Abstract
Context
Current clinical assessments used for patients with anterior cruciate ligament reconstruction (ACLR) may not enable clinicians to properly identify functional deficits that have been found in laboratory studies. Establishing muscular-function assessments, through agility and balance tasks, that can properly differentiate individuals with ACLR from healthy, active individuals may permit clinicians to detect deficits that increase the risk for poor outcomes.
Objective
To compare lower extremity agility and balance between patients with ACLR and participants serving as healthy controls.
Design
Case-control study.
Setting
Controlled laboratory.
Patients or Other Participants
A total of 47 volunteers in 2 groups, ACLR (9 males, 11 females; age = 23.28 ± 5.61 years, height = 173.52 ± 8.89 cm, mass = 70.67 ± 8.89 kg) and control (13 males, 12 females; age = 23.00 ± 6.44, height = 172.50 ± 9.24, mass = 69.81 ± 10.87 kg).
Main Outcome Measure(s)
Participants performed 3 timed agility tasks: Agility T Test, 17-hop test, and mat-hopping test. Balance was assessed in single-legged (SL) stance in 3 positions (straight knee, bent knee, squat) on 2 surfaces (firm, foam) with the participants' eyes open or closed for 10-second trials. Agility tasks were measured for time to completion. Eyes-open balance tasks were measured using center-of-pressure average velocity, and eyes-closed balance tasks were measured using the Balance Error Scoring System.
Results
For the Agility T Test, the ACLR group had slower times than the control group (P = .05). Times on the Agility T Test demonstrated moderate to strong positive relationships for unipedal measures of agility. The ACLR group had greater center-of-pressure average velocity in the SL bent-knee position than the control group. No differences were found between groups for the SL straight-knee and SL-squat balance tasks (P > .05). No differences in errors were present between groups for the eyes-closed balance tasks (P > .05).
Conclusions
The ACLR group demonstrated slower bipedal agility times and decreased postural stability when assessed in an SL bent-knee position compared with the control group.
Keywords: postural control, postural stability, muscle function
Anterior cruciate ligament (ACL) reconstruction (ACLR) is one of the most commonly performed orthopaedic surgeries to restore joint stability after an ACL tear, with up to 175 000 procedures each year in the United States.1 Anterior cruciate ligament injury most often occurs in young, active individuals, and the majority of injuries occur through noncontact mechanisms, such as pivoting and cutting.2,3 Whereas surgical and rehabilitation treatments have been established to address ACL injury, large financial and time burdens can persist long after the initial trauma.2 Only about 63% of patients with ACLR returned to their previous levels of activity after reconstruction.4 Patients with ACLR often experience persistent quadriceps weakness,5,6 a high risk of reinjury,7 and a greater risk of early-onset osteoarthritis.8 Functional assessments are aimed at identifying deficits that increase the risk for poor outcomes.9
In preparation for return to activity after ACLR, functional assessments should test the patient's ability to complete agile movements that simulate the demand of activity and sport.10 Tests such as the Agility T Test, modified pro shuttle, and modified long shuttle are commonly used to assess agility in healthy athletes and determine whether it is safe for injured athletes to return to activity.11,12 Poor performance raises concerns for reinjury. Patients with ACLR have been reported to exhibit deficits, such as larger kinematic and kinetic asymmetries during gait13 and greater knee-abduction moments during a drop-landing task,14 on assessments not typically available to clinicians. These reported deficits may pose a problem for individuals returning to participation after ACLR, as larger abduction moments have been found to be a risk factor for ACL injury.2
When considering which task to use to assess the possibility of a safe return to participation, clinicians should note that most activity tasks in the literature encompass measures of bipedal movement.15 However, much sporting activity is performed in a single-legged (SL) stance, stressing the importance of unilateral testing. For unilateral testing, establishing limb symmetry indexes for agility tasks, similar to strength tests,16 may provide additional information that informs decision making for the return to physical activity after ACLR.
Patients and clinicians benefit from objective information about lower extremity strength and performance that documents the progression through postoperative rehabilitation and better informs decision making for the return to physical activity. Single-limb balance is a common test used to assess postural control in patients with ACLR.17–19 These tasks are often performed with the knee extended, which produces a low internal knee-extensor moment, reducing the demand on the quadriceps.20 Researchers21 have reported no balance differences between patients with ACLR and healthy individuals when these tasks are performed in an extended-knee position. These results may suggest that a straight, stable knee position may not sufficiently activate the surrounding musculature.22 Furthermore, the mechanism of ACL injuries is commonly with the knee in slight flexion,23 which suggests that postural control of the knee should be assessed in this position. Numerous investigators have evaluated postural stability by modulating vision,24 surface,18 and joint position.25 We do not currently know which clinical assessment best differentiates individuals with ACLR who are at risk for reinjury from healthy, active individuals. Given that poor postural control is a risk factor for reinjury,26 it is important to understand which clinical tests identify this deficit in these patients. Therefore, the purpose of our study was to compare performance on agility and balance tasks in SL balance positions between individuals with ACLR and healthy, active participants. We hypothesized that assessments requiring greater knee flexion would demonstrate larger differences in the postural stability of participants with ACLR than in controls. We also hypothesized that unilateral assessments of agility would result in greater magnitudes of difference between patients with ACLR and control participants than dual-limb measures of agility.
METHODS
For this case-control, descriptive laboratory study, the independent variable was group (ACLR, control), and the dependent variables were center-of-pressure (COP) average velocity, balance errors, and the time to complete all agility tasks. Different testing conditions for the balance measures were position (SL straight knee, SL bent knee, SL squat), surface (firm, foam), and vision (eyes open, eyes closed). Agility was assessed using the Agility T Test, 17-hop–agility task, and mat-hopping task.
Participants
A total of 47 people participated in the study: 22 patients with ACLR and 25 healthy, recreationally active individuals (Table 1). All participants were from 18 to 45 years of age and deemed recreationally active according to the American College of Sports Medicine guidelines,27 exercising at least 30 minutes, 3 times each week. Individuals with ACLR were included if they had undergone a primary, unilateral, uncomplicated ACLR and reported no history of any other lower extremity surgery. Healthy participants were included in the control group if they reported no history of lower extremity injury within the 6 months before the study, no history of lower extremity surgery, and no neurologic conditions. Each participant provided written informed consent, and the study was approved by our university's institutional review board.
Table 1.
Participant Demographics
| Characteristic |
Group |
χ2 Value |
P Value |
|
| Anterior Cruciate Ligament Reconstruction (n = 22) | Control (n = 25) | |||
| No. | ||||
| Sex (males/females) | 9/11 | 13/12 | 0.45 | .45 |
| Graft type | cadaver = 1, patellar tendon = 10, hamstrings = 11 | NA | NA | NA |
| Mean ± SD |
t45 Value |
|||
| Age, y | 23.28 ± 5.61 | 23.00 ± 6.44 | 0.16 | .88 |
| Height, cm | 173.52 ± 8.89 | 172.50 ± 9.24 | 0.39 | .70 |
| Mass, kg | 70.67 ± 8.89 | 69.81 ± 10.87 | 0.25 | .81 |
| Time since surgery, mo | 28.11 ± 19.30 | NA | NA | NA |
| Tegner Activity Scale score | 6.59 ± 1.59 | 6.56 ± 1.58 | 0.67 | .95 |
| Godin Leisure-Time Exercise Questionnaire score | 264.44 ± 195.40 | 280.05 ± 166.22 | 0.29 | .77 |
| International Knee Documentation Committee Subjective Knee Form score | 85.95 ± 10.31 | 98.30 ± 3.15 | 5.70 | <.001 |
Abbreviation: NA, not applicable.
Instruments
Each participant completed the Tegner Activity Scale,28 Godin Leisure-Time Exercise Questionnaire,29 and International Knee Documentation Committee Subjective Knee Form.30 Completion times for the Agility T Test, 17-hop task, and mat-hopping task were collected using the Trainer (Fitlight Corp, Aurora, ON, Canada) set to trigger the time at the start and finish of each task. The Agility T Test has demonstrated reliability and was performed similar to the description in the literature.11 The 17-hop–agility task was modified from the speedy-jump test, which has been reported to be reliable for functional testing.31 Lastly, to assess unipedal agility, we adapted the mat-hopping task, which Caffrey et al32 developed to assess functional ankle instability and termed the square-hop test.
The COP average velocity was collected using the Pressure Mat (Tekscan, Inc, South Boston, MA) and processed via the FootMat Software for Researchers (version 7.10-13; Tekscan, Inc) for all eyes-open tasks. The eyes-closed balance tasks were recorded via video with the LifeCam Cinema Webcam (Microsoft Corp, Redmond, WA). A clear, plastic goniometer (Fabrication Enterprises Inc, White Plains, NY) was used to set the knee-flexion angle to 30° before the SL bent-knee balance task. Balance tasks on a foam surface were performed on a foam pad (Airex Balance Pad; Perform Better, West Warwick, RI). A tape measure was used to set up the agility tasks and to measure the reach distance on the SL squat.
Testing Procedures
Participants completed a single testing session. After a standard warmup of a 5-minute jog, participants completed agility tests and then balance tasks while wearing the athletic shoes of their choice. For all unilateral tasks of balance and agility, we tested the uninvolved limb of participants with ACLR and the dominant limb of the control individuals and then tested the opposite limb. Limb dominance for the controls was defined subjectively as the limb with which they would kick a ball for distance.
Agility Tests
Participants completed the Agility T Test (Figure 1) followed by the 17-hop task (Figure 2) and mat-hopping task (Figure 3). After a walkthrough of the Agility T Test course with the clinician (A.N.K.), participants completed practice trials until they were comfortable with the task. We instructed participants to (1) sprint forward from cone A and touch cone B, (2) side shuffle laterally to the left and touch cone C, (3) side shuffle to the right to touch cone D, (4) side shuffle back to the left to touch cone B, and (5) back pedal until they reached cone A (Figure 1). After the practice trials, participants completed the course as quickly as possible. Each participant completed 1 timed trial of this task.
Figure 1.
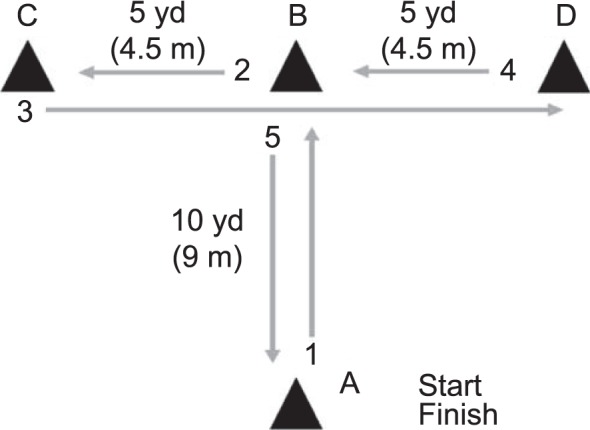
Course instruction for the Agility T Test.
Figure 2.
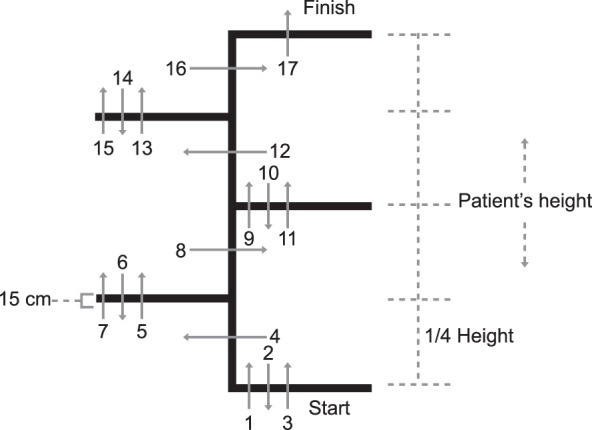
Course instruction for the 17-hop agility test as performed on the right foot. When starting on the left foot, participants start on the opposite side. This test was adapted from Hildebrandt et al.31
Figure 3.
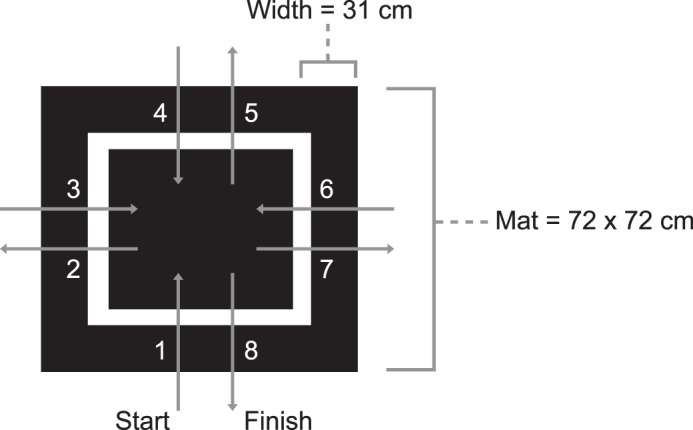
Course instruction for the mat-hopping test as performed clockwise on the right foot for a total of 8 hops. This test was adapted from Caffrey et al.32
The 17-hop–task course was standardized to each participant's height, with each section measuring one-fourth of the total height (Figure 2). Participants had to clear 15-cm-wide tape rungs, instead of the hurdles described in the literature,31 for patient safety. With this modification, the tape width was equal to that of the commonly performed cross-hop-for-distance assessment.33 Participants were shown the 17-hop pattern (Figure 2) and then completed practice trials until they were comfortable with the task. We recorded 1 timed test trial per limb, starting with the uninvolved or dominant limb. Hildebrandt et al31 provided a more detailed description of this test.
The mat-hopping task was completed on a 72- × 72-cm mat placed on a firm, flat surface with a 41- × 41-cm inner box taped on the mat. The clinician (A.N.K.) demonstrated the 8-hop pattern (Figure 3) that participants were to complete. Starting on the uninvolved limb, participants completed as many practice trials as needed followed by 1 timed test trial. We recorded 1 timed test trial per limb starting with the uninvolved or dominant limb. Caffrey et al32 offered a more detailed description of this test.
Key Points
Compared with the healthy control group, the anterior cruciate ligament reconstruction (ACLR) group demonstrated slower times for bipedal agility testing and worse single-legged (SL) postural control when performed in a bent-knee position.
When performed in a straight-knee or squat position, SL balance was not different between the ACLR and control groups.
Performance on the Agility T Test was moderately correlated with scores on the mat-hopping task and strongly correlated with scores on the 17-hop task.
When evaluating patients with ACLR, clinicians should include bipedal measures of agility and SL balance with the knee flexed to best identify deficits.
Balance Tasks
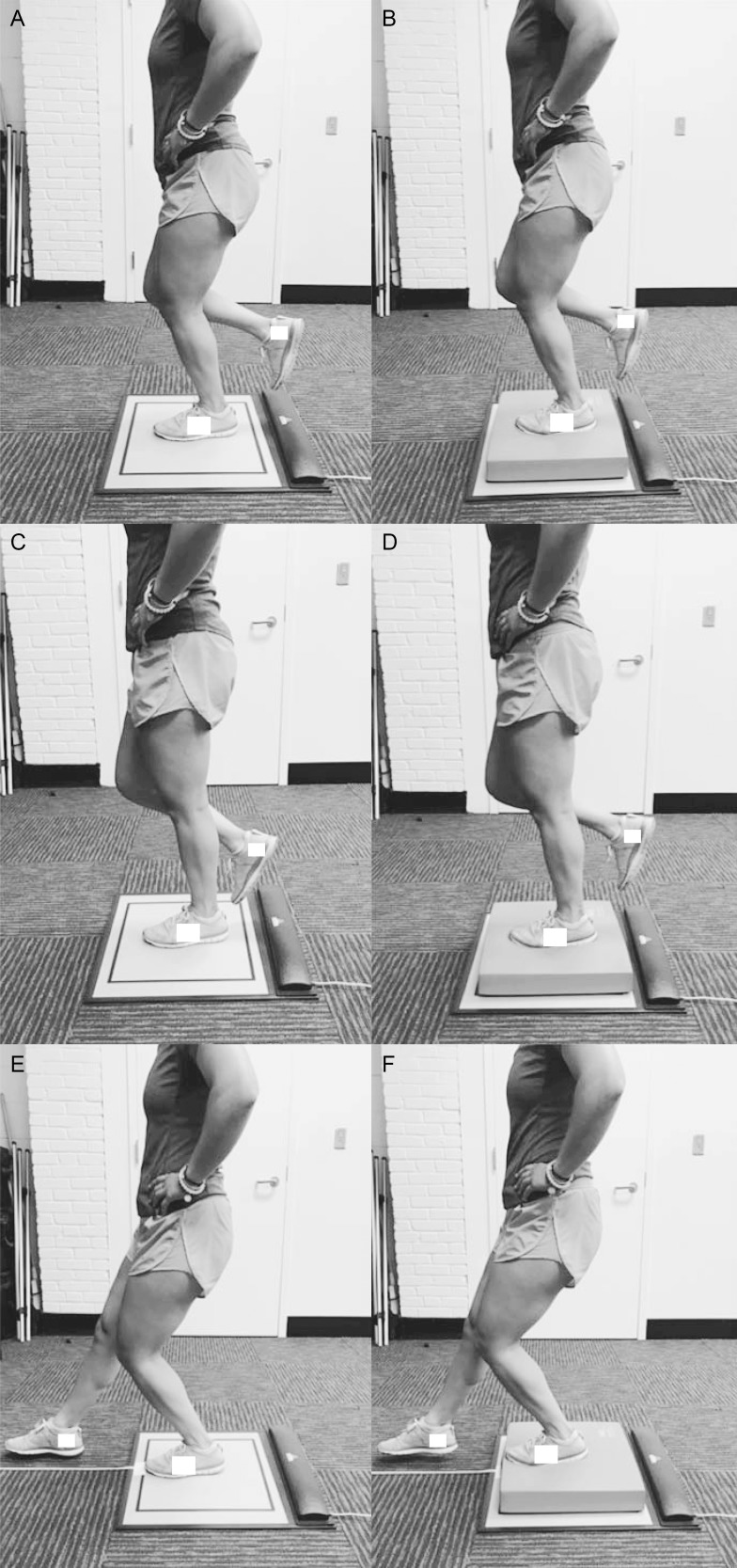
Balance tasks consisted of SL balance in 3 conditions (Figure 4): SL straight knee, SL bent knee, and SL squat. All balance tasks were performed as one 10-second trial on the uninvolved limb, followed by the involved limb. A minimum 60-second rest was given between trials to limit fatigue. Each limb was tested with the participants' eyes open and closed, as well as while standing on firm and foam surfaces. For all eyes-open tasks, the COP average velocity was measured using the Pressure Mat. A single clinician (A.N.K.) recorded the trials and retrospectively scored balance errors for all eyes-closed tasks. Errors were scored consistent with the Balance Error Scoring System guidelines.34
Figure 4.
Participant position for all single-legged balance tasks. The participants' position for the straight-knee balance task on the, A, firm and, B, foam surfaces. The participants' position for the bent-knee balance task on the, C, firm and, D, foam surfaces. Their knees were bent to a 30° angle as measured by a plastic goniometer before the start of each trial. The participants' position for the single-legged squat balance task on, E, firm and, F, foam surfaces. Participants were instructed to reach out anteriorly with the contralateral foot as far as possible. Reach distance was recorded in centimeters.
The SL straight-knee balance task was the first balance task completed (Figure 4). After the clinician (A.N.K.) demonstrated the task, participants performed one 10-second trial of balancing with a straight knee on the firm surface with their eyes open. They performed 1 timed trial on the uninvolved limb, followed by 1 timed trial on the involved limb. Participants completed the same tasks with their eyes closed and then repeated the tasks on the foam surface.
The second balance task was the SL bent-knee balance task (Figure 4). Participants completed all trials with their knees bent to a 30° angle as measured by the clinician (A.N.K.) using a plastic goniometer before each trial. They performed this task with their eyes open on a firm surface while standing on the uninvolved limb for one 10-second trial, followed by standing on the involved limb for one 10-second trial. They completed the same tasks with their eyes closed and then repeated these tasks on the foam surface.
The SL squat used in our study was modified from the anterior-reach direction of the Star Excursion Balance Test. This test has demonstrated decreased anterior-reach distances in patients with ACLR.35 For our study, participants were instructed to stand with their eyes open and their hands on their hips and to reach anteriorly with the foot as far as they could (Figure 4). They performed one 10-second trial on the uninvolved limb and then one 10-second trial on the involved limb. Participants completed the same tasks with their eyes closed and then repeated these tasks on the foam surface.
Data Processing
Limb Symmetry Index For Agility
We calculated the limb symmetry index for the 17-hop and mat-hopping tasks using the following equation36:
 |
Center-of-Pressure Average Velocity for Balance Tasks
We collected the COP average velocity via the Pressure Mat at a sampling rate of 50 Hz. The outcome measure for the eyes-open tasks was COP average velocity (cm/s), which was calculated by the path distance divided by the trial duration in seconds via the FootMat software.37
Balance Error Evaluation
Balance errors were scored by a single clinician (A.N.K.) for the balance-task trials with the participants' eyes closed. An error occurred if participants took their hands off their hips, touched down with the contralateral foot, fell, took a step, flexed or abducted the hip more than 30°, lifted the stance foot off the ground, opened their eyes, or remained out of the testing position for more than 5 consecutive seconds.
Statistical Analysis
Sample size was estimated from previous research38 in which COP path velocity was compared between participants with ACLR and control individuals. Using a minimal difference of 1.3 cm/s, a group variance of 1.48, an α level of .05, and a β level of 0.8, we estimated that we would need 21 participants per group.
Demographics were compared between groups (ACLR, control) using independent-samples t tests for continuous measures and χ2 tests for categorical variables with the α level set a priori at .05.
For all agility tasks, independent-samples t tests were used to compare measures between groups. Balance tasks were analyzed via 2 × 2 × 3 analyses of variance separately for the eyes-open and eyes-closed trials to compare the effects of group (ACLR, control) by surface (firm, foam) by position (SL straight knee, SL bent knee, SL squat). We used post hoc independent-samples t tests to measure differences between groups at each position and used 1-way analyses of variance with Tukey post hoc tests to compare positions within each group. Cohen d effect sizes and 95% confidence intervals (CIs) were calculated to assess the magnitude of differences between groups. Effect sizes were categorized as weak (<0.4), moderate (0.41–0.7), or strong (>0.7).
We conducted Pearson product moment correlation coefficients (2 tailed) for the involved-limb trials between reach distance and COP average velocity during the SL squat task to assess if postural stability was related to squat depth. Exploratory Pearson product moment correlation coefficients (2 tailed) were calculated between SL measures of agility and the Agility T Test to examine whether these assessments were measuring similar outcomes. We used paired t tests to compare reach distances on firm versus foam surfaces. All statistics were performed using SPSS (version 24; IBM Corp, Armonk, NY). The α level was set a priori at ≤.05.
RESULTS
Demographics
Demographic variables did not differ between groups for sex, age, height, mass, or activity level (Table 1). Differences between groups were observed for subjective knee function assessed via the International Knee Documentation Committee form (P < .001).
Agility
The ACLR group demonstrated slower times on the Agility T Test (t45 = 1.98, P = .05) with a large effect size (Cohen d = 0.93 [95% CI = 0.33, 1.53]). We noted no differences between groups for the involved limb or symmetry measures of the 17-hop task or the mat-hopping task and weak to moderate effect sizes (Table 2). Agility T Test times were correlated with SL agility times for the 17-hop (r = 0.574, P < .001) and mat-hopping (r = 0.70, P < .001) tasks for both groups.
Table 2.
Measures of Agility Between Groups
| Test |
Group, Mean ± SD |
t Value |
P Value |
Cohen d Effect Size (95% Confidence Interval) |
|
| Anterior Cruciate Ligament Reconstruction |
Control |
||||
| Agility T Test, s | 12.69 ± 1.84 | 11.76 ± 1.36 | 1.98 | .05 | 0.93 (0.33, 1.53) |
| 17-hop task | |||||
| Involved limb, s | 7.43 ± 1.68 | 6.91 ± 1.13 | 1.25 | .22 | 0.38 (−0.22, 0.98) |
| Limb Symmetry Index,a % | 98.50 ± 10.90 | 100.48 ± 10.80 | 0.62 | .54 | −0.14 (−0.72, 0.44) |
| Mat-hopping task | |||||
| Involved limb, s | 3.58 ± 1.49 | 3.20 ± 0.61 | 1.14 | .26 | 0.33 (−0.25, 0.91) |
| Limb Symmetry Index,a % | 103.35 ± 12.37 | 104.63 ± 13.08 | 0.34 | .73 | −0.16 (−0.73, 0.41) |
Involved limb/uninvolved limb. The involved limb was defined as the anterior cruciate ligament-reconstructed limb for the anterior cruciate ligament reconstruction group and the nondominant limb for the control group.
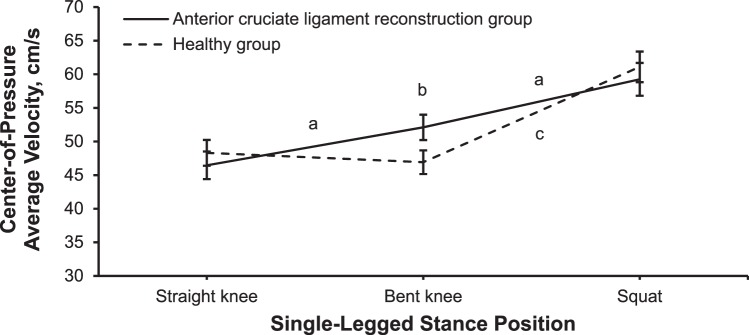
Eyes-Open Balance
We observed a position-by-group interaction for the eyes-open balance tasks (F2,86 = 3.91, P = .02; Figure 5). Regardless of surface, the ACLR group (52.11 ± 1.89 cm/s) demonstrated higher COP average velocities than the control group (46.92 ± 1.76 cm/s) for the SL bent-knee position (P = .009; Cohen d = 2.85 [95% CI = 2.03, 3.67]).
Figure 5.
Group-by-position interaction for the eyes-open single-legged balance condition collapsed across surfaces. a Difference between positions for the anterior cruciate ligament reconstruction group. b Difference between groups. c Differences between positions for the control group.
For the control group, the COP average velocity was lower in the SL bent-knee position than in the SL squat position (P < .001, Cohen d = 1.42 [95% CI = 0.79, 2.05]) but not different from the SL straight-knee position (P = .30, Cohen d = 0.16 [95% CI = −0.41, 0.72]). For the ACLR group, the COP average velocity was higher in the SL bent-knee position than in the SL straight-knee position (P = .01, Cohen d = 0.61 [95% CI = 0.01, 1.22]) and lower than in the SL squat position (P < .001, Cohen d = 0.70 [95% CI = 0.09, 1.31]).
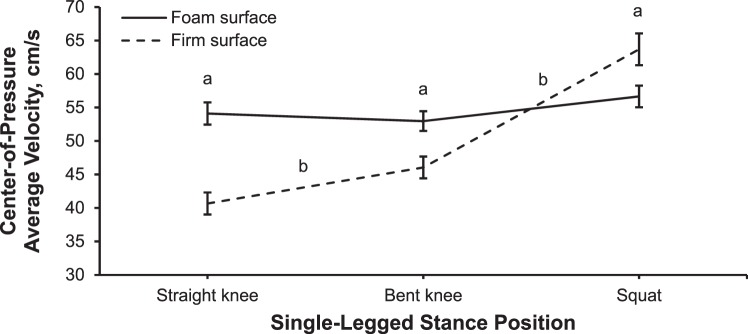
We identified a surface-by-position interaction (F2,86 = 30.11, P = .001) for the eyes-open balance tasks (Figure 6). For all participants, COP average velocities were higher while balancing on the foam compared with the firm surface in the SL straight-knee (P < .001, Cohen d = 1.20 [95% CI = 0.75, 1.64]) and SL bent-knee (P < .001, Cohen d = 0.49 [95% CI = 0.08, 0.91]) positions. During the SL squat, the COP average velocity was lower while balancing on the foam than the firm surface (P = .002, Cohen d = 0.51 [95% CI = 0.10, 0.93]).
Figure 6.
Surface-by-position interaction for the eyes-open single-legged balance condition collapsed across groups. a Difference between surfaces. b Difference between positions on a firm surface.
Regardless of group, during testing in the SL squat position, normalized reach distances were shorter while balancing on the foam than the firm surface (P < .001, Cohen d = 1.42 [95% CI = 0.79, 2.05]). Reach distances between groups were not different, with weak to moderate effect sizes on the firm (P = .08, Cohen d = 0.51 [95% CI = −0.07, 1.10]) and foam (P = .12, Cohen d = 0.40 [95% CI = −0.18, 0.98]) surfaces.
For the control group, reach distance was moderately positively correlated with COP average velocity on the firm (r = 0.59, P = .002) and foam (r = 0.518, P = .008) surfaces. For the ACLR group, reach distance was not correlated with COP average velocity on either surface.
Eyes-Closed Balance
We found a main effect for position (F2,82 = 3.51, P = .03) on the eyes-closed balance tasks. On average, all participants exhibited fewer errors in the SL bent-knee than the SL straight-knee position (P = .002, Cohen d = 0.47 [95% CI = 0.04, 0.97]). A main effect was noted for surface (F1,41 = 13.1, P < .001), with more errors while balancing on the foam than the firm surface (P < .001, Cohen d = 1.67 [95% CI = 1.18, 2.17]). No other group differences or interactions were present for the eyes-closed balance tasks.
DISCUSSION
The ACLR group exhibited slower times during agility testing and decreased SL postural control in the bent-knee position than the control group. No differences in SL balance were seen between groups when the participants were assessed in the SL straight-knee or SL squat position. A moderate correlation occurred between the performances on the Agility T Test and the mat-hopping task, and a strong correlation occurred between the performances on the Agility T Test and the 17-hop test. However, no differences in performances of the mat-hopping task or the 17-hop task were found between groups.
We selected the balance tasks to compare postural control between groups. The different conditions were selected to modify afferent feedback via different joint positions, surfaces, and visual input. When the environment was manipulated by a change in the joint position, the ACLR group demonstrated worse postural control than the control group. During every postural task, stability is maintained as the body gathers information from the visual, vestibular, and somatic senses.39 Our findings are consistent with those of researchers40,41 who suggested that, when 1 or more of these components was altered, the task could be completed but at a decreased level. In addition, all participants demonstrated worse postural stability on the foam than the firm surface in the SL straight- and bent-knee positions. This result supports the current rehabilitation literature in which investigators42 proposed the introduction of an unstable surface to increase the difficulty of the task.
Patients with ACLR have exhibited compensatory movement patterns, suggesting muscle weakness, motor asynergies, and neuromuscular deficiencies.43 We used both bilateral and unilateral limb measures of agility to test for differences in function between groups. Of the 3 agility tasks, only the Agility T Test demonstrated differences between groups. This task requires patients with ACLR to use both limbs as they accelerate and decelerate in various directions. Given the known limb asymmetries in this population,16 the Agility T Test may have exposed compensatory patterns as reflected in the group's slower times, requiring an equal number of cuts by both limbs. We did not observe differences in the unilateral measures of agility (17-hop and mat-hopping tasks). Whereas performances on the unilateral measures and the Agility T Test (designed to assess sport agility44) were correlated, the former did not seem to be sensitive enough to differentiate between participants with and those without a history of ACLR. Contrary to previous research,12 our findings may indicate that a bilateral measure of agility that incorporates changes in direction and acceleration is a more beneficial sport-specific task for assessing deficits in a population with ACLR than symmetry indexes of unilateral tasks.
Efferent response of muscle activation in response to sensory input is a critical component for maintaining postural control during functional tasks. To maintain stability, an individual must appropriately activate the stabilizing muscles. Our results indicated decreased postural control in the ACLR group but only during the SL bent-knee task. The SL bent-knee position places a greater internal moment on the quadriceps muscle group, which commonly demonstrates strength deficits after ACLR.20 However, differences were not observed in the SL squat position, which places a similarly increased demand on the quadriceps. The control group displayed worse postural stability in the SL squat than the bent-knee position (Figure 5). In this task, participants were instructed to reach out as far as they could, which may have put them on the threshold of postural instability. Whereas not statistically different, moderate effect sizes for reach distances between groups may support previous findings35 of group differences for the anterior reach. The interpersonal differences from the “reach out anteriorly as far as you can” instruction may have “washed out” group differences in postural stability. After ACL injury and ACLR, patients have presented with decreased motor control,43,45,46 which was hypothesized to result from the loss of mechanoreceptor input from the ACL and distention of the joint capsule, indicating the need for clinical proprioceptive assessments. Compared with an SL straight-knee task, the flexed-knee position may provide greater afferent input from mechanoreceptors, which increase activity with activation of the surrounding musculature.47,48 In an open kinetic chain task after ACLR, the quadriceps muscles were inhibited, with evidence to support dysfunction of the muscle spindle and γ system.49,50 The possible roles of persistent muscle weakness and altered sensory input on postural stability in individuals with ACLR are areas of future research.
Changes in visual input have also been shown to cause a deterioration in postural control.41,48 Contrary to previous investigators41 who revealed differences between participants with ACLR and healthy participants during eyes-closed tasks, we found no differences in the number of errors between groups. Although some researchers25 noted differences between participants with ACLR and healthy individuals, we used a different trial duration. They used 20-second trials, whereas we used 10-second trials to remain consistent with the eyes-open trials. During pilot testing, we determined that a 20-second trial caused touch downs of the nontest limb, which contaminated the COP average velocity output. The decrease in trial time, as well as testing the participants with a bent knee instead of a straight knee, may explain the different results.
The agility and balance tasks that we used can be implemented in clinical practice with limited equipment. The Agility T Test and the SL bent-knee balance test differentiate participants with ACLR from active, healthy individuals, which may be beneficial for clinical objective evaluation of function after ACLR.
LIMITATIONS
Our study had the following limitations. First, the 17-hop task31 and mat-hopping task32 were both novel activities that we adapted from previous reports. Second, before each SL bent-knee balance trial, all participants bent their knees to the same angle as measured by a goniometer; the angle may have changed during the 10-second trial and resulted in variable displacements of the center of mass in individuals of different heights. We used a goniometer to allow better translation of our method to clinical settings and to standardize the amount of knee flexion. Whereas we measured the depth of the SL squat to compare groups, we could not compare knee flexion during the SL squat task and the SL bent-knee condition. Flexion of the knee during a closed kinetic chain task would increase activation of the hamstrings, gluteal, and quadriceps muscles. Given our methods, we were unable to differentiate the primary muscular source of the postural deficits. We chose assessments that would be available for clinical use. Although the Balance Error Scoring System can easily be implemented in clinical practice, recording COP measures requires instrumentation that may not be available in most clinics. We also do not know if time recorded by a stopwatch would show results similar to those from the timing gates used in this study.
CONCLUSIONS
The ACLR group demonstrated slower agility times and worse postural stability in an SL bent-knee position than the control group. When evaluating patients with ACLR, clinicians may find it beneficial to include bipedal measures of agility and SL balance with the knee in a flexed position to best identify deficits.
REFERENCES
- 1.Leathers MP, Merz A, Wong J, Scott T, Wang JC, Hame SL. Trends and demographics in anterior cruciate ligament reconstruction in the United States. J Knee Surg. 2015;28(5):390–394. doi: 10.1055/s-0035-1544193. [DOI] [PubMed] [Google Scholar]
- 2.Kobayashi H, Kanamura T, Koshida S, et al. Mechanisms of the anterior cruciate ligament injury in sports activities: a twenty-year clinical research of 1700 athletes. J Sports Sci Med. 2010;9(4):669–675. [PMC free article] [PubMed] [Google Scholar]
- 3.Boden BP, Sheehan FT, Torg JS, Hewett TE. Noncontact anterior cruciate ligament injuries: mechanisms and risk factors. J Am Acad Orthop Surg. 2010;18(9):520–527. doi: 10.5435/00124635-201009000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- 5.Hart JM, Pietrosimone B, Hertel J, Ingersoll CD. Quadriceps activation following knee injuries: a systematic review. J Athl Train. 2010;45(1):87–97. doi: 10.4085/1062-6050-45.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neeter C, Gustavsson A, Thomee P, Augustsson J, Thomee R, Karlsson J. Development of a strength test battery for evaluating leg muscle power after anterior cruciate ligament injury and reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(6):571–580. doi: 10.1007/s00167-006-0040-y. [DOI] [PubMed] [Google Scholar]
- 7.Leys T, Salmon L, Waller A, Linklater J, Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012;40(3):595–605. doi: 10.1177/0363546511430375. [DOI] [PubMed] [Google Scholar]
- 8.Luc B, Gribble PA, Pietrosimone BG. Osteoarthritis prevalence following anterior cruciate ligament reconstruction: a systematic review and numbers-needed-to-treat analysis. J Athl Train. 2014;49(6):806–819. doi: 10.4085/1062-6050-49.3.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sernert N, Kartus J, Kohler K, et al. Analysis of subjective, objective and functional examination tests after anterior cruciate ligament reconstruction: a follow-up of 527 patients. Knee Surg Sports Traumatol Arthrosc. 1999;7(3):160–165. doi: 10.1007/s001670050141. [DOI] [PubMed] [Google Scholar]
- 10.Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697–1705. doi: 10.1016/j.arthro.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Munro AG, Herrington LC. Between-session reliability of four hop tests and the Agility T-test. J Strength Cond Res. 2011;25(5):1470–1477. doi: 10.1519/JSC.0b013e3181d83335. [DOI] [PubMed] [Google Scholar]
- 12.Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41(6):377–387. doi: 10.2519/jospt.2011.3547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41(6):1310–1318. doi: 10.1177/0363546513482718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 15.Sheppard JM, Young WB. Agility literature review: classifications, training and testing. J Sports Sci. 2006;24(9):919–932. doi: 10.1080/02640410500457109. [DOI] [PubMed] [Google Scholar]
- 16.Menzer H, Slater LV, Diduch D, et al. The utility of objective strength and functional performance to predict subjective outcomes after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2017;5(12):2325967117744758. doi: 10.1177/2325967117744758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Negahban H, Mazaheri M, Kingma I, van Dieen JH. A systematic review of postural control during single-leg stance in patients with untreated anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2014;22(7):1491–1504. doi: 10.1007/s00167-013-2501-4. [DOI] [PubMed] [Google Scholar]
- 18.Smith MD, Bell DR. Negative effects on postural control after anterior cruciate ligament reconstruction as measured by the Balance Error Scoring System. J Sport Rehabil. 2013;22(3):224–228. doi: 10.1123/jsr.22.3.224. [DOI] [PubMed] [Google Scholar]
- 19.Linens SW, Ross SE, Arnold BL, Gayle R, Pidcoe P. Postural-stability tests that identify individuals with chronic ankle instability. J Athl Train. 2014;49(1):15–23. doi: 10.4085/1062-6050-48.6.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mesfar W, Shirazi-Adl A. Biomechanics of the knee joint in flexion under various quadriceps forces. Knee. 2005;12(6):424–434. doi: 10.1016/j.knee.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 21.Bodkin SG, Slater LV, Norte GE, Goetschius J, Hart JM. ACL reconstructed individuals do not demonstrate deficits in postural control as measured by single-leg balance. Gait Posture. 2018;66:296–299. doi: 10.1016/j.gaitpost.2018.06.120. [DOI] [PubMed] [Google Scholar]
- 22.Bolgla LA, Shaffer SW, Malone TR. Vastus medialis activation during knee extension exercises: evidence for exercise prescription. J Sport Rehabil. 2008;17(1):1–10. doi: 10.1123/jsr.17.1.1. [DOI] [PubMed] [Google Scholar]
- 23.Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 24.Louw Q, Gillion N, van Niekerk SM, Morris L, Baumeister J. The effect of vision on knee biomechanics during functional activities: a systematic review. J Sci Med Sport. 2015;18(4):469–474. doi: 10.1016/j.jsams.2014.06.009. [DOI] [PubMed] [Google Scholar]
- 25.Mohammadi F, Salavati M, Akhbari B, Mazaheri M, Khorrami M, Negahban H. Static and dynamic postural control in competitive athletes after anterior cruciate ligament reconstruction and controls. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1603–1610. doi: 10.1007/s00167-011-1806-4. [DOI] [PubMed] [Google Scholar]
- 26.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand: quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 28.Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890–897. doi: 10.1177/0363546508330143. [DOI] [PubMed] [Google Scholar]
- 29.Wilson PM, Mack DE, Gunnell KE, et al. Assessing leisure-time physical activity in young adults with the Godin Leisure-Time Exercise Questionnaire: normative values, gender differences, and non-response error. Ann Behav Med. 2010;39(suppl 1):s188. [Google Scholar]
- 30.Higgins LD, Taylor MK, Park D, et al. Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Joint Bone Spine. 2007;74(6):594–599. doi: 10.1016/j.jbspin.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 31.Hildebrandt C, Muller L, Zisch B, Huber R, Fink C, Raschner C. Functional assessments for decision-making regarding return to sports following ACL reconstruction, part I: development of a new test battery. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1273–1281. doi: 10.1007/s00167-015-3529-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Caffrey E, Docherty CL, Schrader J, Klossner J. The ability of 4 single-limb hopping tests to detect functional performance deficits in individuals with functional ankle instability. J Orthop Sports Phys Ther. 2009;39(11):799–806. doi: 10.2519/jospt.2009.3042. [DOI] [PubMed] [Google Scholar]
- 33.Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87(3):337–349. doi: 10.2522/ptj.20060143. [DOI] [PubMed] [Google Scholar]
- 34.Broglio SP, Zhu W, Sopiarz K, Park Y. Generalizability theory analysis of Balance Error Scoring System reliability in healthy young adults. J Athl Train. 2009;44(5):497–502. doi: 10.4085/1062-6050-44.5.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Clagg S, Paterno MV, Hewett TE, Schmitt LC. Performance on the Modified Star Excursion Balance Test at the time of return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2015;45(6):444–452. doi: 10.2519/jospt.2015.5040. [DOI] [PubMed] [Google Scholar]
- 36.Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2015;47(7):1426–1434. doi: 10.1249/MSS.0000000000000560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goetschius J, Feger MA, Hertel J, Hart JM. Validating center-of-pressure balance measurements using the MatScan(R) pressure mat. J Sport Rehabil. 2018;27(1) doi: 10.1123/jsr.2017-0152. [DOI] [PubMed] [Google Scholar]
- 38.Culvenor AG, Alexander BC, Clark RA, et al. Dynamic single-leg postural control is impaired bilaterally following anterior cruciate ligament reconstruction: implications for reinjury risk. J Orthop Sports Phys Ther. 2016;46(5):357–364. doi: 10.2519/jospt.2016.6305. [DOI] [PubMed] [Google Scholar]
- 39.McCollum G, Shupert CL, Nashner LM. Organizing sensory information for postural control in altered sensory environments. J Theor Biol. 1996;180(3):257–270. doi: 10.1006/jtbi.1996.0101. [DOI] [PubMed] [Google Scholar]
- 40.Okuda K, Abe N, Katayama Y, Senda M, Kuroda T, Inoue H. Effect of vision on postural sway in anterior cruciate ligament injured knees. J Orthop Sci. 2005;10(3):277–283. doi: 10.1007/s00776-005-0893-9. [DOI] [PubMed] [Google Scholar]
- 41.Molka AZ, Lisinski P, Huber J. Visual biofeedback exercises for improving body balance control after anterior cruciate ligament reconstruction. J Phys Ther Sci. 2015;27(7):2357–2360. doi: 10.1589/jpts.27.2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bousquet BA, O'Brien L, Singleton S, Beggs M. Post-operative criterion based rehabilitation of ACL repairs: a clinical commentary. Int J Sports Phys Ther. 2018;13(2):293–305. [PMC free article] [PubMed] [Google Scholar]
- 43.Swanik CB, Lephart SM, Giannantonio FP, Fu FH. Reestablishing proprioception and neuromuscular control in the ACL-injured athlete. J Sport Rehabil. 1997;6(2):182–206. [Google Scholar]
- 44.Pauole K, Madole K, Garhammer J, Lacourse M, Rozenek R. Reliability and validity of the T-test as a measure of agility, leg power, and leg speed in college-aged men and women. J Strength Cond Res. 2000;14(4):443–450. [Google Scholar]
- 45.Limbird TJ, Shiavi R, Frazer M, Borra H. EMG profiles of knee joint musculature during walking: changes induced by anterior cruciate ligament deficiency. J Orthop Res. 1988;6(5):630–638. doi: 10.1002/jor.1100060503. [DOI] [PubMed] [Google Scholar]
- 46.Fischer-Rasmussen T, Jensen PE. Proprioceptive sensitivity and performance in anterior cruciate ligament-deficient knee joints. Scand J Med Sci Sports. 2000;10(2):85–89. doi: 10.1034/j.1600-0838.2000.010002085.x. [DOI] [PubMed] [Google Scholar]
- 47.Lephart SM, Pincivero DM, Rozzi SL. Proprioception of the ankle and knee. Sports Med. 1998;25(3):149–155. doi: 10.2165/00007256-199825030-00002. [DOI] [PubMed] [Google Scholar]
- 48.Riemann BL, Lephart SM. The sensorimotor system, part II: the role of proprioception in motor control and functional joint stability. J Athl Train. 2002;37(1):80–84. [PMC free article] [PubMed] [Google Scholar]
- 49.Konishi Y, Fukubayashi T, Takeshita D. Possible mechanism of quadriceps femoris weakness in patients with ruptured anterior cruciate ligament. Med Sci Sports Exerc. 2002;34(9):1414–1418. doi: 10.1097/00005768-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 50.Konishi Y, Aihara Y, Sakai M, Ogawa G, Fukubayashi T. Gamma loop dysfunction in the quadriceps femoris of patients who underwent anterior cruciate ligament reconstruction remains bilaterally. Scand J Med Sci Sports. 2007;17(4):393–399. doi: 10.1111/j.1600-0838.2006.00573.x. [DOI] [PubMed] [Google Scholar]