Abstract
Radical prostatectomy (RP) is the gold standard treatment method of localized prostate cancer. Today, this surgery is performed with open or minimally invasive methods. The history of open perineal RP (RPP) is very old, but it is not often preferred by urologists. The use of robot-assisted laparoscopic RP (RALP) is very frequently applied today. Robotic perineal RP (r-RPP) by using a Gel-Point and insufflating CO2 into the perineal region was first described in 2014. In this case report, we report a 68-year-old patient with localized prostate cancer in whom we successfully performed gasless r-RPP, and according to our knowledge, this is the first case of gasless r-RPP to be reported.
Keywords: Gasless, perineal approach, radical prostatectomy, robotic surgery
Introduction
Open radical prostatectomy (RP) has been the standard and primary treatment for localized prostate cancer. However, in recent years robot-assisted laparoscopic RP (RALP) has gained acceptance among urologists. Open perineal RP (RPP) was first described by Young in 1905.[1] This method was modified by approaching the prostate between the circumferential fibers of the external anal sphincter and the longitudinal fibers of the rectum by Belt.[2] In 1947, Millin[3] described prostatectomy through a retropubic approach. Walsh and Donker[4] described neurovascular bundles and nerve-sparing approach during retropubic prostatectomy in 1980s. Then, many urologists preferred the retropubic approach, which has less complex anatomy and the perineal approach has lost its popularity over time.[5] Weldon and Travel[6] defined the nerve-sparing RPP in 1988. However, this development has not reduced interest in the retropubic approach.
RALP was first applied by Binder and Kramer[7] in Europe in 2000 and its use has spread rapidly in recent years. Robotic perineal RP (r-RPP) was first performed by Kaouk et al.[8,9] in a cadaver model and then in 4 living cases. Then, we published our experience on 15 patients in whom we performed r-RPP and showed that r-RPP was feasible and effective.[10]
r-RPP is performed by inserting a Gel-Point and insufflating CO2 into the perineal region. In this case report, we aimed to present the first successfully performed case of r-RPP without the use of Gel-Point and gas.
Case presentation
A 68-year-old male patient was admitted to urology outpatient clinic with symptoms of nocturia. He had no additional disease other than hypertension. He had a history of open appendectomy and cholecystectomy. His prostate-specific antigen (PSA) was 7.7 ng/mL and a transrectal ultrasound-guided prostate biopsy was performed. Gleason score 7 (3 + 4) adenocarcinoma was reported in 4 of 12 foci. In multiparametric magnetic resonance imaging (mpMRI), a Prostate Imaging Reporting and Data System (PI-RADS) 4 lesion was detected on the right peripheral zone and no extraprostatic invasion was observed. The prostate volume was 30 cc. International Index of Erectile Function (IIEF) was 17. Gasless r-RPP was planned.
The patient was kept in the position of exaggerated lithotomy with 15° Trandelenburg. An 18 fr Foley catheter was inserted and the urinary bladder was emptied. To perform a rectal examination during the surgery, a sterile glove was placed in the rectum and sutured to the anus circumferentially. A 6-cm surgical incision was made between bilateral tuberculum ischiadicum (Figure 1a). Then, an incision was made in the central tendon (Figure 1b). Using the Belt approach, rectourethral muscles were reached and cut and the dissection was terminated. Retractors was placed in situ (Figure 1c). A Da Vinci XI robotic system (Intuitive Surgical Inc., Sunnyvale, CA, USA) was used without using gas and Gel-Point. Using three 8-mm robotic trocars, and monopolar curved scissors, and when required, a large needle driver were placed in the right side, fenestrated bipolar forceps was placed in the left side and 30° up scope was placed at the 12 o’clock position (Figure 1d).
Figure 1. a–d.
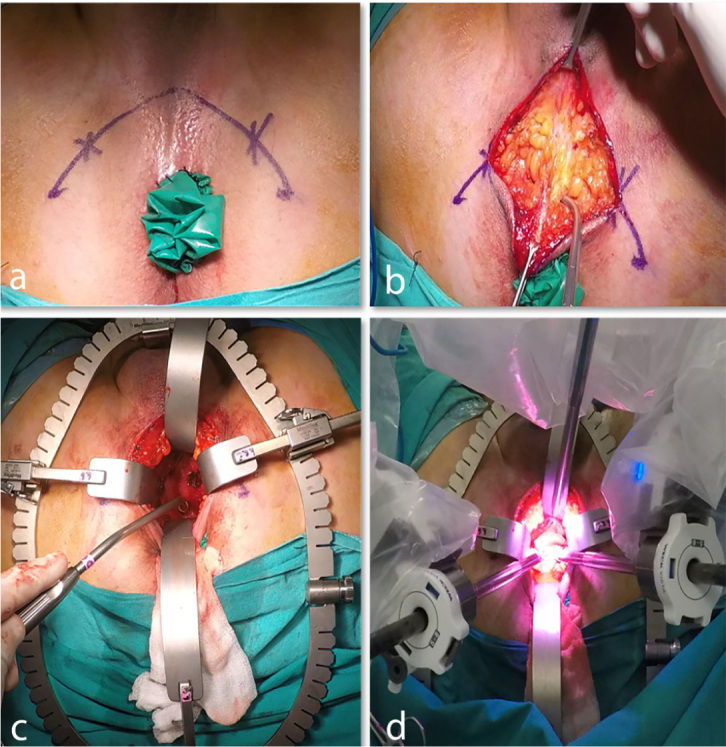
The perineal access for the gasless robotic perineal radical prostatectomy. (a) Glove placed in the rectum and incision between bilateral tuberculum ischiadicum; (b) Incision of central tendon; (c) Placement of retractors; (d) 30° up scope at the 12 o’clock position, monopolar curved scissors in the right side, fenestrated bipolar forceps in the left side
The dissection was started from the prostate apex and extended to lateral areas, then posterior and posterolateral pedicles were dissected (Figure 2a). The membranous urethra was then dissected while protecting the external urinary sphincter (Figure 2b). Hem-o-lok clip (Teleflex Medical, Research Triangle Park, North Carolina, USA) was placed on the Foley catheter for retraction and the Foley catheter was cut using laparoscopic scissors from the distal to the clip (Figure 2c). The dissection was expanded to the basis with protection of the deep dorsal vein complex and endopelvic fascia, and the bladder neck was dissected (Figure 2d). The dissection was expanded posteriorly and the prostatectomy was completed with dissection of the seminal vesicles. Vesicourethral anastomosis was completed using two 3/0 V-Loc™sutures (Covidien, Mansfield, MA, USA). The bladder was inflated with 200 mL physiologic saline and no leakage was observed.
Figure 2. a–d.
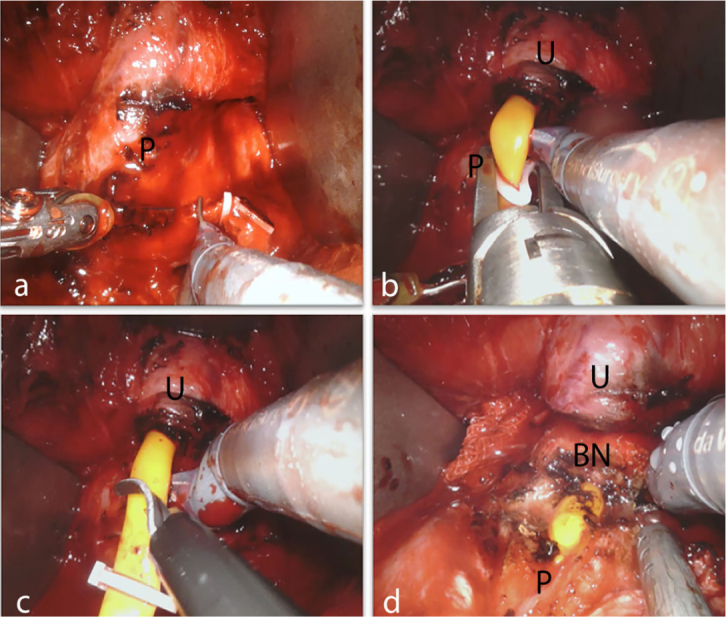
Gasless robotic perineal radical prostatectomy. (a) Dissection of posterolateral pedicles; (b) Dissection of the membranous urethra; (c) Cutting of Foley catheter distal to the clip; (d)
Bladder neck dissection. U: urethra; P: prostate; BN: bladder neck
The duration of the operation was 130 min, and the estimated blood loss was 130 cc. No perioperative or postoperative complications were observed. The patient was discharged on the 3rd postoperative day. The Foley catheter was removed in the 10th postoperative day. The patient was continent immediately. The postoperative pathology report showed pT2c, Gleason 7 (3+4) adenocancer and negative surgical margins.
Discussion
RPP is not preferred by many urologists today, compared with retropubic RP (RRP). However, the prostate is easily reached from the perineum and it is clear that the perineal approach is much more advantageous in the selected patient group. Patients who have had previous pelvic surgery, hernia repair using mesh, renal transplantation, pelvic/abdominal vascular by-pass grafting, and radiotherapy because of prostate cancer but needed salvage prostatectomy are more appropriate patient groups for the perineal approach. The perineal approach may also be more appropriate for obese patients.[11] The studies showed that RRP was not superior to RPP in terms of cancer control and continence rates, even though RPP is related with shorter hospital stay, lesser blood loss, lower transfusion rates, lesser amount of analgesic use, and lower postoperative incidence of anastomotic stenosis compared with RRP.[8] In addition, RPP is performed in the extraperitoneal compartment, which also reduces patient discomfort and the possibility of postoperative ileus and provides an early return of appetite and bowel movements. Another advantage of RPP is that it protects the deep dorsal vein complex by retracting it upwards.[12]
There are disadvantages of RPP. First, the surgery is performed in a narrow area which makes it difficult for the surgeon to work ergonomically. Also, the surgeon’s vision is restricted which complicates the surgery. r-RPP, defined by Kaouk et al.[8,9], overcomes such difficulties and allows for better maneuverability inside the narrow area with robotic instruments and renders magnified 3D image of the operative field. It seems that robotic surgery is increasing the interest in the perineal approach.
Uro-oncological surgeries are successfully conducted in many centers because of the increased experience in laparoscopic and robotic surgery. In addition to the advantages of laparoscopic surgery, it has a few disadvantages. The most important of these are complications related to CO2 insufflation. For instance, due to the increased intraabdominal pressure, the vena cava inferior is compressed, resulting in decreased venous return and cardiac output. At the same time, the mean arterial pressure increases, and cardiac index decreases, while CO2 absorption causes hypercarbia decreasing blood pH. In addition, an unexpected vascular injury can lead to CO2 embolism, which requires immediate resuscitation. Pneumoperitoneum and the Trendelenburg position compress the diaphragm, which leads to a significant decrease in forced expiratory volume, peak expiratory flow, and forced vital capacity, resulting in a decrease in pulmonary compliance.[13] In trials comparing extraperitoneal and intraperitoneal CO2 insufflation in RALP, it was found that CO2 absorption and acidosis were more likely with extraperitoneal RALP.[14] Therefore, since perineal field is situated in the extraperitoneal area, it may be thought that complications due to CO2 insufflation may be seen more frequently. We reported that one patient was converted to open surgery due to CO2 retention in our case series involving 15 r-RPP patients.[10] To our knowledge, this case report is the first description of gasless r-RPP.
To prevent complications caused by pneumoperitoneum, gasless laparoscopic methods have been tried. Paolucci et al.[15] described the technique of removing the abdominal wall with a fan-formed wall retractor, which was placed subcutaneously to create a space for the surgeon to work without creating a pneumoperitoneum. Kakde et al.[13] described a challenging approach during RALP without CO2 insufflation that uses a procedure called ‘tenting of abdominal wall’ after docking the robotic arms. The authors showed that this technique reduced peak airway pressure while maintaining adequate abdominal cavity. Dal Moro and Mangano[16] emphasized that it was not always possible to conclude all the steps of RALP without gas, that there was a risk of massive bleeding during dissection of Santorini plexus or neurovascular bundle, and that CO2 insufflation should be resumed in these phases until venous vessels were closed. This advantage of CO2 insufflation may be overlooked for r-RPP because the deep dorsal vein complex is not opened in r-RPP and r-RPP gives opportunity to intervene neurovascular bundles from a shorter distance.
This case report is particularly interesting because of favorable anesthesiologic and oncologic outcomes. In our opinion, the main benefit of the gasless method is the absence of the CO2 retention risk. Another advantage is the relatively shorter operative time. In gasless r-RPP, we start the surgery with robotic arms directly, but in r-RPP with gas, Gel-Point is placed, then the subcutaneous adipose tissue is hung on the skin with sutures and stabilized on the skin with a hem-o-lok clips to increase exposure, the robotic arms are then placed in the Gel-Point. Another benefit of gasless r-RPP is that it is more cost-effective than r-RPP with gas. The advantage of this method compared with RPP is the magnified 3D view and maneuverability in a narrow area, which are provided by robotic surgery. We believe that the disadvantage of this method is that the estimated amount of bleeding compared with r-RPP with gas may increase due to the lack of CO2 pressure; nevertheless, we believe that this risk is no greater than encountered in RPP.
In conclusion, gasless r-RPP may be an effective and feasible method, but comparative studies with greater number of patients are needed.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – A.İ.T., A.Ş., V.T.; Design – A.İ.T., A.Ş.; Supervision – A.İ.T., A.Ş., V.T.; Resources – A.İ.T., A.Ş., V.T., S.Ş.; Materials – E.Ş., K.G.Ş., S.Ş.; Data Collection and/or Processing – A.Ş., K.G.Ş., Ş.Ş., F.A.A.; Analysis and/or Interpretation – A.Ş., E.Ş., K.G.Ş., F.A.A.; Literature Search – A.Ş., E.Ş., K.G.Ş., F.A.A.; Writing Manuscript – A.Ş., E.Ş., K.G.Ş., S.Ş.; Critical Review – A.Ş., E.Ş., F.A.A.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Young HH. The early diagnosis and radical cure of carcinoma of the prostate. Being a study of 40 cases and presentation of a radical operation which was carried out in four cases. 1905. J Urol. 2002;168:914–21. doi: 10.1016/S0022-5347(05)64542-9. [DOI] [PubMed] [Google Scholar]
- 2.Belt E, Turner RD. A study of 229 consecutive cases of total perineal prostatectomy for cancer of the prostate. J Urol. 1957;77:62–77. doi: 10.1016/S0022-5347(17)66523-6. [DOI] [PubMed] [Google Scholar]
- 3.Millin T. Retropubic prostatectomy. J Urol. 1948;59:267–80. doi: 10.1016/S0022-5347(17)69374-1. [DOI] [PubMed] [Google Scholar]
- 4.Walsh PC, Donker PJ. Impotence following radical prostatectomy: insight into etiology and prevention. J Urol. 1982;128:492–7. doi: 10.1016/S0022-5347(17)53012-8. [DOI] [PubMed] [Google Scholar]
- 5.Akca O, Zargar H, Kaouk JH. Robotic Surgery Revives Radical Perineal Prostatectomy. Eur Urol. 2015;68:340–1. doi: 10.1016/j.eururo.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Weldon VE, Tavel FR. Potency-sparing radical perineal prostatectomy: anatomy, surgical technique and initial results. J Urol. 1988;140:559–62. doi: 10.1016/S0022-5347(17)41718-6. [DOI] [PubMed] [Google Scholar]
- 7.Binder J, Kramer W. Robotically-assisted laparoscopic radical prostatectomy. BJU Int. 2001;87:408–10. doi: 10.1046/j.1464-410x.2001.00115.x. [DOI] [PubMed] [Google Scholar]
- 8.Laydner H, Akça O, Autorino R, Eyraud R, Zargar H, Brandao LF, et al. Perineal robot-assisted laparoscopic radical prostatectomy: feasibility study in the cadaver model. J Endourol. 2014;28:1479–86. doi: 10.1089/end.2014.0244. [DOI] [PubMed] [Google Scholar]
- 9.Kaouk JH, Akca O, Zargar H, Caputo P, Ramirez D, Andrade H, et al. Descriptive Technique and Initial Results for Robotic Radical Perineal Prostatectomy. Urology. 2016;94:129–38. doi: 10.1016/j.urology.2016.02.063. [DOI] [PubMed] [Google Scholar]
- 10.Tuğcu V, Akça O, Şimşek A, Yiğitbaşı İ, Şahin S, Taşçı Aİ. Robot-assisted radical perineal prostatectomy: first experience of 15 cases. Turk J Urol. 2017;43:476–83. doi: 10.5152/tud.2017.35488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holzbeierlein JM, Porter HJ, 2nd, Thrasher JB. The craft of urologic surgery: modern radical perineal prostatectomy. Urol Clin North Am. 2004;31:629–41. xi–xii. doi: 10.1016/j.ucl.2004.04.021. [DOI] [PubMed] [Google Scholar]
- 12.Gillitzer R, Thüroff JW. Relative advantages and disadvantages of radical perineal prostatectomy versus radical retropubic prostatectomy. Crit Rev Oncol Hematol. 2002;43:167–90. doi: 10.1016/S1040-8428(02)00016-1. [DOI] [PubMed] [Google Scholar]
- 13.Kakde AS, Wagh HD. An observational study: Effects of tenting of the abdominal wall on peak airway pressure in robotic radical prostatectomy surgery. Saudi J Anaesth. 2017;11:279–82. doi: 10.4103/sja.SJA_560_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dal Moro F, Crestani A, Valotto C, Guttilla A, Soncin R, Mangano A, et al. Anesthesiologic effects of transperitoneal versus extraperitoneal approach during robot-assisted radical prostatectomy: results of a prospective randomized study. Int Braz J Urol. 2015;41:466–72. doi: 10.1590/S1677-5538.IBJU.2014.0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paolucci V, Gutt CN, Schaeff B, Encke A. Gasless laparoscopy in abdominal surgery. Surg Endosc. 1995;9:497–500. doi: 10.1007/BF00206834. [DOI] [PubMed] [Google Scholar]
- 16.Moro FD, Mangano A. Why should a “gasless” oncologic robotic procedure be performed? Saudi J Anaesth. 2017;11:260–1. doi: 10.4103/sja.SJA_53_17. [DOI] [PMC free article] [PubMed] [Google Scholar]


