Abstract
BACKGROUND:
Few diseases truly require emergency surgery today. We investigated the relationship between access to operating room (OR) and outcomes for patients with life-threatening emergency general surgery (LT-EGS) diseases at US hospitals.
METHODS:
In 2015, we surveyed 2,811 US hospitals on EGS practices, including how OR access is assured (e.g., OR staffing, block time). There were 1,690 (60%) hospitals that responded. We anonymously linked survey data to 2015 Statewide Inpatient Sample data (17 states) using American Hospital Association identifiers. Adults admitted with life-threatening diagnoses (e.g., necrotizing fasciitis, perforated viscus) who underwent operative intervention the same calendar day as hospital admission were included. Primary outcome was in-hospital mortality. Univariate and multivariable regression analyses, clustered by treating hospital and adjusted for patient factors, were performed to examine hospital-level OR access variables.
RESULTS:
Overall, 3,620 patients were admitted with LT-EGS diseases. The median age was 63 years (interquartile range, 51–75), with half having three or more comorbidities (50%). Thirty-four percent had one or more major systemic complication, and 5% died. The majority got care at hospitals with less than 1 day of EGS block time but with policies to ensure emergency access to the OR. After adjusting for age, sex, race, insurance status, comorbidities, systemic complications, and surgical complications, we found that less presence of an in-house EGS surgeon, compared with around the clock, was associated with increased mortality (rarely/never in-house surgeon: odds ratio, 2.4; 95% confidence interval [CI],1.1–5.3; sometimes in-house surgeon: odds ratio, 1.6; 95% CI, 1.1–2.3). In addition, after controlling for other factors, on-call overnight recovery room nurse, compared with in-house, was associated with an increased mortality (odds ratio, 2.2; 95% CI, 1.5–3.1).
CONCLUSION:
Round-the-clock availability of personnel, specifically emergency general surgeons and recovery room nurses, is associated with decreased mortality. These findings have implications for the creation of EGS patient triage criteria and Acute Care Surgery Centers of Excellence.
LEVEL OF EVIDENCE:
Therapeutic, level III.
Keywords: Emergency general surgery, mortality, survey
Surgeons providing emergency general surgery (EGS) care provide urgent evaluation and possible operation for patients with numerous diseases of varying severity, ranging from appendicitis to necrotizing soft tissue infections (NSTI). Not all surgical emergencies are equal.1 Most surgeons would agree that only a subgroup of surgical emergencies are life-threatening.1 Typically, life-threatening (LT) EGS is indicated for diseases which, in the absence of expeditious source control, can progress rapidly to severe systemic illness, loss of affected organs, or even death. Thus, prompt identification and treatment of these diseases, such as perforated viscus and necrotizing fasciitis, is an imperative for health systems and surgeons providing EGS care.
Physiologic derangement of LT-EGS disease includes septic shock (perforation and/or obstruction of the gastrointestinal tract, with or without abdominal organ ischemia/necrosis) or hemorrhagic shock (without tissue injury).2 Survival is enhanced by early surgical intervention before the development of physiologic derangement.3 Timing of surgical intervention is crucial for LT-EGS diseases. Delay in access to the operating room has been shown to be associated with increased mortality.4 For perforated peptic ulcer disease, an LT-EGS disease, patients had worse outcomes if they were operated on more than 24 hours after their perforation.5 For NSTI, the average time to the operating room was less than 24 hours for those who survived, compared with more than 24 hours for those who died.3,6
The acute care surgery model has been shown to decrease time to the operating room for non–LT-EGS7–10 and LT-EGS diseases.11 However, little is known about factors of a dedicated EGS service that contribute to the improved outcomes associated with acute care surgery models. It is unclear whether the processes, policies, or personnel availability of hospitals are associated with outcomes of patients with LT-EGS diseases. Therefore, the aim of our study was to investigate the relationship between access to operative intervention at hospitals across the United States and outcomes for LT-EGS diseases. We hypothesized that outcomes, in particular mortality, would be improved at hospitals with dedicated resources for round-the-clock access to emergency operations.
METHODS
In 2015, we surveyed 2,811 hospitals across the United States regarding their EGS practices, including how to access surgical care is assured through a number of key structural and process features (e.g., overnight presence of EGS surgeon, scrub technicians, operating room nurses, recovery room nurses, anesthesiologists, and certified registered nurse anesthetists;, EGS surgery block time; process for tiering emergency cases). Hereafter, these will be referred to as, “OR access resources.” The methods of the survey development and implementation have been previously described.12 In total, 1,690 US hospitals were represented in our survey data (60.1% response).
Respondent answers to queries regarding OR access structure and process measures were anonymously linked to 2015 State Inpatient Databases (SID) using American Hospital Association Unique identifiers (AHAID). The SID are a product of the Healthcare Cost and Utilization Project (HCUP) with 48 states currently participating. Each SID is an all-payer database that includes inpatient discharge records from community hospitals (nonfederal, nonprison, accessible to any community member) in any given state that is translated by HCUP into a uniform format to facilitate multi-state comparisons and analyses. Together, the SID encompass about 97% of all US community hospital discharges.13 In 2015, 17 states released data with AHAID thus allowing for linkage to survey responses from the 368 hospitals in our overall sample located in those states.
From SID data, we identified all emergent/urgent admissions for adults 18 years and older to acute care hospitals with a primary LT-EGS diagnoses (e.g., necrotizing fasciitis, perforated viscus, strangulated hernia) (Supplemental Digital Content, Appendix 1, http://links.lww.com/TA/B371) requiring an operation (Supplemental Digital Content, Appendix 2, http://links.lww.com/TA/B371) on the date of admission. Since only dates, and not times, of procedures are coded in the SID data, operation on the same date as admission was considered an emergency operation. Patients who did not undergo operation were excluded to prevent double counting patients treated at more than one hospital for the same episode of an LT-EGS condition and to exclude those who did not undergo surgery but rather died soon after admission due to unmeasured reasons, such as preexisting code status. The primary outcome was in-hospital mortality. Secondary outcomes included length of stay, systemic complications, and surgical complications (Supplemental Digital Content, Appendix 3, http://links.lww.com/TA/B371).
Using bivariate and multivariable models, we measured the association between the outcome of interest and the treating hospital’s OR access resources. Multivariable models were adjusted for patient demographic characteristics and clinical covariates, including age, sex, race, insurance status, Elixhauser comorbidity index,14 systemic complications, and surgical complications. This research was reviewed and approved by the institutional review boards at both the University of Massachusetts Medical School and the Ohio State University College of Medicine.
RESULTS
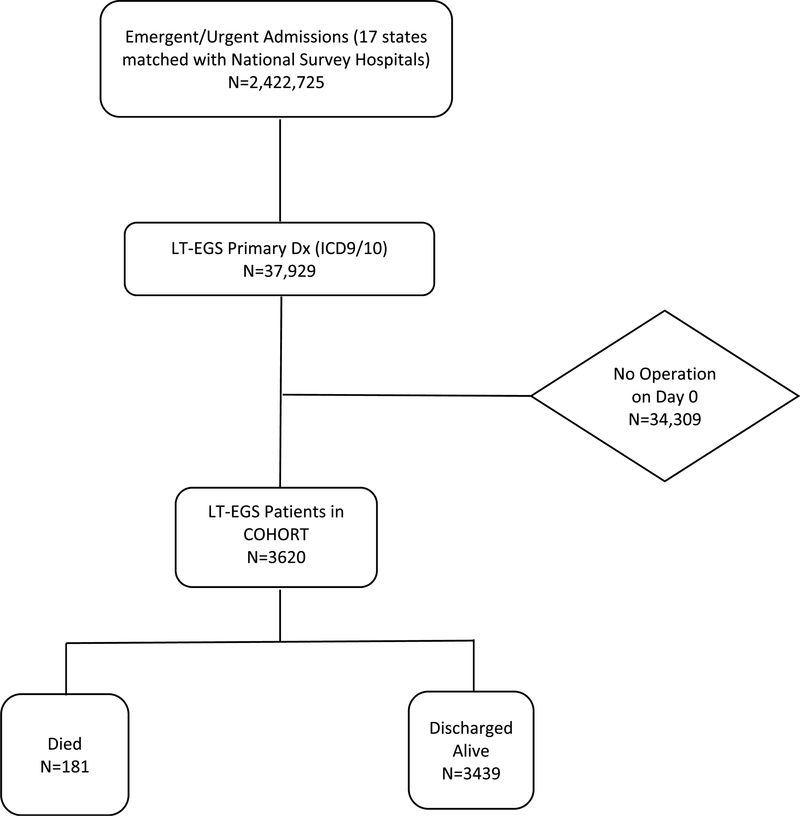
We identified 3,620 patients with LT-EGS diagnoses requiring surgical intervention on the same calendar day as hospital admission (Fig. 1). Table 1 shows the hospital level resources, policies, or procedures aimed at ensuring access to operation. Of the 368 hospitals, majority had EGS block time of less than 1 day, an overnight surgeon available, and always or often had the daytime on-call surgeon working postcall. Table 2 describes characteristics, interventions, and outcomes for our cohort. The median age was 63 years (interquartile range [IQR], 51–75), with 50% having three or more comorbidities. 34% had one or more major systemic complication, 31% had a major operative complication, and 5% died.
Figure 1.
Flow diagram of the creation of the study’s cohort and patient outcomes.
TABLE 1.
Hospital Level Resources, Policies, or Procedures Aimed at Ensuring Access to Operation
| Resource, Policy, or Procedure Aimed at Ensuring Access to Operation |
No. Hospitals, n = 368 (%) |
|---|---|
| Total operating rooms, median (IQR) | 19 (9–28) |
| Block time for EGS | |
| <1 day (none, <1) | 276 (75.0%) |
| 1–4 days (1,2, 3, 4) | 15 (4.1%) |
| ≥5 days (5, >5) | 65 (17.7%) |
| Tiered system for booking emergent surgical cases | 235 (63.9%) |
| Process to defer elective cases | 251 (68.2%) |
| Overnight OR access available | 364 (71.4%) |
| Total number of surgeons covering EGS, Median (IQR) | 5 (3, 8) |
| Daytime surgeons covering EGS free of other clinical duties | 57 (15.5%) |
| Daytime surgeon on call for EGS working postcall | |
| Always/often | 280 (76.1%) |
| Sometimes | 40 (10.9%) |
| Rarely/never | 31 (8.4%) |
| Daytime EGS coverage scheme | |
| On service weeks—5 consecutive days or greater (reference) | 50 (13.6%) |
| Ad hoc daytime shift coverage | 34 (9.2%) |
| Traditional 24-hour coverage | 228 (62.0%) |
| Other | 13 (3.5%) |
| In-house surgeon overnight for EGS | |
| Always/often | 132 (35.9%) |
| Sometimes | 23 (6.3%) |
| Rarely/never | 196 (53.3%) |
| Overnight surgeon also responsible for covering trauma | |
| Always/often | 235 (63.9%) |
| Sometimes | 16 (4.3%) |
| Rarely/never | 101 (27.4%) |
| Overnight surgeon also responsible for covering ICU care | |
| Always/often | 132 (35.9%) |
| Sometimes | 34 (9.2%) |
| Rarely/never | 186 (50.5%) |
| Overnight surgeon also responsible for covering EGS at more than one hospital | |
| Always/often | 55 (14.9%) |
| Sometimes | 40 (10.9%) |
| Rarely/never | 256 (69.6%) |
| Overnight scrub technicians | |
| None | — |
| On-call | 248 (67.4%) |
| In-house | 113 (30.7%) |
| Overnight OR nurses | |
| None | — |
| On-call | 250 (67.9%) |
| In-house | 111 (30.2%) |
| Overnight recovery room nurses | |
| None | 7 (1.9%) |
| On-call | 293 (79.6%) |
| In-house | 58 (15.8%) |
| Overnight anesthesia staff (MD, DO, CRNA) | |
| None | 44 (12.0%) |
| On-call | 192 (52.2%) |
| In-house | 121 (32.9%) |
Total may not add to 368 given missing data from variables. SNF, Skilled nursing facility; LTAC, Long-term acute care hospital.
TABLE 2.
Characteristics, Interventions, and Outcomes for Patients Admitted in 2015 to 368 Hospitals in 17 States With a LT-EGS
| Variables | Patients With LT-EGS (N = 3,620), n (%) |
|---|---|
| Demographics | |
| Age (median, IQR) | 62.5 (51–75) |
| Male | 1,737 (48.0) |
| Race | |
| Non-Hispanic White | 2,720 (75.1) |
| Black | 286 (7.9) |
| Hispanic | 158 (4.4) |
| Other | 88 (2.4) |
| Unknown | 368 (10.2) |
| Insurance | |
| Medicare | 1,665 (46.0) |
| Medicaid | 475 (13.1) |
| Private | 1,204 (33.3) |
| Self-pay | 159 (4.4) |
| Other | 116 (3.2) |
| Arrival status | |
| Directly to ER | 3,401 (94.0) |
| From Skilled nursing facility, rehab, | 164 (4.5) |
| LTAC | |
| For other acute care hospital | 55 (1.5) |
| LT-EGS condition category | |
| NSTI | 150 (4.1) |
| Intra-abdominal catastrophe | 3,470 (95.9) |
| Comorbidities | |
| Elixhauser Index | |
| No comorbidities | 505 (13.9) |
| 1 comorbidity | 659 (18.2) |
| 2 comorbidities | 633 (17.5) |
| 3 or more comorbidities | 1,823 (50.4) |
| Outcomes | |
| In-patient mortality | 181 (5.0%) |
| Total hospital length of stay, median (IQR) | 7 (5–10) |
| Major systemic complications | 1,230 (34.0) |
| Major operative complications | 1,131 (31.2) |
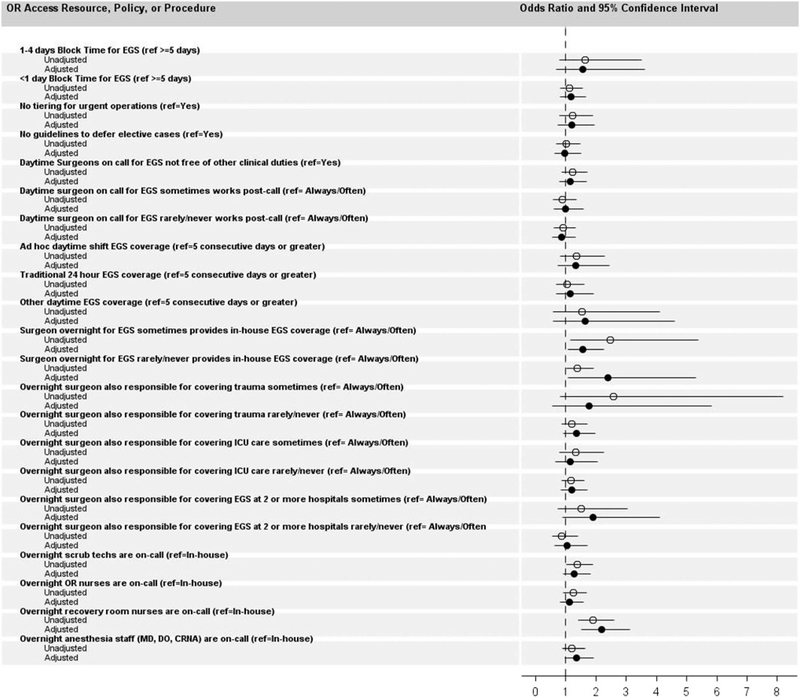
Table 3 shows patient-level differences in exposure to hospital-level operating room resources among patient who died and were discharged alive. The median number (IQR) of operating rooms in hospitals where patients survived to discharge was 19 (IQR, 9–28) compared to a median of 20 operating rooms (IQR, 10–33) in hospitals where patients died (p = 0.03). Figure 2 shows unadjusted and adjusted odds ratio for patients with each operating room access variable. After adjusting for age, sex, race, insurance status, comorbidities, systemic complications, and surgical complications, we found that less availability of an in-house EGS surgeon, compared to “around the clock,” was associated with increased mortality (rarely/never in-house surgeon: odds ratio, 2.4; 95% CI, 1.1–5.3; sometimes in-house surgeon: odds ratio, 1.6; 95% CI, 1.1–2.3). In addition, after controlling for other factors, on-call overnight recovery room nurse, compared with in-house, was associated with increased mortality (odds ratio, 2.2; 95% CI, 1.5–3.1). On-call overnight anesthesia staff (MD, DO, CRNA), compared with in-house was associated with a 1.4 times increased odds of mortality, however, was not significant (95% CI, 0.96–1.2).
TABLE 3.
Patient-Level Differences in Exposure to Hospital-Level OR Resources Among Patient Who Died and Were Discharged Alive
| Hospital Level Resources, Policies, or Procedures Aimed at Ensuring Access to Operation |
Survived to Discharge (n = 3439), n (%) |
Died (n = 181), n (%) | p value |
|---|---|---|---|
| Total operating rooms, median (IQR) | 19 (9–28) | 20 (10–33) | 0.03 |
| Block time for EGS | 0.40 | ||
| <1 d (none, <1) | 2,150 (62.5) | 110 (60.8) | |
| 1–4 d (1, 2, 3, 4) | 231 (6.7) | 8 (4.4) | |
| ≥5 d (5, >5) | 960 (27.9) | 55 (30.4) | |
| Tiered system for booking emergent surgical cases | 2,510 (73) | 144 (79.6) | 0.38 |
| Process to defer elective cases | 2,476 (72) | 136 (75.1) | 0.97 |
| Overnight OR access available | 3,417 (99.4) | 178 (98.3) | 0.98 |
| Total number of surgeons covering EGS, Median (IQR) | 5 (3, 8) | 7 (4, 9) | 0.87 |
| Daytime surgeons covering EGS free of other clinical duties | 745 (21.7) | 47 (26) | 0.26 |
| Daytime surgeon on call for EGS working postcall (%) | 0.78 | ||
| Always/often | 2,118 (61.6) | 109 (60.2) | |
| Sometimes | 480 (14) | 28 (15.5) | |
| Rarely/never | 648 (18.8) | 37 (20.4) | |
| Daytime EGS coverage scheme | 0.46 | ||
| On service weeks—5 consecutive days or greater (reference) | 524 (15.2) | 26 (14.4) | |
| Ad hoc daytime shift coverage | 518 (15.1) | 35 (19.3) | |
| Traditional 24-hour coverage | 2,023 (58.8) | 104 (57.5) | |
| Other | 66 (1.9) | 5 (2.8) | |
| In-house surgeon overnight for EGS | 0.01 | ||
| Always/often | 1,627 (47.3) | 105 (58) | |
| Sometimes | 269 (7.8) | 7 (3.9) | |
| Rarely/never | 1,358 (39.5) | 63 (34.8) | |
| Overnight surgeon also responsible for covering trauma | 0.16 | ||
| Always/often | 2,223 (64.6) | 129 (71.3) | |
| Sometimes | 133 (3.9) | 3 (1.7) | |
| Rarely/never | 898 (26.1) | 43 (23.8) | |
| Overnight surgeon also responsible for covering ICU care | 0.45 | ||
| Always/often | 1,335 (38.8) | 79 (43.6) | |
| Sometimes | 381 (11.1) | 17 (9.4) | |
| Rarely/never | 1,534 (44.6) | 77 (42.5) | |
| Overnight surgeon also responsible for covering EGS at more than one hospital | 0.17 | ||
| Always/often | 420 (12.2) | 21 (11.6) | |
| Sometimes | 391 (11.4) | 13 (7.2) | |
| Rarely/Never | 2,432 (70.7) | 139 (76.8) | |
| Overnight scrub techs | 0.04 | ||
| None | — | — | |
| On-call | 1,534 (44.6) | 66 (36.5) | |
| In-house | 1,865 (54.2) | 111 (61.3) | |
| Overnight OR nurses | 0.17 | ||
| None | — | — | |
| On-call | 1,560 (45.4) | 72 (39.8) | |
| In-house | 1,839 (53.5) | 105 (58) | |
| Overnight recovery room nurses | <0.01 | ||
| None | 53 (1.5) | 2 (1.1) | |
| On-call | 2,405 (69.9) | 100 (55.2) | |
| In-house | 929 (27) | 74 (40.9) | |
| Overnight anesthesia staff (MD, DO, CRNA) | 0.20 | ||
| None | 95 (2.8) | 2 (1.1) | |
| On-call | 1,464 (42.6) | 70 (38.7) | |
| In-house | 1,838 (53.4) | 106 (58.6) | |
Figure 2.
Unadjusted and adjusted odds ratio for patients from hospitals with or access variables.
DISCUSSION
Although a myriad of studies report improved outcomes associated with a dedicated EGS service, such as an acute care surgery model,7–9,11,15,16 little was previously known regarding specific resources which contributed to the improved survival among EGS patients. This present study found that round-the-clock availability of personnel, specifically emergency general surgeons and recovery room nurses, was associated with decreased mortality. Interestingly, we found that processes and policies to expedite OR access during the day was not associated with improved survival. This is the first study to demonstrate the relationship between round-the-clock presence of personnel and improved survival among patients with LT-EGS diseases. In an era when EGS comprises a significant proportion of mortality associated with the field of general surgery,17 it is crucial that we strive to implement EGS processes that will reduce the mortality rates nationally.
Single-center studies have previously shown that availability of emergency general surgeons, as proxy of utilization of an acute care surgery model, may improve outcomes. Early et al.9 suggested that increased availability of surgeons may be associated with shorter time to operative intervention for appendicitis. In addition, Moore et al.11 reported that increased availability of EGS surgeons appears to improve survival among patients undergoing emergent colon resection. Neither studies investigated the availability of emergency general surgeons as a dependent variable, but rather suggested that the availability of surgeons is what may have driven the relationship between acute care model utilization and improved patient outcomes. Compared with previous studies, our study is unique given that we deliberately studied the availability of personnel, and our results represent more granular operating room access variables with data from 17 states. We included variables studying OR processes and policies to expedite OR access, and none of these variables were significant. Therefore, it is less likely that our results are related to increased availability of personnel being a surrogate for a well-resourced hospital. Understanding which specific EGS structures and processes expedite operative intervention will aid in the development of highly effective EGS care teams in an era of decreasing access to EGS care.12
The disproportionately higher mortality associated with EGS compared with elective surgery17–19 may be due to variability of EGS care nationally20,21 in addition to patient variability, such as acute physiology and chronic comorbidities. We found that processes at the system level, such as a having a tiered system to book emergent surgical cases occurred in less than half of the hospitals. This is one example of the variability between hospitals in processes. In addition, system variability, such as EGS workforce and operating room access, may be just as crucial. Columbus et al.20 suggested that system variability is one potential domain for quality improvement in EGS care. McIsaac et al.4 also showed that the predominant reason for delay was system issues, such as the physician availability and physical resources. These delays to the operating room, however, are associated with greater mortality of patients.4
Given the results of this study, strategies to improve the availability of surgeons and recovery room nurses must be urgently sought. A potential solution to improve availability of operating room staff and resources may be the widespread adoption of acute care surgery models to provide EGS care. It is important to highlight that our previous work demonstrated that certain hospitals, such as large hospitals with academic affiliations, may have the needed infrastructure, resources, and human capital to support an acute care surgery model providing round-the-clock staffing and resources.21 To prevent poor outcomes among hospitals unable to provide these necessary infrastructure and human capital to expedite access to operative intervention in true emergencies, regionalization of Acute Care Surgery into Centers of Excellence may prove beneficial.
Our results must be understood in the context of a number of limitations. Although we have robust primary data representing OR access resources from 368 hospitals in the United States capable of providing EGS care, our survey, like all such surveys utilizing self-reported data, is subject to social desirability bias, recall bias, and lack of generalizability. However, our stepwise method of survey creation and pilot testing, along with our high response rate, mitigate these risks. In addition, our patient-level outcomes data are generated from administrative data; limitations of such data sets include the possibility of systematic upcoding and lack of clinical granularity. In addition, given the definition of LT-EGS as the same calendar day as hospital admission, we may have underrepresented the number of LT-EGS cases. If a patient with LT-EGS disease presented to the hospital and underwent LT-EGS within 24 hours, yet the surgery was on the calendar day following admission, the patient was not classified as LT-EGS in an attempt to be conservative.
Despite these limitations, this study is unique given that we linked the surgeons’ responses about EGS processes and hospital characteristics with patient outcomes extracted from state-wide databases. In addition, focusing on LT-EGS diseases, instead of all EGS diseases that include non–life-threatening diseases, created a more homogenous population of patients.
This study reveals an important aspect of improving LT-EGS care. Round-the-clock in-house availability of personnel, specifically EGS surgeons and recovery room nurses, may need prioritization to improve the timeliness of LT-EGS care. That people are in fact more important than policies aimed at ensuring OR access has important implications for the design of optimal EGS care delivery models. Given the resource intensiveness required for all hospitals to have round-the-clock in-house EGS staff, there are implications for the creation of EGS patient triage criteria and acute care surgery centers of excellence.
Supplementary Material
ACKNOWLEDGMENTS
We thank Catarina I. Kiefe, MD, PhD for her expertise and mentorship throughout all the aspects of the study.
Presentations: This article was presented as an oral presentation at the 32nd Eastern Association for the Surgery of Trauma Annual Scientific Assembly in Austin, Texas from January 15–19, 2019. This article was also the winner of the 2019 Raymond H. Alexander, MD Resident Paper Competition (Clinical Science Paper).
FUNDING STATEMENT: This research is supported by a grant from the Agency for Healthcare Research Quality (R01HS022694) to HPS. The content represents the thoughts and opinions of the authors and not the funding agencies. Dr. Heena Santry had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
EDITORIAL CRITIQUE
Dr. Daniel and colleagues have linked the HCUP Statewide Inpatient Sample data with survey data identifying availability of surgical resources to address whether having an in-house surgical attending and team, rather than an on-call team, would improve patient outcomes. Their data analyses imply that in-house surgical coverage is critical to patient outcomes from truly emergent surgical disease. These data however must be taken in context.
There is a growing evidence to suggest a volume to outcomes relationship for emergency general surgery (EGS). Specifically, hospitals with higher EGS volumes have better outcomes. The authors were unable to assess hospital size, volume of EGS operations or trauma center designation; without these data they are unable to determine whether having in-house surgical coverage was merely a surrogate for larger hospitals, with higher volumes of EGS and therefore better outcomes.
The authors focused on patients who had their care delivered within a 24-hour period but not actual time to source control, a level of granularity that addresses the crux of emergency surgical care. This again would beg the question whether institutions with in-house surgical teams better reflect the ready availability of a wide range of resources necessary to care for critically ill patients.
Finally, while I applaud the successes of the trauma system, I think we need to be cautious when discussing regionalization of emergency general surgery. Most EGS is performed in the 90% of hospitals that are outside of the trauma systems. Many of these institutions represent critical access hospitals that may not have the volume of EGS or the patient acuity to support costly in-house surgical resources. Recent work from Dr. Shahid Shafi would suggest that only 5% of EGS patient have a degree of complexity that would mandate tertiary or quaternary care. We must thoughtfully balance resources to patient need to assure optimal care.
I would like to congratulate the authors for taking on a question which will continue to confound national surgical leadership as we endeavor to provide optimal care for our patients with time critical surgical disease. This is a timely and important topic that deserves ongoing investigation.
Kimberly A. Davis MD, MBA
Footnotes
DISCLOSURE
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
Disclosure Information
In accordance with the ACCME Accreditation Criteria, the American College of Surgeons, as the accredited provider of this journal activity, must ensure that anyone in a position to control the content of J Trauma Acute Care Surg articles selected for CME credit has disclosed all relevant financial relationships with any commercial interest. Disclosure forms are completed by the editorial staff, associate editors, reviewers, and all authors. The ACCME defines a `commercial interest' as “any entity producing, marketing, re-selling, or distributing health care goods or services consumed by, or used on, patients.” “Relevant” financial relationships are those (in any amount) that may create a conflict of interest and occur within the 12’months preceding and during the time that the individual is engaged in writing the article. All reported conflicts are thoroughly managed in order to ensure any potential bias within the content is eliminated. However, if you’perceive a bias within the article, please report the circumstances on the evaluation form.
Please note we have advised the authors that it is their responsibility to disclose within the article if they are describing the use of a device, product, or drug that is not FDA approved or the off-label use of an approved device, product, or drug or unapproved usage.
Disclosures of Significant Relationships with Relevant Commercial Companies/Organizations by the Editorial Staff
Ernest E. Moore, Editor: PI, research support and shared U.S. patents Haemonetics; PI, research support, Instrumentation Laboratory, Inc.; Co-founder, Thrombo Therapeutics. Associate Editors David Hoyt, Ronald V. Maier and Steven Shackford have nothing to disclose. Editorial staff and Angela Sauaia have nothing to disclose.
Author Disclosures
None.
Reviewer Disclosures
The reviewers have nothing to disclose.
REFERENCES
- 1.Leppaniemi A What is acceptable delay in emergency abdominal surgery? Scand J Surg. 2013;102(2):54. [DOI] [PubMed] [Google Scholar]
- 2.Weber DG, Bendinelli C, Balogh ZJ. Damage control surgery for abdominal emergencies. Br J Surg. 2014;101(1):e109–e118. [DOI] [PubMed] [Google Scholar]
- 3.Gunter OL, Guillamondegui OD, May AK, Diaz JJ. Outcome of necrotizing skin and soft tissue infections. Surg Infect (Larchmt). 2008;9(4):443–450. [DOI] [PubMed] [Google Scholar]
- 4.McIsaac DI, Abdulla K, Yang H, Sundaresan S, Doering P, Vaswani SG, Thavorn K, Forster AJ. Association of delay of urgent or emergency surgery with mortality and use of health care resources: a propensity score-matched observational cohort study. CMAJ. 2017;189(27):E905–E12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vester-Andersen M, Lundstrom LH, Buck DL, Moller MH. Association between surgical delay and survival in high-risk emergency abdominal surgery. A population-based Danish cohort study. Scand J Gastroenterol. 2016;51(1): 121–128. [DOI] [PubMed] [Google Scholar]
- 6.McHenry CR, Piotrowski JJ, Petrinic D, Malangoni MA. Determinants of mortality for necrotizing soft-tissue infections. Ann Surg. 1995;221(5): 558–563; discussion 563–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chana P, Burns EM, Arora S, Darzi AW, Faiz OD. A systematic review of the impact of dedicated emergency surgical services on patient outcomes. Ann Surg. 2016;263(1):20–27. [DOI] [PubMed] [Google Scholar]
- 8.Cubas RF, Gomez NR, Rodriguez S, Wanis M, Sivanandam A, Garberoglio CA. Outcomes in the management of appendicitis and cholecystitis in the setting of a new acute care surgery service model: impact on timing and cost. J Am Coll Surg. 2012;215(5):715–721. [DOI] [PubMed] [Google Scholar]
- 9.Earley AS, Pryor JP, Kim PK, Hedrick JH, Kurichi JE, Minogue AC, Sonnad SS, Reilly PM, Schwab CW. An acute care surgery model improves outcomes in patients with appendicitis. Ann Surg. 2006;244(4):498–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Michailidou M, Kulvatunyou N, Friese RS, Gries L, Green DJ, Joseph B, O’Keeffe T, Tang AL, Vercruysse G, Rhee P. Time and cost analysis of gallbladder surgery under the acute care surgery model. J Trauma Acute Care Surg. 2014;76(3):710–714. [DOI] [PubMed] [Google Scholar]
- 11.Moore LJ, Turner KL, Jones SL, Fahy BN, Moore FA. Availability of acute care surgeons improves outcomes in patients requiring emergent colon surgery. Am J Surg. 2011;202(6):837–842. [DOI] [PubMed] [Google Scholar]
- 12.Khubchandani JA, Ingraham AM, Daniel VT, Ayturk D, Kiefe CI, Santry HP. Geographic diffusion and implementation of acute care surgery: an uneven solution to the National Emergency General Surgery Crisis. JAMA Surg. 2018;153(2):150–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Introduction to the HCUP State Inpatient Databases (SID). Rockville, MD: Agency for Healthcare Research & Policy (AHRQ); 2018. [Google Scholar]
- 14.Elixhauser A, Steiner C, Harris DR, Coffey RM . Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 15.Diaz JJ Jr., Norris P, Gunter O, Collier B, Riordan W, Morris JA Jr Triaging to a regional acute care surgery center: distance is critical. J Trauma. 2011; 70(1):116–119. [DOI] [PubMed] [Google Scholar]
- 16.To KB, Kamdar NS, Patil P, et al. Acute care surgery model and outcomes in emergency general surgery. J Am Coll Surg. 2019;228(1):21–28.e7. [DOI] [PubMed] [Google Scholar]
- 17.Havens JM, Peetz AB, Do WS, Cooper Z, Kelly E, Askari R, Reznor G, Salim A. The excess morbidity and mortality of emergency general surgery. J Trauma Acute Care Surg. 2015;78(2):306–311. [DOI] [PubMed] [Google Scholar]
- 18.Ingraham AM, Cohen ME, Bilimoria KY, et al. Comparison of 30-day outcomes after emergency general surgery procedures: potential for targeted improvement. Surgery. 2010;148(2):217–238. [DOI] [PubMed] [Google Scholar]
- 19.Ingraham AM, Cohen ME, Raval MV, Ko CY, Nathens AB, Hall BL. Comparison of hospital performance in emergency versus elective general surgery operations at 198 hospitals. J Am Coll Surg. 2011;212(1): 20–8.e1. [DOI] [PubMed] [Google Scholar]
- 20.Columbus AB, Morris MA, Lilley EJ, Harlow AF, Haider AH, Salim A, Havens JM. Critical differences between elective and emergency surgery: identifying domains for quality improvement in emergency general surgery. Surgery. 2018;163(4):832–838. [DOI] [PubMed] [Google Scholar]
- 21.Daniel VT, Ingraham AM, Khubchandani JA, Ayturk D, Kiefe CI, Santry HP. Variations in the delivery of emergency general surgery care in the era of acute care surgery. Jt Comm J Qual Patient Saf. 2019;45(1):14–23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.