Abstract
Stafne bone cavity (SBC) is a rare mandibular defect, and the diagnosis and management may be confused with the unusual contents and location. This report for the first time presented a case of SBC with a lymph node content. Meanwhile, a rare case of anterior SBC with fatty tissue content is reported. Typical SBCs with salivary glands content are asymptomatic and showed a well-shaped, ovoid, radiolucent image in the posterior mandible below the inferior alveolar canal in panoramic radiograph. The case of SBC with a lymph node content underwent surgical operation, and definite diagnosis is confirmed by histopathological examination. The case of anterior SBC with fatty tissue content is clarified by MRI confirmed the presence of the fatty tissue and avoided surgical exploration. Surgical interventions would be an unnecessary option in the management of SBC except for the doubtful cases or concomitant other pathologies.
Keywords: Stafne bone cavity, Lingual mandibular bone defect, Lymph node, Fatty tissue, Anterior
Introduction
Stafne bone cavity (SBC) is a rare mandibular defect with unknown etiology. SBC was first described by Edward Stafne in 1942, who reported asymptomatic unilateral radiolucent defects in the posterior region of the mandible.1 The cavities appearing as round or ovoid, well-demarcated, unilocular radiolucency were located between the mandibular angle and the third molar, below the inferior alveolar canal and above the mandibular base.1
The anterior variant of this cavity, which is a radiolucent cavity usually located between the canine and premolar mandibular region, was first reported by Richard and Ziskind in 1957.2 The clinical and radiographic features of the anterior SBC are similar to the posterior variant. Posterior SBCs can be easily diagnosed due to their unique features on radiographs; however, the anterior variants may be misdiagnosed and confused with other pathological entities owing to their unusual locations.3
In the literature review, the contents within the bone cavity are usually salivary glands. Hardly any reports are available so far on lymphoid and fatty tissues being the content. In this study, we report a quite rare non-typical case of posterior SBC with a lymph node content and a rare non-typical case of anterior SBC with fatty tissue content, and compare their diagnoses and managements with 2 typical cases with salivary glands content. The causes, clinical and radiographic features, and differential diagnoses of this rare condition are also discussed.
Patients and methods
The four cases of SBC who attended the Department of Oral and Maxillofacial-Head and Neck Oncology, Shanghai Ninth People's Hospital, Shanghai, China were collected and reviewed by the authors. These cases who had a suspected SBC based on panoramic radiography made for other reasons, or as part of the complementary studies of a first visit to the authors' clinic. The radiographs revealed a rounded or ovoid radiolucent image, in the posterior or anterior area of the mandible, having no apparent relationship with the teeth, and either below or superimposed on the inferior alveolar canal. The following data were collected by the same professional: age, gender, reason for consultation, clinical symptoms, history of trauma, shape, radiological features, variant, treatment and evolution. This study was approved by the local institutional review board.
Results
Clinical and radiographic features
Baseline characteristics of the present four cases of SBC are summarized in Table 1. The four cases in this report were discovered radiologically by accident with no symptoms. The patients did not complain of any pain, discomfort, or numbness in the mandible, and palpation of the defect were also not painful. Intraorally, there were no visible swelling on the lingual or buccal side of the lesion region of the mandible. The patient's medical history was not significant. They also denied any trauma to the mandible or significant surgical history. These cavities were asymptomatic and showed a well-shaped, unilocular, ovoid, radiolucent image by panoramic radiograph. They appeared to have no relationship with the adjacent teeth that gave positive responses to the vitality tests either below or superimposed on the inferior alveolar canal.
Table 1.
Baseline characteristics of the present 4 cases of Stafne bone cavity.
| Case | Age (y) | Gender | Side | Lesion size (cm) | Location variant | Content | Treatment |
|---|---|---|---|---|---|---|---|
| 1 | 47 | Male | Right | 1.3*1.2*1.1 | Posterior | Lymph node | Surgical exploration |
| 2 | 37 | Female | Right | 1.1*0.8*0.5 | Anterior | Fatty tissue | Watch and see |
| 3 | 52 | Male | Left | 1.0*0.7*0.6 | Posterior | Salivary gland | Watch and see |
| 4 | 43 | Male | Left | 1.1*0.9*0.8 | Posterior | Salivary gland | Watch and see |
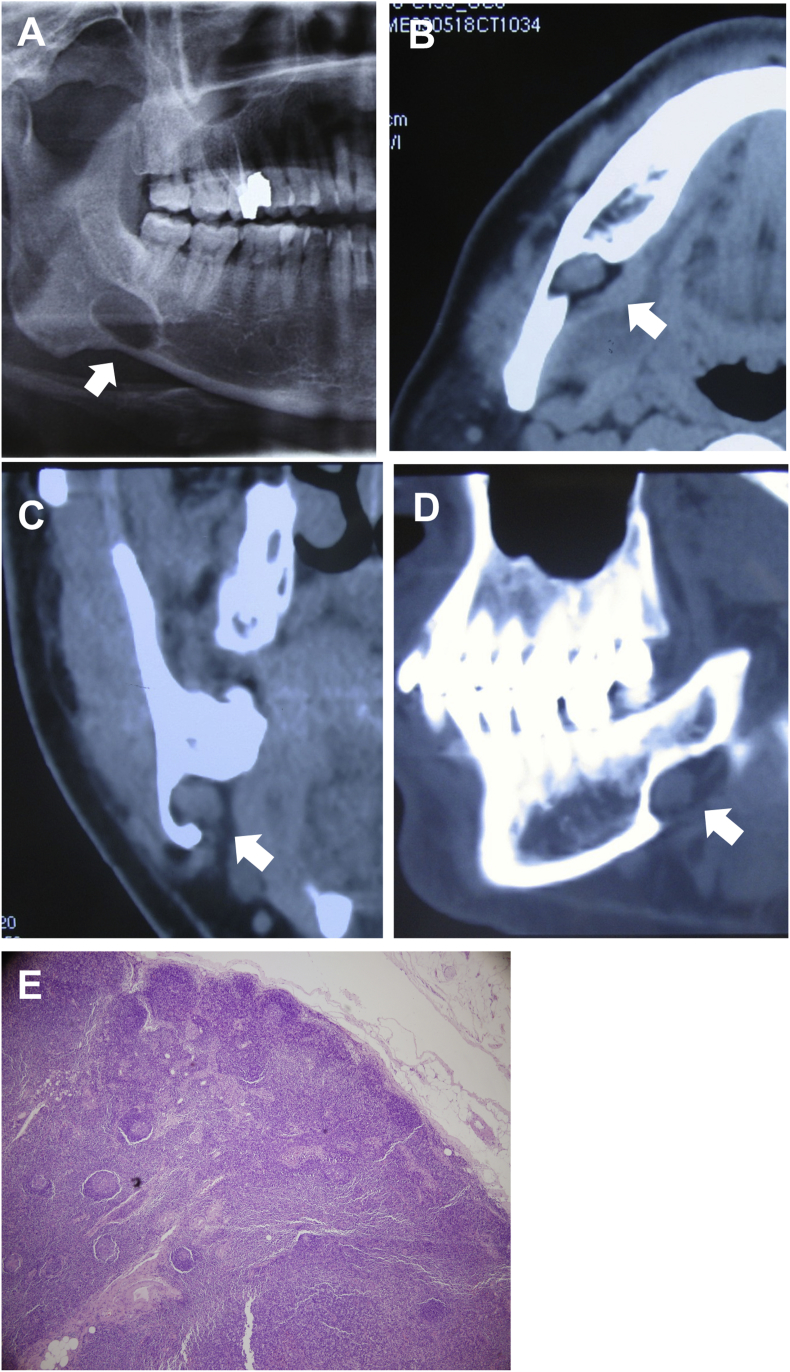
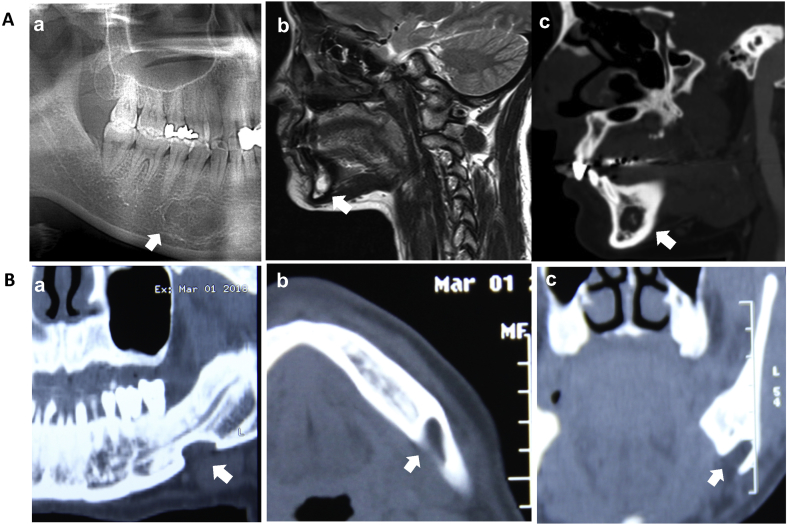
Panoramic radiograph of Case 1 (a 47-years-old male) showed an ovoid radiolucent image in right mandibular angle located below the root of third molar. The CT image showed a soft tissue in the lingual mandibular bone cavity measured approximately 1.3 × 1.2 × 1.1 cm with clear boundary (Fig. 1). The inferior alveolar canal was not clear around the lesion. The panoramic radiograph of Case 2 (a 37-years-old female) showed an oval radiolucent image located at the premolar and canine regions of the mandible. MRI image showed high signal intensity on T2WI and T1WI, but showed low signal intensity on fat-suppression T2WI (Fig. 2A). The radiographs of Case 3 (a 52-years-old male) and Case 4 (a 43-years-old male) as typical posterior SBCs showed radiolucent defects below inferior alveolar canal and a connection to the base of the mandible (Fig. 2B).
Figure 1.
A non-typical case of posterior SBC with a lymph node content. (A) panoramic radiograph, (B) cross, (C) coronal and (D) sagittal CT examination. (E) histopathological examination revealed a lymph node.
Figure 2.
(A) Radiographs of a non-typical case of anterior SBC with fatty tissue content. (a) panoramic radiograph, (b) high signal intensity on T2WI, and (c) low signal intensity on fat-suppression T2WI in MRI examination. (B) Radiographs of a case of typical posterior SBC. (a) panoramic radiograph, (b) cross and (c) coronal CT examination.
Diagnosis and treatment strategy
The contents of the typical SBCs are usual salivary glands in the literature. Rare case reports have been published regarding the lymphatic and fatty tissues related to the cavity. Herein, we reported a quite rare non-typical case of a lymph node within posterior SBC (Case 1) and a rare non-typical case of fatty tissue within anterior SBC (Case 2).
For the Case 1, the relationship between inferior alveolar canal and the lesion was not clear. This may be misdiagnosed and confused with several pathologic entities such as schwannoma, giant cell granuloma, and odontogenic keratocyst. In order to clarify the diagnosis, the patient underwent surgical operation, and a submandibular incision was made. During the operation, a lymph node with clear boundary was found between the mandible and submandibular gland. The histopathological examination revealed the absence of any cystic or tumor lesion and salivary gland but rather a normal lymph node (Fig. 1E). The lesion was finally diagnosed as a SBC with a lymph node being the content. The healing period was uneventful, and no signs of pathology were noted at 3-year follow-up.
Case 2 was also a rare non-typical case of SBC, which the radiolucent bone cavity located on the anterior mandible. A complementary test, MRI, was completed to identify the tissue content within the cavity. This case was clarified by MRI confirmed the presence of the fatty tissue (Fig. 2A). A diagnosis of an anterior SBC with fatty tissue being the content was made and it was decided that the patient would not undergo surgery with a 6-month follow-up period. No remarkable changes were observed for the 2 years following diagnosis. Cases 3 and 4 can be readily diagnosed as typical posterior SBC due to the features of typical posterior SBC. The patients were informed about the lesion and it was decided that the patients would not undergo surgery. Both were scheduled for follow-up, and no remarkable changes were noted over 2-year follow-up.
Discussion
Typical SBCs were usual located at posterior mandible and the contents were usual glandular tissue. Posterior variant of SBC has an incidence of between 0.08 and 0.48% when diagnosed radiologically,4, 5, 6 and the incidence of the anterior variant is quite rare with just over 50 cases reported in the English-language literature.3 In this study, a quite rare non-typical case of posterior SBC with a lymph node content and a rare non-typical case of anterior SBC with fatty tissue content were presented.
The cause of SBC is uncertain. The concept that the pressure of the glandular tissue on the lingual cortex of the mandible causes a lingual bony depression is widely accepted.4, 5, 6 The submandibular salivary gland is responsible for the posterior variant of SBCs, whereas the sublingual gland causes anterior variant. Indeed, glandular tissue within cavities during surgical exploration were found by many investigators.4, 5, 6 Although salivary glands as the contents thought to be responsible for SBC, our report confirmed that fatty and lymphoid tissues were associated to the bone cavity.
SBCs are unilocular radiolucent cavities and commonly discovered incidentally in routine radiographic evaluation because they are asymptomatic, and our cases were in keeping with this notion. SBCs mostly affect male in the fifth or sixth decade of life, three out of four cases were males and in the fourth decade of life in this report. The contents of the typical SBCs are usual salivary glands in the literature,4, 5, 6 a rare non-typical case of fatty tissue within anterior SBC was reported.7 This case was clarified by MRI confirmed the presence of the fatty tissue and avoided surgical exploration. CT is preferred to identify whether the bone lesion was another mandible pathology. MRI has the advantage of showing the soft tissue prolapsed into the bony cavity without exposing the patient to radiation, which is suggested to identify the contents of the cavity.8
It is noteworthy that a SBC case with a lymph node being the content is reported. To our knowledge, it is reported for the first time that this case had the detailed clinical and radiographic data and demonstrated by histopathologic examination. Although the management strategy of typical cases would not undergo surgery, surgical intervention and pathologic examination of the content tissue may be indicated in atypical cases, or when doubts exist as to diagnosis. This is the only way in which to discount a neoplastic pathology with certainty. Indeed, a case of metastatic node of hepatocellular carcinoma and prostate cancer into the mandible mimicking a SBC was reported, respectively.9,10
In conclusion, typical posterior SBC can be readily diagnosed by panoramic radiograph due to their unique features. Advanced radiological assessment with CT and MRI scans are usually sufficient to achieve a final diagnosis of atypical SBC so as to avoid overtreatment. Surgical interventions would be an unnecessary option in the management of SBC except for the doubtful cases or concomitant other pathologies.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgments
This work was supported by National Key R&D Program of China (2017YFC0840100, 2017YFC0840110) and Commission of Health and Family Planning Foundation of Shanghai Municipality (201840021).
Contributor Information
Yongjie Hu, Email: drhuyongjie@126.com.
Wei Liu, Email: liuweb@hotmail.com.
References
- 1.Stafne E.C. Bone cavities situated near the angle of the mandible. J Am Dent Assoc. 1942;29:1969–1972. [Google Scholar]
- 2.Richard E.L., Ziskind J. Aberrant salivary gland tissue in mandible. Oral Surg Oral Med Oral Pathol. 1957;10:1086–1090. doi: 10.1016/0030-4220(57)90059-2. [DOI] [PubMed] [Google Scholar]
- 3.Katz J., Chaushu G., Rotstein I. Stafne's bone cavity in the anterior mandible: a possible diagnostic challenge. J Endod. 2001;27:304–307. doi: 10.1097/00004770-200104000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Schneider T., Filo K., Locher M.C. Stafne bone cavities: systematic algorithm for diagnosis derived from retrospective data over a 5-year period. Br J Oral Maxillofac Surg. 2014;52:369–374. doi: 10.1016/j.bjoms.2014.01.017. [DOI] [PubMed] [Google Scholar]
- 5.Assaf A.T., Solaty M., Zrnc T.A. Prevalence of Stafne's bone cavity--retrospective analysis of 14,005 panoramic views. In Vivo. 2014;28:1159–1164. [PubMed] [Google Scholar]
- 6.Hisatomi M., Munhoz L., Asaumi J., Arita E.S. Stafne bone defects radiographic features in panoramic radiographs: assessment of 91 cases. Med Oral Patol Oral Cir Bucal. 2019;24:e12–e19. doi: 10.4317/medoral.22592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Friedrich R.E., Zustin J., Scheuer H.A., Assaf A.T., Gröbe A. An unilateral basal bone defect of the mandible occupied by fatty tissue: Stafne's cavity. In Vivo. 2012;26:1045–1048. [PubMed] [Google Scholar]
- 8.Minowa K., Inoue N., Sawamura T., Matsuda A., Totsuka Y., Nakamura M. Evaluation of static bone cavities with CT and MRI. Dentomaxillofac Radiol. 2003;32:2–7. doi: 10.1259/dmfr/92201340. [DOI] [PubMed] [Google Scholar]
- 9.Fujihara H., Chikazu D., Saijo H. Metastasis of hepatocellular carcinoma into the mandible with radiographic findings mimicking a radicular cyst: a case report. J Endod. 2010;36:1593–1596. doi: 10.1016/j.joen.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 10.da Silva W.G., Kemp A.T., Dos Santos-Silva A.R., Diz M.D.P., Brandão T.B. Stafne's bone defect in a metastatic prostate cancer patient: a diagnostic conundrum. J Clin Exp Dent. 2018;10:e88–e91. doi: 10.4317/jced.53656. [DOI] [PMC free article] [PubMed] [Google Scholar]