A 32-year-old man presented to the emergency department of this hospital because of persistent right temporal headache for one week after difficult right lower wisdom tooth extraction (the procedure was over one hour) in a dental clinic. The patient had been in good health and was smoking 1/2 pack of cigarettes per day for 10 years. Neurological examination was normal and there was clear consciousness. He was prescribed ketorolac and acetamiophen. Two days later, he presented to the emergency department with right temporal headache, aggravated by neck flexion and swollen sensation of the right eyeball. Mild nuchal stiffness and meningitis was suspected. Computed tomography (CT) of brain revealed no active lesion (Fig. 1A). Lumbar puncture was performed, cerebrospinal fluid was clear and laboratory examinations were unremarkable. He was admitted, fever developed on the 2nd hospital day and two sets of blood culture were collected. The white blood cell count was 16,680/μL, cefuroxime was administered intravenously. He was discharged on 6th hospital day with no abnormal finding and fever subsided. 5 days later, he presented to the emergency department because of left upper limb weakness (muscle power 4/5), swallowing disturbance and persistent headache. CT of brain revealed hypodensities over the right frontal, temporal, and occipital lobes and basal ganglia with a minimal mass effect on the right frontal horn, right middle cerebral artery territory infarction was noted (Fig. 1B). Two additional sets of blood culture were collected, intravenous ceftriaxone, and metronidazole were administered. He was admitted to intensive care unit for 4 days and trans-esophageal echocardiogram (TEE) revealed no vegetation or thrombi. All four sets blood culture yielded Prevotella denticola and antimicrobial treatment was changed to two-week course of meropenem. Intravenous anticoagulation was not used due to septic emboli. After 17 days of hospitalization, he was discharged with no headache and left upper limb weakness improved. 10 days later, he was admitted again because of severe headache, dizziness, neck pain and vomiting. On 3rd hospital day, he was referred to the tertiary medical center for neurosurgical drainage of Prevotella brain abscess.
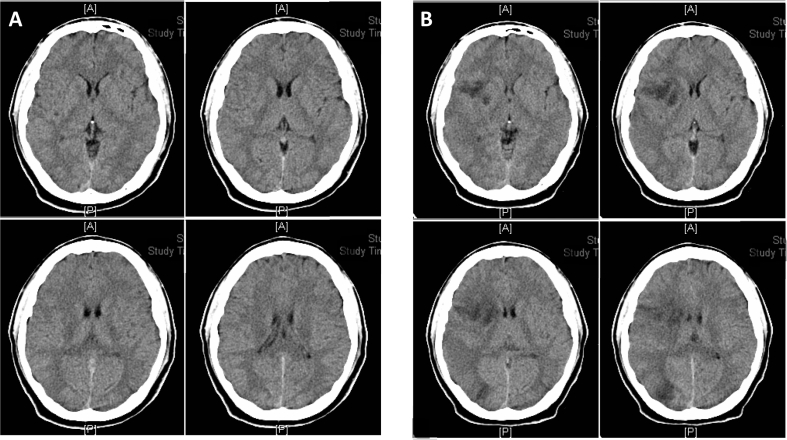
Figure 1.
Computed tomography (CT) of the brain of our patient. (A) No active lesion in the brain CT images. (B) Hypodensity involved the right frontal, temporal, occipital lobes, and basal ganglia. Minimal mass effect on the right frontal horn but no midline shift was found. Effaced ventricle, cistern and sulci due to edema were noted.
Prevotella species originate mostly from the oral cavity, are pigmented anaerobic Gram-negative rods and important pathogens in endodontic infections.1 Anaerobic bacteria are generally considered to be of relatively low virulence and are especially prevalent in infections associated with underlying conditions such as trauma or dental extraction, thus affording an opportunity to penetrate deeper tissues or blood stream and inaugurate infection.2 The P. denticola strain cultured from the patient's blood was sensitive to ampicillin/sulbactam, chloramphenicol, clindamycin, metronidazole, cefmetazole and cefoxitin, but resistant to penicillin.3 The Prevotella species are disseminated by hematogenous route and harbor the brain tissue to form abscess gradually although his blood was sterilized after antibiotic treatment with meropenem. If the diagnosis of P. denticola can be obtained before dental extraction, antibiotic treatment may lead to complete resolution.4 Chloramphenicol is a bacteriostatic, highly effective and has an excellent activity against anaerobic bacteria and is specially indicated for prolonged use in seriously ill patients in suspected central nervous system infections.5
Conflicts of interest
None declared.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jds.2019.04.006.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Kumar P.S., Griffen A.L., Barton J.A., Paster B.J., Moeschberger M.L., Leys E.J. New bacterial species associated with chronic periodontitis. J Dent Res. 2003;82:338–344. doi: 10.1177/154405910308200503. [DOI] [PubMed] [Google Scholar]
- 2.Nadkarni M.A., Chhour K.L., Browne G.V. Age-dependent changes in Porphyromonas gingivalis and Prevotella species/phylotypes in healthy gingiva and inflamed/diseased sub-gingival sites. Clin Oral Investig. 2015;19:911–919. doi: 10.1007/s00784-014-1301-7. [DOI] [PubMed] [Google Scholar]
- 3.Sherrard L.J., Graham K.A., McGrath S.J. Antibiotic resistance in Prevotella species isolated from patients with cystic fibrosis. J Antimicrob Chemother. 2013;68:2369–2374. doi: 10.1093/jac/dkt191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loesche W. Dental caries and periodontitis: contrasting two infections that have medical implications. Infect Dis Clin North Am. 2007;21:471–502. doi: 10.1016/j.idc.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 5.Feder H.M., Jr. Chloramphenicol: what we have learned in the last decade. South Med J. 1986;79:1129–1134. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.