Abstract
Chronic neuropathic pain due to iliohypogastric (IH) or ilioinguinal (IL) nerve entrapment or injury may demonstrate as referred pain to the genito-urinary organs. Our patient is a 67-year-old woman who presented with a 9-month history of bladder pain, dyspareunia and nocturia that all began following a laparoscopic pyeloplasty. This report describes improvement of bladder pain syndrome following surgical resection of the II and IH nerves.
Introduction
Neuropathy resulting from an injury to the ilioinguinal (IL) and/or iliohypogastric (IH) nerves is a well-recognized complication following lower abdominal and pelvic surgeries.1,2 Both nerves are most commonly injured at time of skin incision during inguinal herniorrhaphy, appendectomy, urological or gynecologic operations performed via a low transverse incision. The injuries may also occur at the deeper levels of abdominal musculature and have been reported following abdominoplasty, abdominal wall reconstruction and transversus abdominis muscle (TRAM) breast reconstruction. Although the incidence of iatrogenic nerve injury sustained during gynecologic or urologic surgery is unknown, there is an estimated 5% risk of clinically significant postoperative neuropathic pain due to injury to these nerves secondary to a lateral laparoscopic or robotic port placement, and fascial closures with commonly used devices such as Carter-Thomason (Inlet Medical Inc., Eden Prairie, MN).
Mechanisms of injury to the sensory branches of the IH and IL nerves can include direct damage via a partial or complete resection, crush, stretch, contusion or electrocoagulation. Secondary damage may also occur as result of inflammation surrounding the nerve, tissue compression exerted onto it, or a neuroma formation.
Recent developments in the pain management arena paved the way to the IL and IH neurectomy as a novel treatment of low abdominal and groin pain.3 Here, we report a case of IL and IH neuropathy successfully treated with their surgical resection.
Case presentation
A 67-year-old female presented with suprapubic and left lower quadrant (LLQ) abdominal pain associated with bladder filling, q1hr nocturia and dyspareunia. All her symptoms developed following a left laparoscopic pyeloplasty performed eight months prior to this presentation.
Patient's LLQ abdominal pain was constant, localized to one of her laparoscopic port sites. Palpation of her port site scar exacerbated her pain and reproduced sensation of urinary urgency. Her initial examination demonstrated a specific trigger point in the distribution of the IL and IH nerves.
Her urinary and painful bladder symptoms improved significantly following an IL/IH nerve block. Based on this, her history and absence of hernia on physical examination, she was diagnosed with the neuromas of the left IL and IH nerves.
Preoperatively, her O'Leary/Sant Interstitial Cystitis Symptom Index and Problem Index (OSPI) scores were 20 and 16, respectively. Her Pelvic Pain and Urgency/Frequency Patient Symptoms Scale (PUF) Score was 18 with a bother of 10.
Patient underwent a resection of her left IL and IH nerves in July 2018 (Fig. 1). At time of her follow-up, four weeks post-operatively, she reported resolution of her bladder and abdominal pain and improvement in her dyspareunia and urinary symptoms. At six weeks post-operatively, her O'Leary/Sant Interstitial Cystitis Symptom Index and Problem Index (OSPI) scores were 4 and 1, respectively. Her Pelvic Pain and Urgency/Frequency Patient Symptoms Scale (PUF) Score was 5 with a bother of 3.
Fig. 1.
Intra-operative photographs demonstrating main steps of IL/IH nerve resection. A. Incision demarcated above the inguinal ligament. Patient's trigger point marked with the asterisk. B. IH nerve pointed out by the scissor tips, with the IL nerve inferior to it. C. IH nerve resection. D. IL and IH nerve resection completed.
At her 6-month follow-up in January of 2019, her symptoms stabilized, and her O'Leary/Sant Interstitial Cystitis Symptom Index and Problem Index (OSPI) scores were 13 and 13, respectively. Her Pelvic Pain and Urgency/Frequency Patient Symptoms Scale (PUF) Score was 6 with a bother of 8.
Discussion
Our patient noted her left lower quadrant pain, urinary symptoms and dyspareunia soon after a left laparoscopic pyeloplasty. Since her trigger point localized to one of the lateral port sites in the absence of a hernia, her neuralgia was most likely caused by the fascial closure at the time of pyeloplasty.
The standard approach to the patients experiencing IL/IH neuralgia is to perform a thorough physical examination. Once all other potential causes for the patient's pain are ruled out, patient may undergo further evaluation and treatment with a diagnostic and therapeutic nerve block. If the nerve block provides any temporary relief, the surgery should be undertaken in order to further treat this condition.4 Although neurolysis and neurectomy have been described before, there is no one standard recommended treatment as of now.4 While pain relief with nerve blocks is reported to range from 40% to 50%, neurectomy/neurolysis procedures usually result in up to 90% pain relief eliminating the need for use of analgesia. The side effects of this surgery are reported to be persistent numbness below the resected nerve, loss of cremasteric reflex in men, rare superficial skin infections and recurrence.
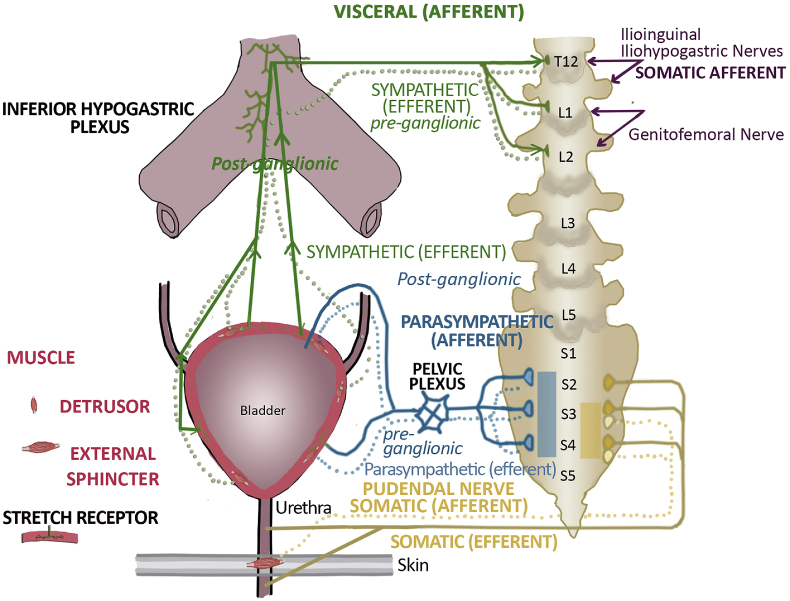
In order to prevent iatrogenic injuries to the IL/IH nerves and appropriately evaluate and manage patients with neuropathic pain contributing to lower genitourinary tract symptoms, one must be familiar with neural anatomy and function. The IL nerve originates from L1 and sometimes T12 and L2 spinal levels and it supplies supero-medial thigh, the root of the penis and upper scrotum in men and the skin of the mons pubis and labia majora in women. The IH nerve arises from L1 and T12 nerves and supplies the skin of the hypogastric and gluteal regions. Pain perceived in the deep pelvis, rectum or proximal vagina may be referred from the IH nerve and examination of any of these organs should stimulate painful response, which will ultimately radiate to the region near the site of previous surgery. Our patient's symptoms included bladder pain and dyspareunia, which were associated with the trigger point at the skin level, and this all clearly corresponds to the distribution of the IH and IL innervation. Her significant improvement in urinary symptoms further suggests referred pain from either the IL and/or IH nerve to the bladder. The hypothesis that bladder pain syndrome can be a referred pain syndrome from injury to the IL and IH nerves seems to be confirmed by the findings in the case reported here.5 The somatic afferent impulses from the IL and IH nerves enter the spinal cord at the same thoracolumbar outflow tract as the sympathetic efferent and the visceral afferent fibers that accompany the sympathetic nerves to the bladder. (See Fig. 2 for the proposed physiologic explanation of this phenomenon). As result, painful afferent impulses from the IL and IH neuromas are interpreted as bladder pain. According to this hypothesis, and as demonstrated in the case reported here, resection of the IL and IH nerves stops the pain input to the dorsal horn of the spinal cord, stopping the perception that the bladder is sending a pain message.
Fig. 2.
Bladder innervation and referred bladder pain pathway. Three separate neuronal pathways (containing both afferent and efferent fibers): thoracolumbar, sacral visceral and sacral somatic contribute to bladder innervation. For the referred pain pathway, the thoracolumbar region (T12-L2) contains the visceral afferent (dark green) input from stretch receptors in the bladder/detrusor muscle wall. These participate in spinal reflex for bladder filling. Once a certain bladder volume has been reached, the intensity of neural impulses peaks, and this perception passes to the conscious level to permit voiding. It is hypothesized that the somatic afferent input from the IH and IL (and perhaps genitofemoral) nerves (dark purple) into the T12-L2 dorsal spinal cord can be misinterpreted as arising from the visceral afferents from this same level, causing bladder pain syndrome.5 (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Funding
None.
Declaration of competing interest
None.
References
- 1.Cardosi R.J., Cox C.S., Hoffman M.S. Postoperative neuropathies after major pelvic surgery. Obstet Gynecol. 2002;100(2):240–244. doi: 10.1016/s0029-7844(02)02052-5. [DOI] [PubMed] [Google Scholar]
- 2.Sippo W.C., Gomez A.C. Nerve-entrapment syndromes from lower abdominal surgery. J Fam Pract. 1987;25(6):585–587. [PubMed] [Google Scholar]
- 3.Lee C.H., Dellon A.L. Surgical management for groin pain of neural origin. J Amer Col Surg. 2000;191(2):137–142. doi: 10.1016/s1072-7515(00)00319-7. [DOI] [PubMed] [Google Scholar]
- 4.Hahn L. Clinical findings and results of operative treatment in ilioinguinal nerve entrapment syndrome. Br J Obstet Gynaecol. 1989;96(9):1080–1083. doi: 10.1111/j.1471-0528.1989.tb03385.x. [DOI] [PubMed] [Google Scholar]
- 5.Dellon A.L., Herati A.S. Review of bladder pain and referred T12-L2 input as one etiology for interstitial cystitis. J Reconstr Microsurg Open. 2019;4(2):e58–e63. [Google Scholar]