Abstract
Computed tomography angiography is frequently used for double rule out of obstructive coronary artery disease and pulmonary embolism in patients presenting to the emergency department with acute chest pain, but it is rare to see concomitant acute coronary occlusion and pulmonary embolism on the same computed tomography angiography scan. (Level of Difficulty: Beginner.)
Key Words: computed tomography angiography, double rule out, paradoxical coronary embolism, patent foramen ovale
Graphical abstract
Computed tomography angiography is frequently used for double rule out of obstructive coronary artery disease and pulmonary embolism in patients…
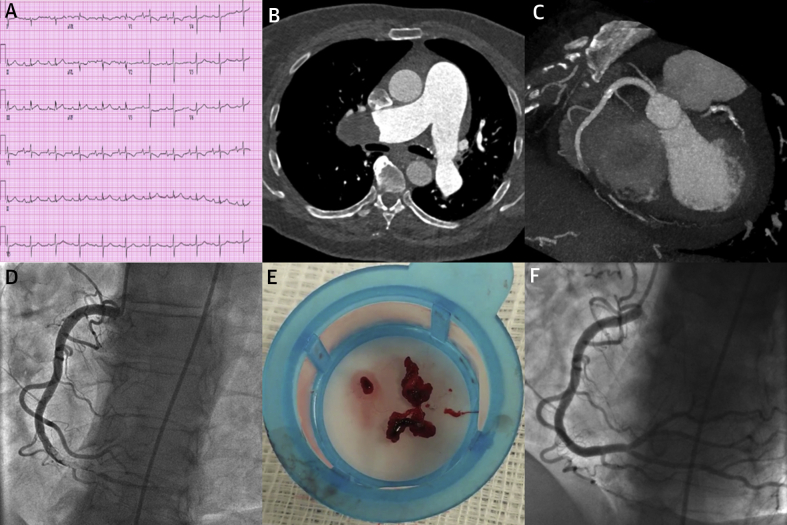
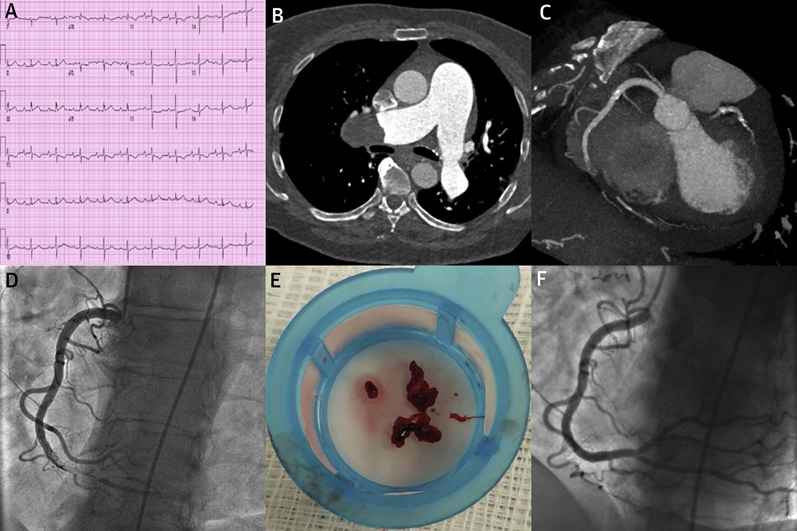
A 71-year-old female patient with a history of recurrent pulmonary emboli (PE), chronic thromboembolic pulmonary hypertension, and multiple coronary artery disease risk factors presented to the emergency department with chest pain and a mildly elevated troponin level. An electrocardiogram showed a normal sinus rhythm of 62 beats/min, first-degree atrioventricular block, right-axis deviation, and nonspecific ST-T wave changes (Figure 1A). Computed tomography angiography of the pulmonary and coronary circulation was performed for a double rule out (single contrast bolus of 120 ml, 2 separate scans, Siemens SOMATOM Definition Flash, Siemens Health Diagnostics, Tarrytown, New York). It showed recurrent PE, with nearly complete occlusion of the right pulmonary artery (Figure 1B). Surprisingly, it also showed a 3-cm long occlusion of the distal right coronary artery (Figure 1C). This lesion was believed to be acute because of the absence of any calcification or bridging collateral vessels. There was no thrombus seen in the left heart chambers. She underwent urgent invasive coronary angiography that confirmed the right coronary artery occlusion (Figure 1D). Aspiration thrombectomy of the right coronary artery was performed with removal of a large thrombus burden (Figure 1E). There was no underlying plaque seen, and hence stent placement was deferred (Figure 1F). She was deemed to have a coronary embolism, and a paradoxical source (with right-to-left shunt) was suspected given the presence of a new PE. Echocardiography showed a patent foramen ovale (PFO) with right-to-left shunting. She was not a candidate for PFO closure because of severe pulmonary hypertension and right ventricular dysfunction.
Figure 1.
Concomitant Acute Coronary Occlusion and Pulmonary Embolism
(A) Electrocardiogram showing a normal sinus rhythm at 62 beats/min, first degree atrioventricular block, right axis deviation, and nonspecific ST-T wave changes. (B) Computed tomography angiography showing a large clot in the right pulmonary artery. (C) Computed tomography angiography showing occlusion of the distal right coronary artery. The acute contrast cutoff along with absence of any calcification is suggestive of thrombotic occlusion. (D) Invasive coronary angiogram showing thrombotic occlusion of the distal right coronary artery. (E) Photograph of fresh thrombus retrieved with aspiration thrombectomy. (F) Invasive coronary angiogram performed after aspiration thrombectomy that shows complete resolution of the right coronary artery occlusion without any residual plaque.
Paradoxical coronary embolism is a rare cause of acute coronary syndrome (1). In patients presenting to the emergency department with acute chest pain, computed tomography angiography is frequently used for double rule out of obstructive coronary artery disease and PE when the diagnosis is not clear (2). A 2018 European interdisciplinary position paper on PFO management gave a strong recommendation to perform percutaneous closure of a PFO in carefully selected patients 18 to 65 years of age with confirmed systemic embolism and an estimated high probability of a causal role of the PFO (3). Concomitant acute coronary occlusion and PE have been reported, but it is rare to see both (double rule in) disorders on the same computed tomography angiography scan.
Footnotes
Dr. Prins has received funding from the National Heart, Lung and Blood Institute (grant K08 HL140100). All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Informed consent was obtained for this case.
References
- 1.Prizel K.R., Hutchins G.M., Bulkley B.H. Coronary artery embolism and myocardial infarction. Ann Intern Med. 1978;88:155–161. doi: 10.7326/0003-4819-88-2-155. [DOI] [PubMed] [Google Scholar]
- 2.Raff G.L., Chinnaiyan K.M., Cury R.C. SCCT guidelines on the use of coronary computed tomographic angiography for patients presenting with acute chest pain to the emergency department: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr. 2014;8:254–271. doi: 10.1016/j.jcct.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 3.Pristipino C., Sievert H., D’Ascenzo F. European position paper on the management of patients with patent foramen ovale. General approach and left circulation thromboembolism. Eur Heart J. 2019;40:3182–3195. doi: 10.1093/eurheartj/ehy649. [DOI] [PubMed] [Google Scholar]