Abstract
Purpose
Fractures of distal radius are one of the common orthopaedic injuries. Placing the plate on volar surface requires release of underlying pronator quadratus (PQ) muscle. No consensus is present in the literature about the repair or not of the PQ. The purpose of this study was to evaluate the influence of PQ repair on functional outcome and complications.
Methods
Retrospectively 83 patients of distal radius fractures managed with volar plating between 2014 and 2016 were evaluated. Demographic data, operative notes and physical therapy records were retrieved. Patients were divided into group A where PQ repair was done and group B where no repair was done. Functional data such as range of motion (ROM), grip strength, visual analogue scale (VAS) score and disabilities of arm, shoulder and hand (DASH) score at 4 weeks, 3 months, 6 months and finial follow-up were retrieved.
Results
Totally 63 patients (n = 29 in group A and n = 34 in group B) with the mean age of 51.64 years were examined. Patients were followed up for a mean of 35.2 months (range 27.2–47.1 months) in group A and 38.6 months (range 28.6–51.0 months) in group B. Though functional outcome of the affected limb was not significantly different between two groups after 3 months, PQ repair did affect the recovery at an early stage. Repair group had significantly better ROM (p = 0.0383) and VAS score at 4 weeks (p = 0.017) while grip strength (p = 0.014) was significantly better at 3 months.
Conclusions
Repair of PQ may provide pain relief and increased ROM in early postoperative period and hence every attempt should be made to achieve the repair.
Keywords: Distal radius fractures; Disabilities of arm, shoulder and hand; Volar plate; Pronator quadratus; Grip strength
Introduction
Fracture of the distal radius is one of the commonest fractures seen in orthopaedics and its incidence is in an increasing trend in the ageing population because of the increased prevalence of osteoporosis.1 Distal radius fractures have a bimodal distribution, which attack the young population due to high energy trauma and the elderly due to low velocity injuries like simple fall.
Various operative and nonoperative treatment modalities are available, but every fracture is different and an ideal treatment for a given fracture type and the patients is still conjectural.2 Locking plates provide immediate stable fixation that allows early mobilization3 and may result in a more rapid recovery and improve regain of function. Placing the plate on the volar surface stabilizes the fractured distal radius by distributing the load in the subchondral bone, which minimizes the load across the fracture site by acting as a load sharing implant.4 The distal radius metaphysis is covered with transverse pronator quadratus (PQ) muscle and during the volar approach for visualization of the fracture and for plate fixation, the release of PQ from the radial end is required.5 Repairing the PQ muscle after the placement of volar plate can be quite challenging for operating surgeons because of poor tissue quality & addition of hardware. In cases of comminuted fractures there might be buttonholing of the fragments through the muscle thus making it more difficult for repair.
Some studies have shown restoration of pronation strength and increased stability of distal radioulnar joint following the repair of muscle.6 Tight closure may also lead to ischemic contracture of the muscle which will eventually affect the range of motion (ROM).7 Traditional teaching goes with whatever structures are released in the surgery requires repair in the order. We conducted this study with the hypothesis that PQ repair after volar plating should benefit the overall outcome in terms of grip strength, ROM, pain relief and disabilities of arm, shoulder and hand (DASH).
Methods
Inclusion and exclusion criteria
This study was done at a tertiary care hospital with prior approval from the institutional ethics committee. We analyzed the hospital records for distal radius fracture patients who underwent volar plating between February 2014 and June 2016 and a total of 83 patients were found during the study period. Patients with A2-C2 types of distal radius fractures according to the AO classification within the age range of 18–80 years, either male or female were included in the study. Patients with previous wrist surgeries, old distal radius fractures in the same wrist, ipsilateral shoulder & elbow injuries or traumatic brain injuries were excluded from the list. After application of the inclusion and exclusion criteria, this study consisted of 68 patients.
Grouping and functional assessment
Patients were classified into two groups: group A in which PQ was repaired and group B in which PQ was not repaired based upon the operative notes in the case files. The follow-up notes were obtained from the physiotherapy department and patients. The physical therapy at our centre is done by a team of certified hand therapist. Outpatient records and values for ROM including flexion (palmar flexion), extension (dorsiflexion), pronation and supination were collected. Grip strength measurement was done at 3 months and 6 months.
The patients were called for final follow-up and ROM measurement was done by a goniometer. The grip strength measurement was done by a hand therapist using JAMAR® Hydraulic hand dynamometer (Fig. 1). The therapists were not aware of the repair status of PQ. Pain quantification was done using visual analogue scale (VAS) score and functional assessment using DASH score.5 Patients who did not attend the clinic for final follow-up were excluded from the study.
Fig. 1.
Measure of Grip strength using Jamar dynamometer.
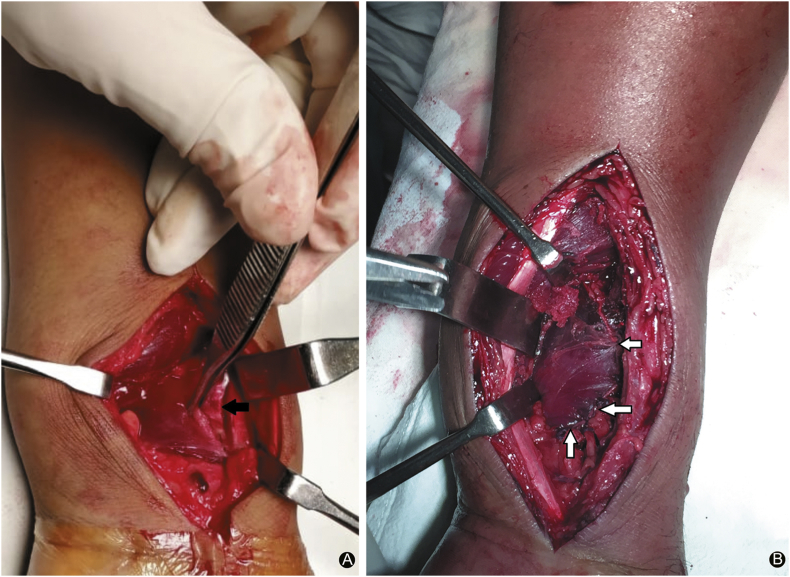
Surgical procedure
The surgeries were performed under regional block with or without supplementation of general anaesthesia. The tourniquet was used to operate under bloodless field. The distal radius was exposed using the volar flexor carpi radialis approach. After identifying the PQ, the muscle was incised longitudinally at the radial border and then elevated as a flap using a periosteal elevator (Fig. 2A). The fracture was visualised and fixed using a volar locking plate in all cases. In group A, the PQ was repaired in its anatomical location with interrupted sutures using a polyfilament, syntheticsuture (Vicryl 3-0, Ethicon) (Fig. 2B). Varying degrees of muscle injuries were observed in some cases, but repair was successful. In group B, the PQ was flipped back over its anatomical location, just to cover the implant so as to prevent injuries to flexor tendons.
Fig. 2.
(A) Pronator quadratus incision over radial border (black arrow); (B) Pronator quadratus repair done using interrupted sutures (white arrow).
Postoperative management
All the patients were given a below elbow slab with soft dressing and were encouraged to elevate the limb and begin finger movements. Patients were started on anti-oedema protocol and analgesics. Sutures were removed in 10–14 days in the outpatient department. As a routine protocol, radiographs were taken at 3 weeks and 6 weeks. Immobilization was discontinued between 1 and 2 weeks depending upon the fracture morphology and fixation; physical therapy was begun to restore wrist flexion, wrist extension and forearm rotation after discontinuation of immobilization. At 4 weeks postoperatively, patients were advised strengthening and resistance exercises, depending upon the radiograph check result and patient's tolerance. Further re-evaluation radiographs were taken. At 12 weeks postoperatively, patients were advanced to a work hardening program or discharged from therapy depending on occupational needs.
Statistical analysis
Statistical analysis was performed using SPSS statistical software version 13.0. Data were presented as mean, median, and proportion according to the underlying distribution. Continuous variables were presented as mean ± standard deviation (SD) and student's t-test was used for analysis. The p value for statistical significance was set as less than 0.05.
Results
The final study group consisted of 63 patients with 39 females and 24 males. Left side was affected in 17 patients and right side in the remaining 46 patients. The mean age of the study group was 51.64 years ranging from 26 to 78 years. The mean follow-up of patients was 35.2 months (range 27.2–47.1 months) in group A and 38.6 months (range 28.6–51 months) in group B. The demographic data of patients are given in Table 1.
Table 1.
Demographic data of patients in each group.
| Group | n (female/male) | Age (years) | Mean follow-up (month) |
|---|---|---|---|
| A (PQ repair) | 29 (18/11) | 54.86 (24–77) | 35.2 (27.2–47.1) |
| B (No PQ repair) | 34 (21/13) | 48.62 (22–72) | 38.6 (28.6–51) |
| p value | 0.089 | 0.063 | 0.381 |
Data are expressed as n or mean (range).
ROM
The assessment done at 4 weeks showed significantly greater extension, pronation and flexion in group A compared to group B. At 3 months and 6 months there was no significant difference in ROM. The mean flexion, extension, pronation and supination at the final follow-up in group A were 72°, 78°, 78° and 74° while the corresponding data in group B were 70°, 72°, 76°, 70°, respectively (Table 2).
Table 2.
Range of motion at different follow-up periods (mean ± SD).
| Follow-up time | Range of motion in degrees |
|||||
|---|---|---|---|---|---|---|
| Flexion | Extension | Pronation | Supination | Radial deviation | Ulnar deviation | |
| 4 weeks | ||||||
| Group A | 48 ± 6 | 52 ± 10 | 58 ± 12 | 62 ± 11 | 8 ± 3 | 18 ± 2 |
| Group B | 38 ± 7 | 40 ± 9 | 44 ± 9 | 60 ± 10 | 9 ± 3 | 12 ± 3 |
| p value | 0.046* | 0.038* | 0.029* | 0.821 | 0.967 | 0.092 |
| 3 months | ||||||
| Group A | 62 ± 11 | 74 ± 9 | 74 ± 6 | 68 ± 11 | 14 ± 4 | 32 ± 6 |
| Group B | 66 ± 8 | 66 ± 11 | 74 ± 8 | 64 ± 9 | 16 ± 2 | 32 ± 7 |
| p value | 0.671 | 0.062 | 0.000 | 0.071 | 0.623 | 0.000 |
| 6 months | ||||||
| Group A | 70 ± 12 | 76 ± 7 | 74 ± 6 | 72 ± 6 | 16 ± 6 | 32 ± 6 |
| Group B | 68 ± 11 | 72 ± 9 | 68 ± 6 | 72 ± 6 | 16 ± 6 | 28 ± 6 |
| p value | 0.938 | 0.079 | 0.072 | 0.000 | 0.000 | 0.086 |
| Final follow-up | ||||||
| Group A | 72 ± 6 | 78 ± 5 | 74 ± 6 | 78 ± 6 | 18 ± 8 | 30 ± 9 |
| Group B | 70 ± 4 | 72 ± 6 | 70 ± 8 | 76 ± 4 | 16 ± 7 | 28 ± 6 |
| p value | 0.836 | 0.074 | 0.168 | 0.319 | 0.729 | 0.826 |
Note: * means significant difference between PQ repair and not repair groups.
VAS score
At 4 week follow-up, VAS score between 0 and 4 was seen in 74% of patients in group A and 56% of patients in group B (p = 0.023); and at final follow-up VAS between 0 and 2 was seen in >93% patients of both groups, showing no clinical significance (p = 0.310).
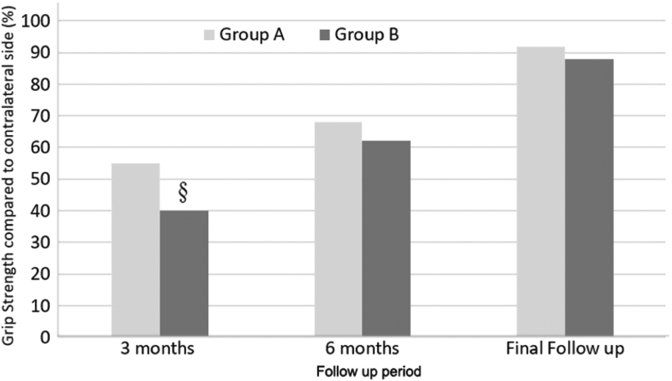
Grip strength
The mean grip strength in group A was significantly higher at 3 months, i.e. 55% (38%–72%) of the contralateral limb than that in group B, i.e. 40% (28%–62%) (p = 0.014). At 6 months, the grip strength showed a significant improvement in both groups, and the final results showed that the affected limb achieved >85% grip strength compared to the contralateral limb in both groups (Fig. 3). No significant difference was found between patients with PQ repair or not after 6 months.
Fig. 3.
Grip strength at different follow-up period. §: Statistically significant lower grip strength is seen in group B at 3 months (p < 0.05).
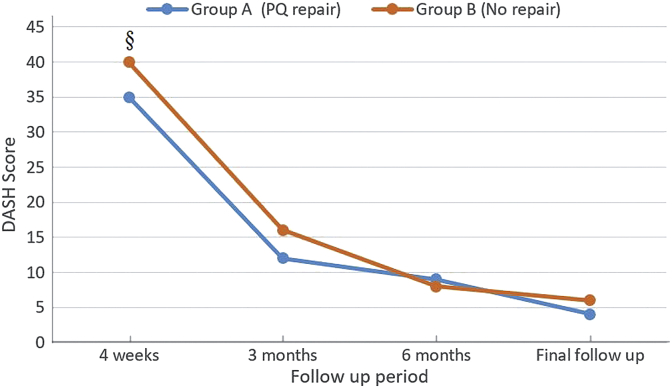
DASH score
At postoperative 4 weeks, the mean DASH score was 31 (range 18–52) in group A and 46 (range 16–64) in group B (p = 0.033). At 12 weeks the limb function improved and DASH score decreased to 12 (range 6–21) in group A and 16 (range 9–26) in group B (p = 0.746). At final follow-up, the mean DASH score was significantly improved to 4 (0–13) in group A and 6 (0–11) in group B (p = 0.623) (Fig. 4).
Fig. 4.
DASH scores at different follow-up periods. §: Statistically significant higher DASH score is seen in group B at 4 weeks (p < 0.05).
Discussion
Whether to repair or not to repair the PQ after volar fixation has been a question for a while with no definitive answer. Repair of the PQ can be quite challenging due to various reasons such as traumatic rupture, button hole of fragments through the muscle, inadequate muscle cuff to be repaired on the radial end and bulk of the implant. Many authors in their studies have found that repair of PQ may provide benefit to the flexor tendons from attrition injury during wrist flexion,7,8 although cases of late tendon irritation even after PQ repair have been reported9 and some studies concluded placement of volar plate distal to watershed line as an important risk factor for flexor tendon rupture.10, 11, 12 In recent literature technique sparing PQ and sliding the plate from distal end has been described.13
In our study, the range of pronation, flexion and extension was significantly lower (p = 0.038) in group B (no repair) than in group A (repair) at 4 weeks. There was no significant difference in ROM at 6 months and final follow-up between two groups. The grip strength at 3 months was significantly lower in group B than in group A (p = 0.014). The power analysis yielded around 68% grip strength and 76% pronation at 6 months follow-up. Significant lower DASH score was found in group A (DASH = 31) than in group B (DASH = 46) at 3 months (p = 0.033), which was improved in subsequent follow-ups. The final follow-up demonstrated near normal pre-injury ROM (comparable to contralateral side) and DASH score <2 in both groups which indicate almost no upper extremity disability and excellent overall functional outcome despite clinically significant differences in the early follow-up.
Our findings are comparable to those published in the literature. Tosti et al.14 conducted a double blinded prospective trial of PQ repair vs. no repair in 60 patients with distal radius fractures. At follow-up of 6 months the authors found significantly higher grip strength in repair group as compared with no repair group, however, at 12 months follow-up there was no significant difference between two groups regarding ROM at the wrist, DASH scores, grip strength, and VAS scores.
Huh et al.15 in a study of 34 patients fixed with volar locking plates for distal radius fractures demonstrated reduced isokinetic pronation and supination strength at 6 months in the surgery forearm compared to normal side, which was not significant at 12 months postoperatively. The authors concluded that dissection of PQ has minimal impact on function.
In a retrospective study of 108 patients by Ahsan et al.16 with complete and incomplete PQ repair found no significant difference in ROM, grip strength at a mean follow-up of 3 months.
Mulders et al.17 in a systemic review reported 169 patients with distal radius fractures. Among them 95 patients underwent PQ repair and 74 did not. At 12 months follow-up authors found no statistically significant differences regarding functional outcomes and complications no matter PQ muscle was repaired or not after volar plate fixation.
Few studies16,18 comparing complete and incomplete PQ repair has concluded that at least an incomplete repair helps prevent flexor tendon irritation and rupture. We found that just placing the PQ over its anatomical location without any repair with sutures also yielded the same result and incomplete suture repair is not better than no repair.
There was one case with flexor pollicis longus rupture in group B at 6 month follow-up. The patient denied for any surgical intervention. There were no cases of flexor tenosynovitis in both groups at 12 months and similar results have been shown in literature.16
The incidence of flexor pollicis longus tendon rupture has been reported to range from 2% to 12% with the rupture occurring as early as 4 months or as late till 68 months.4,18 Studies have demonstrated a lower rate of flexor tendon complications associated with volar plating, but rates have still been reported as high as 16%.10 Some studies have demonstrated that flexor tendon rupture can even occur with PQ repair and have attributed it to volar plate placement distal to the watershed line which increases contact pressure between the plate tendon interface.12,19 However, few studies found correlation between placement of plate as an independent risk factor for flexor tendon rupture.20 In this study all the volar plates were placed proximal to watershed line and the incidence of flexor tendon rupture was 2.9%, but the actual incidence can go higher in a longer term follow-up as incidence of late flexor tendon ruptures has been reported.21
We encountered a case of complex regional pain syndrome in group A at 8 week follow up. Patient was managed with analgesics and gabapentin and physiotherapy. On further follow-up the patient improved at 3 months, but at final follow-up this patient had a low grip strength and ROM and a high DASH score (DASH = 13).
The significant decrease in pain after PQ repair (group A compared to group B) at 4 weeks could be explained by the fact that volar plate has a better coverage in group A, thus there will be less flexor tendon irritation in the early healing period of muscle. However, at final follow-up the VAS score in both groups were comparable.
This study has some limitations. The PQ repair may influence the pronation strength which has not been assessed objectively. No fixed protocol was followed for immobilization as the study had vast diversity in the patient's characteristics. The quality of reduction using radiological parameters was not taken into assessment which may influence the pain, functional outcome and thereby the DASH score.
In conclusion, although repair of PQ does not affect the final functional outcome statistical difference in pain and ROM appear in the early period after surgery, which increases the compliance for early postoperative rehabilitation thereby improved ROM and hence every attempt should be made to repair PQ.
Funding
Nil.
Ethical statement
Approval has been obtained from the institutional ethics committee before conduction of this study.
Conflicts of interest
The authors report no conflicts of interest concerning the materials or methods used in this study or the findings specified in this paper.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Nellans K.W., Kowalski E., Chung K.C. The epidemiology of distal radius fractures. Hand Clin. 2012;28:113–125. doi: 10.1016/j.hcl.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lichtman D.M., Bindra R.R., Boyer M.I. Treatment of distal radius fractures. J Am Acad Orthop Surg. 2010;18:180–189. doi: 10.5435/00124635-201003000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Drobetz H., Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop. 2003;27:1–6. doi: 10.1007/s00264-002-0393-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berglund L.M., Messer T.M. Complications of volar plate fixation for managing distal radius fractures. J Am Acad Orthop Surg. 2009;17:369–377. doi: 10.5435/00124635-200906000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Orbay J., Badia A., Khoury R.K. Volar fixed-angle fixation of distal radius fractures: the DVR plate. Tech Hand Up Extrem Surg. 2004;8:142–148. doi: 10.1097/01.bth.0000126570.82826.0a. [DOI] [PubMed] [Google Scholar]
- 6.Johnsons R.K., Shrewsbury M.M. The pronator quadratus in motions and in stabilization of the radius and ulna at the distal radioulnar joint. J Hand Surg. 1976;1:205–209. doi: 10.1016/s0363-5023(76)80039-1. [DOI] [PubMed] [Google Scholar]
- 7.Rhee P.C., Dennison D.G., Kakar S. Avoiding and treating perioperative complications of distal radius fractures. Hand Clin. 2012;28:185–198. doi: 10.1016/j.hcl.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Orbay J.L. The treatment of unstable distal radius fractures with volar fixation. Hand Surg. 2000;5:103–112. doi: 10.1142/s0218810400000223. [DOI] [PubMed] [Google Scholar]
- 9.Brown E.N., Lifchez S.D. Flexor pollicis longus tendon rupture after volar plating of a distal radius fracture: pronator quadratus plate coverage may not adequately protect tendons. Eplasty. 2011;11:e43. [PMC free article] [PubMed] [Google Scholar]
- 10.Arora R., Lutz M., Hennerbichler A. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007;21:316–322. doi: 10.1097/BOT.0b013e318059b993. [DOI] [PubMed] [Google Scholar]
- 11.Cross A.W., Schmidt C.C. Flexor tendon injuries following locked volar plating of distal radius fractures. J Hand Surg. 2008;33:164–167. doi: 10.1016/j.jhsa.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 12.Soong M., Earp B.E., Bishop G. Volar locking plate implant prominence and flexor tendon rupture. J Bone Jt Surg. 2011;93:328–335. doi: 10.2106/JBJS.J.00193. [DOI] [PubMed] [Google Scholar]
- 13.Remedios C., Nebout J., Benlarbi H. Pronator quadratus preservation for distal radius fractures with locking palmar plate osteosynthesis. Surgical technique. Chir Main. 2009;28:224–229. doi: 10.1016/j.main.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 14.Tosti R., Ilyas A.M. Prospective evaluation of pronator quadratus repair following volar plate fixation of distal radius fractures. J Hand Surg. 2013;38:1678–1684. doi: 10.1016/j.jhsa.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Huh J.K., Lim J.Y., Song C.H. Isokinetic evaluation of the pronation after volar plating of a distal radius fracture. Injury. 2012;43:200–204. doi: 10.1016/j.injury.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Ahsan Z.S., Yao J. The importance of pronator quadratus repair in the treatment of distal radius fractures with volar plating. Hand. 2012;7:276–280. doi: 10.1007/s11552-012-9420-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mulders M.A., Walenkamp M.M., Bos F.J. Repair of the pronator quadratus after volar plate fixation in distal radius fractures: a systematic review. Strategies Trauma Limb Reconstr. 2017;12:181–188. doi: 10.1007/s11751-017-0288-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jupiter J.B., Marent-Huber M., LCP Study Group Operative management of distal radial fractures with 2.4-millimeter locking plates: a multicenter prospective case series. J Bone Joint Surg Am. 2009;91:55–65. doi: 10.2106/JBJS.G.01498. [DOI] [PubMed] [Google Scholar]
- 19.Tanaka Y., Aoki M., Izumi T. Effect of distal radius volar plate position on contact pressure between the flexor pollicis longus tendon and the distal plate edge. J Hand Surg. 2011;36:1790–1797. doi: 10.1016/j.jhsa.2011.08.027. [DOI] [PubMed] [Google Scholar]
- 20.White B.D., Nydick J.A., Karsky D. Incidence and clinical outcomes of tendon rupture following distal radius fracture. J Hand Surg. 2012;37:2035–2040. doi: 10.1016/j.jhsa.2012.06.041. [DOI] [PubMed] [Google Scholar]
- 21.Nunley J.A., Rowan P.R. Delayed rupture of the flexor pollicis longus tendon after inappropriate placement of the π plate on the volar surface of the distal radius. J Hand Surg. 1999;24:1279–1280. doi: 10.1053/jhsu.1999.1279. [DOI] [PubMed] [Google Scholar]