Abstract
Objective
To define patient demographics, preoperative, and intraoperative surgical variables associated with successful or failed repair of bucket-handle meniscal tears.
Design
All patients who underwent arthroscopic repair of a bucket-handle meniscus tear at a single institution between May 2011 and July 2016 with minimum 6-month follow-up were retrospectively identified. Patient demographic, preoperative (including imaging), and operative variables were collected and evaluated. A Kaplan-Meier curve was generated to demonstrate meniscus repair survivorship.
Results
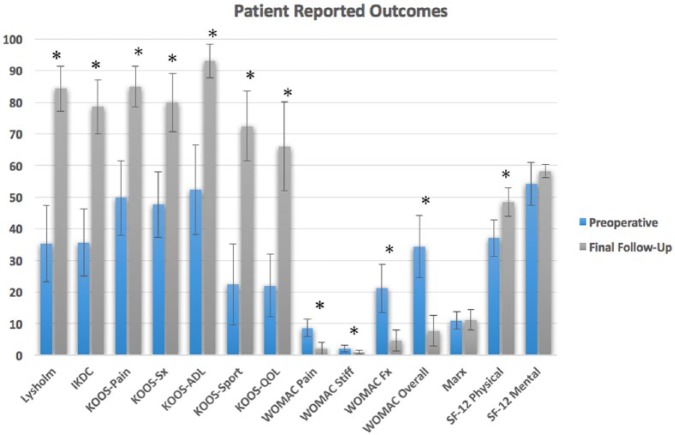
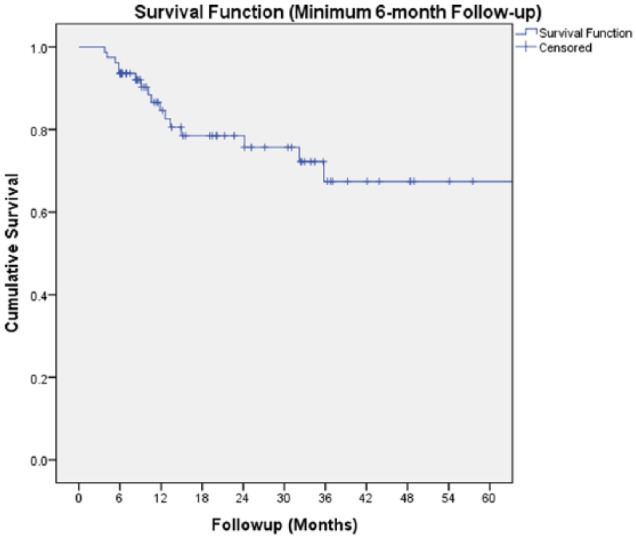
In total, 75 patients (78 knees) with an average age of 26.53 ± 10.67 years met inclusion criteria. The average follow-up was 23.41 ± 16.43 months. Fifteen knees (19.2%) suffered re-tear of the repaired meniscus at an average 12.24 ± 9.50 months postoperatively. Survival analysis demonstrated 93.6% survival at 6 months, 84.6% survival at 1 year, 78.4% survival at 2 years, and 69.9% survival at 3 years. There was significant improvement from baseline to time of final follow-up in all patient-reported outcome (P < 0.05) except Marx score (P = 0.933) and SF-12 Mental Subscale (P = 0.807). The absence of other knee pathology (including ligament tear, contralateral compartment meniscal tear, or cartilage lesions) noted intraoperatively was the only variable significantly associated with repair failure (P = 0.024). Concurrent anterior cruciate ligament reconstruction (vs. no concurrent anterior cruciate ligament reconstruction) trended toward significance (P = 0.059) as a factor associated with successful repair.
Conclusions
With the exception of the absence of other knee pathology (including ligament tear, contralateral compartment meniscal tear, or cartilage lesions) noted intraoperatively, no other variables were significantly associated with re-tear. The results are relatively durable with 84.6% survival at 1 year. Surgeons should attempt meniscal repair when presented with a bucket-handle tear.
Keywords: meniscus, tear, bucket-handle, repair
Introduction
Preservation of meniscal tissues is imperative to maintaining proper biomechanical function within the knee. The menisci are important for knee joint load transmission, stabilization, lubrication, and shock absorption; this explains why partial or total meniscectomy has been demonstrated to contribute to the progression of osteoarthritis.1,2 Thus, meniscal repair is preferable to debridement when injury requires surgical intervention, although the potential to heal after reparative surgery is not always definitive and outcomes are not always absolute.3 Factors found to significantly influence success rates with meniscal repair include anterior cruciate ligament (ACL) concomitant reconstruction, tear length, chronicity of the tear, and meniscus laterality.4
Bucket-handle meniscal tears represent 10% to 26% of all meniscus tears and define a subgroup of meniscal injury involving a vertical or oblique longitudinal tear with an attached fragment displaced away from the periphery of the meniscus.5,6 These tears can begin at the posterior meniscal insertion onto the tibia and propagate anteriorly past the anterior-middle third junction. Displacement of the inner segment into the intercondylar notch can additionally occur7 and can lead to mechanical symptoms, locking, pain, and perceived instability. Proper repair of this type of tear is particularly important, as failure can lead to total or subtotal loss of meniscal function.4 Successful repair is important to preserve joint kinematics and prevent progressive osteoarthritis in a typically young, athletic patient population.8
Few case reports or clinical studies with limited cohort sizes of repair of bucket-handle meniscus tears exist in the literature, and limited studies clearly define the patient demographics and compare preoperative or intraoperative surgical variables in those with successful repair or failed repair.4,9-14 The purpose of this study was to evaluate a single academic institution’s cohort of patients with bucket-handle meniscus tears who underwent arthroscopic repair. Specifically, we sought to (1) report patient demographic information for those who sustained bucket-handle meniscus tears; (2) evaluate patient clinical outcomes, return to sport, complications, and reoperation/revision rates after arthroscopic repair of bucket-handle meniscus tears; and (3) to compare the subgroups of patients with successful outcomes to those with failure after repair in order to identify any correlative patient-related, surgical technique-related, or pathology-related factors. Our hypotheses were that overall good patient outcomes could be obtained with repair of bucket-handle meniscus tears, and identifiable variables could be isolated that correlate with higher likelihood of failure after repair.
Methods
Following institutional review board approval (#16082001), all patients who underwent arthroscopic repair of a bucket-handle meniscus tear at a single academic institution (4 attending surgeons) between May 2011 and July 2016 with a minimum 6-month clinical follow-up were retrospectively identified from a database of prospectively collected data. The following demographic and preoperative data were recorded: patient gender; age at surgery; body mass index (BMI); affected knee laterality; affected meniscus laterality; smoking status; Worker’s Compensation status; duration of symptoms prior to surgery; sports participation; highest activity level (recreational, competitive [middle or high school], elite [college or professional]); and prior index knee surgery (including meniscal surgery, anterior cruciate ligament reconstruction [ACLR]). Plain radiographs were assessed for Kellgren-Lawrence grade and/or joint space narrowing, and patient injury. Magnetic resonance imaging (MRI) scans were evaluated for subchondral edema in the affected compartment and/or a double posterior cruciate ligament (PCL) sign. Two authors (EJC, KCW) reviewed all imaging independently. The following intraoperative characteristics were documented: tear size and the amount of remaining peripheral meniscal tissue (retrospectively evaluated from arthroscopic images by 2 senior attending physicians [ABY, NNV]); tear location; repair technique (all-inside, inside-out); number of sutures used in repair; performance of microfracture for meniscal healing; presence of concomitant intra-articular pathology including ligament tear, contralateral compartment meniscal tear, or cartilage lesions; concomitant surgery (ACLR, cartilage restoration). Postoperative complications, occurrence (and timing) of meniscus re-tear, occurrence (and timing) of reoperation, patient satisfaction (numeric scale, 1-10 with 10 being completely satisfied) with surgery, visual analog scale (VAS) pain (numeric scale, 0-10), return to sport (RTS; including level of sport), and whether the patient would have the procedure performed again (yes/no).
Patient-reported outcome (PROs) measures were obtained preoperatively, at a minimum 6 months postoperative, and final follow-up postoperatively. These included Lysholm, International Knee Documentation Committee (IKDC), Knee Injury and Osteoarthritis Outcome (KOOS) and 5 subgroups (Pain, Symptoms, Activities of Daily Living [ADL], Quality of Life [QOL], and Sport), Marx rating scale, Short Form (SF)-12 Physical and Mental Component Scores, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) overall and 3 subgroups (Pain, Stiffness, Function).
Patients were subgrouped for comparison into 2 cohorts based on whether or not they sustained a re-tear of the index meniscus, which is how we defined failure for the purposes of this investigation. The aforementioned variables were compared between these 2 cohorts in order to identify significant differences in preoperative or intraoperative characteristics.
Authors’ Preferred Surgical Technique and Patient Rehabilitation
While there may be slight variations in surgical technique between the 4 senior surgeons (NNV, BF, ABY, and BJC) who performed surgeries in this cohort, generally, the technique for bucket-handle meniscus repair with and without ACLR is as follows. In brief, the patient was positioned supine and an examination under anesthesia was performed to evaluate for ligamentous pathology, namely, confirmation of an ACL tear. The surgical limb was then placed in a modified ACL position with care to pad all bony prominences. Following induction of general anesthesia, tourniquet placement, and a time-out, standard medial and lateral transpetellar portals were made and a diagnostic arthroscopy was performed to confirm a bucket-handle meniscus tear, possible ACL tear, and any other concomitant pathology. Once confirmed that the bucket-handle meniscal tear was amenable to repair, the meniscal-capsular junction was freshened up using a shaver. For medial meniscal tears repaired through an inside-out technique, a posteromedial incision was made and carried down sharply to the underlying Sartorius. Dissection was performed between the gastrocnemius and the capsule with a Henning retractor placed. For lateral meniscal tears, an inside-out approach was performed through a 3-cm incision along the lateral aspect of the knee through the window of the biceps femoris and the iliotibial band. Using a guide, inside-out sutures were placed from the anterior margin of the tear on both the superior and inferior surface, moving posteriorly. All inside techniques do not necessitate additional incisions and were performed using Fast-Fix implants (Smith & Nephew, Andover, MD) to achieve stability of the previously torn meniscus. Once the extent of the tear was successfully reduced and deemed stable on probing, attention was then turned to ACLR if applicable. The knee was copiously irrigated and closed in standard layered fashion.
For patients undergoing isolated meniscus repair, they are partial weight bearing with crutches for the first 2 weeks postoperatively, advancing to full weight bearing beginning at 4 weeks. Patients are placed in a hinged knee braced locking full extension for the first 2 weeks taken off only for range of motion exercises. It is highly recommended patients do not weight bear with flexion beyond 90° of flexion until 8 weeks. Progression to achieve full range of motion and strengthening exercises with advancement to sport-specific activities including running and jumping is discouraged until 20 weeks. For patients undergoing concomitant ACLR, they are kept in the knee brace until 4 weeks, partial weight bearing 4 to 8 weeks, and advanced to full weight bearing at 8 weeks. Return to sport-specific activities typically occurs after 6 months once full, pain-free range of motion is achieved and the surrounding muscle strength is returned.
Statistical Analysis
Descriptive statistics were calculated for all variables, including frequencies and mean values. Chi-square and Fisher’s exact tests were used to compare categorical variables. Binomial logistic regression analysis was used to evaluate continuous variables association with odds of failing index bucket-handle meniscus repair. Postoperative PROs were unable to be obtained in the majority of patients (N = 40), and thus only the preoperative PROS (N = 58) were utilized for the purposes of the binomial regression to assess whether these scores were predictive of re-tear. A Kaplan-Meier curve was generated to demonstrate meniscus repair survivorship. A Wilcoxon signed rank test was used to compare preoperative PROs with those of final follow-up. All reported P values are 2-tailed, with an α level of 0.05 detecting significant differences (SPSS Statistics, Version 23.0, IBM, Armonk, New York).
Results
A total of 99 patients underwent bucket-handle meniscus repairs at our institution between May 2011 and July 2016. Of these patients, 75 patients (78 knees, 78.8%) met inclusion criteria with a minimum 6-month follow-up (or failure a time point prior to 6 months postoperative).
Patient Demographics and Preoperative Variables
The mean age for all included patients was 26.53 ± 10.67 years (range = 12.97-49.41 years). Most knees were in male patients (62.8%), and the average BMI was 25.52 ± 5.31 kg/m2. The average time to final follow-up was 23.41 ± 16.43 months. The mean duration of symptoms prior to surgical intervention was 10.01 ± 24.51 months (range = 0.25-155.72 months). Fifty (64.1%) of the meniscus tears occurred on the medial meniscus, and 46 (59.0%) tears occurred in the right knee. The majority of patients were nonsmokers (94.87%) and non-Workman’s Compensation claims (96.16%), self-reported as an athlete (96.1% of knees), had no osteoarthritis (75.7% of knees with KL grade 0), and lacked a “double PCL sign” on MRI (58.7%) preoperatively. Most tears (46.2%) extended from the posterior horn to the body of the meniscus. A complete description of all patient demographic and preoperative variables are reported in Table 1 .
Table 1.
Demographic and Preoperative Variables.
| Variable | Number, SD (%) |
|---|---|
| Time to follow-up in months (range) | 23.41 ± 16.43 (5.49-65.71) |
| Age (range) | 26.53 ± 10.67 (12.97-49.41) |
| Body mass index | 25.52 ± 5.31 |
| Gender (male, female) | 49 (62.8%), 29 (37.2%) |
| Smoking | 4 (5.13%) |
| Workman’s compensation | 3 (3.84%) |
| Knee laterality (right, left) | 46 (59.0%), 32 (41.0%) |
| Meniscus laterality (right, left) | 50 (64.1%), 28 (36.0%) |
| Athlete | 75 (96.1%) |
| Level of athlete | |
| Recreational | 46 (59.0%) |
| Competitive (high school or travel club) | 20 (25.5%) |
| Elite (college or professional) | 9 (11.5%) |
| Previous meniscus surgery | 8 (10.2%) |
| Previous ACL reconstruction | 8 (10.2%) |
| Duration of symptoms in months (range) | 10.1 ± 24.51 (0.25-155.76) |
| Kellgren-Lawrence grade on preoperative radiographsa | |
| 0 | 53 (75.7%) |
| 1 | 12 (15.4%) |
| 2 | 4 (5.1%) |
| 3 | 0 (0%) |
| Subchondral edema on preoperative MRIa | 39 (52%) |
| Double PCL sign on MRIa | 31 (41.3%) |
| Tear location | |
| Posterior horn | 30 (38.5%) |
| Posterior horn to body | 36 (46.2%) |
| Anterior horn to body | 2 (2.3%) |
| Anterior horn | 1 (1.3%) |
| Mid-body only | 8 (10.2%) |
ACL = anterior cruciate ligament; MRI = magnetic resonance imaging; PCL = posterior cruciate ligament.
Not all patients had preoperative imaging available in our database for review; 9 knees did not have preoperative radiographs for review, 3 of those knees did not have MRI. The denominator for plain radiographs was 69 and for MRI 75 knees.
Patient Intraoperative Characteristics
There was an even breakdown of all-inside (50%) versus inside-out (50%) repair techniques performed, with a mean 5.12 ± 3.0 sutures used in the repair. The mean remaining meniscus tissue peripheral to the tear location was 4.88 ± 1.84 mm. Most knees (61.5%) underwent concomitant procedures, particularly ACLR (55.1%). Microfracture was performed concomitantly to stimulate healing in 21 knees (26.9%). A complete description of all patient intraoperative characteristics can be found in Table 2 .
Table 2.
Descriptive Statistics of Intraoperative Variables for the Entire Cohorta.
| Variable | Number, SD (%) |
|---|---|
| Repair technique | |
| All-inside | 39 (50%) |
| Inside-out | 39 (50%) |
| Tear size (%) | 45.52 ± 17.97% |
| Amount of peripheral tissue remaining (mm) | 4.88 ± 1.84 |
| Microfracture to aid in meniscal healing | 21 (26.9%) |
| Number of sutures used in repair (range) | 5.12 ± 3.0 (1-15) |
| Other pathology present at time of index repair | 55 (70.5%) |
| Concomitant procedure performed | 48 (61.5%) |
| Concomitant anterior cruciate ligament reconstruction | 43 (55.1%) |
| Cartilage procedure (debridement, microfracture, graft) | 6 (7.7%) |
All listed numbers, means, and percentages are based off of the total number of knees.
Postoperative Outcomes
Seven knees (9.0%) experienced complications: 1 deep venous thrombosis which was treated with oral anticoagulation; 1 lateral sleeve patella avulsion (in a patient with concurrent ACLR via bone-patellar tendon-bone autograft); 2 with persistent stiffness and limited range of motion; 1 suture which breached the skin and had to be removed; 1 wound dehiscence resulting in prophylactic antibiotic treatment but no irrigation and debridement. This patient had a re-tear 5.85 months after index repair with concomitant ACLR; and one with a persistent anterior clicking sensation. A total of 15 knees (19.2%) suffered re-tear of the repaired meniscus at an average 12.24 ± 9.50 months postoperative. Survival analysis using a Kaplan-Meier curve ( Fig. 1 ) demonstrates 93.6% survival at 6 months, 84.6% survival at 1 year, 78.4% survival at 2 years, and 69.9% survival at 3 years. In our sample, there was a steady rate of failure up to 15-month follow-up. After 15 months, there was a reduced risk of failure in the remaining repairs.
Figure 1.
A Kaplan-Meier survival curve for the overall patient cohort at an average 23.41 ± 16.43 months (range = 5.49-65.71 months) follow-up. Survival analysis demonstrated 93.6% survival at 6 months, 84.6% survival at 1 year, 78.4% survival at 2 years, and 69.9% survival at 3 years.
In total, 18 knees (23.1%) underwent a subsequent operation on the ipsilateral knee, of which 4 were unrelated to the intact status of the index meniscal repair (one case each of manipulation under anesthesia, posterior capsule release and lysis of adhesions, patellar tendon repair for acute rupture, and distal femoral plating for developmental genu varus). Of the 15 patients who developed a re-tear, 14 (93.3%) underwent subsequent partial meniscectomy with no revision meniscal repair attempt. The final re-tear patient is currently scheduled to undergo repeat operative intervention and thus the individual’s treatment is not yet available to be included in this analysis.
Of the 44 patients who were reached to ask if they would choose to undergo the procedure again, 41 (93.2%) stated they would, including 6 patients who failed index repair. Furthermore, the average overall patient satisfaction score was 8.73 ± 2.31 out of 10 at time of final follow-up. The average overall preoperative VAS score was 6.50 ± 2.14 out of 10, and postoperatively it significantly improved to a mean 1.053 ± 1.43 out of 10 (P < 0.001). Furthermore, there was a significant improvement from baseline to time of final follow-up in all PROs (P < 0.05) except Marx score (P = 0.933) and SF-12 Mental Subscale (P = 0.807) ( Fig. 2 ).
Figure 2.
A graph demonstrating the mean preoperative patient reported outcome scores compared with the same metrics at time of final follow-up.
*Denotes statistical significance at P < 0.05. Abbreviations: IKDC = International Knee Documentation Committee; KOOS = Knee Injury and Osteoarthritis Outcome; Sx = symptoms; ADL = activities of daily living; QOL = quality of life; SF-12 = Short Form-12; WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
Subgroup Comparison: Patients with Re-tear versus No Re-tear
Patient demographic, preoperative, and intraoperative categorical ( Table 3 ) and continuous ( Table 4 ) variables were evaluated for any significant relationships between those individuals who failed index bucket-handle meniscus repair and those who did not. Only the presence of other pathology (including ligament tear, contralateral compartment meniscal tear, or cartilage lesions) in the knee noted intraoperatively was associated with successful repair. Notably, there was no association based on such variables as smoking status, meniscus laterality, tear location/size or remaining meniscus peripheral to tear, repair technique (or suture number), concomitant ACLR, or preoperative PROs.
Table 3.
Chi Square or Fisher’s Exact Test Analysis of demographic, Preoperative Imaging and Operative, and Immediate Postoperative Categorical Variables Associated with Failed Bucket-Handle Meniscus Repair.
| Variable | Failure (n) | No Failure (n) | P Value |
|---|---|---|---|
| Smoking | 0.999 | ||
| Yes | 0 | 4 | |
| No | 15 | 59 | |
| Workman’s compensation | 0.478 | ||
| Yes | 1 | 2 | |
| No | 14 | 61 | |
| Gender | 0.801 | ||
| Male | 9 | 40 | |
| Female | 6 | 23 | |
| Knee laterality | 0.570 | ||
| Right | 10 | 36 | |
| Left | 5 | 27 | |
| Meniscus laterality | 0.999 | ||
| Medial | 10 | 40 | |
| Lateral | 5 | 23 | |
| Athlete | 0.478 | ||
| Yes | 14 | 61 | |
| No | 1 | 2 | |
| Previous meniscus surgery | 0.646 | ||
| Yes | 2 | 6 | |
| No | 13 | 57 | |
| Previous ACL reconstruction | 0.342 | ||
| Yes | 0 | 8 | |
| No | 15 | 55 | |
| Kellgren-Lawrence grade on X-raya | 0.541 | ||
| 0 | 10 | 43 | |
| 1 | 4 | 8 | |
| 2 | 1 | 3 | |
| 3 | 0 | 0 | |
| Subchondral edema on MRIa | 0.390 | ||
| Yes | 6 | 33 | |
| No | 9 | 27 | |
| Double PCL sign on MRIa | 0.291 | ||
| Yes | 8 | 23 | |
| No | 7 | 37 | |
| Tear location | 0.886 | ||
| Posterior horn | 6 | 24 | |
| Posterior horn to body | 8 | 28 | |
| Anterior horn to body | 0 | 2 | |
| Anterior horn | 0 | 1 | |
| Mid-body only | 1 | 7 | |
| Repair technique | 0.999 | ||
| All-inside | 8 | 31 | |
| Inside-out | 7 | 32 | |
| MFX to stimulate healing | 0.532 | ||
| Yes | 5 | 16 | |
| No | 10 | 47 | |
| Other pathology in knee | 0.024 | ||
| Yes | 7 | 48 | |
| No | 8 | 15 | |
| Concomitant procedure (other than MFX for healing) | 0.074 | ||
| Yes | 6 | 41 | |
| No | 9 | 22 | |
| Concomitant ACL reconstruction | 0.059 | ||
| Yes | 5 | 38 | |
| No | 10 | 25 | |
| Complications | 0.614 | ||
| Yes | 2 | 5 | |
| No | 13 | 58 |
ACL = anterior cruciate ligament; MRI = magnetic resonance imaging; PCL = posterior cruciate ligament; MFX = microfracture.
Not all patients had preoperative imaging within our imaging storage system that could be independently reviewed.
Table 4.
Binomial Logistic Regression Analysis for Demographic, Preoperative, and Operative Continuous Variables Associated with Failure of Bucket-Handle Meniscus Repair.
| Variable | Odds Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| Age | 0.953 | 0.889-1.022 | 0.175 |
| BMI | 0.909 | 0.776-1.066 | 0.24 |
| Symptom duration (months) | 1.018 | 0.675-1.537 | 0.931 |
| Tear size | 1.051 | 0.985-1.121 | 0.131 |
| Peripheral meniscus remaining | 1.103 | 0.607-2.005 | 0.747 |
| Number of sutures | 1.055 | 0.875-1.271 | 0.576 |
| Preoperative VAS pain | 1 | 0.752-1.329 | 0.999 |
| Lysholm score | 1.011 | 0.965-1.061 | 0.639 |
| IKDC score | 0.96 | 0.761-1.212 | 0.734 |
| KOOS–Pain | 0.83 | 0.615-1.118 | 0.22 |
| KOOS–Symptoms | 1.092 | 0.943-1.264 | 0.241 |
| KOOS–ADL | 1.105 | 0.884-1.381 | 0.382 |
| KOOS–Sport | 1.042 | 0.886-1.227 | 0.617 |
| KOOS–QOL | 1.027 | 0.930-1.135 | 0.594 |
| MARX | 0.848 | 0.607-1.183 | 0.332 |
| SF-12 Mental | 1.088 | 0.946-1.250 | 0.236 |
| SF-12 Physical | 1.116 | 0.989-1.259 | 0.075 |
BMI = body mass index; VAS = Visual Analog Scale; IKDC = International Knee Documentation Committee; KOOS = Knee Injury and Osteoarthritis Outcome Score; ADL = activities of daily living; QOL = quality of life; SF = Short Form.
Discussion
The results of the current study suggest that few complications occur after arthroscopic repair of bucket-handle meniscus tears, and the results are relatively durable with 84.6% survival at 1 year, 78.4% survival at 2 years, and 69.9% survival at 3 years. Patients who did fail index repair (as defined by symptomatic re-tear) did so at a mean 12.24 ± 9.50 months postoperative. Notably, there was no association for failure or nonfailure cases based on variables such as smoking status, meniscus laterality, tear location/size or remaining meniscus peripheral to tear, repair technique (or suture number), concomitant ACLR, notch microfracture, or preoperative PROs. In the absence of specific factors associated with failure of repair that we could delineate—and given the young, athletic population that is affected by this injury pattern—surgeons should attempt meniscal repair at the index surgery when presented with a bucket-handle tear.
While there are several techniques for repairing a meniscal tear—inside-out, outside-in, and all-inside—the classic inside-out technique remains for many surgeons the “gold standard” for bucket-handle tears by which other methods are compared to.15 All-inside repair is gaining popularity for smaller tears requiring fewer sutures, and outside-in repair is preferred specifically for anterior horn tears.16 Inside-out repair methods are widely considered the treatment of choice for complex tears, middle one-third meniscal tears, or tears requiring >3 to 4 sutures (for reasons of cost comparisons).4,17 The benefits of all-inside repair devices include a less invasive means with quicker procedure time, lower morbidity and complications; however, concerns exist with its high cost, and questions in the literature of its biomechanical integrity in comparison with inside-out repair.18-20 Solheim et al.21 reported on 82 patients at a median 10 years postoperative with all-inside repair of bucket-handle meniscus tears, and demonstrated a failure rate (defined as a repeat surgical procedure in the same knee and same meniscus as the index meniscal repair procedure) of 48%; the authors suggested that all-inside repair devices were thus associated with poor long-term results and a high failure rate. Our results challenge this finding, as through comparison of failure and nonfailure cases we report no difference in suture number or surgical technique. We propose that surgeons should perform their meniscal repair with a surgical technique (all-inside or inside-out) that they are most comfortable utilizing as our data do not suggest superiority of either in providing successful results. This aligns more closely with the findings and recommendations gleaned by Albrecht-Olsen et al.9 who randomized 68 patients with bucket-handle meniscus tears to repair with either arrow (all-inside) or inside-out techniques. At second-look arthroscopy 3 to 4 months postoperative, they reported no differences between the 2 techniques in terms of healing. While arrow (all-inside) devices are falling out of clinical relevance in favor of newer, more durable all-inside devices, a recent systematic review of 27 studies comparing failure rates, functional outcomes, and complications between modern all-inside meniscus repairs with inside-out repairs17 reported no difference in clinical failure or anatomic failure between techniques. Although this review was not conducted exclusively in cohorts with bucket-handle meniscus tears, their results corroborate the findings of the current study.
Shelbourne and Johnson22 have previously promoted a 2-stage procedure for those patients with displaced bucket-handle meniscus tears and ACL rupture in order to reduce the formation of arthrofibrosis. O’Shea and Shelbourne13 reported a success rate of 89% in their 59 patients who underwent staged procedures of bucket-handle meniscus tear repair and ACLR (at repeat arthroscopic surgery a mean 77 days later). Other authors have more recently felt that providing ligamentous stability at the time of meniscal intervention is important to the biomechanical integrity of the repair site and may provide an additional healing milieu within the knee joint.23 For instance, Espejo-Reina et al.24 reported complete healing in 83% of their cohort of 24 patients at a mean 48 months postoperative (range = 24-112 months) with repair of chronic bucket-handle medial meniscal tears (date of injury >2 months prior to intervention; mean 10 months), with a 21-fold greater risk of failure in patients who did not undergo concurrent ACLR. Reasons for this may include the greater release of factors (marrow elements from drill holes) that promote healing, and a slower rehabilitation that may protect the meniscal repair site.25,26 Our data suggested that concomitant ACLR (P = 0.059) and concurrent procedures (ligament reconstruction, cartilage restoration, repair/debridement of the other meniscus) trended toward significance as associated variables with successful (vs. failed) repair; with increased patient numbers it is possible that we would have added power to demonstrate statistical significance. When combining the presence of other injury in the knee as “other pathology” (including ligament tear, contralateral compartment meniscal tear, cartilage lesions) noted at the time of bucket-handle repair, we found this overall variable to be significantly associated (P = 0.024) with successful repair. This suggests that even the presence of unaddressed or untreated pathology in the knee at the time of surgery may be stimulating the intra-articular reparative environment.
Arthroscopic repair of meniscal tears extending within the avascular central third of the meniscus or beyond 4 mm form the meniscosynovial junction have demonstrated failure rates of 25% to 100%, respectively.25,27 The outer 25% to 30% of meniscal tissue (or within 3-4 mm of the capsule) represents the “red-red” zone of the meniscus, where healing rates and reparability are higher due to more robust blood supply.16,28 However, in some patients, the vascularized portion of the meniscus may extend beyond the conventionally reference peripheral one-third of tissue:3 the mean tear distance from the meniscosynovial junction in our patient cohort was 4.88 mm, and repair was successful in >80% of our overall cohort. Furthermore, there were no associations between amount of peripheral tissue remaining and success or failure in outcome. These findings further challenge the prior teaching that meniscal tears outside of the outer 3 to 4 mm are less apt to heal after repair. Moreover, meniscectomy in these patients is not a benign option; Pengas et al.29 demonstrated at 40-year follow-up a 4-fold increased risk of radiographic arthritis in 30 patients—all of whom were symptomatic at follow-up—treated previously with total meniscectomy for meniscal pathology.
Kaplan-Meier survival analysis projected only 69.9% survival at 3 years postoperative. However, most patients—including those with subsequent surgical intervention for repeat index meniscus tear—still stated that they would undergo the procedure again at time zero if given the opportunity again. Significant improvements in VAS pain, Lysholm, IKDC, KOOS subscores, WOMAC subscores and overall, SF-12 physical component, and high patient satisfaction scores were additionally demonstrated. Given that the salvage procedure (partial meniscectomy) is relatively simple, with low patient morbidity,30 and does not appear to be affected by a prior repair attempt, an attempt to maintain meniscal tissue through repair efforts at the index procedure is valid and appropriate. Kaplan-Meier survival analysis also suggests that there is a steady rate of failure up to 15-month follow-up; following 15 months, there was a reduced risk of failure in the remaining repairs. Future studies evaluating bucket-handle meniscus tears should thus consider this time point as a minimum follow-up for which to capture as many failures as possible that occur.
For comparison, other publications have reported even greater success in outcomes: Yilmaz et al.31 noted complete meniscal healing in all but one of 52 patients (mean age = 28.4 years) who underwent a combined inside-out and all-inside technique for repair of bucket-handle meniscus tears at a mean 31.3-month follow-up. Ahn et al.32 retrospectively evaluated 13 patients with a median age of 20 years at a median 4.0 years follow-up after modified all-inside or combination all-inside/outside-in repair of lateral meniscus bucket-handle tears. The authors reported no reoperations during the follow-up period, no recurrence of mechanical locking symptoms, and significant improvements in Lysholm, HSS score, and Tegner activity levels. Feng et al.4 evaluated a series of 64 second-look cases with 67 repairs. They reported an overall meniscal healing rate of 89.6%, including 82.1% completely healed and 7.5% incompletely healed. At an average 26-month follow-up, the failure rate comprising recurrent locking or catching was 10.4% (7 of 67 repairs), including 4 failures in ACLR knees.
Our patient cohort additionally corroborates what is often considered the patient demographic at risk for sustaining a bucket-handle meniscus tear: relatively young, male, normal BMI athlete, with medial meniscus involvement more often than lateral meniscus involvement. The long duration of preoperative symptoms in some of our patients also points toward the fact that the etiology of bucket-handle meniscus tears is not always purely the result of a single, traumatic episode, and may additionally have a degenerative component.33 Similar patient demographics are frequently seen among the prior referenced literature, suggesting that this is the patient population whom orthopedic surgeons should be counseling on general knee health and knee injury prevention measures where applicable.
Limitations
Our study is limited inherently by its retrospective design, and the lack of a control group for comparison. While a heterogeneous cohort (in terms of exact tear types, locations, etc.) allowed us to perform comparative analyses, it limits what would otherwise be greater power with which we could draw conclusions from a homogeneous patient series. Determination of treatment failures was also based on patient follow-up with the treating surgeons at our institution, and so those who failed meniscal repair but presented to an outside institution would go unreported. We did not routinely perform second-look arthroscopy or repeat advanced imaging to confirm healing of the meniscal tissue, and thus asymptomatic re-tears or failures to heal may have gone unnoticed through postoperative examinations or clinical questioning. Our definition for “failure” of repair is thus a clinical failure rather than necessarily demonstrating a failure of repair. Additionally, our minimum follow-up of 6 months is relatively short; however, some authors have demonstrated through second-look arthroscopy that a bucket-handle meniscus tear can heal within 3 months after repair, and thus our minimum follow-up in this context is thus an appropriate timeframe to identify early postoperative failures while allowing for more significant power for regression analysis and minimizing the risk of selection bias into our data.23 However, some authors have additionally suggested that partial healing may be more common than we expect, and these situations may be asymptomatic but potentially still prone to repeat injury; these authors thus advocate longer-term studies in this patient population.21 Finally, as the treating surgeons in our study are sports fellowship trained with dedicated sports-specific practices, their surgical techniques and expertise may not be generalizable to all surgeon practices.
Conclusions
With the exception of the absence of other pathology (including ligament tear, contralateral compartment meniscal tear, or cartilage lesions) in the knee noted intraoperatively, no other variables were significantly associated with re-tear. The results are relatively durable with 84.6% survival at 1 year. Surgeons should attempt meniscal repair—using whichever surgical technique (inside-out/all-inside) they are most comfortable with—when presented with a bucket-handle tear.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Eric Cotter, Richard Rice, Blaine Manning, and Kevin Wang have nothing to disclose.
Bryan Saltzman reports the following disclosures: NOVA Science Publishers and Postgraduate Institute for Medicine: Publishing royalties.
Brian Forsythe reports the following disclosures: Arthrex, Inc.: Research support; Arthrosurface: Paid presenter or speaker; Jace Medical: Stock or stock options; Smith & Nephew: Research support; Sonoma: Paid consultant, Paid presenter or speaker; Stryker: Research support.
Nikhil Verma reports the following disclosures: American Orthopaedic Society for Sports Medicine: Board or committee member; American Shoulder and Elbow Surgeons: Board or committee member; Arthrex, Inc.: Research support; Arthroscopy: Editorial or governing board, Publishing royalties, financial or material support; Arthroscopy Association Learning Center Committee: Board or committee member; Arthrosurface: Research support; Cymedica: Stock or stock options; DJ Orthopaedics: Research support; Journal of Knee Surgery: Editorial or governing board; Minivasive: Paid consultant, stock or stock options; Omeros: Stock or stock options; Orthospace: Paid consultant; Ossur: Research support; SLACK Incorporated: Editorial or governing board; Smith & Nephew: IP royalties; paid consultant, research support; Athletico: Research support; ConMed Linvatec: Research support; Miomed: Research support; Mitek: Research support; Vindico Medical-Orthopedics Hyperguide: Publishing royalties, financial or material support.
Adam Yanke reports the following disclosures: Arthrex, Inc.: Research support; JRF Ortho: Paid consultant; Organogenesis: Research support.
Brian Cole reports the following disclosures: Aesculap/B. Braun: Research support; American Journal of Orthopaedics: Editorial or governing board; American Journal of Sports Medicine: Editorial or governing board; Aqua Boom: Stock or stock options; Arthrex, Inc.: IP royalties, Paid consultant, Research support; Arthroscopy: Editorial or governing board; Arthroscopy Association of North America: Board or committee member; Athletico: Other financial or material support; Biomerix: Stock or stock options; Cartilage: Editorial or governing board; DJ Orthopaedics: IP royalties; Elsevier Publishing: IP royalties; Flexion: Paid consultant; Geistlich: Research support; Giteliscope: Stock or stock options; International Cartilage Repair Society: Board or committee member; Journal of Bone and Joint Surgery–American: Editor only: Editorial or governing board; Journal of Shoulder and Elbow Surgery: Editor only: Editorial or governing board; Journal of the American Academy of Orthopaedic Surgeons: Editor only: Editorial or governing board; JRF Ortho: Other financial or material support; National Institutes of Health (NIAMS & NICHD): Research support; Operative Techniques in Sports Medicine: Publishing royalties, financial or material support; Ossio: Stock or stock options; Regentis: Paid consultant, stock or stock options; Sanofi-Aventis: Research support; Smith & Nephew: Other financial or material support, paid consultant; Tornier: Other financial or material support; Zimmer: Paid consultant, research support.
Ethical Approval: Ethical approval was provided by the institutional review board (#16082001).
Informed Consent: Informed consent was not sought for the present study because it was a retrospective observational cohort study that did not involve any invasive procedures. All prospectively collected data was part of the standard of care and quered retrospectively.
ORCID iD: Blaine T. Manning  https://orcid.org/0000-0001-8457-6602
https://orcid.org/0000-0001-8457-6602
References
- 1. Johnson RJ, Kettelkamp DB, Clark W, Leaverton P. Factors effecting late results after meniscectomy. J Bone Joint Surg Am. 1974;56:719-29. [PubMed] [Google Scholar]
- 2. DeHaven KE, Black KP, Griffiths HJ. Open meniscus repair. Technique and two to nine year results. Am J Sports Med. 1989;17:788-95. [DOI] [PubMed] [Google Scholar]
- 3. Thoreux P, Réty F, Nourissat G, Riviére X, Safa P, Durand S, et al. Bucket-handle meniscal lesions: magnetic resonance imaging criteria for reparability. Arthroscopy. 2006;22:954-61. [DOI] [PubMed] [Google Scholar]
- 4. Feng H, Hong L, Geng XS, Zhang H, Wang XS, Jiang XY. Second-look arthroscopic evaluation of bucket-handle meniscus tear repairs with anterior cruciate ligament reconstruction: 67 consecutive cases. Arthroscopy. 2008;24:1358-66. [DOI] [PubMed] [Google Scholar]
- 5. Magee TH, Hinson GW. MRI of meniscal bucket-handle tears. Skeletal Radiol. 1998;27:495-9. [DOI] [PubMed] [Google Scholar]
- 6. Wright DH, De Smet AA, Norris M. Bucket-handle tears of the medial and lateral menisci of the knee: value of MR imaging in detecting displaced fragments. AJR Am J Roentgenol. 1995;165:621-5. [DOI] [PubMed] [Google Scholar]
- 7. Shakespeare DT, Rigby HS. The bucket-handle tear of the meniscus. A clinical and arthrographic study. J Bone Joint Surg Br. 1983;65:383-7. [DOI] [PubMed] [Google Scholar]
- 8. Vautrin M, Schwartz C. Future of 34 meniscectomies after bucket-handle meniscus tear: a retrospective study with a follow-up over 22 years. Eur J Orthop Surg Traumatol. 2016;26:435-40. [DOI] [PubMed] [Google Scholar]
- 9. Albrecht-Olsen P, Kristensen G, Burgaard P, Joergensen U, Toerholm C. The arrow versus horizontal suture in arthroscopic meniscus repair. A prospective randomized study with arthroscopic evaluation. Knee Surg Sports Traumatol Arthrosc. 1999;7:268-73. [DOI] [PubMed] [Google Scholar]
- 10. Boody BS, Omar IM, Hill JA. Displaced medial and lateral bucket handle meniscal tears with intact ACL and PCL. Orthopedics. 2015;38:e738-e741. [DOI] [PubMed] [Google Scholar]
- 11. Krych AJ, Pitts RT, Dajani KA, Stuart MJ, Levy BA, Dahm DL. Surgical repair of meniscal tears with concomitant anterior cruciate ligament reconstruction in patients 18 years and younger. Am J Sports Med. 2010;38:976-82. [DOI] [PubMed] [Google Scholar]
- 12. Lim HC, Bae JH, Kim TS, Yang JH, Park SC, Yoon JR. Intra-articular patterns of bucket handle meniscal tears and its relation to reducibility. Clin Orthop Surg. 2012;4:129-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. O’Shea JJ, Shelbourne KD. Repair of locked bucket-handle meniscal tears in knees with chronic anterior cruciate ligament deficiency. Am J Sports Med. 2003;31:216-20. [DOI] [PubMed] [Google Scholar]
- 14. Sood A, Gonzalez-Lomas G, Gehrmann R. Influence of health insurance status on the timing of surgery and treatment of bucket-handle meniscus tears. Orthop J Sports Med. 2015;3:2325967115584883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Johnson D, Weiss B. Meniscal repair using the inside-out suture technique. Sports Med Arthrosc Rev. 2012;20:68-76. [DOI] [PubMed] [Google Scholar]
- 16. Burns TC, Giuliani JR, Svoboda SJ, Owens BD. Meniscus repair and transplantation techniques. J Knee Surg. 2011;24:167-74. [DOI] [PubMed] [Google Scholar]
- 17. Fillingham YA, Riboh JC, Erickson BJ, Bach BR, Jr, Yanke AB. Inside-out versus all-inside repair of isolated meniscal tears: an updated systematic review. Am J Sports Med. 2017;45:234-42. [DOI] [PubMed] [Google Scholar]
- 18. Mehta VM, Terry MA. Cyclic testing of 3 all-inside meniscal repair devices: a biomechanical analysis. Am J Sports Med. 2009;37:2435-9. [DOI] [PubMed] [Google Scholar]
- 19. Ramappa AJ, Chen A, Hertz B, Wexler M, Grimaldi Bournissaint L, DeAngelis JP, et al. A biomechanical evaluation of all-inside 2-stitch meniscal repair devices with matched inside-out suture repair. Am J Sports Med. 2014;42:194-9. [DOI] [PubMed] [Google Scholar]
- 20. Rosso C, Kovtun K, Dow W, McKenzie B, Nazarian A, DeAngelis JP, et al. Comparison of all-inside meniscal repair devices with matched inside-out suture repair. Am J Sports Med. 2011;39:2634-9. [DOI] [PubMed] [Google Scholar]
- 21. Solheim E, Hegna J, Inderhaug E. Long-term outcome after all-inside meniscal repair using the RapidLoc system. Knee Surg Sports Traumatol Arthrosc. 2016;24:1495-500. [DOI] [PubMed] [Google Scholar]
- 22. Shelbourne KD, Johnson GE. Locked bucket-handle meniscal tears in knees with chronic anterior cruciate ligament deficiency. Am J Sports Med. 1993;21:779-82. [DOI] [PubMed] [Google Scholar]
- 23. Tecklenburg K, Schoepf D, Hoser C, Fink C. Anterior cruciate ligament injury with simultaneous locked bucket-handle tears of both medial and lateral meniscus in a 19-year-old female professional ski racer: a case report. Knee Surg Sports Traumatol Arthrosc. 2007;15:1125-9. [DOI] [PubMed] [Google Scholar]
- 24. Espejo-Reina A, Serrano-Fernandez JM, Martin-Castilla B, Estades-Rubio FJ, Briggs KK, Espejo-Baena A. Outcomes after repair of chronic bucket-handle tears of medial meniscus. Arthroscopy. 2014;30:492-6. [DOI] [PubMed] [Google Scholar]
- 25. Cannon WD, Jr, Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med. 1992;20:176-81. [DOI] [PubMed] [Google Scholar]
- 26. Wasserstein D, Dwyer T, Gandhi R, Austin PC, Mahomed N, Ogilvie-Harris D. A matched-cohort population study of reoperation after meniscal repair with and without concomitant anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:349-55. [DOI] [PubMed] [Google Scholar]
- 27. Noyes FR, Barber-Westin SD. Arthroscopic repair of meniscal tears extending into the avascular zone in patients younger than twenty years of age. Am J Sports Med. 2002;30:589-600. [DOI] [PubMed] [Google Scholar]
- 28. Flynn JM. OKU 10: Orthopaedic knowledge update. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2011. Available from: http://digital.aaos.org/OKU_10/ [Google Scholar]
- 29. Pengas IP, Assiotis A, Nash W, Hatcher J, Banks J, McNicholas MJ. Total meniscectomy in adolescents: a 40-year follow-up. J Bone Joint Surg Br. 2012;94:1649-54. [DOI] [PubMed] [Google Scholar]
- 30. Shieh AK, Edmonds EW, Pennock AT. Revision meniscal surgery in children and adolescents: risk factors and mechanisms for failure and subsequent management. Am J Sports Med. 2016;44:838-43. [DOI] [PubMed] [Google Scholar]
- 31. Yilmaz S, Cankaya D, Firat A, Deveci A, Ozkurt B, Bozkurt M. Combined inside-out and all-inside technique in bucket-handle meniscus tears. Acta Orthop Bras. 2016;24:179-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ahn JH, Kim KI, Wang JH, Kyung BS, Seo MC, Lee SH. Arthroscopic repair of bucket-handle tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2015;23:205-10. [DOI] [PubMed] [Google Scholar]
- 33. Meister K, Indelicato PA, Spanier S, Franklin J, Batts J. Histology of the torn meniscus: a comparison of histologic differences in meniscal tissue between tears in anterior cruciate ligament-intact and anterior cruciate ligament-deficient knees. Am J Sports Med. 2004;32:1479-83. [DOI] [PubMed] [Google Scholar]