Highlights
-
•
Some prolonged seizures (even nonconvulsive) can cause neuronal damage and warrant aggressive treatment.
-
•
Highly sedating anti-seizure drugs can also cause morbidity and should be avoided when possible.
-
•
Treatment aggressiveness should be tailored the type of SE and its refractoriness.
-
•
Some flexible ‘‘experience-based” recommendations are made for treatment of refractory SE.
Abstract
This article presents a “debate” about the appropriate level of aggressiveness of treatment for nonconvulsive status epilepticus (NCSE), held at the International Congress of Clinical Neurophysiology in Washington D.C. on 4 May 2018. The proposition for discussion was “Nonconvulsive seizures and status epilepticus in the intensive care unit should be treated aggressively.” Dr. Andrea O. Rossetti from Lausanne, Switzerland, spoke in support of the proposition and Dr. Lawrence J. Hirsch from New Haven, Connecticut, discussed reasons for rejecting the proposal. Dr. Frank W. Drislane from Boston, Massachusetts, was asked by the conference organizers to add comments and perspective.
1. Dr Andrea O Rossetti
1.1. Pro: nonconvulsive seizures and status epilepticus in the intensive care unit should be treated aggressively
Electrical seizures are rhythmic or periodic EEG alterations with evolution of field, amplitude and frequency over at least 10 s, while focal status epilepticus (SE) is defined as prolonged seizures (or repeated self-limited events without return to baseline clinical conditions) lasting at least 5 min (for tonic-clinic seizures, which may evolve into nonconvulsive SE in coma), or 10 min (for nonconvulsive seizures, or focal SE with or without impaired consciousness or cognitive dysfunction). In that definition, a second temporal threshold at 30–60 min is correlated with the risk of neuronal damage (Trinka et al., 2015). It is essentially to prevent this risk that a consequent seizure and SE treatment is justified.
While seizures or SE occur in up to 50% of critically ill patients with altered consciousness (Sutter, 2016), in more than 80% they present without movements (Claassen et al., 2004). It appears therefore mandatory to consider EEG recordings very liberally in this clinical setting; however, it is of utmost importance to underscore that patients with a severe underlying structural brain damage will do poorly even with the best and most aggressive antiepileptic drugs (AED) treatment (Bauer and Trinka, 2010). The tight interplay between electrical and anatomical dysfunction needs always to be considered.
Since the seminal observations by Meldrum and colleagues nearly half a century ago indicating that prolonged seizures could cause neurologic damage (Meldrum and Horton, 1973), additional evidence has linked seizures (Palmio et al., 2008) and SE (DeGiorgio et al., 1999) to neuronal damage as, for example, indicated by elevated levels of neuron-specific enolase. Microdialysis demonstrated that the local metabolic balance is severely disrupted during seizures or periodic discharges in brain-injured patients (Vespa et al., 2016, Witsch et al., 2017). Furthermore, from a more epidemiological point of view, seizure density over time correlates with increased risk of poor cognitive and neurological outcome, both in children (Payne et al., 2014) and adults (DeMarchis et al., 2016). In addition, occurrence of electric seizures or periodic discharges (as detailed in Hirsch et al., 2013) has been independently associated to poor outcome in medical (Oddo et al., 2009) and neurological critical care patients (Claassen et al., 2007), and to development of hippocampal atrophy following brain trauma (Vespa et al., 2010).
A groundbreaking observation of 15 years ago showed that in critically ill patients at least 48 h of continuous EEG are needed in order to capture more than 90% of epileptic events (Claassen et al., 2004). Recent high-quality work, mostly involving my opposer, Dr Hirsch, has identified several variables modulating the seizure risk in this clinical situation. Lateralized periodic discharges on EEG occurring at some point are directly correlated with the occurrence of clinical seizures (not necessarily at the same time) depending on their frequency, while generalized periodic discharges or lateralized rhythmic delta activity seems to bear an association with frequencies only above 1.5 Hz (Rodriguez Ruiz et al., 2017). In a constellation of lack of previous seizures, concurrent coma, and lateralized periodic or rhythmic delta activity, 20 min of EEG recordings seem reasonable (Struck et al., 2017a, Shafi et al., 2012), while indeed up to 48 h seem required if several of the above mentioned features are at play. A useful seizure-risk predicting tool (using the eponym of “2HELPS2B”) has been proposed (Struck et al., 2017b). Of course, application of the current ACNS EEG nomenclature is strongly encouraged (Hirsch et al., 2013).
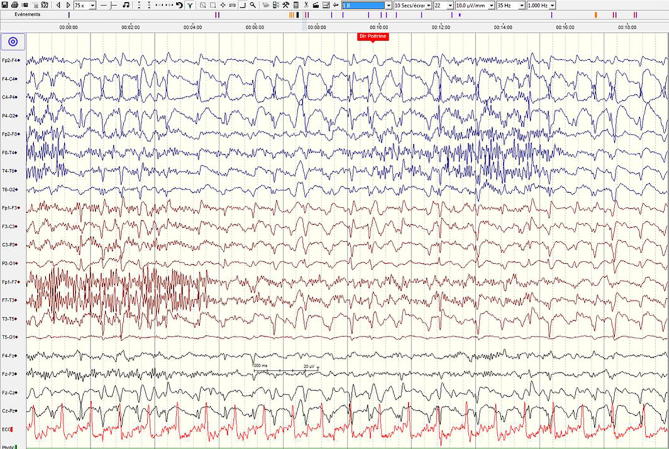
Despite this information, one may continue to face considerable challenges regarding the optimal management of these patients. For example, a middle aged lady still comatose 6 days after subarachnoid bleeding from a right middle cerebral artery aneurysm was found on continuous EEG to have intermittent episodes of right sided rhythmic delta slowing with intermixed sharp transients (LRDA + S, 1.5 Hz), but not clear-cut seizures (see Fig. 1). The structural damage was moderate and confined to the non-dominant hemisphere. A few days after receiving antiepileptic drugs (AEDs: levetiracetam, lacosamide, and small benzodiazepine doses) she started following commands. Retrospectively, this constellation, which at first glance does not seem to represent nonconvulsive SE, may fulfil its most recent definition, requiring response to treatment in doubtful cases (Leitinger et al., 2016). This illustrates the practice, admittedly relying on weak evidence, of considering introducing non-sedating AEDs in the presence of these EEG findings on the ictal-interictal continuum (see: Chong and Hirsch, 2005), and the good clinical evolution suggests a causal relationship.
Fig. 1.
48 year old woman with subarachnoid bleeding and coma persisting after 6 days. The EEG (average referential montage, 20 mm/sec) shows intermittent right-sided lateralized rhythmic delta activity with superimposed sharp elements (LRDA + S). [In these figures, right-sided channels are displayed on the top, in red lines; left, on bottom, in blue.]
In any case, compelling evidence seems to favour a consequent treatment of electrographic seizures and SE in critical care patients, in order to prevent permanent neuronal injury.
2. Dr Lawrence J Hirsch
2.1. Con: nonconvulsive seizures and status epilepticus in the intensive care unit should NOT be treated aggressively
My position can be summarized by the statement that “nonconvulsive seizures and status epilepticus should be diagnosed and treated as quickly as possible but are often overtreated.” I concede many points about NCSE, most already made by Dr. Rossetti: most seizures in the ICU are nonconvulsive and require EEG to recognize; NCSE is often harmful to neurons, especially in the setting of acute brain injury; the earlier seizures of all types are recognized, the more likely they are to respond, with early treatment leading to shorter hospital stays and better outcome; and many highly epileptiform patterns (periodic discharges of any location [GPDs, LPDs, lateralized rhythmic delta activity [LRDA], and brief potentially ictal rhythmic discharges [BIRDs]) are strongly associated with definite clinically evident seizures (as reviewed in Osman, 2018). However, this is sometimes misunderstood to mean that those patterns are themselves seizures and need to be treated. They do not -- they simply represent a risk for seizures, a need to be vigilant (usually with ongoing continuous EEG monitoring), and typically lead to use of prophylactic anti-seizure drugs (ASDs), especially if real-time EEG monitoring cannot be performed.
Dr. Rossetti quoted the literature that has shown that prolonged seizures (NCSE) or a high seizure burden are independently associated with worse outcomes, short-term and long-term. However, it is important to note that this was not shown in all studies; for example, neither seizures nor NCSE were significant predictors of outcome in a large study of patients with intracerebral haemorrhage (Claassen et al., 2007). In addition, it is important to note that several of the cited studies showed that isolated seizures are not harmful. In the Topjian et al. study from Toronto, where NCSE was associated with higher mortality and neurological worsening, isolated seizures showed no association with outcome (Topjian et al., 2013). In the Wagenman et al. series from Philadephia, multivariate analysis showed the same: NCSE was associated with worse outcome, but isolated seizures were not (Wagenman et al., 2014). Finally, in the Payne et al. publication (Payne et al., 2014), a seizure burden of <20% was not associated with worse outcome at all (57% declined neurologically, vs 60% in the matched group with no seizures), though higher burdens were (>90% declined).
From this discussion, it should be clear that at least some seizure activity can probably be tolerated, especially if not easily stopped. What about the safety of our aggressive treatments? Twenty years ago, a study compared outcomes in two groups of elderly patients with nonconvulsive status epilepticus: one with advance directives managed without ICU care and without IV benzodiazepines, and the other managed more aggressively with IV benzodiazepines of some kind (Litt et al., 1998). The mean hospitalization duration was 39 days in the IV benzodiazepine group and 22 days in the other. More importantly, the use of IV benzodiazepines was associated with an increased risk of death (p = 0.03). More recently, there have been several retrospective studies that have found that IV anesthetic drips used for treatment of refractory SE (RSE) are associated with worse outcomes. Sutter et al. reviewed 171 consecutive patients with RSE, excluding those post-cardiac arrest (Sutter et al., 2014). The use of continuous IV anesthetic-dose anti-seizure medications was associated with higher mortality, intubation, hypotension and poor function with long-term outcome. {I will note that these findings were no longer significant when accounting for the severity of RSE.} Marchi et al. (with my opposer, Dr. Rossetti, as senior author) reviewed 415 cases of SE lasting >30 min, and found that therapeutic coma was associated with worse outcome at hospital discharge, new disability (with a relative risk, RR of 4.6), mortality (RR 5.5), more infections, and longer hospital stays (Marchi et al., 2015). While the association with worsened outcomes does not prove causality, it should at least make us concerned about their use.
Although there are no randomized trials comparing aggressive to non-aggressive treatment of RSE, Alvarez et al. took advantage of a natural difference in treatment practices in two different centers to examine this effect (Alvarez et al., 2016). They reviewed 126 cases of RSE treated in Boston to 236 cases treated in Lausanne, Switzerland at Dr. Rossetti’s institution. Despite similar scores on the Status Epilepticus Severity Score, therapeutic coma was used in 25% of patients in Boston, but in only 10% in Lausanne (it seems that Dr. Rossetti’s team is not so aggressive after all, at least compared with the one in Boston). There was no difference in mortality, but therapeutic coma was associated with increased hospital length of stay. Lastly, even in a study of 31 cases of super-refractory SE treated with IV pentobarbital that concluded that “continuous IV pentobarbital effectively aborts super-refractory SE and complications are infrequent” (Pugin et al., 2014), there were many complications and poor outcome: 1/3 of patients had pneumonia; vasopressors were needed in almost 1/3; there was 1 propylene glycol toxicity and 1 cardiac arrest; and 90% of patients had poor outcomes: 74% died and 16% were severely disabled. This is a good reminder of a quote from Max Lerner: “When you choose the lesser of two evils, always remember that it is still an evil.” Refractory SE is bad, but some of our treatments are occasionally as bad or worse.
In the past few years, I have seen several cases where patterns thought to be potentially ictal (on the “ictal-interictal continuum” were treated in a prolonged and aggressive fashion, and only after stopping this did the patient wake up. I completely agree that many of these patterns (typically with periodic discharges and/or rhythmic delta between 1 and 2.5 Hz with fluctuations or equivocal evolution) deserve an IV anti-seizure drug trial, including those with so-called “triphasic waves” (O'Rourke et al., 2016), as many will indeed represent NCSE and significant fraction will improve clinically with such a trial (Hopp et al., 2011). However, many will not, and one should aggressively avoid over-aggressive treatment that can cause more harm than the underlying illness. There are similarly confusing and highly epileptiform patterns that come and go without treatment upon withdrawal from anesthesia, especially barbiturates and propofol (Das et al., 2018).
In summary, diagnose and treat quickly, but in the end, make sure the treatment is truly necessary, and avoid being too aggressive or treating for too long. First, do no harm.
3. In response to Dr Hirsch’s comments Dr Rossetti added
Dr Hirsch mentioned excellent points, and it is of no doubt that one has to avoid being too aggressive in every single case, as indeed at times “the cure may be worse than the disease” (Kaplan, 2000).
Nevertheless, as treating physicians, it seems more than reasonable to attempt what is in one’s power in order to help the patient, before giving way to nihilistic thoughts. A practical example will illustrate this. A 42 year old woman suffered cardiac arrest due to a severe myocardial infarction. She had ventricular fibrillation and a relatively prolonged time to return of a spontaneous rhythm of 36 min. Soon after normothermic temperature management and sedation weaning, she started having subtle erratic myoclonus. Her EEG showed a continuous, poorly developed theta background with superimposed periodic generalized discharges having a maximum over the vertex and right central regions (GPDs 1–2 Hz; see Fig. 2). Importantly for her prognosis, discharges were not of high voltage and the background was reactive to stimulation (Elmer et al., 2016, Aicua Rapun et al., 2017), suggesting a potentially treatable condition. On top of propofol, she received levetiracetam, and valproate. Multimodal work-up did not identify any robust feature heralding poor outcome (Rossetti et al., 2009, Rossetti et al., 2016). She recovered brainstem reflexes; early cortical somatosensory evoked potentials were recorded bilaterally; and serum neuron-specific enolase levels were below 30 µmol/l. After several days of sedation and continuing AED treatment, she slowly emerged from coma, and was responsive to commands on day 17 (see Fig. 3); she recovered to the baseline after 3 months, still on levetiracetam and valproate.
Fig. 2.
42 year old woman with cardiac arrest. The EEG 27 h later (bipolar longitudinal montage, 30 mm/sec) shows periodic sharp waves (GPDs) somewhat more prominent or the right, superimposed on an irregular theta background that appears reactive upon pain stimulation (red mark).
Fig. 3.
(Same patient as in Fig. 2) 17 days after cardiac arrest, treated with levetiracetam and valproate, she interacts with the environment; her EEG shows a poorly developed diffuse theta activity that reacts promptly upon stimulation, accelerating towards alpha frequencies.
This patient highlights the fact that SE has been found to independently modulate prognosis of the underlying etiology, not only post-anoxic ischemic brain damage (Rossetti et al., 2007), but also stroke (Knake et al., 2006). Even patients having SE without identifiable cause are at higher mortality risk that those after a single seizure in similar situations (Logroscino et al., 2008). Once again, leaving these patients without a robust AED and at times anesthetic treatment may expose them to an increased risk of morbidity and mortality.
4. In response to Dr Rossetti’s comments Dr Hirsch added
I completely concur with Dr. Rossetti’s point that convulsive SE needs to be treated aggressively in almost all cases, including postanoxic SE of all types -- as shown most clearly in a paper that came out after our debate, showing that aggressive treatment of postanoxic refractory SE led to good outcome in 44% of 36 patients (Beretta et al., 2018). Nonetheless, as shown by Rossetti et al. (2007), having SE after cardiac arrest is still likely a significant predictor of worse outcome (relative risk of 6 for worse outcome), but is certainly not a guarantee of bad outcome and should still be treated early and aggressively. Presence of SE is also a much less robust predictor of outcome than other measures such as exam and SSEPs (Sandroni et al., 2014). My thinking on this is that the status epilepticus prevents proper examination and assessment of the patient until it is stopped. Thus, to give the patient a chance to wake up, one must stop the seizures in order to assess the extent of underlying brain damage from anoxia. However, this is not to say that postanoxic SE is a good prognostic sign by any means, or that one should be aggressive with occasional brief seizures or with periodic discharges at <1.5–2 Hz. In general, I would tolerate those or treat only with non-sedating medications rather than escalating anesthetic-dose medications.
5. Dr Frank W Drislane’s comments
As nonconvulsive seizures and status epilepticus (NCSE) have become more and more frequently diagnosed, especially in ICU patients, treatment decisions have become increasingly complicated. Almost all neurologists agree that such seizures and prolonged epileptic states should be treated, but it is difficult to decide which medications to use, whether and for how long to use highly sedating anti-seizure drugs (ASDs), and how to transition to less sedating drugs. This perspective will focus on (1) different forms of SE requiring different treatments and (2) effort that should be made to shorten ICU stays.
5.1. Different types of status epilepticus; different treatments
As the famed electroencephalographer Ernst Niedermeyer, said years ago, “There is no one illness called epilepsy. There are many epilepsies,” there are also many forms of status epilepticus (SE) and NCSE, several of which require different, individualized treatments. Even criteria for diagnosing the many forms of NCSE are controversial, although recent guidelines and criteria from the American Clinical Neurophysiology Society (Hirsch et al., 2013), Salzburg criteria (Leitinger et al., 2015), and ILAE (Trinka et al., 2015) are of great value.
In 1999, Lowenstein et al. (1999) proposed the temporal criterion of 5 min for generalized convulsive SE (GCSE), an “operational” definition designed to help diagnose and treat SE expeditiously. It often seems forgotten that this proposal applied to GCSE alone, but it has been used by some (if without demonstrated validity) for all types of SE.
The 2015 ILAE definitions acknowledge that there are different forms of NCSE, likely warranting different temporal criteria and, by implication, different intensities of treatment. The ILAE time, ‘t1’ (beyond which seizures are unlikely to stop on their own) is also 5 min for GCSE, and 10 min for absence SE (and for complex partial SE or ‘focal SE with impaired awareness (or consciousness),’ but completely speculative for other forms of NCSE.
5.2. Other forms of status epilepticus
Other forms of SE (some considered convulsive, and some nonconvulsive) include myoclonic SE. MSE may occur in the ‘benign’ primary ‘idiopathic’ generalized epilepsies (IGE), e.g. absence or juvenile myoclonic epilepsy (Koutroumanidis, 2018, Serafini et al., 2018), where gentle treatment with previously used ASDs (but usually not sodium channel drugs) or low doses of benzodiazepines (BDZs) is often sufficient. In other conditions such as Lennox Gastaut syndrome (LGS), with severe or progressive encephalopathies, ASDs may halt the SE, but patients often return to a poor baseline. In progressive myoclonus epilepsies (e.g. storage diseases) and “symptomatic” MSE (due to severe toxic, metabolic, or infectious encephalopathies) the EEG shows an encephalopathy, occasionally with epileptic features; valproate and BDZs may control the myoclonus, but the outcome depends more upon treatment of the underlying illness, and highly-sedating drugs are best avoided.
Among the unusual forms of NCSE seen primarily in children, atypical absence SE tends to occur in LGS, manifested by a (further) reduction in cognitive function, and a slower, often ∼2.5 Hz, “slow-spike-and-wave” pattern on EEG (Nolan et al., 2005). ASDs may halt seizures, but patients often return to a poor baseline. Electrical status epilepticus in sleep (ESES) implies activation by sleep of persistent epileptiform activity suggestive of SE, though not all these children have clinical seizures. With an associated clinical ESES syndrome, there is some evidence that treatment of the frequent discharges may improve long-term outcome (Riviello, 2018).
Absence SE (Lennox, 1945), simple partial SE or aura continua i.e. prolonged or recurrent epileptic sensory phenomena (Penfield and Jasper, 1954), and CPSE with confusion, fluctuating abnormal behavior, and even unresponsiveness (Gastaut and Roger, 1956) have been recognized for over 50 years. CPSE more often becomes refractory than does absence SE. There are also several forms of “focal-onset NCSE with dyscognitive features” including ‘ictal’ aphasia, hemianopia, dysmnesia, and neglect syndromes (Krishnan et al., 2018), with maintained alertness.
5.3. “Non-classic” nonconvulsive status epilepticus
The forms of NCSE described above constitute the ‘classic’ types of NCSE – absence SE and similar forms of generalized NCSE on the one hand, and focal-onset NCSE with altered awareness or dyscognitive features on the other. Most are related to prior epilepsy syndromes. Over the last two decades, however, increasing numbers of cases of NCSE are not of these ‘classic‘ types, but rather related to acute and serious medical, neurologic, or traumatic illnesses -- occasionally superimposed upon epilepsy syndromes but more often arising anew during an acute illness. For this “non–classic” NCSE (Drislane, 2018), ILAE definitions could not assign a definite ‘t1’ or ‘t2’ specifying the urgency of treatment. They are likely the most common types of NCSE found by continuous EEG monitoring (C-EEG) in ICUs -- and include many or most of the cases Drs Rossetti and Hirsch covered in their discussions.
Many NCSE patients with generalized discharges on EEG (but without prior IGEs) have been labeled as in ‘absence’ SE (incorrectly), but actually have secondarily generalized SE (DeLorenzo et al., 1996, Thomas et al., 1999), often precipitated by other underlying illnesses. Classic absence SE is relatively uncommon and usually responds readily to ASDs; secondarily generalized NCSE is harder to treat and usually carries the prognosis of the underlying illness.
Probably the most important “non-classic” NCSE is the continuation of SE after unsuccessful (and often inadequate) treatment of GCSE, a relatively common finding on C-EEG monitoring. Many of these patients have minimal or no motor signs (DeLorenzo et al., 1998) and are referred to as in “subtle GCSE” (Treiman et al., 1990). Most epileptologists agree that this NCSE is a later stage of GCSE in terms of pathophysiology and clinical implications and should be treated urgently, and aggressively if necessary.
Prolonged “non-classic” NCSE is not rare. Even before the era of C-EEG, one group found that of 164 patients with apparently-controlled GCSE, 14% were in NCSE (DeLorenzo et al., 1998) and that of 236 comatose patients with no clinical evidence of seizures, 8% were in NCSE (Towne et al., 2000). Summarizing many studies of critically ill patients with various illnesses (infection, stroke, trauma, etc), about 20% of patients on C-EEG had frequent nonconvulsive seizures, or often, NCSE (Herman et al., 2015).
These patients have been described as in “subtle GCSE” or electrographic status epilepticus (Drislane and Schomer, 1994). Others refer to “NCSE in coma” -- but there are many levels of ‘impaired awareness,’ not just coma (“generalized NCSE in sick patients” might be better). Some are labeled as having “epileptic encephalopathies,” because the underlying illness causes the discharges, but this term is probably best reserved for childhood conditions such as ESES.
Each case of “non-classic” NCSE might be treated best as tailored to the type of NCSE, the underlying illness, and the overall clinical context. Patients with “classic” NCSE such as absence and CPSE seldom warrant aggressive treatment, while more aggressive treatment with heavily sedating drugs may be necessary, including for the ‘subtle’ SE that follows inadequate treatment of GCSE. One decision analysis paper (Ferguson et al., 2013) considered factors including NCSE etiologies and the consequences of each, and the efficacy and effects of different treatments. It favored non-aggressive treatment for etiologies of low morbidity (absence SE or discontinuation of ASDs) but aggressive treatment with a major risk of seizure-induced neurologic damage (e.g. due to intraparenchymal hemorrhage). No recommendation could be offered for NCSE due to hypoxia/ischemia, given the poor outcome with any treatment. (The study could not cover most forms of non-classic NCSE.)
While much SE research has focused on determining the “best” drug (Treiman et al., 1998, Silbergleit and Lowenstein, 2011), several more recent studies have focused on three important (additional, not replacing) factors: (1) ascertaining quickly the correct diagnosis – both of the type of SE [GCSE is obvious; for others, especially MSE and NCSE, the exact syndrome is important to know and use] and its precise etiology (which can alter treatment in up to 40% of cases (Alvarez et al., 2014)); (2) ensuring that treatment is started sooner; it is far too often delayed (Gaínza-Lein et al., 2018)]; and (3) that the initial treatment of SE uses adequate doses of ASDs; initial BDZ doses are far too frequently inadequate and should be augmented substantially (Alvarez et al., 2015) -- often even reducing complications (Alldredge et al., 2001, Fernandez et al., 2014).
5.4. Risks of overtreatment
There is an association between the use of highly sedating drugs (sometimes called ‘anesthetic’), usually midazolam, propofol, or barbiturates, and worsened outcome in patients treated for RSE (Sutter et al., 2014, Marchi et al., 2015), even when controlled for confounders such as duration and severity of SE, and comorbidities. Still, some such studies included patients treated for absence and CPSE, and it is extremely difficult to control for the refractoriness of the SE -- that may have led clinicians to choose more aggressive treatment in the first place.
While aggressive treatment of RSE may be necessary in some cases, and while etiology (rather than those drugs) may be the primary cause of poor outcomes, it is worrisome that outcome in RSE and “super-refractory SE” (SRSE), including many with NCSE, is so poor overall. Patients with RSE have about a 30% mortality, and it may be as little as 20% with SRSE and ‘new onset refractory SE’ (NORSE) who return to their previous or normal baseline levels of functioning (Alvarez and Drislane, 2016).
5.5. Recommendations (of all three authors)
-
1.
The proper diagnosis of both the SE type and its etiology should be determined quickly, and treatment should start as soon as possible, at appropriate, adequate doses.
-
2.
The management and treatment of refractory GCSE and SRSE is now clearly established (Brophy et al., 2012). If early ASDs fail, it is appropriate to use BDZs, propofol, and pentobarbital, as necessary (Brophy et al., 2012, Shorvon and Ferlisi, 2011).
-
3.
Patients with the continuation of GCSE in its later, ‘subtle SE’ form (where the EEG shows definite or probable NCSE by current EEG definitions) are seriously ill and warrant the same treatment (Treiman et al., 1990, Treiman et al., 1998).
-
4.
When NCSE follows a generalized convulsion or GCSE and early ASDs fail, lean toward aggressive treatment, with eventual taper.
-
5.
SE with prior epilepsy syndromes (absence, simple partial, CPSE, and ‘benign’ MSE) often does well and should rarely be treated aggressively. Treat with higher doses of the patient’s earlier ASDs. Other options include i.v. DPH, PB, VPA, LEV, LCM, or other non-sedating i.v. ASDs or other BDZs.
-
6.
If there was NO earlier convulsion or definite seizure, or if seizure activity has been entirely nonconvulsive, or it is unclear how worrisome the NCSE is, try to rely on non-sedating ASDs agents or non-pharmacologic therapy.
-
7.
For the Non-Classic NCSE [or “NCSE in coma (or in sick patients)”], if there was an earlier convulsion or definite clinical seizure, lean toward aggressive treatment if early ASDs fail.
-
8.
Beyond the type of SE, consider also the etiology, EEG pattern (discharge frequency, “seizure burden” etc.), likely side effects of medications and especially of the prolonged ICU course; plus age, social (family) setting, medical comorbidities, and overall prognosis.
-
9.
In all cases, treat vigorously, following clinically, and on EEG.
[Experienced clinicians will often deviate from these suggestions depending on the individual circumstances.]
5.6. Why do so many refractory status patients die in the ICU?
The suggestions above are for treatment in the early hours and days in the ICU. Aggressive treatment is often necessary, but it is important to ask why so many patients with RSE (most of which is the ‘non-classical’ NCSE seen in ICUs) treated with highly sedating drugs do so poorly. Almost all series attribute this to the underlying illness, rather than to the seizures themselves (Claassen et al., 2002). Risk of death in SE has been associated with “catastrophic etiologies” (Pugin et al., 2014), age, comorbidities, and respiratory failure (Koubeissi and Alshekhlee, 2007).
In one paper linking aggressive therapy with poor outcomes, most deaths were due to infection and some to multiorgan failure (Sutter et al., 2014). In another series, 80% of 78 patients with SE lasting over a week had a poor outcome; half died, and 63% of deaths were due to multiorgan failure (Lai et al., 2015). In our center, infection and multiorgan failure are the primary causes of death in RSE patients in the ICU over a week; cardiac, cerebrovascular, and hematologic problems contribute. Most of these appear to have been acquired after the early treatment. Patients appear most likely to die from complications encountered in prolonged ICU courses (partly occasioned by the use of highly sedating drugs, but also by underlying illnesses) than they are from the SE itself or the direct effects of those drugs, e.g. hypotension (Sutter et al., 2014, Lai et al., 2015). It is crucially important to attend to the many medical complications that prolong the ICU course; as soon as possible, attention must turn to tapering medications and getting the patient out of the ICU.
5.7. Getting out of the ICU
Avoiding the complications of aggressive treatment of long ICU stays might be facilitated by several measures, including trying to shorten their durations. The suggestions that follow (as those above) are not particularly “evidence-based,” but based rather on discussions at conferences like the ICCN (Robakis and Hirsch, 2006). They are endorsed by all three authors. As above, this should begin with the prompt and correct diagnosis of SE type and etiology, and rapid and adequate dosing of the initial treatment.
-
1.
If there is a characteristic clinical presentation (or even a suggestion) of an immune-mediated SE, including the condition of unexplained new-onset refractory SE (NORSE), consider immunotherapy earlier in the course, even before confirmed by antibody testing.
-
2.
In tapering highly sedating medication, assure adequate doses and levels of concomitant non-sedating ASDs (two or more).
-
3.
Perhaps after one unsuccessful attempt to taper highly sedating drugs, consider ketamine or non-coma-inducing therapies such as ketogenic diet. In even more prolonged refractory cases, consider various forms of stimulation or even focal respective surgery -- when the focus can be identified.
-
4.
Relatively high doses and slower tapering of less sedating ASDs may help in the withdrawal of the more highly-sedating drugs used to induce ‘iatrogenic coma.’ This may include moderate to high doses of shorter-acting BDZs such as lorazepam, or relatively high doses of phenobarbital (to which patients may habituate in terms of respiratory effort and even responsiveness) (Pugin et al., 2014, Crawford et al., 1988, Krishnamurthy and Drislane, 1997, Hocker, 2018).
-
5.
When treatment must be re-intensified (e.g. For relapses of SE), try non-sedating ASDs first.
-
6.
During the tapering, tolerate a few seizures per day, especially if purely electrographic or nonconvulsive, and if focal, or brief (a few minutes each), but not generalized convulsions, rather than intensifying suppressive treatment when they occur. Do not increase treatment for isolated, slower, or briefer periodic discharges.
-
7.
Throughout, maintain compulsive surveillance for (and management of) infection, hematologic problems, and organ failure.
[As above, experienced neurologists may well choose entirely different plans.]
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Andrea O. Rossetti, Email: andrea.rossetti@chuv.ch.
Lawrence J. Hirsch, Email: Lawrence.Hirsch@Yale.edu.
Frank W. Drislane, Email: fdrislan@bidmc.harvard.edu.
References
- Aicua Rapun I., Novy J., Solari D., Oddo M., Rossetti A.O. Early Lance-Adams syndrome after cardiac arrest: prevalence, time to return to awareness, and outcome in a large cohort. Resuscitation. 2017;115:169–172. doi: 10.1016/j.resuscitation.2017.03.020. [DOI] [PubMed] [Google Scholar]
- Alldredge B.K., Gelb A.M., Isaacs S.M., Corry M.D., Allen F., Ulrich S. A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N. Engl. J. Med. 2001;345:631–637. doi: 10.1056/NEJMoa002141. [DOI] [PubMed] [Google Scholar]
- Alvarez V., Drislane F.W. Is favorable outcome possible after prolonged refractory status epilepticus? J. Clin. Neurophysiol. 2016;33:32–41. doi: 10.1097/WNP.0000000000000223. [DOI] [PubMed] [Google Scholar]
- Alvarez V., Westover M.B., Drislane F.W., Dworetzky B.A., Curley D., Lee J.W., Rossetti A.O. Evaluation of a clinical tool for early etiology identification in status epilepticus. Epilepsia. 2014;55:2059–2068. doi: 10.1111/epi.12852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez V., Lee J.W., Drislane F.W., Westover M.B., Novy J., Dworetzky B.A., Rossetti A.O. Practice variability and efficacy of clonazepam, lorazepam, and midazolam in status epilepticus: a multicenter comparison. Epilepsia. 2015;56:1275–1285. doi: 10.1111/epi.13056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez V., Lee J.W., Westover M.B., Drislane F.W., Novy J., Faouzi M. Therapeutic coma for status epilepticus: differing practices in a prospective multicenter study. Neurology. 2016;87:1650–1659. doi: 10.1212/WNL.0000000000003224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer G., Trinka E. Nonconvulsive status epilepticus and coma. Epilepsia. 2010;51:177–190. doi: 10.1111/j.1528-1167.2009.02297.x. [DOI] [PubMed] [Google Scholar]
- Beretta S., Coppo A., Bianchi E., Zanchi C., Carone D., Stabile A. Neurologic outcome of postanoxic refractory status epilepticus after aggressive treatment. Neurology. 2018;91:e2153–e2162. doi: 10.1212/WNL.0000000000006615. [DOI] [PubMed] [Google Scholar]
- Brophy G.M., Bell R., Claassen J., Alldredge B., Bleck T.P., Glauser T., Laroche S.M., Care Neurocritical. Society status epilepticus guideline writing committee. Guidelines for the evaluation and management of status epilepticus. Neurocrit. Care. 2012;17(1):3–23. doi: 10.1007/s12028-012-9695-z. [DOI] [PubMed] [Google Scholar]
- Chong D.J., Hirsch L.J. Which EEG patterns warrant treatment in the critically ill? Reviewing the evidence for treatment of periodic epileptiform discharges and related patterns. J. Clin. Neurophysiol. 2005;22:79–91. doi: 10.1097/01.wnp.0000158699.78529.af. [DOI] [PubMed] [Google Scholar]
- Claassen J., Hirsch L.J., Emerson R.G., Mayer S.A. Treatment of refractory status epilepticus with pentobarbital, propofol, or midazolam: a systematic review. Epilepsia. 2002;43:146–153. doi: 10.1046/j.1528-1157.2002.28501.x. [DOI] [PubMed] [Google Scholar]
- Claassen J., Mayer S.A., Kowalski R.G., Emerson R.G., Hirsch L.J. Detection of electrographic seizures with continuous EEG monitoring in critically ill patients. Neurology. 2004;62:1743–1748. doi: 10.1212/01.wnl.0000125184.88797.62. [DOI] [PubMed] [Google Scholar]
- Claassen J., Jette N., Chum F., Green R., Schmidt M., Choi H. Electrographic seizures and periodic discharges after intracerebral hemorrhage. Neurology. 2007;69:1356–1365. doi: 10.1212/01.wnl.0000281664.02615.6c. [DOI] [PubMed] [Google Scholar]
- Crawford T.O., Mitchell W.G., Fishman L.S., Snodgrass S.R. Very-high-dose phenobarbital for refractory status epilepticus in children. Neurology. 1988;38:1035–1040. doi: 10.1212/wnl.38.7.1035. [DOI] [PubMed] [Google Scholar]
- Das A.S., Lee J.W., Rosenthal E.S., Vaitkevicius H. Successful wean despite emergence of ictal-interictal EEG patterns during the weaning of prolonged burst-suppression therapy for super-refractory status epilepticus. Neurocrit. Care. 2018;29:452–462. doi: 10.1007/s12028-018-0552-6. [DOI] [PubMed] [Google Scholar]
- DeGiorgio C.M., Heck C.N., Rabinowicz A.L., Gott P.S., Smith T., Correale J. Serum neuron-specific enolase in the major subtypes of status epilepticus. Neurology. 1999;52:746–749. doi: 10.1212/wnl.52.4.746. [DOI] [PubMed] [Google Scholar]
- DeLorenzo R.J., Hauser W.A., Towne A.R., Boggs J.G., Pellock J.M., Penberthy L. A prospective, population-based epidemiologic study of status epilepticus in Richmond, Virginia. Neurology. 1996;46:1029–1035. doi: 10.1212/wnl.46.4.1029. [DOI] [PubMed] [Google Scholar]
- DeLorenzo R.J., Waterhouse E.J., Towne A.R., Boggs J.G., Ko D., DeLorenzo G.A. Persistent nonconvulsive status epilepticus after the control of convulsive status epilepticus. Epilepsia. 1998;39:833–840. doi: 10.1111/j.1528-1157.1998.tb01177.x. [DOI] [PubMed] [Google Scholar]
- DeMarchis G.M., Pugin D., Meyers E., Velasquez A., Suwatcharanangkoon S., Park S. Seizure burden in subarachnoid hemorrhage associated with functional and cognitive outcome. Neurology. 2016;86:253–260. doi: 10.1212/WNL.0000000000002281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drislane F.W. Evolving concepts of nonconvulsive status epilepticus. Chapter 19. In: Drislane F.W., Kaplan P.W., editors. Status Epilepticus: A Clinical Perspective. second ed. Humana Press; Cham Switzerland: 2018. pp. 227–240. [Google Scholar]
- Drislane F.W., Schomer D.L. Clinical implications of generalized electrographic status epilepticus. Epilepsy Res. 1994;19:111–121. doi: 10.1016/0920-1211(94)90021-3. [DOI] [PubMed] [Google Scholar]
- Elmer J., Rittenberger J.C., Faro J., Molyneaux B.J., Popsecu A., Callaway C.W., Baldwin M., Pittsburgh Post-Cardiac Arrest Clinically distinct electroencephalographic phenotypes of early myoclonus after cardiac arrest. Ann. Neurol. 2016;80:175–184. doi: 10.1002/ana.24697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson M., Bianchi M.T., Sutter R., Rosenthal E.S., Cash S.S., Kaplan P.W., Westover M.B. Calculating the risk benefit equation for aggressive treatment of non-convulsive status epilepticus. Neurocrit. Care. 2013;18:216–227. doi: 10.1007/s12028-012-9785-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez A., Lantigua H., Lesch C., Shao B., Foreman B., Schmidt J.M. High-dose midazolam infusion for refractory status epilepticus. Neurology. 2014;82:359–365. doi: 10.1212/WNL.0000000000000054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaínza-Lein M., Sánchez Fernández I., Jackson M., Abend N.S., Arya R., Brenton J.N., Carpenter J.L. Pediatric Status Epilepticus Research Group. Association of time to treatment with short-term outcomes for pediatric patients with refractory convulsive status epilepticus. JAMA Neurol. 2018;75:410–418. doi: 10.1001/jamaneurol.2017.4382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gastaut H., Roger A. Sur la signification de certain fugues épileptiques: état de mal temporal. Rev. Neurol. 1956;94:298–301. [PubMed] [Google Scholar]
- Herman S.T., Abend N.S., Bleck T.P., Chapman K.E., Drislane F.W., Emerson R.G. Consensus Statement on Continuous EEG in Critically Ill Adults and Children, part i: indications. J. Clin. Neurophysiol. 2015;32:87–95. doi: 10.1097/WNP.0000000000000166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch L.J., LaRoche S.M., Gaspard N., Gerard E., Svoronos A., Herman S.T. American Clinical Neurophysiology Society's Standardized Critical Care EEG Terminology: 2012 version. J. Clin. Neurophysiol. 2013;30:1–27. doi: 10.1097/WNP.0b013e3182784729. [DOI] [PubMed] [Google Scholar]
- Hocker S. Treatment of refractory and super-refractory status epilepticus. Chapter 17. In: Drislane F.W., Kaplan P.W., editors. Status Epilepticus: A Clinical Perspective. second ed. Humana Press; Cham Switzerland: 2018. pp. 201–214. [Google Scholar]
- Hopp J.L., Sanchez A., Krumholz A., Hart G., Barry E. Nonconvulsive status epilepticus: value of a benzodiazepine trial for predicting outcomes. Neurologist. 2011;17:325–329. doi: 10.1097/NRL.0b013e31822f688c. [DOI] [PubMed] [Google Scholar]
- Kaplan P.W. No, some types of nonconvulsive status epilepticus cause little permanent neurologic sequelae (or: “the cure may be worse than the disease”) Neurophysiol. Clin. 2000;30:377–382. doi: 10.1016/s0987-7053(00)00238-0. [DOI] [PubMed] [Google Scholar]
- Knake S., Rochon J., Fleischer S., Katsarou N., Back T., Vescovit M. Status epilepticus after stroke is associated with increased long-term case fatality. Epilepsia. 2006;47:2020–2026. doi: 10.1111/j.1528-1167.2006.00845.x. [DOI] [PubMed] [Google Scholar]
- Koubeissi M., Alshekhlee A. In-hospital mortality of generalized convulsive status epilepticus: a large US sample. Neurology. 2007;69:886–893. doi: 10.1212/01.wnl.0000269791.96189.70. [DOI] [PubMed] [Google Scholar]
- Koutroumanidis M. Myoclonic status epilepticus in the idiopathic generalized epilepsies. Chapter 15. In: Drislane F.W., Kaplan P.W., editors. Status Epilepticus: a clinical perspective. second ed. Humana Press; Cham Switzerland: 2018. pp. 173–191. [Google Scholar]
- Krishnamurthy K.B., Drislane F.W. Phenobarbital and benzodiazepine assisted withdrawal of prolonged pentobarbital treatment for refractory status epilepticus. J. Epilepsy. 1997;10:211–214. [Google Scholar]
- Krishnan V., Drislane F.W., Benatar M. Cognitive manifestations of focal status epilepticus. Chapter 21. In: Drislane F.W., Kaplan P.W., editors. Status Epilepticus: A Clinical Perspective. second ed. Humana Press; Cham Switzerland: 2018. pp. 259–273. [Google Scholar]
- Lai A., Outin H.D., Jabot J., Mégarbane B., Gaudry S., Coudroy R. Functional outcome of prolonged refractory status epilepticus. Crit. Care. 2015;19:199. doi: 10.1186/s13054-015-0914-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leitinger M., Beniczky S., Rohracher A., Gardella E., Kalss G., Qerama E. Salzburg consensus criteria for non-convulsive status epilepticus – approach to clinical application. Epilepsy Behav. 2015;49:158–163. doi: 10.1016/j.yebeh.2015.05.007. [DOI] [PubMed] [Google Scholar]
- Leitinger M., Trinka E., Gardella E., Rohrbacher A., Kalss G., Qerama E. Diagnostic accuracy of the Salzburg EEG criteria for non-convulsive status epilepticus: a retrospective study. Lancet Neurol. 2016;15:1054–1062. doi: 10.1016/S1474-4422(16)30137-5. [DOI] [PubMed] [Google Scholar]
- Lennox W.G. The treatment of epilepsy. Med. Clin. North Am. 1945;29:1114–1128. [Google Scholar]
- Litt B., Wityk R.J., Hertz S.H., Mullen P.D., Weiss H., Ryan D.D., Henry T.R. Nonconvulsive status epilepticus in the critically ill elderly. Epilepsia. 1998;39:1194–1202. doi: 10.1111/j.1528-1157.1998.tb01311.x. [DOI] [PubMed] [Google Scholar]
- Logroscino G., Hesdorffer D.C., Cascino G., Hauser W.A. Status epilepticus without an underlying cause and risk of death: a population-based study. Arch. Neurol. 2008;65:221–224. doi: 10.1001/archneurol.2007.43. [DOI] [PubMed] [Google Scholar]
- Lowenstein D.H., Bleck T., Macdonald R.L. It’s time to revise the definition of status epilepticus. Epilepsia. 1999;40:120–122. doi: 10.1111/j.1528-1157.1999.tb02000.x. [DOI] [PubMed] [Google Scholar]
- Marchi N.A., Novy J., Faouzi M., Stähli C., Burnand B., Rossetti A.O. Status epilepticus: impact of therapeutic coma on outcome. Crit. Care Med. 2015;43:1003–1009. doi: 10.1097/CCM.0000000000000881. [DOI] [PubMed] [Google Scholar]
- Meldrum B.S., Horton R.W. Physiology of status epilepticus in primates. Arch. Neurol. 1973;28:1–9. doi: 10.1001/archneur.1973.00490190019001. [DOI] [PubMed] [Google Scholar]
- Nolan M., Bergazar M., Chu B., Cortez M.A., Snead O.C. Clinical and neurophysiologic spectrum associated with atypical absence seizures in children with intractable epilepsy. J. Child. Neurol. 2005;20:404–410. doi: 10.1177/08830738050200050201. [DOI] [PubMed] [Google Scholar]
- Oddo M., Carrera E., Claassen J., Mayer S.A., Hirsch L.J. Continuous electroencephalography in the medical intensive care unit. Crit. Care Med. 2009;37:2051–2056. doi: 10.1097/CCM.0b013e3181a00604. [DOI] [PubMed] [Google Scholar]
- O'Rourke D., Chen P.M., Gaspard N., Foreman B., McClain L., Karakis I. Response rates to anticonvulsant trials in patients with triphasic-wave EEG patterns of uncertain significance. Neurocrit. Care. 2016;24:233–239. doi: 10.1007/s12028-015-0151-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman G.M., Riviello J.J., Hirsch L.J. EEG in the intensive care unit: anoxia, coma, brain death and related disorders. Chapter 22. In: Schomer D.L., Lopes da Silva F., editors. Niedermeyer’s Electroencephalography, Basic Principles, Clinical Applications, and Related Fields. seventh ed. Oxford University Press; New York: 2018. pp. 610–658. [Google Scholar]
- Palmio J., Kerannen T., Alapirtti T., Hulkkonen J., Makinen R., Holm P. Elevated serum neuron-specific enolase in patients with temporal lobe epilepsy: a video-EEG study. Epilepsy Res. 2008;81:155–160. doi: 10.1016/j.eplepsyres.2008.05.006. [DOI] [PubMed] [Google Scholar]
- Payne E.T., Zhao X.Y., Frndova H., McBain K., Sharma R., Hutchinson J.S., Hahn C.D. Seizure burden is independently associated with short term outcome in critically ill children. Brain. 2014;137:1429–1438. doi: 10.1093/brain/awu042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penfield W., Jasper H.H. Little Brown; Boston: 1954. Epilepsy and Functional Anatomy of the Human Brain. [Google Scholar]
- Pugin D., Foreman B., De Marchis G.M., Fernandez A., Schmidt J.M., Czeisler B.M. Is pentobarbital safe and efficacious in the treatment of super-refractory status epilepticus: a cohort study. Crit. Care. 2014;18(3):R103. doi: 10.1186/cc13883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riviello J.J. Pediatric status epilepticus: initial management and the special syndromes of status epilepticus in children. Chapter 27. In: Drislane F.W., Kaplan P.W., editors. Status Epilepticus: A Clinical Perspective. 2nd ed. Humana Press; Cham Switzerland: 2018. pp. 333–353. [Google Scholar]
- Robakis T.K., Hirsch L.J. Literature review, case report, and expert discussion of prolonged refractory status epilepticus. Neurocrit. Care. 2006;4:35–46. doi: 10.1385/NCC:4:1:035. [DOI] [PubMed] [Google Scholar]
- Rodriguez Ruiz A., Vlachy J., Lee J.W., Gilmore E.J., Ayer T., Haider H.A. CCEMRC. Association of periodic and rhythmic electroencephalographic patterns with seizures in critically ill patients. JAMA Neurol. 2017;74:181–188. doi: 10.1001/jamaneurol.2016.4990. [DOI] [PubMed] [Google Scholar]
- Rossetti A.O., Logroscino G., Liaudet L., Ruffieux C., Ribordy V., Schaller M.D. Status epilepticus: an independent outcome predictor after cerebral anoxia. Neurology. 2007;69:255–260. doi: 10.1212/01.wnl.0000265819.36639.e0. [DOI] [PubMed] [Google Scholar]
- Rossetti A.O., Oddo M., Liaudet L., Kaplan P.W. Predictors of awakening from postanoxic status epilepticus after therapeutic hypothermia. Neurology. 2009;72:744–749. doi: 10.1212/01.wnl.0000343006.60851.62. [DOI] [PubMed] [Google Scholar]
- Rossetti A.O., Rabinstein A.A., Oddo M. Neurological prognostication of outcome in patients in coma after cardiac arrest. Lancet Neurol. 2016;15:597–609. doi: 10.1016/S1474-4422(16)00015-6. [DOI] [PubMed] [Google Scholar]
- Sandroni C., Cariou A., Cavallaro F., Cronberg T., Friberg H., Hoedemaekers C. Prognostication in comatose survivors of cardiac arrest: an advisory statement from the European Resuscitation Council and the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40:1816–1831. doi: 10.1007/s00134-014-3470-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serafini A., Gerard E.E., Schuele S.U. Myoclonic status epilepticus. Chapter 12. In: Drislane F.W., Kaplan P.W., editors. Status Epilepticus: A Clinical Perspective. second ed. Humana Press; Cham Switzerland: 2018. pp. 139–153. [Google Scholar]
- Shafi M.M., Westover M.B., Cole A.J., Kilbride R.D., Hoch D.B., Cash S.S. Absence of early epileptiform abnormalities predicts lack of seizures on continuous EEG. Neurology. 2012;79:1796–1801. doi: 10.1212/WNL.0b013e3182703fbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorvon S., Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain. 2011;134:2802–2818. doi: 10.1093/brain/awr215. [DOI] [PubMed] [Google Scholar]
- Silbergleit R., Lowenstein D., Durkalski V., Conwit R. Neurological Emergency Treatment Trials (NETT) Investigators. RAMPART (Rapid Anticonvulsant Medication Prior to Arrival Trial): a double-blind randomized clinical trial of the efficacy of intramuscular midazolam versus intravenous lorazepam in the prehospital treatment of status epilepticus by paramedics. Epilepsia. 2011;52(suppl 8):45–47. doi: 10.1111/j.1528-1167.2011.03235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Struck A.F., Osman G., Rampal N., Biswal S., Legros B., Hirsch L.J. Time-dependent risk of seizures in critically ill patients on continuous electroencephalogram. Ann. Neurol. 2017;82:177–185. doi: 10.1002/ana.24985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Struck A.F., Ustun B., Ruiz A.R., Lee J.W., LaRoche S.M., Hirsch L.J. Association of an electroencephalography-based risk score with seizure probability in hospitalized patients. JAMA Neurol. 2017;74:1419–1424. doi: 10.1001/jamaneurol.2017.2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutter R. Are we prepared to detect subtle and nonconvulsive status epilepticus in critically ill patients? J. Clin. Neurophysiol. 2016;33:25–31. doi: 10.1097/WNP.0000000000000216. [DOI] [PubMed] [Google Scholar]
- Sutter R., Marsch S., Fuhr P., Kaplan P.W., Rüegg S. Anesthetic drugs in status epilepticus – risk or rescue? Results from a six-year cohort study. Neurology. 2014;82:656–664. doi: 10.1212/WNL.0000000000000009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas P., Zifkin B., Migneco O., Lebrun C., Darcourt J., Andermann F. Nonconvulsive status epilepticus of frontal origin. Neurology. 1999;52:1174–1183. doi: 10.1212/wnl.52.6.1174. [DOI] [PubMed] [Google Scholar]
- Topjian A.A., Gutierrez-Colina A.M., Sanchez S.M., Berg R.A., Friess S.H., Dlugos D.J., Abend N.S. Electrographic status epilepticus is associated with mortality and worse short-term outcome in critically ill children. Crit. Care Med. 2013;41:215–223. doi: 10.1097/CCM.0b013e3182668035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towne A.R., Waterhouse E.J., Boggs J.G., Garnett L.K., Brown A.J., Smith J.R., Jr Prevalence of nonconvulsive status epilepticus in comatose patients. Neurology. 2000;54:340–345. doi: 10.1212/wnl.54.2.340. [DOI] [PubMed] [Google Scholar]
- Treiman D.M., Walton N.Y., Kendrick C. A progressive sequence of electroencephalographic changes during generalized convulsive status epilepticus. Epilepsy Res. 1990;5:49–60. doi: 10.1016/0920-1211(90)90065-4. [DOI] [PubMed] [Google Scholar]
- Treiman D.M., Meyers P.D., Walton N.Y., Collins J.F., Colling C., Rowan A.J. A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. N. Engl. J. Med. 1998;339:792–798. doi: 10.1056/NEJM199809173391202. [DOI] [PubMed] [Google Scholar]
- Trinka E., Cock H., Hesdorffer D., Rossetti A.O., Scheffer I.E., Shinnar S. A definition and classification of status epilepticus – report of the ILAE task force on classification of status epilepticus. Epilepsia. 2015;56:1515–1523. doi: 10.1111/epi.13121. [DOI] [PubMed] [Google Scholar]
- Vespa P.M., McArthur D.L., Xu Y., Eliseo M., Etchepare M., Dinvo I. Nonconvulsive seizures after traumatic brain injury are associated with hippocampal atrophy. Neurology. 2010;75:792–798. doi: 10.1212/WNL.0b013e3181f07334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vespa P., Tubi M., Claassen J., Blanco M., McArthur D., Velazquez A.G. Metabolic crisis occurs with seizures and periodic discharges after brain trauma. Ann. Neurol. 2016;79:579–590. doi: 10.1002/ana.24606. [DOI] [PubMed] [Google Scholar]
- Wagenman K.L., Blake T.P., Sanchez S.M., Schultheis M.T., Radcliffe J., Berg R.A. Electrographic status epilepticus and long-term outcome in critically ill children. Neurology. 2014;82:396–404. doi: 10.1212/WNL.0000000000000082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witsch J., Frey H.P., Schmidt J.M., Velazquez A., Falo C.M., Reznik M. Electroencephalographic periodic discharges and frequency-dependent brain tissue hypoxia in acute brain injury. JAMA Neurol. 2017;74:301–309. doi: 10.1001/jamaneurol.2016.5325. [DOI] [PMC free article] [PubMed] [Google Scholar]