Abstract
Background and Aims:
BlockBuster® Laryngeal Mask Airway, a newer supraglottic airway device, is claimed to be an efficient conduit for endotracheal intubation. Intubating laryngeal mask airway (LMA) is an established device for the same. This randomised study was undertaken to evaluate the success rate of blind intubation using either of these LMAs.
Methods:
Sixty patients of age group 20-60 years undergoing general anaesthesia were randomised in 2 groups, of 30 patients each, for tracheal intubation using either BlockBuster® LMA (Group B) or the Intubating LMA Fastrach® (Group F). After induction of anaesthesia, LMAs were inserted and on achieving adequate ventilation with the device, fibreoptic scopy was performed to assess the glottis visualisation score. Blind intubation was attempted through the supraglottic airway devices (SAD). The primary objective was first pass successful intubation and secondary outcomes were ease, time for LMA insertion, oropharyngeal seal pressure (OSP), LMA removal time, fibreoptic scoring and complications. Data was analysed using SPSS V22 software.
Results:
The first-attempt success rate of tracheal intubation was 90% in Group B and 66.6% in Group F (P = 0.028), while the overall success rate of intubation was 96.6% in Group B and 89.9% in Group F (P = 0.3). The OSP in Group B was 33.7 ± 1.8 and 22.7 ± 1.5 cm H2O in Group F (P = 0.001). Complications such as sore throat and blood stain were reduced with BlockBuster® LMA.
Conclusion:
BlockBuster® LMA provides higher first pass success rate of blind tracheal intubation with less complications like sore throat and blood staining.
Key words: BlockBuster®, Fastrach®, laryngeal mask airway, tracheal intubation
INTRODUCTION
Securing airway is a vital responsibility of anaesthesiologists. Recently supraglottic airway devices with a conduit for blind tracheal intubation are gaining popularity as a bridge connecting ventilation and intubation in all genres of patients. Laryngeal mask airways with intubation conduit are useful and are also recommended by 'All India Difficult Airway Association' guidelines 2016.[1]
A newer LMA called Tourens BlockBuster® LMA invented in 2012 (Tuoren Medical Instrument co, Ltd, Changyuan city, China) has been gaining popularity to provide increased safety and quality of anaesthesia. Invented by Professor Ming Tian, it is advantageous in providing ventilation and increased green channel for intubation.[2] The Fastrach® LMA invented in 1997 (Teleflex Medical, Dublin, Ireland) is one such LMA specially designed for intubation. There are studies suggesting successful blind intubation in anticipated and unanticipated airways to be approximately 90-95%, with fewer incidence of complications.[3,4]
Many authors have studied the success rate of blind intubation via the BlockBuster® LMA.[2,5] We chose blind tracheal intubation because design of both these devices allows for unobstructed passage of a tracheal tube and previous studies have demonstrated a favorable alignment with the glottis inlet. The purpose of this study was to compare the first pass success rate of blind tracheal intubation through BlockBuster® LMA and LMA Fastrach®. The hypothesis of the study was that, because of higher airway seal pressure, lesser angle of emergence (30°) of endotracheal tube through the cuff of BlockBuster® LMA and the unique tip of the Parker flexi tip tube to prefer nonresistant areas, we assumed a better success rate during blind tracheal intubation with BlockBuster® LMA.[5]
The primary aim of this study was to compare the BlockBuster® LMA with LMA Fastrach® in regard to first-attempt success rate of blind tracheal intubation. Secondary outcomes assessed were the ease, time, attempts and the success of the device placement, oropharyngeal seal pressure, fibreoptic grade of laryngeal view, along with the time for removal of the device after successful tracheal intubation.
METHODS
This study was registered with Clinical Trials Registry-India (CTRI/2019/03/018250). After obtaining institutional ethical committee approval (SNMC/IECHSR/2018-19/A-77/1.1 and 11/02/2019), written informed consent was taken from all the 60 patients of American Society of Anesthesiologists (ASA) physical status I -II, modified mallampati classification (MMT) I-III, aged between 20 to 60 years undergoing elective surgeries under general anaesthesia between December 2018 and May 2019. Exclusion criteria included patient's refusal, mouth opening less than 2 cm, oropharyngeal pathology, morbid obesity, risk of regurgitation and pregnancy. The study was performed in accordance with the principles of the Declaration of Helsinki.
Patients were randomly allocated into two groups –Group B (BlockBuster® LMA) and Group F (Fastrach® LMA), with 30 patients in each group. Random allocation into these groups was done by computer generated random numbers. Group allocations were placed in sealed, opaque envelopes on initial randomisation. An anaesthesiologist with an experience of 25 successful insertions and intubations with both the devices performed blind tracheal intubation using either of the LMAs'. The same anaesthesiologist performed all the intubations. Observation and data collection was done by an independent observer. Computer-based randomisation of the device assignment was revealed to anaesthesiologist just prior to the device placement. The entire study was not blinded.
Patients were kept nil by mouth (NBM) for 6 hours prior to surgery. Tablet alprazolam 0.5 mg was given for all patients orally one day before surgery. After arrival in the operating room, an 18G/20G peripheral intravenous catheter was inserted into patient forearm. Standard multichannel monitoring was used throughout the procedure, including non-invasive blood pressure (NIBP), electrocardiograph (ECG), pulse oximetry (SPO2) and end tidal carbon dioxide (ETCO2). Pre-medication was given with intravenous glycopyrrolate 0.2 mg, ondansetron 4mg, midazolam 0.02 mg/kg, fentanyl 2 μg/kg. All patients were pre-oxygenated with 100% oxygen for 3 minutes and anaesthesia induced with intravenous propofol 2 mg/kg in slow incremental dose and adequacy of mask ventilation noted.
After confirming adequate mask ventilation, vecuronium 0.1 mg/kg was administered for neuromuscular blockade. After 3 minutes, either of the devices was inserted using a midline insertion technique in neutral neck position for both the groups. The appropriate size of LMA was selected according to body weight. Size 3 for (30-50kg) and size 4 for (50-70kg) as per the manufacturers' guidelines.[4,5] Adequate ventilation was confirmed by chest movements and ETCO2 waveforms. The lungs were ventilated with a mixture of oxygen and sevoflurane for an end-tidal concentration of 2%.[6] Time required for insertion of LMA was defined from removal of facemask to the time where adequate ventilation as established through LMA with normal square wave capnogram. Adequate ventilation was defined by easy bag ventilation, bilateral equal air entry and absence of audible air leak around the cuff. Soon after the insertion, LMA cuff was inflated with air using Smiths cuff pressure manometer (Smiths Medical International Ltd. Boundary Road, Hythe, KentCT216JL, UK) as per recommendations, to a pressure of 60 cm H2O. The LMA was connected to the breathing circuit. The number of attempts for LMA insertion was noted. The ease of LMA placement was assessed using a subjective scale of 1-4 (1-no resistance, 2-mild resistance, 3-moderate resistance, and 4-inability to place the device).[7] Successful placement was confirmed with the ability to achieve tidal volume of at least 7 ml/kg with a square wave capnogram. The oropharyngeal seal pressure was measured with expiratory valve closed and fresh gas flow of 3L/m until equilibrium was seen on the pressure gauge (not allowed to exceed 40cm H2O).[8] The position of both the LMAs was determined by fibreoptic scopy as well. The position of BlockBuster® was determined by a fibreoptic scope at a position 1 cm proximal to the distal end of the airway tube and in Fastrach® tube score was assessed just when the fibreoptic scope elevated the epiglottis elevating bar.[9] We used fibreoptic scope to assess the glottis visualisation score (Brimacombe score) and not for intubation. There are four grades: 1) only cords seen, 2) cords with posterior epiglottis seen, 3) cords plus anterior epiglottis seen, and 4) no cords seen, but function adequate.[10] The anaesthesiologist who performed blind intubation through the LMAs was not aware of the fibreoptic score.
The time for successful tracheal intubation started when the endotracheal tube was inserted into the green channel of LMA until the confirmation through capnographic waveform.[10] Intubation was performed blindly through the LMAs, using LMA specific tubes like BlockBuster® tubes (Parker flex tip) and Fastrach® tubes (armoured silicone tip). The number of intubation attempts were also noted. Time for first intubation attempt was measured, whereas time taken for second attempt was not assessed as it was not in our objectives as per the studies we referred.
For failed first attempt of blind intubation in Group B, second attempt was done by the same anaesthesiologist with a change in the technique applied.
For Group F, blind intubation in first attempt was done with Chandy manoeuvre which is a two-step approach. In step 1, the metal handle was used to rotate the device in sagittal and coronal plane to establish optimal ventilation with minimum resistance to bag ventilation and audible leaks during manual ventilation. Then the handle was held in this position to optimise the passage of tracheal tube. The second step was to use the handle to lift the LMA away from the posterior pharyngeal wall,[11] if intubation failed in first attempt, second attempt was done using the manufactures guidelines for resistance encountered as mentioned below:
-
1)
If resistance was felt after advancing the tube beyond the distal opening of the Fastrach® airway tube, then the device was too small and a larger LMA was needed
-
2)
If resistance was felt within 1 cm while advancing the tube, the device was too large and a smaller Fastrach® LMA was needed
-
3)
If resistance was felt at 2-2.5cm beyond the distal opening of the LMA, then there must be a down folding of epiglottis and was not within the reach of epiglottic elevating bar, in such case LMA was withdrawn and reinserted.[11]
To avoid airway trauma, force was not used to advance the endotracheal tube. The numbers of intubation attempts were limited to three.
Following successful intubation, the device was removed based on the manufacturers' recommendations using a removable stylet as a stabilising rod. Time for removal of the device started with disconnection of breathing circuit till ETCO2 waveform was observed. The intubation was stated as failed when it was not successful even after three attempts and if the tube was dislodged during the removal of LMA. At the end of the procedure, tube was removed if standard extubation criteria were met.[12] Complications such as sore throat, blood staining on the device, vomiting, bronchospasm/laryngospasm, post extubation stridor etc., were noted.
We defined sore throat as pain, scratchiness or irritation of throat that often worsens on swallowing. Assessed by4 point scale, 1- No sore throat, 2- mild (complaints of sore throat only on inquiry), 3- moderate (complaints of sore throat without inquiry), and 4- Severe (sore throat with soreness and associated with throat pain). Nausea is defined as a feeling of sickness with an inclination to vomit. Vomiting is defined as forceful expulsion of contents of the stomach out through the mouth. Assessed by a 5 point scale, 0- no complaints, 1- mild nausea, 2- moderate nausea and vomiting, 3- frequently vomiting, and 4- Severe continuous vomiting. All these complications were assessed at frequent time intervals like immediate postoperative, every 15 minutes for 2 hours then 4th hourly for 8 hours and then at 6, 12, 24 hours.
Sample size was calculated using Open Epi Software Version 2.3.1. At 95% confidence level, 80% power of study.
Yunluo LYU, Yaun Z et al.,[13] conducted a study on application of BlockBuster® LMA in urology surgery. Their main aim was to compare the success rate of intubation. The success rate of intubation through BlockBuster® LMA was 90.5%. The anticipated difference in intubation success rate which was used for calculating sample size was 33.4%. Based on this study we choose intubation success rate as the primary criteria for calculating our sample size; which came as 29 in each group. We recruited 30 patients for each device within each group to increase power of the study and allowing for possible dropouts as shown in consort chart [Figure 1].
Figure 1.
Consort chart
Data was entered in MS-Excel and analysed in SPSS V22. Descriptive statistics were represented with percentages, Mean with SD or Median with IQR depending on nature of the data. Chi-square test/Fisher Exact test, Independent t-test/Mann-Whitney U test were calculated. P < 0.05 was considered as statistically significant. Kolmogorov-Smirnov normality test was applied for all the parameters.
RESULTS
Demographic variables like age, weight, gender, ASA status and modified mallampati classification status were all comparable between the groups [Table 1]. Successful LMA device placement in both the Group B and Group F was achieved on first attempt in all 60 patients. The overall time for successful device placement in our study was similar in both the groups [Table 2].
Table 1.
Demographic characteristics of the patients
| Demographic data | Group B (n=30) | Group F (n=30) |
|---|---|---|
| Age, years (mean±SD) | 36±15 | 35±14 |
| Weight, Kg (mean±SD) | 63±10 | 64±8 |
| Gender (male:female) | 16:14 | 15:15 |
| ASA grade (I:II:III) | 15:10:5 | 16:12:2 |
| MPC (I:II:III) | 12:12:6 | 10:12:8 |
| Duration of surgery (mean±SD) | 112±10 | 100±14 |
*ASA – American Society of Anesthesiologists, *MPC – Mallampati Classification *SD – Standard deviation, *P<0.05
Table 2.
Comparison of LMA insertion, tracheal intubation and Success rate between two groups
| Variables | Group B | Group F | P |
|---|---|---|---|
| Time for LMA insertion(s) (mean±SD) | 12.2±1.5 | 12.1±1.5 | 1 |
| Ease of insertion (I/II/III/IV) | I/II (12:18) | I/II (16:14) | 0.8 |
| Time for intubation(s) (mean±SD) | 18±3 | 32±4 | 0.001 |
| Time for removal of LMA(s) (mean±SD) | 33±2 | 45±4 | 0.001 |
| First pass successful intubation (%) | 90 (27/30) | 66.6 (20/30) | 0.028 |
| Second attempt successful intubation (%) | 6.6 (2/30) | 23.3 (7/30) | 0.037 |
| Overall success (%) | 96.6 (29/30) | 89.9 (27/30) | 0.3 |
*n – Number of patients,*LMA – Laryngeal mask airway, *P<0.05
There was a significant difference in the oropharyngeal seal pressure between the groups. It was 33.7 ± 1.8 cm H2O in Group B and 22.7 ± 1.5 cm H2o in Group F, P = 0.001 [Figure 2]. The time for intubation was lesser in Group B (18.2 ± 2.7s) compared to (31.8 ± 3.9s) in Group F, P = 0.001 [Table 2].
Figure 2.
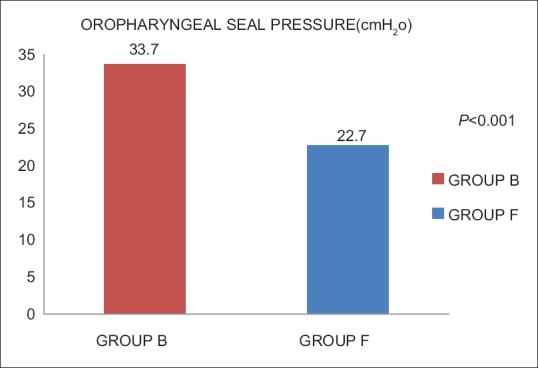
Oropharyngeal sealing pressure between Group B and Group F. P < 0.005 significant
Success rate of first attempt, in Group B was 90% (27/30) and in Group F was 66.6% (20/30), P = 0.028. In second attempt, in Group B it was 6.6% (2/30), while in Group F it was 23.3% (7/30) [Figure 3], P = 0.037. Overall success rate of intubation in both the groups is similar, P = 0.3. In Group B one patient (3.3%) and in Group F three patients (9.9%) required laryngoscopic intubation [Figure 3]. The fibreoptic scoring system showed the glottis view through the fibreoptic scope was better with Group B compared to Group F [Table 3]. The time for LMA removal after intubation was significantly less in Group B (33.0 ± 2.1s) when compared to Group F (45.1 ± 4.4s), P = 0.001.
Figure 3.
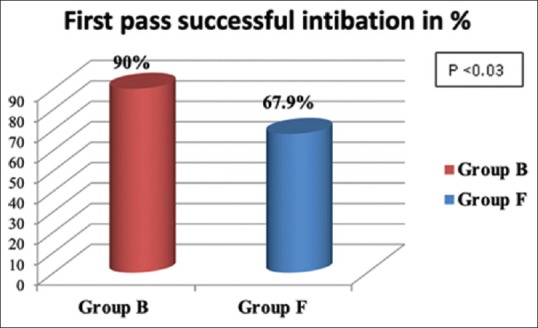
First pass successful intubation between Group B and Group F
Table 3.
Assessment of LMA position by fiber optic scoring between two groups
| Fiberoptic position | Group B | Group F |
|---|---|---|
| I (Vocal cords not seen)% | 3.3 (1/30) | 10 (3/30) |
| II (cords plus anterior epiglottis)% | 20 (6/30) | 23.3 (7/30) |
| III (cords plus posterior epiglottis)% | 30 (10/30) | 50 (15/30) |
| IV (only vocal cords) % | 43.3 (13/30) | 16.6 (5/30) |
Complications like incidence of sore throat in Group B and Group F 10% (3/30) and 53.3% (16/30) P = 0.003 respectively. Incidence of blood staining in Group B and Group F 3.3% (1/30) and 20% (6/30) P = 0.04 respectively, which was significant [Table 4].
Table 4.
Comparison of the incidence of complications between two groups
| Complications | No. of Patients |
P | |
|---|---|---|---|
| Group B | Group F | ||
| Sore throat% | 10 (3/30) | 53.3 (16/30) | 0.003 |
| Nausea and vomiting % | 6.6 (2/30) | 20 (6/30) | 0.12 |
| Blood staining % | 3.3 (1/30) | 20 (6/30) | 0.04 |
| Cough | 0 | 0 | |
| Haemodynamic instability | 0 | 0 | |
| Laryngospasm | 0 | 0 | |
| Aspiration | 0 | 0 | |
DISCUSSION
In the present study, first attempt success rate of blind tracheal intubation was 90% in Group B similar to Yunluo et al.[13] Unlike in our study, they did not mention the attempts taken for intubation. We also did fibreoptic assessment in our study which was not done in their study. Success of first attempt success in Group F was 66.6% similar Liu et al.[14] However, the difference was that they did not do fibreoptic assessment of LMA position as done in our study.
Our results of first pass success do not correspond with Wang et al.[15] because they compared intubation through BlockBuster® LMA with respect to sevoflurane concentration which was not so in our study. The reasons for such high success rate of intubation through BlockBuster® LMA is because of suitable anatomy and alignment of the LMA, the airway tube is >95° angulated and short which aligns with the oropharyngeal curve. Parker flex, inverted tip of BlockBuster® tube helps to overcome impingement of the tube to the anterior tracheal wall during intubation that finds a way in the least resistant areas and the angle made by the BlockBuster® tube while coming out of the cuff is around 30° while it is 40°in Fastrach® LMA [Figure 4] as stated by Su K et al.[16]
Figure 4.
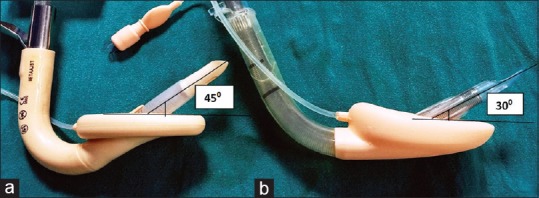
Angle of emergence of endotracheal tube from the cuff of LMA. (a) Fastrach® LMA, (b) BlockBuster® LMA
The overall success rate of insertion of the devices in both the groups was 100% which was similar to various previously conducted studies.[13,17,18] Both the devices were easy to insert with grades being 1 or 2 similar to previous studies.[14,15]
Time for intubation was significantly less in Group B than Group F. The reason for lesser time for intubation in Group B is evident based on the shape and anatomy of the LMA and short airway tube. Our results are similar to previous studies.[13,14,17,18]
Oropharyngeal seal pressure is often used as a surrogate marker for the quality of the airway seal. The clinical implication of higher seal pressures is that such devices provide better and higher peak inspiratory pressures and aid in positive pressure ventilation. In this study the Group B demonstrated higher seal pressures than Group F. The seal pressures were similar to previous studies.[13,15,16] The reason for such high seal pressure is because of an additional dorsal cuff of BlockBuster® LMA which improves seal ability and may reduce the risk of aspiration.
The fibreoptic score of glottis visualisation through LMA was found to be better with BlockBuster® LMA similar to Wang et al.[15] and Keller C et al.[19] The time for removal of LMA was lesser with Group B when compared to Group F. The reason for delay in removal of Fastrach® LMA could be the J shape of the LMA, which if stuck in oropharynx could make it difficult taking more time for removal.
The supraglottic injury score or complication rates like sore throat were less in Group B when compared to Group F because of low resistance exerted by BlockBuster® tube during passage causing reduced subglottic mucosal injury. The results were similar to Su K et al.[16,20] study.
Although BlockBuster® LMA and Fastrach® LMA have similar overall success rate of intubation, BlockBuster® LMA is the preferred choice, because it provides quick and reliable security of airway with good sealing capacity, making it useful for positive pressure ventilation. It has less pharyngeal stimulation causing lesser post use complications. In addition to all this it has extubation capability which helps in safer extubation, with fewer complications.
The significance of our study lies in the fact that although we did blind intubation, we confirmed the actual position of both the devices through fibreoptic scopy so that failure in intubation is not because of faulty position of our devices.
The limitations of this study are that our sample size is less; a higher sample size may be needed to confirm the outcomes. We could not do blinding in our study, so there could be bias. We used a standard scale for assessing the ease of LMA insertion, but it is a subjective scale.
Future scope: Although BlockBuster® LMA came to existence from 2013, very few Chinese studies and no Indian studies are available. More studies need to be done comparing various intubation devices. Our study outcomes can be implemented in normal as well as ASA III and IV (respiratory compromised) patients such that morbidity due to failure in intubation and prolonged apnoea time can be reduced. Patient stay in hospital can also be reduced as airway morbidities lessen.
There are no systematic reviews to refer to with BlockBuster® LMA. Our study outcomes can be implemented for further systematic reviews or meta-analysis.
CONCLUSION
BlockBuster® LMA provides higher success rate of blind tracheal intubation with fewer complications like sore throat and blood staining.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank Dr Shivanand Hulakund, Professor and Head, Department of Anaesthesiology, S N Medical College; Sameer Joshi for providing reference articles; Dr Manjula K, Associate Professor, Department of Community Medicine, for providing statistical help, Dr Bheemappa Bangennavar for providing constant support in writing of the study.
REFERENCES
- 1.Myatra SN, Shah A, Kundra P, Patwa A, Ramkumar V, Divatia JV, et al. All India difficult airway association 2016 guidelines for the management of unanticipated difficult tracheal intubation in adults. Indian J Anaesth. 2016;60:885–98. doi: 10.4103/0019-5049.195481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xiufeng Z, Tian M. The effect of Blockbuster laryngeal mask equipped with ET Tube topatients under general anesthesia. J Pract Med. 2016;32:506–7. [Google Scholar]
- 3.Teoh WH, Lim Y. Comparison of the single use and reusable intubating laryngeal mask airway. Anaesthesia. 2007;62:381–4. doi: 10.1111/j.1365-2044.2007.04980.x. [DOI] [PubMed] [Google Scholar]
- 4.Levitan RM, Ochroch EA, Stuart S, Hollander JE. Use of the intubating laryngeal mask airway by medical and non medical personnel. Am J Emerg Med. 2000;84:103–5. doi: 10.1016/s0735-6757(00)90040-8. [DOI] [PubMed] [Google Scholar]
- 5.Shuai Z, Jing Z, Ye Z, Fang X, Ming T. Application of blind orotracheal intubation via Blockbuster laryngeal mask in patients undergoing general anesthesia. Int J Anesth Resus. 2016;10:917–24. [Google Scholar]
- 6.Ouellette RG. The effect of nitrous oxide on laryngeal mask cuff pressure. AANA J. 2000;68:411–4. [PubMed] [Google Scholar]
- 7.Jagannathan N, Sohn LE, Sawardekar A, Gordon J, Shah RD, Mukherji II, et al. A Randomised trial comparing the Ambu Aura-i with air-q™ intubating LMA as a conduit for tracheal intubation in children. Paediatr Anaesth. 2012;22:156–60. doi: 10.1111/pan.12024. [DOI] [PubMed] [Google Scholar]
- 8.Damodaran S, Sethi S, Malhotra SK, Samra T, Maitra S, Saini V. Comparison of oropharyngeal leak pressure of air-Q™, i-gel™, and laryngeal mask airway supreme™ in adult patients during general anesthesia: A randomized controlled trial. Saudi J Anaesth. 2017;11:390–5. doi: 10.4103/sja.SJA_149_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McNeillis N, Timberlake C, Avidan M, Sarang K, Choyce A, Radcliffe J. Fibreoptic views through the laryngeal mask and the intubating laryngeal mask. Eur J Anaesthesiol. 2001;18:471–5. doi: 10.1046/j.1365-2346.2001.00870.x. [DOI] [PubMed] [Google Scholar]
- 10.Brimacombe J, Berry A. A proposed fibrer-optic scoring system to standardise the assessment of laryngeal mask airway position. Anesth Analg. 1993;76:457. [PubMed] [Google Scholar]
- 11.Siamdoust SS, Rokhtabnak F, Motlagh SD, Rahimzadeh P, Hassani V, Farnaghizad M. Comparison of the Success Rate of IntubationBetween the LMA Fastrach and AirQ-ILA Methods in Patients Undergoing Elective Surgery During General Anaesthesia. Anesth Pain Med. 2018;8:e63424. doi: 10.5812/aapm.63424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kundra P, Garg R, Patwa A, Ahmed SM, Ramkumar V, Shah A, et al. All India Difficult Airway Association 2016 guidelines for the management of anticipated difficult extubation. Indian J Anaesth. 2016;60:915–21. doi: 10.4103/0019-5049.195484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yunluo LY, Yong Z, Yuan Z, Yajie XU, Yanna SI, Hongguang BA. Application of Blockbuster intubating laryngeal mask in urologic day surgery. J Clin Anaesth. 2016;32:960–2. [Google Scholar]
- 14.Liu EH, Goy RW, Lim Y, Chen FG. Success of tracheal intubation with intubating laryngeal mask airways: A randomised trial of the LMA Fastrach and LMA CTrach. Anesthesiology. 2008;108:621–6. doi: 10.1097/ALN.0b013e318167af61. [DOI] [PubMed] [Google Scholar]
- 15.Wang H, Gao X, Wei W, Miao H, Meng H, Tian M. The optimum sevoflurane concentration for supraglottic airway Blockbuster insertion with spontaneous breathing in obese patients. BMC Anesthesiol. 2017;17:156–64. doi: 10.1186/s12871-017-0449-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Su K, Gao X, Xue FS, Ding GN, Zhang Y, Tian M. Difficult tracheal tube passage and subglottic airway injury during intubation with the Glide Scopevideolaryngoscope: A randomized, controlled comparison of three tracheal tubes. Anaesthesia. 2017;72:504–11. doi: 10.1111/anae.13755. [DOI] [PubMed] [Google Scholar]
- 17.Gerstein NS, Braude DA, Hung O, Sanders JC, Murphy MF. The Fastrach™ intubating laryngeal mask airway: An overview and update. Can J Anesth. 2010;57:588–601. doi: 10.1007/s12630-010-9272-x. [DOI] [PubMed] [Google Scholar]
- 18.Ferson DZ, Rosenblatt WH, Johansen MJ, Osborn I, Ovassapian A. Use of intubating LMA- Fastrachin 254 patients with difficult to manage airways. Anesthesiology. 2001;95:1175–81. doi: 10.1097/00000542-200111000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Keller C, Brimacombe J, Pühringer F. A fibreoptic scoring system to assess the position of laryngeal mask airway devices. Interobserver variability and a comparison between the standard, flexible and intubating laryngeal mask airways. Anasthesiol Intensivmed Notfallmed Schmerzther. 2000;35:692–4. doi: 10.1055/s-2000-8164. [DOI] [PubMed] [Google Scholar]
- 20.Kapoor S, Jethava DD, Gupta P, Jethava D, Kumar A. A comparison of supraglottic devices i-gel and LMA Fastrach as conduit for endotracheal intubation. Indian J Anaesth. 2014;58:397–402. doi: 10.4103/0019-5049.138969. [DOI] [PMC free article] [PubMed] [Google Scholar]


