forward trafficking, where they exert their main biological role (Figure 2). Upon removal from the plasma membrane, channel proteins can enter the degradation pathway in a process named backward trafficking. In addition, KIR channels can enter several recycling pathways. Each of these processes is well regulated and depends mainly on specific trafficking motifs in the channels primary sequence in concert with specific interacting proteins that direct and/or support subsequent trafficking steps. Incorrectly folded proteins will enter the endoplasmic-reticulum-associated protein degradation pathway.
Figure 2.
Schematic representation of intracellular trafficking pathways of KIR channels. TGN, trans-Golgi network; MVB, multivesicular body.
ER-export signals have been determined in several KIR channels [10,11,12,13], see also Section 5.3, with homology between subfamily members (e.g., FCYENE in KIR2.x channels), although not always among other KIR family members. Not all KIR members possess an ER-export signal, and some might even restrict forward trafficking or stimulate lysosomal breakdown when part of a heteromeric channel, as seen for KIR3.3 [12]. Other channels even have ER-retention signals that only become masked upon proper channel assembly, as seen for the KIR6 family [13].
Trans-Golgi transport of several KIR channels has been demonstrated to depend on interaction with Golgin tethers that reside in the trans-Golgi network. For example, Golgin-160 interacts with the C-terminal domain of KIR1.1 channels which results in increased forward trafficking and an increase in KIR1.1 currents [14]. In a similar fashion, Golgin-97 was shown to interact with the C-terminus of KIR2.1 and promotes transport to the Golgi-export sites [15]. Golgi-export signals have been characterized in a few KIR channels [16,17]. By a combination of cytoplasmic N- and C-terminal domains, a so-called Golgi-export signal patch is formed that interacts with the AP-1 clathrin adaptor protein.
Protein motifs involved in backward trafficking have been studied less. KIR1.1 internalization depends on clathrin-dynamin mediated endocytosis which involved N375 in the KIR1.1 putative internalization motif NPN [18]. Internalized KIR1.1 channels depend on CORVET and ESCRT protein complexes for subsequent trafficking to the early endosome and the multivesicular body that eventually fuses with the lysosome, respectively [19]. KIR2.1 channels are regulated by the ESCRT machinery also [20]. It was demonstrated, by a pharmacological approach, that KIR2.1 degradation also depends on clathrin mediated endocytosis and lysosomal activity, and their inhibition resulted in enhanced IK1 currents [21,22]. The TPVT motif of the KIR5.1 channel protein binds the Nedd4-2 E3 ubiquitin ligase. In KIR5.1/KIR4.1 heteromeric complexes, this was suggested to result in ubiquitination and subsequent degradation of KIR4.1 in the proteasome [23].
Finally, trafficking, anchoring and plasma membrane localization of KIR channels is regulated by their interaction with scaffolding proteins. The C-terminal KIR2.2 SEI PDZ-binding domain interacts with SAP97, PSD-95, Chapsyn-110, SAP102, CASK, Dlg2, Dlg3, Pals2, Veli1, Veli3, Mint1, and abLIM from rat brain lysates, and SAP97, CASK, Veli-3, and Mint1 from rat heart lysates [24,25,26]. Additionally, interactions between syntrophins, dystrobrevins and the KIR2.2 PDZ domain were shown by these authors. KIR2.1 and KIR2.3 also interact with SAP97 in the heart. Using an NMR approach, it was found that additional residues close to the KIR2.1 PDZ domain were involved in PSD-95 interaction [27]. Furthermore, PSD-95 interacts with KIR4.1 and KIR5.1 in the optic nerve and brain, and PSD-95 interaction is essential for KIR5.1 expression at the plasma membrane of HEK293 cells [28,29]. The C-terminal PDZ-binding motif SNV interacts with PSD-95, and KIR4.1 mediated current density more than doubled upon PSD-95 cotransfection in HEK293 cells, and increased even threefold upon SAP97 cotransfection [30]. Upon silencing of SAP97, the IK1 current decreased due to reduced plasma membrane expression of KIR2.1 and KIR2.2 ion channels [31]. Residues 307–326 of KIR2.1 are involved in interactions with the actin binding protein filamin A. Interestingly, these interactions are unaffected by the Andersen–Tawil deletion Δ314/315 [32]. In arterial smooth muscle cells, filamin A and KIR2.1 colocalize in specific regions of the plasma membrane. Although filamin A is not essential for KIR2.1 trafficking to the plasma membrane, its absence reduces the amount of KIR2.1 channels present at the plasma membrane [32].
Whereas this research field provided many new insights during the last two decades, one has to emphasize that no complete trafficking pathway for any KIR channel protein has been deciphered in detail yet. Furthermore, most of our current knowledge is derived from ectopic expressions systems rather than human native tissue or cells. Currently, we cannot exclude that KIR subtype and/or tissue specific pathways exist. The observations that several diseases associate with KIR channel trafficking malfunction might help us to further understand KIR protein trafficking processes in their natural environments in vivo.
4. Diseases and Syndromes Associated with KIR Channel Dysfunction
A number of human diseases associate with mutations in KIR channels, as indicated in Table 1. Bartter syndrome type II is a salt-losing nephropathy resulting in hypokalemia and alkalosis associated with loss-of-function mutations in KIR1.1 channel proteins. KIR1.1 channels are essential for luminal extrusion of K+ in the thick ascending limb of Henle’s loop, thereby permitting continued activity of the NKCC2 cotransporter important for sodium resorption [33]. Loss-of-function in KIR2.1 causes Andersen–Tawil syndrome characterized by periodic skeletal muscle paralysis, developmental skeletal abnormalities, as well as biventricular tachycardia with or without the presence of long QT. On the other hand, KIR2.1 gain-of-function mutations result in cardiac phenotypes, atrial fibrillation and short QT syndrome, explained by increased repolarization capacity and thus shortened cardiac action potentials [34,35]. Thyrotoxic hypokalemic periodic paralysis associated with KIR2.6 loss-of-function mutations affect skeletal muscle excitability under thyrotoxic conditions [36]. Keppen–Lubinsky syndrome is an extremely rare condition associated with KIR3.2 gain-of-function mutations. Its phenotype encompasses lipodystrophy, hypertonia, hyperreflexia, developmental delay and intellectual disability [37,38]. Familial hyperaldosteronism type III is associated with loss-of-function mutations in KIR3.4 channel proteins. The disease is characterized by early onset of severe hypertension and hypokalemia. Mutant KIR3.4 channels lack potassium specificity and the resulting inflow of Na+ and accompanying cell depolarization of zona glomerulosa cells increases intracellular Ca2+ concentrations, which activates transcription pathways that raise aldosterone production [39]. Loss-of-function mutations in KIR3.4 associate with long QT syndrome 13, which indicates that these acetylcholine activated channels, mostly known from nodal tissues, also play a role in ventricular repolarization processes [40]. EAST (epilepsy, ataxia, sensorineural deafness, tubulopathy)/SeSAME syndrome is a salt-losing nephropathy combined with severe neurological disorders. The disease associated loss-of-function mutations in KIR4.1 channels expressed in the distal convoluted tubule, result in hypokalemic metabolic acidosis. Impaired KIR4.1 function in glial cells will increase neural tissue potassium levels giving rise to neuron depolarization, whereas reduced potassium concentration in the endolymph affect cochlear hair cell function [41]. Cantú syndrome results from gain-of-function of IKATP channels, either due to mutation in KIR6.1 or the SUR2 subunits. Many of these mutations decrease the sensitivity of the channel to ATP-dependent closure [42]. Insulin release by pancreatic beta-cells is regulated by their membrane potential and L-type Calcium channel activity. Depolarization activates Ca2+ influx inducing insulin release from intracellular stores into the extracellular fluid. Loss-of-function mutations in KIR6.2 result in membrane depolarization and thus insulin release and associate with hyperinsulism and hypoglycemia. Gain-of-function mutations on the other hand impair insulin release and associate with different forms of diabetes [43]. KIR7.1 channels are expressed in the apical membrane of retinal pigmented epithelial cells and contribute to K+ homeostasis in the subretinal space. Loss-of-function mutations in KIR7.1 associate with retinal dysfunction observed in Lever congenital amaurosis type 16 and Snowflake vitreoretinal degeneration [44].
Table 1.
Human diseases associated with abnormal KIR channel function.
| Protein | Gene | Syndrome/Disease Character (OMIM)1 | Main Affected System(s) | Recent Review |
|---|---|---|---|---|
| KIR1.1 | KCNJ1 | Bartter syndrome, type 2 (241200) | Kidney; head; face; ear; eye; vascular; gastrointestinal; skeleton; skeletal muscle; CNS; platelets | [33] |
| KIR2.1 | KCNJ2 | Andersen syndrome (170390) Familial atrium fibrillation 9 (613980) Short QT syndrome 3 (609622) |
Head; face; ear; eye; teeth; heart; skeleton; CNS | [34,35] |
| KIR2.2 | KCNJ12 | Non-described | ||
| KIR2.3 | KCNJ4 | Non-described | ||
| KIR2.4 | KCNJ14 | Non-described | ||
| KIR2.6 | KCNJ18 | Thyrotoxic hypokalemic periodic paralysis (613239) | Cardiovascular; skeletal muscle; CNS; eye | [36] |
| KIR3.1 | KCNJ3 | Non-described | ||
| KIR3.2 | KCNJ6 | Keppen–Lubinsky Syndrome (614098) | CNS; head; skin; skeleton; eye, face | No review available |
| KIR3.3 | KCNJ9 | Non-described | ||
| KIR3.4 | KCNJ5 | Familial hyperaldosteronism 3 (613677) Long QT syndrome 13 (613485) |
Cardiovascular; kidney; skeletal muscle | [39,40] |
| KIR4.1 | KCNJ10 | Digenic enlarged vestibular aqueduct (600791) EAST/SESAME syndrome (612780) |
Ear (hearing); vascular; kidney; CNS | [41] |
| KIR4.2 | KCNJ15 | Non-described | ||
| KIR5.1 | KCNJ16 | Non-described | ||
| KIR6.1 | KCNJ8 | Cantú syndrome (239850) | Head; face; cardiovascular; skeleton; hair; CNS | [42] |
| KIR6.2 | KCNJ11 | Transient neonatal diabetes mellitus 3 (610582) Permanent neonatal diabetes with or without neurologic features (606176) Familial hyperinsulinemic hypoglycemia 2 (601820) Maturity-onset diabetes of the young 13 (616329) Susceptible to diabetes mellitus 2 (125853) |
Pancreas (beta-cells); CNS | [43] |
| KIR7.1 | KCNJ13 | Leber congenital amaurosis 16 (614186) Snowflake vitreoretinal degeneration (193230) |
Eye (retina) | [44] |
OMIM1: OMIM®—Online Mendelian Inheritance in Man® https://omim.org assessed on 24 July 2019, CNS, central neural system.
In many of the above-mentioned diseases, loss-of-function has been associated with aberrant trafficking, most likely forward trafficking. Nonetheless, enhanced backward trafficking or impaired plasma-membrane anchoring cannot be excluded. However, most gain-of-function mutations are likely not related to trafficking abnormalities. Loss-of-specificity mutations, as seen in some KIR3.4 mutations, neither result from trafficking issues.
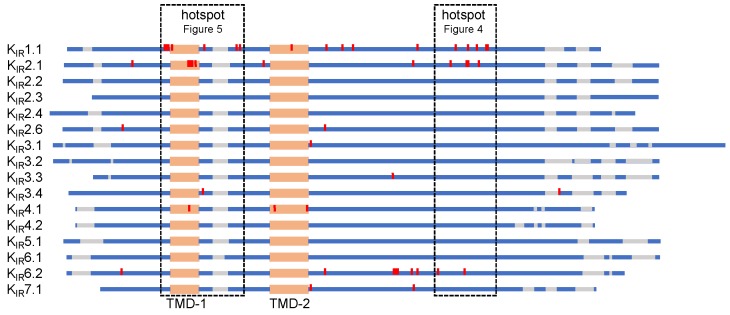
5. KIR Protein Alignment of Trafficking Associated Disease Mutations
In order to identify potential protein domains associated with KIR trafficking defects in human disease, we aligned all KIR isoforms and highlighted residues (in red) of which the mutations are experimentally proven to associate with trafficking defects (Figure 3, Supplementary Figure S1). Furthermore, additional mutations in other KIR isoforms at homologues positions, but currently not related to impaired trafficking, are indicated (Supplementary Figure S1, in green). Trafficking associated mutations are found dispersed along the protein sequence, with one “hotspot” in the G-loop and adjacent C-terminal region, and one “hotspot” in and around transmembrane domain 1. Additionally, from a structural point of view, there is another “hotspot” at the immunoglobulin-like domain (IgLD), which is described in Section 6.1.
Figure 3.
Schematic representation of inward rectifier channels (KIR1–7) sequence alignment. Red: mutations associated with aberrant trafficking; mutation hotspots are boxed. Orange: transmembrane domain; blue: KIR protein sequence; gray: sequence gap.
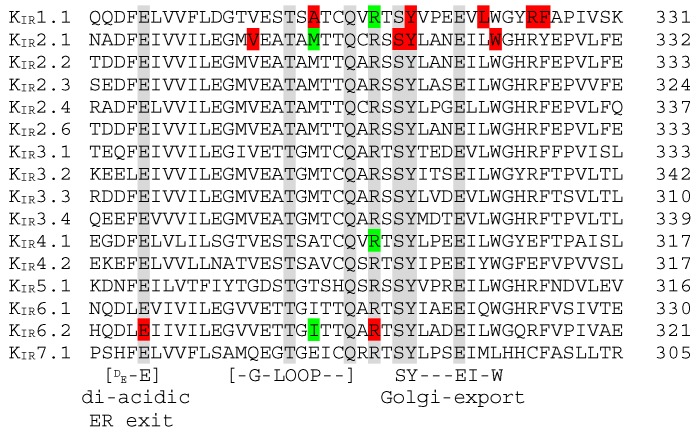
5.1. C-Terminal Trafficking Mutation Hotspot
Figure 4 depicts the alignment of the C-terminal hotspot, having ten trafficking associated mutations/deletions located in KIR1.1, KIR2.1 and/or KIR6.2 over a stretch of 44 residues. This region also covers the filamin A interaction domain of KIR2.1 (307–326) [32]. The loss-of-function E282K mutation in KIR6.2 is associated with congenital hyperinsulinism [45]. This mutation affects normal function of a highly conserved di-acidic ER exit signal (DxE) that prevents mutant channels to enter ER exit sites, which thus fail to traffic to the plasma membrane [45]. The Andersen–Tawil loss-of-function KIR2.1 mutation V302M is located in the G-loop and displays intracellular, but no plasma-membrane expression, upon transfection of HEK293 cells [46]. However, Ma et al., [47] demonstrated that the KIR2.1 V302M mutation does not affect trafficking. The Bartter syndrome associated loss-of-function A306T mutation in KIR1.1 is also located in the G-loop. Its expression in the Xenopus oocyte membrane is strongly reduced compared to wildtype channels [48]. At homologues positions, disease causing mutations have been found in KIR2.1 [49] and KIR6.2 [50] whose cause for loss- and gain-of-function, respectively, is unknown but may be caused by trafficking abnormalities. Hyperinsulinism associated KIR6.2 R301H/G/C/P loss-of-function mutations are located just C-terminal from the G-loop domain. These mutants display reduced surface expression when expressed in COSm6 or INS cells [51]. Interestingly, however, the R301A mutation displays normal expression at the plasma membrane [51]. At homologues positions, mutations have also been found in KIR1.1 [52] and KIR4.1 [53].
Figure 4.
KIR1–7 sequence alignment of the C-terminal mutation hotspot. Red: Mutations associated with aberrant trafficking; Green: Residues whose mutations are currently not related to impaired trafficking. Numbers at the right refer to the last amino-acid residue in the respective sequence shown. Conserved residues among all KIR members are shaded gray. Locations of the di-acidic ER exit, G-loop and the Golgi-Export signal sequence (see text) are indicated below the alignment.
By use of homology comparison and structure guided mutagenesis, a common Golgi-export signal patch was found to be formed by a C-terminal stretch of hydrophobic residues and basic residues from the N-terminus [16,17]. The C-terminal stretch sequence is formed by residues SYxxxEIxW indicated in Figure 4. Two Bartter syndrome associated KIR1.1 (Y314C; L320P) and two Andersen–Tawil syndrome associated KIR2.1 (delSY; W322S) confirmed trafficking mutations have been described in this region [46,48,54]. Interestingly, the W residue is not conserved in the KIR7.1 channel protein, which may indicate KIR subtype specific use of the entire Golgi-export signal motif. Two additional KIR1.1 mutations leading to altered trafficking, R324L and F325C have been located directly C-terminal from the Golgi-export signal stretch [48,52].
Fallen et al. [55] showed that mutations A198T and Y314C in the IgLD, located in the CTD of KIR1.1, are associated with defects in channel trafficking and gating, see also Section 6.1. Y314C is present within the C-terminal trafficking mutation hotspot and part of the Golgi-export signal as discussed above. If incorrectly folded, the aberrant KIR1.1 proteins will enter the endoplasmic-reticulum-associated protein degradation pathway [56].
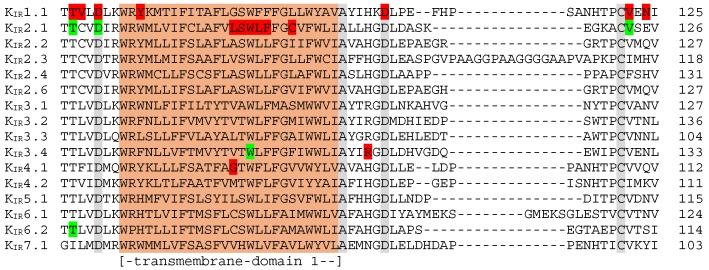
5.2. Transmembrane Region 1 Mutation Hotspot
Figure 5 depicts the alignment of transmembrane domain 1 and adjacent sequences, containing 15 trafficking associated mutations located in KIR1.1, KIR2.1, KIR3.4 or KIR4.1. Three mutations in the cytoplasmic domain, positioned just in front of the first transmembrane region in KIR1.1 (T71M, V72M and D74Y), have been demonstrated to strongly decrease plasma-membrane expression and mutant channels were retained in the cytoplasm [48,57]. However, membrane expression of T71M in Xenopus oocytes could be rescued by increasing the amount of injected RNA, in contrast to the other two mutations. For KIR1.1 T71M, mutations at the homologues positions were found in KIR2.1 (T75) [58,59,60,61,62] and KIR6.2 (T62) [63,64] associated with Andersen–Tawil syndrome and Familial hyperinsulinemic hypoglycemia type 2, respectively. The KIR2.1 T75R protein was observed at the plasma membrane upon overexpression in HL1 cells [60]. Moreover, T75A, T75R and T75M channel proteins were also expressed at the plasma membrane in Xenopus oocytes, HEK293 or COS-7 cells [58,61,65]. In contrast, impaired plasma-membrane localization of T75M KIR2.1 was observed in HEK293 cells in another study [62]. Two KIR2.1 mutations, i.e., D78G and D78Y, are at the equivalent position as D74 in KIR1.1, and also D78Y was found at the plasma membrane in Xenopus oocytes and HEK293 cells [59,65,66]. These comparisons indicate that findings on plasma-membrane expression may be influenced by the degree of overexpression and cell type. KIR2.1 T75 and D78 residues are positioned on the hydrophilic side of the slide helix that interacts with the cytoplasmic domain. The D78Y mutation disrupts this interaction [65].
Figure 5.
KIR1–7 sequence alignment of the transmembrane domain 1 mutation hotspot. Red: mutations associated with aberrant trafficking; Green: residues whose mutations are currently not related to impaired trafficking. Numbers at the right refer to the last amino-acid residue in the respective sequence shown. Conserved residues among all KIR members are shaded gray. Location of the transmembrane domain 1 (orange) is indicated below the alignment.
Trafficking associated mutations in the highly conserved transmembrane region 1 are described for KIR1.1, KIR2.1 and KIR4.1 [46,48,67,68,69]. Expression of KIR1.1 Y79H in the Xenopus oocyte plasma-membrane increases upon increasing the amount of RNA injection by ten-fold [48]. The KIR2.1 L94P, Δ95-98 and KIR4.1 G77R channel proteins localize intracellularly [46,68,69]. The molecular mechanisms by which these mutations affect normal trafficking remain to be solved. However, interactions with wildtype subunits appear not to be affected and may explain the dominant negative properties of these mutations. The familial sinus node disease associated KIR3.4 W101C gain-of-function mutation is located at a position homologues to KIR2.1 W96 [70]. In an ectopic expression system, the KIR3.4 W101C protein is expressed at the plasma membrane, however it decreased surface expression of KIR3.1 when co-expressed [70].
Confirmed trafficking associated mutations C-terminal from the transmembrane region 1 are found in KIR1.1 and KIR3.4 [48,71,72]. KIR1.1 D108H and V122E mutants did not display membrane staining in Xenopus oocytes or HEK293 cells [48]. When comparing single channel characteristics with macroscopic currents, it was concluded that loss-of-function of KIR1.1 N124K was caused by a reduction of functional channels at the plasma membrane [71]. The KIR3.4 R115W mutation was obtained from aldosterone-producing adenoma linked to hyperaldosteronism, and displayed decreased plasma-membrane expression in HEK293 cells [72]. A mutation, at a position homologues to V122 in KIR1.1, has also been identified in KIR2.1 [59].
5.3. N-Terminal Golgi-Export Patch, KIR2.x ER Export, and KIR6.x ER Exit and Retention Signals
As indicated above, the so-called Golgi-export patch consists of interaction of a C-terminal and N-terminal domain [16,17]. Mutations in the C-terminal domain have been found (see Section 5.1). However, only few mutations have been described in the N-terminal part (KIR2.1 G52V; KIR2.6 R43C) that result in reduced plasma membrane expression by hampering Golgi export [73,74]. Thus far, no mutations of residue R20 in KIR2.3, which is required for Golgi export [17], or at the homologues position in any other KIR channel protein have been identified.
KIR2.x channels share a short C-terminal ER-export signal (FCYENE) [10,11]. KIR3.2 contains N-terminal (DQDVESPV) and C-terminal (ELETEEEE) ER-export signals, whereas KIR3.4 possesses the N-terminal NQDMEIGV ER-export signal [12]. Remarkable, we did not encounter any trafficking associated mutations in any of these domains. In contrast, one mutation (E282K) was present in the di-acidic ER exit signal of KIR6.2 as discussed in Section 5.1. KIR6.x and SURx channel proteins contain a C-terminal ER-retention signal (RKR) [13]. Upon channel assembly, retention signals from both proteins are shielded, supporting subsequent ER-export. No trafficking associated mutations were found in these retention signals in KIR6.x channel proteins.
We therefore propose that mutations in Golgi-export domains have more severe clinical implications than mutations in ER-export/retention signals.
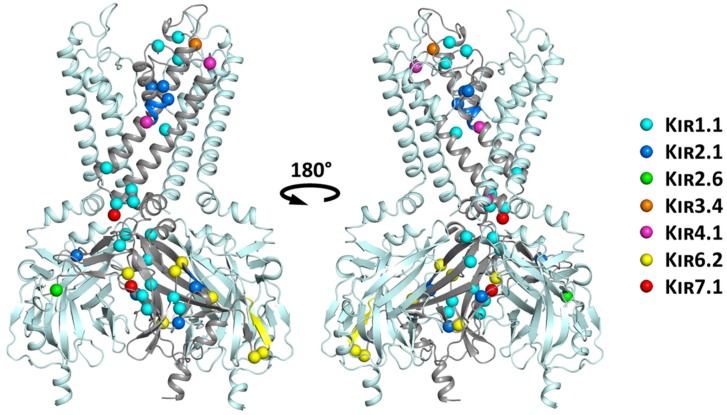
6. Structural Mapping of Trafficking Defect Causing Mutants
Disease causing mutations associated with trafficking deficiencies were mapped onto the common structural scaffold of a recently published high resolution KIR2.2 structure [75]. As illustrated in Figure 6, mutations are globally distributed.
Figure 6.
Structural mapping of trafficking mutants mapped on the KIR2.2 structure. For clarity reasons, only three of the four subunits are shown in side view, with the disease associated mutations highlighted in one subunit only. Mutations of different KIR channel family members are color-coded and shown as spheres of their respective Cα atoms. Deletions are indicated by colored regions on the secondary structure elements.
A group of mutations clusters at regions important for channel gating, including the PIP2 binding site (T71M, V72E, D74Y and Y79H in KIR1.1), the helix bundle crossing gate (A167V in KIR4.1; R162W/Q in KIR7.1) [76,77,78], as well as the G-loop gate (V302M, KIR2.1). It can be expected that these mutations have strong effects on the conformational equilibrium, thereby impairing normal protein function. It is likely that these mutants lead to structurally less-stable proteins, thereby making them more susceptible for degradation. Interestingly, 58% of the currently known trafficking defect causing mutations in KIR channel proteins cluster in the cytoplasmic domain, which has been shown to be crucial for efficient folding in KvAP channels [79].
Another cluster of mutants (D108H, V122E and N124K in KIR1.1; R115W in KIR3.4; C140R in KIR4.1) is found on surface exposed loops of the channel. Except for C140R in KIR4.1 [68], which is part of a disulfide bridge [80], none of the mutations causes changes in polarity or is at important structural motifs, leaving it unclear why these mutants cause trafficking defects.
Mutations G77R in KIR4.1 [68] and C101R in KIR2.1, located on the membrane facing side and near the center of transmembrane helix M1, cause changes in the helical properties and hydrophobicity. It is thus conceivable that they severely affect helical stability and possibly membrane insertion. It has been shown in numerous studies that the cost for exposing arginine to lipid hydrocarbons is prohibitively high [81]. Interestingly, none of the identified disease mutations is located at the interface between subunits.
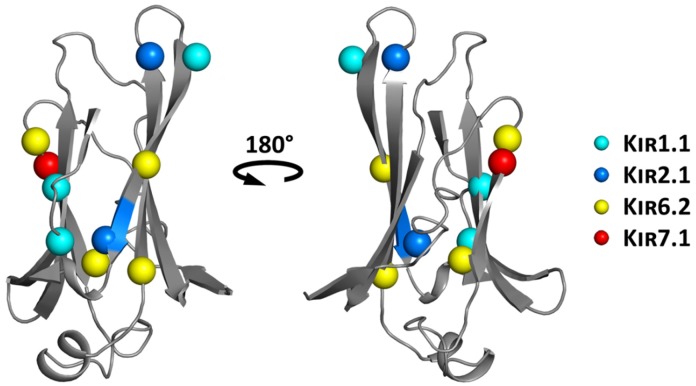
6.1. Structure-Based Hotspot in the IgLD Beta Barrel of the CTD
Two antenatal Bartter syndrome loss-of-function mutations A198T and Y314C, located in the IgLD have been shown to impair forward trafficking and gating of KIR1.1 channels, possibly influencing the core stability of this domain [55]. Interestingly, a trafficking affecting mutation in a homologous position to KIR1.1 A198 has been identified in KIR2.6 (A200P) [74], and another mutation thus far not associated with trafficking has been identified in KIR6.2 (A187V). As shown in Figure 7, quite a large number of disease causing mutations, including A306T (implicated in trafficking) [48], R311W and L320P in KIR1.1 (no data on trafficking), S314-Y315 deletion in KIR2.1 (implicated in trafficking) [16], E282K (prevents ER-export and surface expression of the channel) [45] or L241P in KIR7.1 (implicated in trafficking) [78], have been reported in the literature. This, as well as previous work [55], suggests that this structural motif might be a crucial hotspot implicated in trafficking of KIR channels.
Figure 7.
Structure-based IgLD hotspot (mapped on the KIR2.2 structure), with disease associated mutations highlighted. Mutations of the different family members are color-coded and shown as spheres of their respective Cα atoms.
7. Conclusions
Mutations in KIR potassium ion channels associate with a variety of human diseases in which electrophysiological and potassium homeostasis aberrations are explaining etiology. Many of the mutations associate with abnormal, mostly decreased forward, ion channel trafficking. Trafficking associated mutations are present throughout the primary sequence, but they concentrate in cytoplasmic domains in which channel structures involved in Golgi-export are clinically more important than ER-export regions. Another group of mutations are found in regions important for gating and most likely affect protein folding and stability. Therefore, mutation associated KIR trafficking defects are likely caused by 1) defective interaction with the trafficking machinery due to mutations in specific trafficking motifs, and 2) channel misfolding, destabilization and subsequent endoplasmic-reticulum-associated protein degradation due to mutations in residues important for channel structure.
Supplementary Materials
The following are available online at https://www.mdpi.com/2218-273X/9/11/650/s1, Figure S1: KIR1-7 sequence alignment.
Author Contributions
M.A.G.v.d.H. and A.S.-W. conceptualized the idea. E.-M.Z.-P., M.Q., M.B., A.S.-W. and M.A.G.v.d.H. wrote, edited and reviewed the manuscript. E.-M.Z.-P. and M.A.G.v.d.H. prepared the figures. M.A.G.v.d.H. coordinated the writing up and the submission process. E.-M.Z.-P., M.Q., M.B., A.S.-W. and M.A.G.v.d.H. approved the final version for submission. Funding acquisition by M.Q. and M.A.G.v.d.H.
Funding
Muge Qile was funded by Chinese Scholarship Council.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Katz B. Les constantes électriques de la membrane du muscle. Arch. Sci. Physiol. 1949;2:285–299. [Google Scholar]
- 2.Matsuda H., Saigusa A., Irisawa H. Ohmic conductance through the inwardly rectifying K channel and blocking by internal Mg2+ Nature. 1987;325:156–159. doi: 10.1038/325156a0. [DOI] [PubMed] [Google Scholar]
- 3.Lopatin A.N., Makhina E.N., Nichols C.G. Potassium channel block by cytoplasmic polyamines as the mechanism of intrinsic rectification. Nature. 1994;372:366–369. doi: 10.1038/372366a0. [DOI] [PubMed] [Google Scholar]
- 4.De Boer T.P., Houtman M.J., Compier M., Van der Heyden M.A. The mammalian KIR2. x inward rectifier ion channel family: Expression pattern and pathophysiology. Acta Physiol. 2010;199:243–256. doi: 10.1111/j.1748-1716.2010.02108.x. [DOI] [PubMed] [Google Scholar]
- 5.Wang L., Chiamvimonvat N., Duff H.J. Interaction between selected sodium and potassium channel blockers in guinea pig papillary muscle. J. Pharmacol. Exp. Ther. 1993;264:1056–1062. [PubMed] [Google Scholar]
- 6.Kokubun S., Nishimura M., Noma A., Irisawa H. Membrane currents in the rabbit atrioventricular node cell. Pflügers Arch. 1982;393:15–22. doi: 10.1007/BF00582385. [DOI] [PubMed] [Google Scholar]
- 7.Yang J., Yu M., Jan Y.N., Jan L.Y. Stabilization of ion selectivity filter by pore loop ion pairs in an inwardly rectifying potassium channel. Proc. Natl. Acad. Sci. USA. 1997;94:1568–1572. doi: 10.1073/pnas.94.4.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krapivinsky G., Gordon E.A., Wickman K., Velimirović B., Krapivinsky L., Clapham D.E. The G-protein-gated atrial K+ channel IKACh is a heteromultimer of two inwardly rectifying K+-channel proteins. Nature. 1995;374:135–141. doi: 10.1038/374135a0. [DOI] [PubMed] [Google Scholar]
- 9.Lüscher C., Slesinger P.A. Emerging roles for G protein-gated inwardly rectifying potassium (GIRK) channels in health and disease. Nat. Rev. Neurosci. 2010;11:301–315. doi: 10.1038/nrn2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma D., Zerangue N., Lin Y.F., Collins A., Yu M., Jan Y.N., Jan L.Y. Role of ER export signals in controlling surface potassium channel numbers. Science. 2001;291:316–319. doi: 10.1126/science.291.5502.316. [DOI] [PubMed] [Google Scholar]
- 11.Stockklausner C., Ludwig J., Ruppersberg J.P., Klöcker N. A sequence motif responsible for ER export and surface expression of Kir2.0 inward rectifier K+ channels. FEBS Lett. 2001;493:129–133. doi: 10.1016/S0014-5793(01)02286-4. [DOI] [PubMed] [Google Scholar]
- 12.Ma D., Zerangue N., Raab-Graham K., Fried S.R., Jan Y.N., Jan L.Y. Diverse trafficking patterns due to multiple traffic motifs in G protein-activated inwardly rectifying potassium channels from brain and heart. Neuron. 2002;33:715–729. doi: 10.1016/S0896-6273(02)00614-1. [DOI] [PubMed] [Google Scholar]
- 13.Zerangue N., Schwappach B., Jan Y.N., Jan L.Y. A new ER trafficking signal regulates the subunit stoichiometry of plasma membrane K(ATP) channels. Neuron. 1999;22:537–548. doi: 10.1016/S0896-6273(00)80708-4. [DOI] [PubMed] [Google Scholar]
- 14.Bundis F., Neagoe I., Schwappach B., Steinmeyer K. Involvement of Golgin-160 in cell surface transport of renal ROMK channel: Co-expression of Golgin-160 increases ROMK currents. Cell Physiol. Biochem. 2006;17:1–12. doi: 10.1159/000091454. [DOI] [PubMed] [Google Scholar]
- 15.Taneja T.K., Ma D., Kim B.Y., Welling P.A. Golgin-97 Targets Ectopically Expressed Inward Rectifying Potassium Channel, Kir2.1, to the trans-Golgi Network in COS-7 Cells. Front. Physiol. 2018;9:1070. doi: 10.3389/fphys.2018.01070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma D., Taneja T.K., Hagen B.M., Kim B.Y., Ortega B., Lederer W.J., Welling P.A. Golgi export of the Kir2.1 channel is driven by a trafficking signal located within its tertiary structure. Cell. 2011;145:1102–1115. doi: 10.1016/j.cell.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li X., Ortega B., Kim B., Welling P.A. A Common Signal Patch Drives AP-1 Protein-dependent Golgi Export of Inwardly Rectifying Potassium Channels. J. Biol. Chem. 2016;291:14963–14972. doi: 10.1074/jbc.M116.729822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zeng W.Z., Babich V., Ortega B., Quigley R., White S.J., Welling P.A., Huang C.L. Evidence for endocytosis of ROMK potassium channel via clathrin-coated vesicles. Am. J. Physiol. Renal Physiol. 2002;283:630–639. doi: 10.1152/ajprenal.00378.2001. [DOI] [PubMed] [Google Scholar]
- 19.Mackie T.D., Kim B.Y., Subramanya A.R., Bain D.J., O’Donnell A.F., Welling P.A., Brodsky J.L. The endosomal trafficking factors CORVET and ESCRT suppress plasma membrane residence of the renal outer medullary potassium channel (ROMK) J. Biol. Chem. 2018;293:3201–3217. doi: 10.1074/jbc.M117.819086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kolb A.R., Needham P.G., Rothenberg C., Guerriero C.J., Welling P.A., Brodsky JL. ESCRT regulates surface expression of the Kir2.1 potassium channel. Mol. Biol. Cell. 2014;25:276–289. doi: 10.1091/mbc.e13-07-0394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jansen J.A., de Boer T.P., Wolswinkel R., van Veen T.A., Vos M.A., van Rijen H.V.M., van der Heyden M.A.G. Lysosome mediated Kir2.1 breakdown directly influences inward rectifier current density. Biochem. Biophys. Res. Commun. 2008;367:687–692. doi: 10.1016/j.bbrc.2007.12.168. [DOI] [PubMed] [Google Scholar]
- 22.Varkevisser R., Houtman M.J., Waasdorp M., Man J.C., Heukers R., Takanari H., Tieland R.G., van Bergen En Henegouwen P.M., Vos M.A., van der Heyden M.A. Inhibiting the clathrin-mediated endocytosis pathway rescues K(IR)2.1 downregulation by pentamidine. Pflugers Arch. 2013;465:247–259. doi: 10.1007/s00424-012-1189-5. [DOI] [PubMed] [Google Scholar]
- 23.Wang M.X., Su X.T., Wu P., Gao Z.X., Wang W.H., Staub O., Lin D.H. Kir5.1 regulates Nedd4-2-mediated ubiquitination of Kir4.1 in distal nephron. Am. J. Physiol. Renal Physiol. 2018;315:F986–F996. doi: 10.1152/ajprenal.00059.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leonoudakis D., Mailliard W., Wingerd K., Clegg D., Vandenberg C. Inward rectifier potassium channel Kir2.2 is associated with synapse-associated protein SAP97. J. Cell Sci. 2001;114:987–998. doi: 10.1242/jcs.114.5.987. [DOI] [PubMed] [Google Scholar]
- 25.Leonoudakis D., Conti L.R., Radeke C.M., McGuire L.M., Vandenberg C.A. A multiprotein trafficking complex composed of SAP97, CASK, Veli, and Mint1 is associated with inward rectifier Kir2 potassium channels. J. Biol. Chem. 2004;279:19051–19063. doi: 10.1074/jbc.M400284200. [DOI] [PubMed] [Google Scholar]
- 26.Leonoudakis D., Conti L.R., Anderson S., Radeke C.M., McGuire L.M., Adams M.E., Froehner S.C., Yates J.R., 3rd, Vandenberg C.A. Protein trafficking and anchoring complexes revealed by proteomic analysis of inward rectifier potassium channel (Kir2.x)-associated proteins. J. Biol. Chem. 2004;279:22331–22346. doi: 10.1074/jbc.M400285200. [DOI] [PubMed] [Google Scholar]
- 27.Pegan S., Tan J., Huang A., Slesinger P.A., Riek R., Choe S. NMR studies of interactions between C-terminal tail of Kir2.1 channel and PDZ1,2 domains of PSD95. Biochemistry. 2007;46:5315–5322. doi: 10.1021/bi062228q. [DOI] [PubMed] [Google Scholar]
- 28.Brasko C., Hawkins V., De La Rocha I.C., Butt A.M. Expression of Kir4.1 and Kir5.1 inwardly rectifying potassium channels in oligodendrocytes, the myelinating cells of the CNS. Brain Struct. Funct. 2017;222:41–59. doi: 10.1007/s00429-016-1199-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tanemoto M., Fujita A., Higashi K., Kurachi Y. PSD-95 mediates formation of a functional homomeric Kir5.1 channel in the brain. Neuron. 2002;34:387–397. doi: 10.1016/S0896-6273(02)00675-X. [DOI] [PubMed] [Google Scholar]
- 30.Horio Y., Hibino H., Inanobe A., Yamada M., Ishii M., Tada Y., Satoh E., Hata Y., Takai Y., Kurachi Y. Clustering and enhanced activity of an inwardly rectifying potassium channel, Kir4.1, by an anchoring protein, PSD-95/SAP90. J. Biol. Chem. 1997;272:12885–12888. doi: 10.1074/jbc.272.20.12885. [DOI] [PubMed] [Google Scholar]
- 31.Vaidyanathan R., Taffet S.M., Vikstrom K.L., Anumonwo J.M. Regulation of cardiac inward rectifier potassium current (I(K1)) by synapse-associated protein-97. J. Biol. Chem. 2010;285:28000–28009. doi: 10.1074/jbc.M110.110858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sampson L.J., Leyland M.L., Dart C. Direct interaction between the actin-binding protein filamin-A and the inwardly rectifying potassium channel, Kir2.1. J. Biol. Chem. 2003;278:41988–41997. doi: 10.1074/jbc.M307479200. [DOI] [PubMed] [Google Scholar]
- 33.Seyberth H.W., Weber S., Kömhoff M. Bartter’s and Gitelman’s syndrome. Curr. Opin. Pediatr. 2017;29:179–186. doi: 10.1097/MOP.0000000000000447. [DOI] [PubMed] [Google Scholar]
- 34.Nguyen H.L., Pieper G.H., Wilders R. Andersen-Tawil syndrome: Clinical and molecular aspects. Int. J. Cardiol. 2013;170:1–16. doi: 10.1016/j.ijcard.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 35.Hancox J.C., Whittaker D.G., Du C., Stuart A.G., Zhang H. Emerging therapeutic targets in the short QT syndrome. Expert Opin. Ther. Targets. 2018;22:439–451. doi: 10.1080/14728222.2018.1470621. [DOI] [PubMed] [Google Scholar]
- 36.Fialho D., Robert C.G., Emma M. Handbook of Clinical Neurology. Volume 148. Elsevier; Amsterdam, The Netherlands: 2018. Periodic paralysis; pp. 505–520. [DOI] [PubMed] [Google Scholar]
- 37.Masotti A., Uva P., Davis-Keppen L., Basel-Vanagaite L., Cohen L., Pisaneschi E., Celluzzi A., Bencivenga P., Fang M., Tian M., et al. Keppen-Lubinsky syndrome is caused by mutations in the inwardly rectifying K+ channel encoded by KCNJ6. Am. J. Hum. Genet. 2015;96:295–300. doi: 10.1016/j.ajhg.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Horvath G.A., Zhao Y., Tarailo-Graovac M., Boelman C., Gill H., Shyr C., Lee J., Blydt-Hansen I., Drögemöller B.I., Moreland J., et al. Gain-of-function KCNJ6 Mutation in a Severe Hyperkinetic Movement Disorder Phenotype. Neuroscience. 2018;384:152–164. doi: 10.1016/j.neuroscience.2018.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Korah H.E., Scholl U.I. An Update on Familial Hyperaldosteronism. Horm. Metab. Res. 2015;47:941–946. doi: 10.1055/s-0035-1564166. [DOI] [PubMed] [Google Scholar]
- 40.Bohnen M.S., Peng G., Robey S.H., Terrenoire C., Iyer V., Sampson K.J., Kass R.S. Molecular Pathophysiology of Congenital Long QT Syndrome. Physiol. Rev. 2017;97:89–134. doi: 10.1152/physrev.00008.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abdelhadi O., Iancu D., Stanescu H., Kleta R., Bockenhauer D. EAST syndrome: Clinical, pathophysiological, and genetic aspects of mutations in KCNJ10. Rare Dis. 2016;4:e1195043. doi: 10.1080/21675511.2016.1195043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nichols C.G., Singh G.K., Grange D.K. KATP channels and cardiovascular disease: Suddenly a syndrome. Circ. Res. 2013;112:1059–1072. doi: 10.1161/CIRCRESAHA.112.300514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tinker A., Aziz Q., Li Y., Specterman M. ATP-Sensitive Potassium Channels and Their Physiological and Pathophysiological Roles. Compr. Physiol. 2018;8:1463–1511. doi: 10.1002/cphy.c170048. [DOI] [PubMed] [Google Scholar]
- 44.Kumar M., Pattnaik B.R. Focus on Kir7.1: Physiology and channelopathy. Channels. 2014;8:488–495. doi: 10.4161/19336950.2014.959809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Taneja T.K., Mankouri J., Karnik R., Kannan S., Smith A.J., Munsey T., Christesen H.B., Beech D.J., Sivaprasadarao A. Sar1-GTPase-dependent ER exit of KATP channels revealed by a mutation causing congenital hyperinsulinism. Hum. Mol. Genet. 2009;18:2400–2413. doi: 10.1093/hmg/ddp179. [DOI] [PubMed] [Google Scholar]
- 46.Bendahhou S., Donaldson M.R., Plaster N.M., Tristani-Firouzi M., Fu Y.H., Ptácek L.J. Defective potassium channel Kir2.1 trafficking underlies Andersen-Tawil syndrome. J. Biol. Chem. 2003;278:51779–51785. doi: 10.1074/jbc.M310278200. [DOI] [PubMed] [Google Scholar]
- 47.Ma D., Tang X.D., Rogers T.B., Welling P.A. An andersen-Tawil syndrome mutation in Kir2. 1 (V302M) alters the G-loop cytoplasmic K+ conduction pathway. J. Biol. Chem. 2007;282:5781–5789. doi: 10.1074/jbc.M608776200. [DOI] [PubMed] [Google Scholar]
- 48.Peters M., Ermert S., Jeck N., Derst C., Pechmann U., Weber S., Schlingmann K.P., Seyberth H.W., Waldegger S., Konrad M. Classification and rescue of ROMK mutations underlying hyperprostaglandin E syndrome/antenatal Bartter syndrome. Kidney Int. 2003;64:923–932. doi: 10.1046/j.1523-1755.2003.00153.x. [DOI] [PubMed] [Google Scholar]
- 49.Choi B.O., Kim J., Suh B.C., Yu J.S., Sunwoo I.N., Kim S.J., Kim G.H., Chung K.W. Mutations of KCNJ2 gene associated with Andersen-Tawil syndrome in Korean families. J. Hum. Genet. 2007;52:280–283. doi: 10.1007/s10038-006-0100-7. [DOI] [PubMed] [Google Scholar]
- 50.Gloyn A.L., Pearson E.R., Antcliff J.F., Proks P., Bruining G.J., Slingerland A.S., Howard N., Srinivasan S., Silva J.M., Molnes J., et al. Activating mutations in the gene encoding the ATP-sensitive potassium-channel subunit Kir6.2 and permanent neonatal diabetes. N. Engl. J. Med. 2004;350:1838–1849. doi: 10.1056/NEJMoa032922. [DOI] [PubMed] [Google Scholar]
- 51.Lin Y.W., Bushman J.D., Yan F.F., Haidar S., MacMullen C., Ganguly A., Stanley C.A., Shyng S.L. Destabilization of ATP-sensitive potassium channel activity by novel KCNJ11 mutations identified in congenital hyperinsulinism. J. Biol. Chem. 2008;283:9146–9156. doi: 10.1074/jbc.M708798200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schulte U., Hahn H., Konrad M., Jeck N., Derst C., Wild K., Weidemann S., Ruppersberg J.P., Fakler B., Ludwig J. pH gating of ROMK (K(ir)1.1) channels: Control by an Arg-Lys-Arg triad disrupted in antenatal Bartter syndrome. Proc. Natl. Acad. Sci. USA. 1999;96:15298–15303. doi: 10.1073/pnas.96.26.15298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Scholl U.I., Choi M., Liu T., Ramaekers V.T., Häusler M.G., Grimmer J., Tobe S.W., Farhi A., Nelson-Williams C., Lifton R.P. Seizures, sensorineural deafness, ataxia, mental retardation, and electrolyte imbalance (SeSAME syndrome) caused by mutations in KCNJ10. Proc. Natl. Acad. Sci. USA. 2009;106:5842–5847. doi: 10.1073/pnas.0901749106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Limberg M.M., Zumhagen S., Netter M.F., Coffey A.J., Grace A., Rogers J., Böckelmann D., Rinné S., Stallmeyer B., Decher N., et al. Non dominant-negative KCNJ2 gene mutations leading to Andersen-Tawil syndrome with an isolated cardiac phenotype. Basic Res. Cardiol. 2013;108:353. doi: 10.1007/s00395-013-0353-1. [DOI] [PubMed] [Google Scholar]
- 55.Fallen K., Banerjee S., Sheehan J., Addison D., Lewis L.M., Meiler J., Denton J.S. The Kir channel immunoglobulin domain is essential for Kir1.1 (ROMK) thermodynamic stability, trafficking and gating. Channels. 2009;3:57–68. doi: 10.4161/chan.3.1.7817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.O’Donnell B.M., Mackie T.D., Subramanya A.R., Brodsky J.L. Endoplasmic reticulum-associated degradation of the renal potassium channel, ROMK, leads to type II Bartter syndrome. J. Biol. Chem. 2017;292:12813–12827. doi: 10.1074/jbc.M117.786376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Károlyi L., Konrad M., Köckerling A., Ziegler A., Zimmermann D.K., Roth B., Wieg C., Grzeschik K.H., Koch M.C., Seyberth H.W., et al. Mutations in the gene encoding the inwardly-rectifying renal potassium channel, ROMK, cause the antenatal variant of Bartter syndrome: Evidence for genetic heterogeneity. International Collaborative Study Group for Bartter-like Syndromes. Hum. Mol. Genet. 1997;6:17–26. doi: 10.1093/hmg/6.1.17. [DOI] [PubMed] [Google Scholar]
- 58.Fodstad H., Swan H., Auberson M., Gautschi I., Loffing J., Schild L., Kontula K. Loss-of-function mutations of the K+ channel gene KCNJ2 constitute a rare cause of long QT syndrome. J. Mol. Cell. Cardiol. 2004;37:593–602. doi: 10.1016/j.yjmcc.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 59.Davies N.P., Imbrici P., Fialho D., Herd C., Bilsland L.G., Weber A., Mueller R., Hilton-Jones D., Ealing J., Boothman B.R., et al. Andersen-Tawil syndrome: New potassium channel mutations and possible phenotypic variation. Neurology. 2005;65:1083–1089. doi: 10.1212/01.wnl.0000178888.03767.74. [DOI] [PubMed] [Google Scholar]
- 60.Lu C.W., Lin J.H., Rajawat Y.S., Jerng H., Rami T.G., Sanchez X., DeFreitas G., Carabello B., DeMayo F., Kearney D.L., et al. Functional and clinical characterization of a mutation in KCNJ2 associated with Andersen-Tawil syndrome. J. Med. Genet. 2006;43:653–659. doi: 10.1136/jmg.2006.040816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Eckhardt L.L., Farley A.L., Rodriguez E., Ruwaldt K., Hammill D., Tester D.J., Ackerman M.J., Makielski J.C. KCNJ2 mutations in arrhythmia patients referred for LQT testing: A mutation T305A with novel effect on rectification properties. Heart Rhythm. 2007;4:323–329. doi: 10.1016/j.hrthm.2006.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tani Y., Miura D., Kurokawa J., Nakamura K., Ouchida M., Shimizu K., Ohe T., Furukawa T. T75M-KCNJ2 mutation causing Andersen-Tawil syndrome enhances inward rectification by changing Mg2+ sensitivity. J. Mol. Cell. Cardiol. 2007;43:187–196. doi: 10.1016/j.yjmcc.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 63.Snider K.E., Becker S., Boyajian L., Shyng S.L., MacMullen C., Hughes N., Ganapathy K., Bhatti T., Stanley C.A., Ganguly A. Genotype and phenotype correlations in 417 children with congenital hyperinsulinism. J. Clin. Endocrinol. Metab. 2013;98:355–363. doi: 10.1210/jc.2012-2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mohnike K., Wieland I., Barthlen W., Vogelgesang S., Empting S., Mohnike W., Meissner T., Zenker M. Clinical and genetic evaluation of patients with KATP channel mutations from the German registry for congenital hyperinsulinism. Horm. Res. Paediatr. 2014;81:156–168. doi: 10.1159/000356905. [DOI] [PubMed] [Google Scholar]
- 65.Decher N., Renigunta V., Zuzarte M., Soom M., Heinemann S.H., Timothy K.W., Keating M.T., Daut J., Sanguinetti M.C., Splawski I. Impaired interaction between the slide helix and the C-terminus of Kir2.1: A novel mechanism of Andersen syndrome. Cardiovasc. Res. 2007;75:748–757. doi: 10.1016/j.cardiores.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 66.Yoon G., Oberoi S., Tristani-Firouzi M., Etheridge S.P., Quitania L., Kramer J.H., Miller B.L., Fu Y.H., Ptácek L.J. Andersen-Tawil syndrome: Prospective cohort analysis and expansion of the phenotype. Am. J. Med. Genet. A. 2006;140:312–321. doi: 10.1002/ajmg.a.31092. [DOI] [PubMed] [Google Scholar]
- 67.Ballester L.Y., Benson D.W., Wong B., Law I.H., Mathews K.D., Vanoye C.G., George A.L. Jr. Trafficking-competent and trafficking-defective KCNJ2 mutations in Andersen syndrome. Hum. Mutat. 2006;27:388. doi: 10.1002/humu.9418. [DOI] [PubMed] [Google Scholar]
- 68.Williams D.M., Lopes C.M., Rosenhouse-Dantsker A., Connelly H.L., Matavel A., O-Uchi J., McBeath E., Gray D.A. Molecular basis of decreased Kir4.1 function in SeSAME/EAST syndrome. J. Am. Soc. Nephrol. 2010;21:2117–2129. doi: 10.1681/ASN.2009121227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Takeda I., Takahashi T., Ueno H., Morino H., Ochi K., Nakamura T., Hosomi N., Kawakami H., Hashimoto K., Matsumoto M. Autosomal recessive Andersen–Tawil syndrome with a novel mutation L94P in Kir2.1. Neurol. Clin. Neurosci. 2013;1:131–137. doi: 10.1111/ncn3.38. [DOI] [Google Scholar]
- 70.Kuß J., Stallmeyer B., Goldstein M., Rinné S., Pees C., Zumhagen S., Seebohm G., Decher N., Pott L., Kienitz M.C., et al. Familial Sinus Node Disease Caused by a Gain of GIRK (G-Protein Activated Inwardly Rectifying K+ Channel) Channel Function. Circ. Genom. Precis. Med. 2019;12:e002238. doi: 10.1161/CIRCGEN.118.002238. [DOI] [PubMed] [Google Scholar]
- 71.Derst C., Wischmeyer E., Preisig-Müller R., Spauschus A., Konrad M., Hensen P., Jeck N., Seyberth H.W., Daut J., Karschin A. A hyperprostaglandin E syndrome mutation in Kir1. 1 (renal outer medullary potassium) channels reveals a crucial residue for channel function in Kir1. 3 channels. J. Biol. Chem. 1998;273:23884–23891. doi: 10.1074/jbc.273.37.23884. [DOI] [PubMed] [Google Scholar]
- 72.Cheng C.J., Sung C.C., Wu S.T., Lin Y.C., Sytwu H.K., Huang C.L., Lin S.H. Novel KCNJ5 mutations in sporadic aldosterone-producing adenoma reduce Kir3.4 membrane abundance. J. Clin. Endocrinol. Metab. 2015;100:E155–E163. doi: 10.1210/jc.2014-3009. [DOI] [PubMed] [Google Scholar]
- 73.Gélinas R., El Khoury N., Chaix M.A., Beauchamp C., Alikashani A., Ethier N., Boucher G., Villeneuve L., Robb L., Latour F., et al. Characterization of a Human Induced Pluripotent Stem Cell-Derived Cardiomyocyte Model for the Study of Variant Pathogenicity: Validation of a KCNJ2 Mutation. Circ. Cardiovasc. Genet. 2017;10:e001755. doi: 10.1161/CIRCGENETICS.117.001755. [DOI] [PubMed] [Google Scholar]
- 74.Cheng C.J., Lin S.H., Lo Y.F., Yang S.S., Hsu Y.J., Cannon S.C., Huang C.L. Identification and functional characterization of Kir2.6 mutations associated with non-familial hypokalemic periodic paralysis. J. Biol. Chem. 2011;286:27425–27435. doi: 10.1074/jbc.M111.249656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lee S.J., Ren F., Zangerl-Plessl E.M., Heyman S., Stary-Weinzinger A., Yuan P., Nichols C.G. Structural basis of control of inward rectifier Kir2 channel gating by bulk anionic phospholipids. J. Gen. Physiol. 2016;148:227–237. doi: 10.1085/jgp.201611616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tanemoto M., Abe T., Uchida S., Kawahara K. Mislocalization of K+ channels causes the renal salt wasting in EAST/SeSAME syndrome. FEBS Lett. 2014;588:899–905. doi: 10.1016/j.febslet.2014.02.024. [DOI] [PubMed] [Google Scholar]
- 77.Pattnaik B.R., Tokarz S., Asuma M.P., Schroeder T., Sharma A., Mitchell J.C., Edwards A.O., Pillers D.A. Snowflake vitreoretinal degeneration (SVD) mutation R162W provides new insights into Kir7.1 ion channel structure and function. PLoS ONE. 2013;8:71744. doi: 10.1371/journal.pone.0071744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sergouniotis P.I., Davidson A.E., Mackay D.S., Li Z., Yang X., Plagnol V., Moore A.T., Webster A.R. Recessive mutations in KCNJ13, encoding an inwardly rectifying potassium channel subunit, cause leber congenital amaurosis. Am. J. Hum. Genet. 2011;89:183–190. doi: 10.1016/j.ajhg.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.McDonald S.K., Levitz T.S., Valiyaveetil F.I. A Shared Mechanism for the Folding of Voltage-Gated K+ Channels. Biochemistry. 2019;58:1660–1671. doi: 10.1021/acs.biochem.9b00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cho H.C., Tsushima R.G., Nguyen T.T., Guy H.R., Backx P.H. Two critical cysteine residues implicated in disulfide bond formation and proper folding of Kir2. 1. Biochemistry. 2000;39:4649–4657. doi: 10.1021/bi992469g. [DOI] [PubMed] [Google Scholar]
- 81.Hristova K., Wimley W.C. A look at arginine in membranes. J. Membr. Biol. 2011;239:49–56. doi: 10.1007/s00232-010-9323-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.