Short abstract
Introduction
Adequate planning and implementation of stroke systems of care is key to guarantee a rapid healthcare response and delivery of specific reperfusion therapies among candidates. We assessed the availability of stroke care plans in Europe, and evaluated their impact on rates of reperfusion therapies for stroke.
Patients
Based on the European Stroke Organisation (ESO), the European Society of Minimally Invasive Neurological Therapy (ESMINT), the European Academy of Neurology (EAN), and the Stroke Alliance for Europe (SAFE) survey, we analysed specific prespecified items in the questionnaire regarding availability and adequacy of stroke care plans, organised prehospital care and their potential impact on rates of delivery of reperfusion therapies for stroke at the country level.
Results
Of 44 participating European countries, 37 have stroke care plans that operate at national and/or regional levels. Most stroke care plans take responsibility for the organisation/implementation of stroke systems of care (86%), quality of care assessment (77%), and act as a liaison between emergency medical systems and stroke physicians (79%). As for stroke systems of care, the focus is mainly on prehospital and in-hospital acute stroke care (Code Stroke systems available in 37/44 countries). Preferred urgent transport is via non-medicalised ambulances (70%). Presence of stroke care plans, stroke registry data, transport of urgent stroke patients via non-medicalised ambulances, and drip-and-ship routing of acute patients showed higher reperfusion treatment rates.
Discussion
Availability of stroke care plans, still absent in some European countries, as well as some features of the stroke systems of care are associated with higher reperfusion treatment rates.
Conclusion
Stroke is not yet a priority everywhere in Europe, which is a barrier to the spread of reperfusion therapies for stroke.
Keywords: Stroke, prehospital care, systems of care, quality of care, intravenous thrombolysis, mechanical thrombectomy
Introduction
Large disparities in health exist across and within European countries,1,2 and raising awareness of these health inequalities as well as supporting the development of transnational policies to address them is key to shorten the gap between evidence and practice. In 2017, the publication The Burden of Stroke in Europe by the Stroke Alliance for Europe (SAFE) suggested a 34% increase in stroke incidence by 2035, a 45% increase of stroke deaths, and a 25% increase of stroke survivors living with the consequences of stroke.3 To mitigate the increase in stroke burden, SAFE called EU policy makers to support a joint action on stroke, addressing – among others – topics such as data collection, promotion and implementation of national stroke strategies, and performance assessment. To achieve this, ESO in collaboration with SAFE developed the Action Plan for Stroke in Europe 2018–2030.4
At the national level, concerns of health authorities on the abovementioned projections have translated into the establishment of stroke care plans, strategies, guidelines and programmes of action. To maximise the numbers of acute stroke patients accessing specific reperfusion therapies, stroke care plans have mainly focused on the implementation of organised systems of care that aim to ease rapid access of acute stroke patients to stroke unit (SU) care and such therapies. However, it is unknown to what extension this is true for European countries, what the main lines of action of stroke care plans are, how acute stroke care is organised, etc. Therefore, the objective of this study is to describe the situation among European countries in relation to stroke planning, stroke care organisation and to explore their association with reperfusion treatment rates.
Methods
Study design and participants
This study is based on data from a pan-European survey conducted among European chairs of national stroke societies and stroke experts. The survey’s steering committee consisted of 10 representatives from the European Stroke Organisation (ESO), the European Society of Minimally Invasive Neurological Therapy (ESMINT), the European Academy of Neurology (EAN) and the Stroke Alliance for Europe (SAFE), including at least one board member from each society. The World Health Organization (WHO) definition of the European region consisting of 51 countries was adopted. Countries with less than 100,000 inhabitants (Monaco, Liechtenstein, Andorra, and San Marino) were excluded, and North Cyprus, which was not listed under the WHO definition, was added. Details of the survey have been described in depth elsewhere.5 Briefly, the survey consisted of 64 items organised into five sections corresponding to: (1) organisation of stroke systems of care, (2) prehospital stroke care, (3) specific stroke treatment, (4) stroke registries and quality control, and (5) stroke awareness campaigns. This study focuses on contents of this section and the previous section.
Coordinators and experts from 44 European countries (see Appendix 1 for the list of collaborators) were responsible for identifying the most reliable and recent national data sources (i.e. stroke registries, governmental data sources) to answer the survey questions. In the absence of national or local stroke registries, the coordinator and experts were asked to perform best estimates by consensus and took full responsibility for the validity of the responses provided.
Data collection
The survey was announced through ESO, ESMINT and EAN newsletters six months before it started, and finally performed between 30 October 2016 and 24 February 2017. A draft version of the survey was externally reviewed by four stroke experts (see, Acknowledgments) with extensive research skills and proven experience in drafting European stroke surveys. A pilot feasibility survey was accomplished in Austria, Hungary, Poland, Spain and Switzerland.
Data analyses
Our analyses focused on the planning and organisation of stroke systems of care, including prehospital care. All data were analysed using appropriate descriptive methods. Intravenous thrombolysis (IVT) and endovascular treatment (EVT) rates were compared between groups using the Kruskall–Wallis test by ranks. Number of residents per country, and population-based IVT and EVT rates were derived from the original paper.5
Results
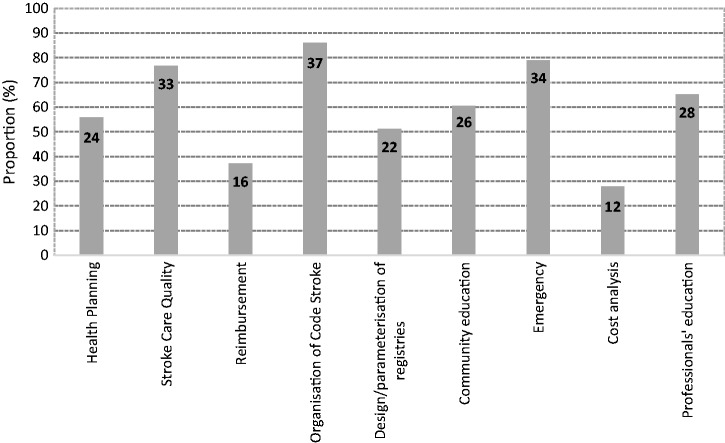
Overall, 44 of 51 invited countries participated in the survey (response rate: 86%). Among the 44 respondents, with an overall population of about 835 millions, the absolute number of incident strokes ranged from 240 to 250,000 cases/year. In 37 (86.1%) out of 44 countries, there was a stroke care plan, which in most countries operated at the national and/or regional level (national only: 20, regional only: 3, and both: 11 countries). In six other countries (Croatia, Kyrgyzstan, Belarus, Greece, Romania, Ukraine), the stroke care plan operated at a local level. There were no differences regarding stroke care plan level (country-, region-, both-, and none) by size of country population (Table 1). As for the specific aims of the respective stroke care plans, involvement in stroke care quality improvement initiatives (n = 33), organising and implementing stroke systems of care (n = 37), and leading Emergency Medical Systems involvement (EMS) and their cooperation with stroke physicians (n = 34) were the most common goals (Figure 1). Across Europe, stroke care plans were not always comprehensive, and often they did not approach the whole continuum of stroke care. However, stroke care plans most commonly focused on the initial Emergency Room admission and the acute hospital management of stroke patients (41 and 43 countries, respectively). In line with this, in 37 out of 44 European countries there existed a Code Stroke protocol with involvement of the EMS. In 2/3 of countries, the Code Stroke was supported by an instruction; that is, an official document that establishes the territorial compartmentalisation and operational criteria. The protocol is activated whenever sudden neurological impairment suggesting a stroke is identified, and common constraints to code stroke activation included late presentation after symptoms onset (59%) and premorbid disability (28%). Most EMS protocols implied transporting acute stroke patients in non-medicalised (staffed with technicians) ambulances (70%) but medicalised ambulances (staffed with a general physician and a nurse) were also available in more than half of the countries surveyed either as first-line carrier or as a second-line resource used in specific clinical conditions. Availability of mobile SUs was only limited.
Table 1.
Description of Stroke Care Plans by country.
| Population subgroup | Country | Population | Total area served (km2) | Stroke Plan | Stroke Plan level | Regional organisation of stroke care | No. of areas | Regional differences |
|---|---|---|---|---|---|---|---|---|
| <1 million | Northern Cyprus | 300,000 | 3355 | No | Region only | Yes | 5 | Yes |
| Iceland | 333,000 | 102,775 | Yes | Country only | No | – | Yes | |
| Malta | 420,000 | 316 | Yes | Country only | Yes | 2 | Yes | |
| Montenegro | 621,000 | 13,812 | Yes | Country only | No | – | No | |
| Overall | 418,500 | 30,065 | 75% | 75% country only | 50% | 75% | ||
| 25% region only | ||||||||
| 1–10 million | Estonia | 1,325,000 | 45,339 | Yes | Country only | No | – | No |
| Latvia | 1,800,000 | 64,589 | Yes | Neither | Yes | 6 | No | |
| Macedonia | 2,000,000 | 25,713 | Yes | Country only | Yes | 4 | Yes | |
| Slovenia | 2,065,000 | 20,273 | Yes | Both | Yes | 12 | No | |
| Lithuania | 3,000,000 | 65,300 | Yes | Country only | Yes | 5 | No | |
| Albania | 3,100,000 | 28,748 | Yes | Region only | No | – | Yes | |
| Bosnia and Herzegovina | 3,517,000 | 51,129 | No | Both | Yes | 11 | Yes | |
| Republic of Moldova | 3,600,000 | 33,846 | Yes | Country only | No | – | No | |
| Georgia | 3,700,000 | 2428 | Yes | Neither | No | – | Yes | |
| Croatia | 4,171,000 | 56,594 | Yes | Local | No | – | Yes | |
| Ireland | 4,800,000 | 70,273 | Yes | Country only | No | – | Yes | |
| Norway | 5,000,000 | 385,178 | Yes | Both | Yes | 5 | No | |
| Slovakia | 5,400,000 | 49,036 | Yes | Country only | No | – | Yes | |
| Finland | 5,495,000 | 338,145 | Yes | Both | Yes | 21 | Yes | |
| Denmark | 5,600,000 | 44,493 | Yes | Country only | Yes | 5 | No | |
| Kyrgyzstan | 6,000,000 | 199,949 | No | Local | Yes | 7 | Yes | |
| Bulgaria | 7,000,000 | 110,994 | Yes | Both | Yes | 28 | Yes | |
| Switzerland | 8,081,000 | 41,290 | Yes | Country only | Yes | 8 | No | |
| Israel | 8,100,000 | 20,770 | Yes | Country only | No | – | Yes | |
| Austria | 8,700,000 | 83,858 | Yes | Both | Yes | 9 | No | |
| Serbia | 8,800,000 | 77,453 | Yes | Country only | Yes | – | Yes | |
| Overall | 4,821,619 | 86,448 | 90% | 48% country only | 62% | 57% | ||
| 5% region only | ||||||||
| 29% country and region | ||||||||
| 10% local | ||||||||
| 9% neither | ||||||||
| 10–20 million | Sweden | 10,000,000 | 449,964 | Yes | Both | Yes | 20 | Yes |
| Belarus | 10,000,000 | 207,600 | Yes | Local | Yes | 1 | Yes | |
| Hungary | 10,000,000 | 93,030 | Yes | Country only | No | – | Yes | |
| Greece | 10,000,000 | 13,194 | No | Local | No | – | Yes | |
| Portugal | 10,460,000 | 91,568 | Yes | Country only | Yes | 6 | Yes | |
| Czech Republic | 10,500,000 | 78,866 | Yes | Country only | No | – | No | |
| Belgium | 11,350,000 | 30,510 | No | Neither | Yes | 3 | Yes | |
| Netherlands | 17,000,000 | 41,198 | Yes | Both | No | – | No | |
| Romania | 19,500,000 | 238,392 | Yes | Local | No | – | Yes | |
| Overall | 12,100,000 | 138,258 | 78% | 33% country only | 44% | 78% | ||
| 22% country and region | ||||||||
| 33% local | ||||||||
| 11% neither | ||||||||
| >20 million | Poland | 38,000,000 | 312,685 | Yes | Country only | Yes | 16 | Yes |
| Ukraine | 42,500,000 | 603,628 | No | Local | Yes | 24 | Yes | |
| Spain | 46,560,000 | 498,468 | Yes | Both | Yes | 17 | Yes | |
| Italy | 60,750,000 | 301,318 | Yes | Region only | Yes | 21 | Yes | |
| United Kingdom | 65,640,000 | 244,820 | Yes | Country only | Yes | 4 | No | |
| France | 66,900,000 | 551,394 | Yes | Both | Yes | 17 | No | |
| Turkey | 78,740,000 | 23,507 | Yes | Both | No | – | – | |
| Germany | 82,670,000 | 357,168 | Yes | Country only | Yes | 300 | Yes | |
| Russia | 146,000,000 | 3,972,400 | Yes | Country only | No | – | No | |
| Overall | 69,800,000 | 762,821 | 89% | 44% country only | 78% | 63% | ||
| 11% region only | ||||||||
| 33% both | ||||||||
| 11% local |
For each population subgroup, overall population and surface express means.
Figure 1.
Distribution of main activity lines of Stroke Care Plans across European countries. Numbers express n of countries including that activity.
The relationship between availability of stroke care plans, their characteristics and the reperfusion treatment rates is shown in Table 2. National stroke registry data were only available in 16 (36.4%) countries. Countries having registry data available showed higher treatment rates per million inhabitants (IVT: 211 vs. 93; EVT: 49 vs. 10). Similarly, countries with a stroke care plan had higher treatment rates (IVT: 140 vs. 30; EVT: 39 vs. 8), which was directly associated with the stroke care plan action level (an increase in treatment rates from local to country level). Moreover, stroke care plans focusing specifically on health care planning, quality improvement, centralised registries and community education activities were associated with higher treatment rates (Table 2). As for the organisation of urgent prehospital stroke care, routine use of non-medicalised ambulances (as compared to medicalised ambulances), and strict orders to transfer acute patients to the nearest centre providing IVT also showed significantly higher rates of both IVT (non-medicalised ambulances: 147 per 100,000 inhabitants-year, p value <0.01; EMS strict transfers: 159 per 100,000 inhabitants-year, p value = 0.001), and EVT (non-medicalised ambulances: 49 per 100,000 inhabitants-year, p value = 0.05, and EMS strict transfers: 48 per 100,000 inhabitants-year, p value= 0.008). Application of a ‘by-pass local stroke centre’ rule according to patient’s baseline features (large vessel occlusion stroke suspicion) showed higher EVT rates (75 per 100,000 inhabitants-year, p value= 0.018).
Table 2.
Association between Stroke Plans features, system of care coverage and reperfusion treatment rates.
| N countries | IVT rate per 106 inhabitants-year, median (IQR) | p value | EVT rate per 106 inhabitants-year, median (IQR) | p value | |
|---|---|---|---|---|---|
| Overall | 42 | 122 (39–211) | 34 (4–71) | ||
| Registry data | 14 | 211 (124–288) | 0.008 | 49 (37–74) | 0.085 |
| No registry data | 28 | 93 (20–176) | 10 (2–64) | ||
| Stroke Plan (active) | 36 | 140 (64–254) | 0.042 | 39 (5–72) | 0.202 |
| No Stroke Plan (active) | 6 | 30 (7–96) | 8 (0–63) | ||
| Stroke Plan level | |||||
| Country level | 31 | 149 (81–266) | 0.008 | 45 (5–74) | 0.021 |
| Region level | 14 | 129 (41–266) | 0.584 | 46 (13–69) | 0.274 |
| Local level | 13 | 39 (11–149) | 0.021 | 6 (4–37) | 0.064 |
| Stroke Plan duties | |||||
| Health planning | 23 | 168 (117–285) | <0.001 | 48 (27–74) | 0.005 |
| Quality assessment | 32 | 154 (93–270) | 0.005 | 49 (5–73) | 0.008 |
| Reimbursement | 15 | 159 (81–243) | 0.194 | 40 (6–71) | 0.243 |
| Organisation | 36 | 140 (49–254) | 0.052 | 42 (5–72) | 0.114 |
| Registries | 21 | 168 (117–288) | 0.001 | 48 (29–74) | 0.027 |
| Community education | 25 | 194 (96–274) | 0.002 | 52 (27–74) | 0.006 |
| Emergency | 33 | 124 (57–199) | 0.444 | 40 (5–71) | 0.108 |
| Cost analysis | 11 | 168 (117–274) | 0.179 | 40 (6–71) | 0.731 |
| Professional education | 27 | 147 (57–266) | 0.281 | 45 (5–75) | 0.083 |
| Stroke system of care coverage | |||||
| Stroke prevention | 17 | 211 (149–288) | <0.001 | 52 (32–74) | 0.005 |
| Emergency admission | 40 | 129 (48–227) | 0.125 | 39 (4–71) | 0.156 |
| Acute hospital care | 43 | – | – | – | |
| Neurorehabilitation | 28 | 140 (64–270) | 0.081 | 30 (5–75) | 0.251 |
| Post-stroke care | 17 | 159 (96–285) | 0.037 | 40 (13–74) | 0.027 |
| Non-medicalised ambulance only | 19 | 147 (96–266) | 0.007 | 49 (27–74) | 0.052 |
| Medicalised ambulance | 23 | 71 (19–134) | 6 (1–63) | ||
| EMS strict transfers | 29 | 159 (91–274) | 0.001 | 48 (7–72) | 0.008 |
| No EMS strict transfers | 13 | 21 (7–121) | 4 (0–37) | ||
| EMS stroke protocol | 28 | 164 (93–270) | 0.004 | 42 (5–71) | 0.268 |
| No EMS protocol | 14 | 36 (11–121) | 6 (2–64) | ||
| ‘By-pass local hospital’ policy | 6 | 267 (117–351) | 0.062 | 75 (45–96) | 0.018 |
| No ‘By-pass local hospital’ policy | 36 | 115 (30–196) | 28 (2–64) |
IQR: interquartile range.
Discussion
This study shows that there is still a considerable proportion of European countries without an appropriate Stroke Strategy or Plan, something that is unfortunately pointing at the low priority that health care decision makers give to stroke in these countries. After two Pan-European Consensus Conferences on Stroke Management, 1995 and 2006,6,7 and despite the very recent European Stroke Action Plan (ESAP),4 there still is a long way to go. Health authorities and decision makers should include stroke in their priority agendas since stroke is the second leading cause of death in European countries, and the most common cause of permanent, non-traumatic disability in adults.8 Turning stroke burden around requires a multifaceted approach that begins with its inclusion in the political agendas. The creation of stroke care plans that operate at national and/or regional level is not enough but a good start. In line with this, availability of valid registry data (currently, only 1/3 of respondents have it) is of utmost importance to keep track of stroke incidence, sociodemographic characteristics, access of residents to evidence-based therapies for acute ischaemic stroke, quality metrics and outcome measurements. Only through high quality registry data, achievements and improvements can be properly monitored. In these regards, it is reassuring that the current study shows significantly higher reperfusion treatment rates in countries with stroke care plans and registry data available. Importantly, this is not to say that there is a cause–effect relationship between stroke care plans and reperfusion treatment rates, something that would need a completely different methodological approach.
It might be expected that large and highly populated countries should have both national stroke strategies and regional stroke care plans where operational aspects of care, including organisation of acute stroke care, are dealt with. However, such association was not seen in this study, something that might be explained by differences in the territorial and political organisation within each country. Most stroke care plans take responsibility for quality of stroke care assessment and organisation of Code Stroke systems with involvement of EMS. Such systems were initially developed during the thrombolytic era to get over the therapeutic nihilism, and to achieve that as many acute ischaemic stroke patients as possible were eventually treated. More recently, demonstration of the efficacy of mechanical thrombectomy is prompting systems of care to adapt to the new reality and streamline the process of care even more. Not only quick on-scene recognition of suspected strokes is necessary but also in-hospital processes must be sped up to shorten the door-in door-out time that allows handover between hospitals. Thus, in most countries, the focus is clearly on acute stroke care, and the post-acute care and rehabilitation phase are aspects of care often not included. Though perhaps satisfactory for stroke and emergency physicians, organising stroke systems of care from that perspective only is insufficient. In that sense, the ESAP includes targets for a series of domains in stroke care: organisation of stroke services, management of acute stroke, prevention, rehabilitation, evaluation of stroke outcome and quality assessment. ESAP also includes two additional domains, on primary prevention and life after stroke, along with research and development priorities for translational stroke research.9
The major limitation of this study is that it relied on self-reported surveyed data. Even though stroke national (or regional, if relevant) contacts were asked to provide only best available information to compile the survey, in countries lacking stroke registries multiple sources of regional and local information were used to extrapolate national figures and, therefore, the information returned might not be that precise. In addition, no audit could be performed to assess the quality of the data. Another limitation of this study is that we surveyed and performed the analyses at the country level. Efforts were made to take into consideration the regions perspectives in countries where regions play an important role in health policy making or where health budged is devolved. However, national survey coordinators were asked to aggregate regions’ responses at the national level. Thus, this study does not properly reflect the situation of those regions with a distinctive stroke care plan that are embedded in large countries with huge variation across regions. Another aspect that should be born in mind is the restricted number of outcome variables included (i.e. number of IVT and EVT/country/year, which were worked out to produce population treatment rates), which are insufficient to assess the impact and quality of Stroke Plans and prehospital stroke care. In this context, it would be especially important to link respective treatment rates with actual patient outcomes as the ultimate goal of all our efforts. Nevertheless, the study is relevant because it encompasses a thorough pan-European perspective that serves to identify organisational shortcomings in a number of countries: most importantly, absence of priority for stroke in some health systems that translates into poor planning and organisation of stroke systems of care, poor community education, lack of registry data and eventually a hindered access to evidence-based therapies. In this respect ‘organisation is also curative’, particularly in diseases where time counts, that is, which require quick and smooth transitions between care levels, and cooperation of relevant professionals from different fields as is the case with stroke.
Acknowledgement
The authors are grateful to all ‘ESO/ESMINT/EAN/SAFE Survey on Stroke Care in Europe’ collaborators. We are also in debt to Bo Norrving, Didier Leys, Kennedy Lees and Turgut Tatlisumak for their useful comments regarding the questionnaire, data collection methodology and policy implications of this paper.
Appendix 1
‘ESO/ESMINT/EAN/SAFE Survey on Stroke Care in Europe’ collaborators
M Petrela, O Taka, E Enesi (Albania); S Kiechl, M Brainin, F Fazekas (Austria); P Konovalov (Belarus); A Peeters, G Vanhooren, L Defreyne (Belgium); H Haris, M Moranjkic (Bosnia and Herzegovina); S Andonova, I Staikov (Bulgaria); H Budincevic, D Ozretic, B Malojčić (Croatia); A Tomek (Czech Republic); H Iversen, SP Jonhsen (Denmark); J Korv, R Vibo, V Malikov (Estonia); T Sairanen, D Strbian, K Lappalainen (Finland); S Timsit, E Touze, D Leys (France); A Tsiskaridze, I Burduladze (Georgia); M Dichgans, J Röther, J Fiehler (Germany); G Tsivgoulis, E Brountzos (Greece); D Bereczki. C Óváry, I Szikora (Hungary); B Thorarinsson, V Vilmarsson (Iceland); J Harbison (Ireland); N Bornstein, D Tanne, A Horev (Israel); D Toni, S Mangiafico, V Caso (Italy); A Murzaliev, I Lutsenko, A Artykbaev, (Kyrgyzstan); E Miglãne, K Kupcs, I Kikule (Latvia); D Jatuzis, D Rastenyte, M Kurminas (Lithuania); D Ulbricht (Luxembourg); A Arsovska, M Smiceska, E Lickova (The former Yugoslav Republic of Macedonia); M Mallia, R Grech, M Schembri (Malta); V Lisnic, E Manole, E Zota (Moldova); M Cukic (Montenegro); D Dippel, C Majoie, H B van der Worp (Netherlands); S Akpinar (Northern Cyprus); E Berge, Hanne Ellekjær (Norway); A Czlonkowska, W Poncyljusz, A Kobayashi (Poland); E Azevedo, V Tedim-Cruz, M Ribeiro (Portugal); C Tiu (Romania); T Kharitonova (Russia); L Bumbasirevic (Serbia); Z Gdovinova, I Vulev, P Turcani (Slovakia); B Zvan, V Svigelj, Z Milosevic (Slovenia); J Gállego, M Rodríguez Yáñez, E Palacio-Portilla, A Gonzallez Mandly, M Gallofré, S Abilleira, C Gimenez, S Calleja-Puerta, J Marta-Moreno, M Óscar Ayo, A Lago (Spain); M Arnold (Switzerland); M Mazya, T Moreira (Sweden); N Uzuner, L Gungor, O Ozdemir (Turkey); H Rodgers, J Dawson, P White (United Kingdom); Y Flomin, D Shcheglov (Ukraine).
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: SA is co-PI of the RACECAT trial. VC received grants and speaker fees from BI. UF is consultant for Stryker, Medtronic and CSL Behring; Research grant from the Swiss National Science Foundation, Swiss Heart Foundation and Medtronic. DAS, TG, FF, AK, IZ, MG and VF have no disclosures.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
Not required.
Informed consent
Not required.
Guarantor
Urs Fisher.
Contributorship
SA contributed to the concept or design of the work and drafted the article. DAS and UF: contributed to data acquisition, interpretation of data, and revised the article. TG, AK, FF, IZ, VC, MG and VF: critically revised the article for intellectual content and approved the version to be published. Each author has participated sufficiently in the work to take public responsibility for appropriate portions of the content.
References
- 1.Olofsson J, Padyab M, Malmberg G. Health disparities in Europe’s ageing population: the role of social network. Glob Health Action 2018; 11: 1445498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. The Lancet 2018; 392: 1072–1088. [DOI] [PubMed]
- 3.The Burden of Stroke in Europe. London, http://www.strokeeurope.eu/downloads/The_Burden_of_Stroke_in_Europe_Report_-_Appendix.pdf (accessed 5 March, 2019).
- 4.Norrving B, Barrick J, Davalos A, et al. Action plan for stroke in Europe 2018–2030. Eur Stroke J 2018; 3: 309–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aguiar de Sousa D, von Martial R, Abilleira S, et al. on behalf of the ESO ESMINT EAN SAFE Survey on Stroke Care Collaborators. Access to and delivery of acute ischaemic stroke treatments: a survey of national scientific societies and stroke experts in 44 European countries. Eur Stroke J 2018; 3: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aboderin I, Venables G. Stroke management in Europe. Pan European Consensus Meeting on stroke management. J Intern Med 1996; 240: 173–180. [DOI] [PubMed] [Google Scholar]
- 7.Kjellstrom T, Norrving B, Shatchkute A. Helsingborg Declaration 2006 on European stroke strategies. Cerebrovasc Dis 2007; 23: 231–241. [DOI] [PubMed] [Google Scholar]
- 8.Townsend N, Wilson L, Bhatnagar P, et al. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J 2016; 37: 3232–3245. [DOI] [PubMed] [Google Scholar]
- 9.Fischer U, Aguiar de Sousa D, Norrving B, et al. Status and perspectives of acute stroke care in Europe. Stroke 2018; 49: 2281–2282. [DOI] [PubMed] [Google Scholar]