Abstract
Background/purpose
The use of osteotomes as a technique for densification and expansion of the residual ridge is one of the most widely used procedures to achieve adequate peri-implant bone quantity and density. The aim of this study was to evaluate the influence of time and the elastic deformation of peri-implant bone in the primary stability of implants placed using osteotomes.
Materials and methods
In each of 10 fresh fragments of cow rib, two implants were placed using osteotomes. The insertion torque and initial implant stability quotient (ISQ) values were measured. In the control implants, the immediate removal torque was measured, while in the test implants, after 15 min of placement, ISQ values were measured again, and the removal torque was measured.
Results
There were significant differences between the ISQ values and between the insertion torque and removal torque at 15 min. The ISQ values (perpendicular/parallel) increased between the initial moment (64.4 ± 9/70.3 ± 5.9) and 15 min (66/71.4 ± 6.4). The removal torque at 15 min (12.4 ± 5.8) was lower than the insertion torque (15.9 ± 5.9). Compression of the trabeculae in contact with the implant placed using osteotomes was observed, as well as a greater number of trabecular fractures in the implants placed using conventional drilling.
Conclusion
There is an increase in ISQ values of dental implants placed using osteotomes after 15 min of placement.
Keywords: Implant stability, Osteotomes, Resonance frequency analysis
Introduction
The use of dental implants for the rehabilitation of dental absences is currently the method most used by clinicians to restore patients who suffer from aesthetic and function loss.1
The prognosis of implant-supported rehabilitation depends on several factors, including having a sufficient quality and quantity of bone for the appropriate three-dimensional placement of the implant and for obtaining correct primary stability.2
Leckholm and Zarb established a classification of bone quality based on the density and distribution of cortical and trabecular bone. Types 3 and 4 describe a low-density bone with thin cortical density and poor trabecular bone compactness, in which the primary stability of the implant may be compromised. Additionally, they established the degrees of reabsorption of the alveolar process that follows the departure of the tooth and determines the amount of bone available. This availability may be insufficient for an ideal placement of the implant considering the optimal comfort zones.3
In cases where there is limited bone availability, both in quantity and quality, the execution of surgical and/or regenerative techniques may be necessary in addition to the placement of the implant.4
The use of osteotomes as a technique for densification and expansion of the residual ridge was first described by Summers and is one of the most widely used procedures to achieve adequate peri-implant bone quantity and density that guarantees the correct prognosis of the treatment.5,6
The achievement of correct primary stability plays an important role in the success of the treatment. An excess of micromovements of the implant in its bed during osseointegration can determine the failure of the process and achievement of fibrointegration.7
Throughout history, various methods have been used to quantify implant stability.8,9 Currently, one of the most valued noninvasive clinical methods is resonance frequency analysis (RFA), introduced by Meredith et al., in 1996.10 An RFA emits a sinusoidal signal to a transducer that is screwed into the implant until it achieves vibration and enters into resonance, obtaining its natural frequency of vibration, translated into a return signal that is captured by the device and interpreted in values of 0–100.11
Several studies show that there is an inverse and linear correlation between the implant stability quotient (ISQ) values of RFA and the micromotion of implants subjected to functional loading.12,13
There are several factors that determine the primary stability of implants, including peri-implant bone density. There are numerous studies that conclude that the greater the bone density, the greater the primary stability of the implant.14,15
Bone is a living tissue under constant remodeling that modifies its structure before the load application.16 As all materials, bone possesses mechanical characteristics that condition its biomechanical behavior; the elasticity or Young's modulus of peri-implant bone is approximately 15 GPa in cortical and 1 GPa in spongy bone, and both have a Poisson's coefficient of approximately 0.33.17 These mechanical characteristics give the bone a certain elasticity when tension is applied. When applying tension to a material, it suffers a deformation depending on the elastic modulus of the material; with the same applied tension, the greater the elastic modulus, the less the deformation, and the lower the elastic modulus, the greater the deformation. This deformation can be elastic up to a certain limit, when the material recovers its original dimensions after eliminating the applied tension, or plastic, if the material suffers a permanent deformation and does not recover its original dimensions after eliminating the tension.18
The technique of using osteotomes for carving the peri-implant bed involves a deformation of the bone based on the application of tension by the instrument, so that unlike drilling, bone is not lost during the instrumentation. According to the hypothesis of this test, this deformation is predominantly elastic and will tend to recover its original shape by eliminating tension.19 Therefore, and according to the hypothesis, the primary stability, measured in RFA and torque values, of implants placed in a bed carved with osteotomes will tend to increase with the passage of time due to the recovery of the elastic deformation suffered by the peri-implant bone.
Consequently, the objective of this trial is to evaluate the influence of the elastic behavior of peri-implant bone in the primary stability of dental implants placed using osteotomes.
Materials and methods
Samples and implants
The samples consisted of 10 cow ribs whose periosteum had been removed (measurements = 45 × 20 × 15 mm). Using a drill mounted on a handpiece, the upper cortical bone was removed while choosing locations of low-density trabecular bone, simulating bone type 3 or 4 according to the classification by Lekholm and Zarb.3 Samples were treated according to the method described by Tricio et al.,20 submerged for 5 days in a 50% ethanol saline solution at room temperature; 12 h before testing, they were stored in saline under refrigeration.
The samples were fixed in plaster blocks to avoid their displacement during the performance of the test (Fig. 1).
Figure 1.

Cow ribs samples inserted in plaster.
Two Klockner Essential Cone implants (Soadco SL, Escaldes Engordany, Andorra), 4 mm in diameter and 10 mm in length with a 1.5 mm polished neck and internal connection with a 4.5 mm platform diameter, were placed in each sample with a minimum separation of 6 mm between the platforms of both implants.
The peri-implant bed was carved by combining drilling and the use of osteotomes, preparing the bed according to the protocol established by the manufacturer: using a 1.8 mm diameter starter drill and a 2.8 mm diameter pilot drill and continuing to carve using osteotomes of 3.3 and 3.6 mm in diameter (Fig. 2).
Figure 2.

Peri-implant bed carved by the use of osteotomes.
Measurements and data collection
All implants were placed in each sample using a calibrated BTG90CN torque wrench (Tohnichi, Tokyo, Japan), and the insertion and removal torque data were recorded in Ncm (Fig. 3). The implants were placed with the entire treated surface buried in the rib and leaving only the polished neck exposed.
Figure 3.

Implants placed using a calibrated torque wrench.
The implant stability in terms of ISQ values was measured by a Penguin RFA device (Integration Diagnostic Sweden AB, Göteborg, Sweden) using a Multipeg (Integration Diagnostic Sweden AB, Göteborg, Sweden) that was screwed into the implant with a 4 to 6 Ncm torque (Fig. 4). The ISQ measurements were performed perpendicular and parallel to the rib and always perpendicular to the axial axis of the implant.
Figure 4.
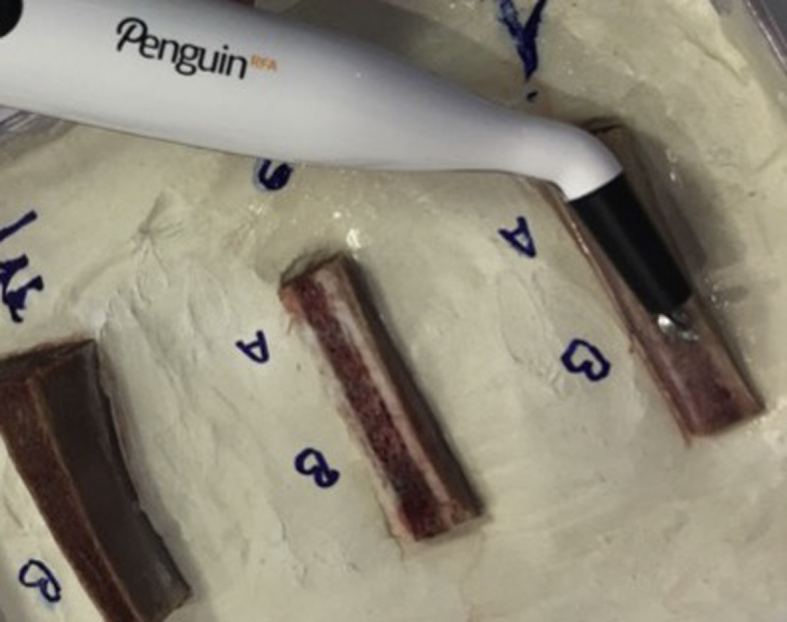
Implant stability measure by a Penguin RFA device.
Two implants were placed in each rib: one test implant (n = 10) and one control (n = 10). In the control implants, the insertion torque and initial ISQ value were measured, and the removal torque was immediately measured. In the test implants, the insertion torque and initial ISQ value were measured, and after 15 min, the ISQ value was measured again, and the removal torque was measured.
To corroborate the existence of a predominant elastic or plastic deformation of the peri-implant bone, computerized microtomographs were performed (SkyScan1174 Bruker, Kontich, Belgium) of one implant sample inserted using conventional drilling and another inserted using osteotomes. The composition of the bone trabeculae in intimate relation with the implant was evaluated using visualization and measurement software (DataViewer SkyScan Bruker, Kontich, Belgium).
Statistical analysis
A descriptive statistical analysis of the data was conducted, obtaining the mean and standard deviation of each variable.
Using the statistical package SPSS 25.0, the differences between measurements (insertion and removal torque and ISQ values) at both time points were measured using Student's t test. The statistical significance was set as p < 0.05.
Results
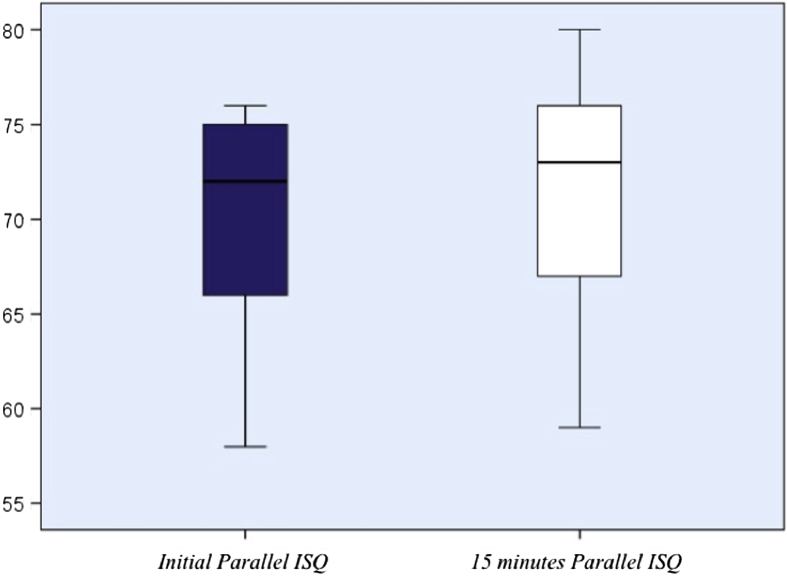
Figure 5, Figure 6, Figure 7 and Table 1 show the descriptive statistics of the study variables according to the evaluation of the control and test groups.
Figure 5.
Descriptive statistical analysis. Mean and standard deviation of parallel ISQ values.
Figure 6.
Descriptive statistical analysis. Mean and standard deviation of perpendicular ISQ values.
Figure 7.
Descriptive statistical analysis. Mean and standard deviation of torque values.
Table 1.
Descriptive statistical analysis. Mean and standard deviation of variables and subgroups.
| Insertion torque | Initial ISQ |
Initial removal torque | ISQ 15 min |
Removal torque 15 min | |||
|---|---|---|---|---|---|---|---|
| Perpend. | Parallel | Perpend. | Parallel | ||||
| Control implants (n = 10) | 15.4 ± 5.2 N/cm2 | 63.1 ± 7.3 | 69.4 ± 5.6 | 11.3 ± 4.4 N/cm2 | – | – | – |
| Test implants (n = 10) | 15.9 ± 5.9 N/cm2 | 64.4 ± 9 | 70.3 ± 5.9 | – | 66 ± 2.5 | 71.4 ± 6.4 | 12.4 ± 5.8 N/cm2 |
The average insertion torque of the control implants was 15.4 ± 5.2 Ncm, while that for the corresponding test implants was 15.9 ± 5.9 Ncm.
The initial mean ISQ value of the control implants was 63.1 ± 7.3 for the perpendicular measurement and 69.4 ± 5.6 for the parallel measurement; for the test implants it was 64.4 ± 9 for the perpendicular measurement and 70.3 ± 5.9 for the parallel measurement.
The mean immediate removal torque of the control implants was 11.3 ± 4.4 Ncm, while the mean removal torque at 15 min for the test implants was 12.4 ± 5.8 Ncm.
The mean ISQ value at 15 min for the test implants was 66 ± 2.5 for the perpendicular measurement and 71.4 ± 6.4 for the parallel measurement.
Table 2 shows comparative statistics from Student's t-test between the ISQ and torque values in both groups.
Table 2.
Comparative statistics from Student's t-test between the ISQ and torque values.
| Related differences |
t | gl | Sig. (bilateral) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Stand. Dev. | Mean tip. error | 95% difference confidence interval |
||||||
| Inferior | Superior | ||||||||
| Par 1 | ISQ_perpend_0 - ISQ_perpend_15 | −1,60000 | 1,77639 | ,56174 | −2,87075 | −,32925 | −2848 | 9 | ,019 |
| Par 2 | ISQ_parallel_0 - ISQ_parallel_15 | −1,10000 | 1,79196 | ,56667 | −2,38189 | ,18189 | −1941 | 9 | ,084 |
| Par 3 | TI - TD_0min | 3,70000 | 2,49666 | ,78951 | 1,91399 | 5,48601 | 4686 | 9 | ,001 |
Statistically significant differences were observed (p < 0.05) in the test group between the perpendicular ISQ values, with a significant increase in these values at 15 min compared to the initial moment. No significant differences were found (p > 0.05) between the parallel ISQ values at both time points and groups.
There were also statistically significant differences (p < 0.05) between the insertion torque and removal torque values at both the initial moment (control group) and at 15 min (test group), resulting in a significant decrease in the removal torque.
Discussion
As is the case for a fracture model, mechanical stabilization between the implant and its bone is critical from the point of view of achieving initial bone healing and subsequent osseointegration. In short, a lack of stabilization of the fracture edges seems to compromise the vascularization of the healing process.21 Primary stability can then be described as a type of inertia of the implant to remain in the same static state during the integration period. Indeed, several studies show that a lack of primary stability increases the risk of suffering from non-osseointegration of the implant and therefore treatment failure.22,23 Micromovements greater than 150 μm due to a lack of implant stability can produce a fibrous encapsulation or fibrointegration of the implant.7
There are some factors that compromise the achievement of correct primary stability; one is deficient bone availability, both in terms of quantity and quality. The use of osteotomes as a surgical technique for densification and bone expansion has been extensively tested and is currently one of the most used techniques for obtaining correct primary stability of implants placed in locations with low density or with a bone width deficit.24,25
Numerous clinical trials demonstrate greater primary stability in implants placed in beds worked with osteotomes compared with those carved using conventional drilling techniques.26, 27, 28
In our trial, we did not find statistically significant differences in the values of insertion torque or initial ISQ in either group, since all the implants were macro- and microscopically identical, and the peri-implant bed was carved according to the same protocol in all implants.29
The reason for the increase in primary stability when using osteotomes is because of the increase in peri-implant bone density when the bone is condensed instead of being removed by drilling. This type of behavior by the bone is a result of its elastic characteristics, since it is a material with a low Young's modulus and, above all, dense type 3 and 4 bones according to the classification of Lekholm and Zarb3 with an approximately 1 GPa modulus. According to Hooke's law, materials with a low elastic modulus will suffer a greater deformation when applying the same tension than will materials with a greater modulus. This deformation will be elastic, and therefore reversible, if the elastic limit of the material is not exceeded. If this were the case, the deformation would be plastic and therefore irreversible. Elastic deformation is defined as deformation that is reversible; therefore, when the applied tension is eliminated, the material tends to recover its original dimensions.17
When performing the technique of condensation and/or expansion using osteotomes, tension is applied to the bone, producing the elastic deformation of the bone. According to the premise mentioned above, when the implant is placed in the peri-implant bone, this bone tend, with time, to recover its primary situation and therefore stabilize the implant even more.
According to the initial ISQ values (64.4 ± 9 and 70.3 ± 5.9) of the test implants and the ISQ values at 15 min (66 ± 2.5 and 71.4 ± 6.4), all the test implants experienced an increase in ISQ values after 15 min of carving of the bed with osteotomes. Additionally, statistically significant differences were found between the perpendicular ISQ values at both time points, but not between the parallel ISQ values. This difference may be due to the size of the section of the sample in the perpendicular direction, which was much smaller than that in the parallel direction, and therefore the bone compression in this sense was less influential.
Evaluation of the computerized microtomographs of the samples showed compaction and compression of the peri-implant bone trabeculae around the implants inserted using osteotomes (Fig. 8), while it showed a greater fracture of the bone trabeculae, in addition to a considerable gap between the bone and the implants inserted using conventional drilling (Fig. 9).
Figure 8.

Computerized microtomograph of implant inserted using osteotomes.
Figure 9.

Computerized microtomograph of implant inserted using conventional drilling.
This compression of the trabeculae, which is produced by carving the bed with osteotomes, can be translated to a large extent into an elastic deformation of the bone with a tendency toward decompression and recovery of its original dimensions, which would validate the initial hypothesis of this test. However, these results do not clearly indicate that the use of osteotomes is preferable to drilling for osseointegration; to arrive at such a conclusion, it would be necessary to know if the condensation that is valued in the trabeculae can have a mechanical response only, or also by mechanisms of osteocitary mechano-perception, which is a catabolic biological response.
On the other hand, together with the increase in ISQ values in the test group, we found opposite results in the values of insertion torque (15.4 ± 5.2 Ncm for the control implants and 15.9 ± 5.9 Ncm for the test implants) and immediate removal torque of the control implants (11.3 ± 4.4 Ncm) and at 15 min for the test implants (12.4 ± 5.8 Ncm), finding statistically significant differences between the insertion torque and removal torque both immediately and at 15 min. These results may seem contradictory, but they are perfectly plausible if one considers that torque and RFA measure two types of inertia or stability in the application of different steering forces: torque is defined as the resistance of the bone to the advance of the implant when rotating around its longitudinal axis, while the RFA expresses the inertia against the application of a force that tends to generate a lateral displacement. The elastic recovery of the bone can then react differently to the combination of two forces that are essentially different. In addition, it is necessary to consider that the entrance of the implant in its bed is equivalent to the passage of a metal bar that produces the shape of the incoming thread, which justifies that the implant has a lower removal torque than insertion torque, both at the initial moment and at 15 min. It is necessary to take into consideration that it is not necessary to remove the implant for the RFA test, and thus the test is not only noninvasive but also does not change the environmental conditions during measurement.
The conflicting results obtained in the torque and ISQ values reflect, as several studies conclude, the use of RFA as a noninvasive method of evaluation of implant stability versus torque, since the latter only responds to the mechanical resistance of bone and it is possible to clinically evaluate primary stability using only the insertion torque.30,31 On the other hand, RFA can be used for the evaluation of primary stability, as well as to monitor the osseointegration process.10
The choice of the waiting time of 15 min between measurements in the test implants was confirmed by carrying out a pilot test that used the same methodology as the one developed in this article and evaluated several waiting times of 0, 5, 10, 15 and 20 min, which showed an increase in ISQ values at 15 min, and after 20 min, a maintenance and stabilization of these values was observed in all the evaluated cases. Even so, we do not know if there would be a difference in a greater period of time, and this can be interpreted as a limitation of the study.
According to the results obtained and discussed in this in vitro test, and considering the limitations inherent to it, the following conclusions can be drawn.
There are statistically significant differences in the ISQ values and insertion and removal torque of implants placed using osteotomes after 15 min of their placement.
In this sense, there is an increase in ISQ values, both perpendicular and parallel, 15 min after implant placement, with a peri-implant bed carved using osteotomes.
However, there is a lower removal torque at 15 min compared with the insertion torque of implants placed using the osteotome technique.
Lastly, in vivo tests are required to obtain more accurate conclusions, since there are many factors that can influence implant stability.
Conflicts of interest statement
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
- 1.Albrektsson T., Zarb G., Worthington P., Eriksson A.R. The long term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implant. 1986;1:1–25. [PubMed] [Google Scholar]
- 2.Sennerby L., Thomsen P., Ericson L.E. A morphometric and biomechanic comparison of titanium implants inserted in rabbit cortical and cancellous bone. Int J Oral Maxillofac Implant. 1992;7:62–71. [PubMed] [Google Scholar]
- 3.Lekholm U., Zarb G.A. Patient selection and preparation. In: Branemark P.I., Zarb G.A., Albrektsson T., editors. Tissue integrated prostheses: osseointegration in clinical dentistry. 1st ed. Quintessence; Chicago, IL: 1985. pp. 199–209. [Google Scholar]
- 4.Teughels W., Merheb J., Quirynen M. Critical horizontal dimensions of interproximal and buccal bone around implants for optimal aesthetic outcomes: a systematic review. Clin Oral Implant Res. 2009;20:134–135. doi: 10.1111/j.1600-0501.2009.01782.x. [DOI] [PubMed] [Google Scholar]
- 5.Summers R.B. A new concept in maxillary implant surgery: the osteotome technique. Compendium. 1994;15:152–160. [PubMed] [Google Scholar]
- 6.Summers R.B. Sinus floor elevation with osteotomes. J Esthet Dent. 1998;10:164–171. doi: 10.1111/j.1708-8240.1998.tb00352.x. [DOI] [PubMed] [Google Scholar]
- 7.Szmukler-Moncler S., Salama H., Reingewirtz Y., Dubruille J.H. Timing of loading and effect of micromotion on bone-dental implant interface: review of experimental literature. J Biomed Mater Res. 1998;43:192–203. doi: 10.1002/(sici)1097-4636(199822)43:2<192::aid-jbm14>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 8.Lages F.S., Douglas-de Oliveira D.W., Costa F.O. Relationship between implant stability measurements obtained by insertion torque and resonance frequency analysis: a systematic review. Clin Implant Dent Relat Res. 2018;20:26–33. doi: 10.1111/cid.12565. [DOI] [PubMed] [Google Scholar]
- 9.Andreotti A.M., Goiato M.C., Nobrega A.S. Relationship between implant stability measurements obtained by two different devices: a systematic review. J Periodontol. 2017;88:281–288. doi: 10.1902/jop.2016.160436. [DOI] [PubMed] [Google Scholar]
- 10.Meredith N., Alleyne D., Cawley P. Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implant Res. 1996;7:261–267. doi: 10.1034/j.1600-0501.1996.070308.x. [DOI] [PubMed] [Google Scholar]
- 11.Brizuela-Velasco A., Álvarez-Arenal Á., Gil-Mur F.J. Relationship between insertion torque and resonance frequency measurements, performed by resonance frequency analysis, in micromobility of dental implants: an in vitro study. Implant Dent. 2015;24:607–611. doi: 10.1097/ID.0000000000000318. [DOI] [PubMed] [Google Scholar]
- 12.Pagliani L., Sennerby L., Peterssoon A., Verrocchi D., Volpe S., Andersson P. The relationship between resonance frequency analysis (RFA) and lateral displacement of dental implants: an in vitro study. J Oral Rehabil. 2013;40:221–227. doi: 10.1111/joor.12024. [DOI] [PubMed] [Google Scholar]
- 13.Sennerby L., Andersson P., Pagliani L. Evaluation of a novel cone beam computed tomography scanner for bone density examinations in preoperative 3D reconstructions and correlation with primary implant stability. Clin Implant Dent Relat Res. 2015;17:844–853. doi: 10.1111/cid.12193. [DOI] [PubMed] [Google Scholar]
- 14.Marquezan M., Osório A., Sant'Anna E., Souza M.M., Maia L. Does bone mineral density influence the primary stability of dental implants? A systematic review. Clin Oral Implant Res. 2012;23:767–774. doi: 10.1111/j.1600-0501.2011.02228.x. [DOI] [PubMed] [Google Scholar]
- 15.Rubin C.T., Lanyon L.E. Regulation of bone formation by applied dynamic loads. J Bone Joint Surg Am. 1984;66:397–402. [PubMed] [Google Scholar]
- 16.Frost H.M. A determinant of bone architecture: the minimum effective strain. Clin Orthop. 1983;175:286–292. [PubMed] [Google Scholar]
- 17.Timoshenko S., Goodier J.N. Flat stresses and flat deformations. In: Timoshenko S., Goodier J.N., editors. Theory of elasticity. 1st ed. Mc Graw-Hill; New York: 1951. pp. 32–50. [Google Scholar]
- 18.Büchter A., Kleinheinz J., Wiesmann H.P. Biological and biomechanical evaluation of bone remodelling and implant stability after using an osteotome technique. Clin Oral Implant Res. 2005;16:1–8. doi: 10.1111/j.1600-0501.2004.01081.x. [DOI] [PubMed] [Google Scholar]
- 19.Tricio J., Van Steenberghe D., Rosenberg D., Duchateau L. Implant stability related to insertion torque force and bone density: an in vitro study. J Prosthet Dent. 1995;74:608–612. doi: 10.1016/s0022-3913(05)80313-0. [DOI] [PubMed] [Google Scholar]
- 20.Brunski J.B. Influence of biomechanical factors at the bone-material interface. In: Davies E.J., editor. The bone-biomaterial interface. 1st ed. University of Toronto Press; Toronto: 1991. pp. 391–405. [Google Scholar]
- 21.Rhinelander F.W. Tibial blood supply in relation to fracture healing. Clin Orthop Relat Res. 1974;105:34–81. [PubMed] [Google Scholar]
- 22.Pilliar R.M., Lee J.M., Maniatopoulos C. Observations of the effect of movement on bone ingrowth into porous surfaces implants. Clin Orthop. 1986;208:108–113. [PubMed] [Google Scholar]
- 23.Elnayef B., Monje A., Lin G.H. Alveolar ridge split on horizontal bone augmentation: a systematic review. Int J Oral Maxillofac Implant. 2015;30:596–606. doi: 10.11607/jomi.4051. [DOI] [PubMed] [Google Scholar]
- 24.Shalabi M.M., Manders P., Mulder J., Jansen J.A., Creugers N.H. A meta-analysis of clinical studies to estimate the 4.5-year survival rate of implants placed with the osteotome technique. Int J Oral Maxillofac Implant. 2007;22:110–116. [PubMed] [Google Scholar]
- 25.Wang L., Wu Y., Perez K.C. Effects of condensation on peri-implant bone density and remodeling. J Dent Res. 2017;96:413–420. doi: 10.1177/0022034516683932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xing Y., Khandelwal N., Petrov S., Drew H.J., Mupparapu M. Resonance frequency analysis (RFA) and insertional torque (IT) stability comparisons of implants placed using osteotomes versus drilling techniques: a preliminary case study. Quintessence Int. 2015;46:789–798. doi: 10.3290/j.qi.a34453. [DOI] [PubMed] [Google Scholar]
- 27.García-Vives N., Andrés-García R., Rios-Santos V. In vitro evaluation of the type of implant bed preparation with osteotomes in bone type IV and its influence on the stability of two implant systems. Med Oral Patol Oral Cir Bucal. 2009;14:455–460. [PubMed] [Google Scholar]
- 28.Elias C.N., Rocha F.A., Nascimento A.L., Coelho P.G. Influence of implant shape, surface morphology, surgical technique and bone quality on the primary stability of dental implants. J Mech Behav Biomed Mater. 2012;16:169–180. doi: 10.1016/j.jmbbm.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 29.Bilhan H., Geckili O., Mumcu E., Bozdag E., Sünbüloğlu E., Kutay O. Influence of surgical technique, implant shape and diameter on the primary stability in cancellous bone. J Oral Rehabil. 2010;37:900–907. doi: 10.1111/j.1365-2842.2010.02117.x. [DOI] [PubMed] [Google Scholar]
- 30.Bayarchimeg D., Namgoong H., Kim B.K. Evaluation of the correlation between insertion torque and primary stability of dental implants using a block bone test. J Periodontal Implant Sci. 2013;43:30–36. doi: 10.5051/jpis.2013.43.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nóbrega A.R., Norton A., Silva J.A., Silva J.P., Branco F.M., Anitua E. Osteotome versus conventional drilling technique for implant Site preparation: a comparative study in the rabbit. Int J Periodontics Restor Dent. 2012;32:109–115. [PubMed] [Google Scholar]