Abstract
Context
Hopping exercises are recommended as a functional training tool to prevent lower limb injury, but their effects on lower extremity biomechanics in those with chronic ankle instability (CAI) are unclear.
Objective
To determine if jump-landing biomechanics change after a hop-stabilization intervention.
Design
Randomized controlled clinical trial.
Setting
Research laboratory.
Patients or Other Participants
Twenty-eight male collegiate basketball players with CAI were divided into 2 groups: hop-training group (age = 22.78 ± 3.09 years, mass = 82.59 ± 9.51 kg, height = 187.96 ± 7.93 cm) and control group (age = 22.57 ± 2.76 years, mass = 78.35 ± 7.02 kg, height = 185.69 ± 7.28 cm).
Intervention(s)
A 6-week supervised hop-stabilization training program that consisted of 18 training sessions.
Main Outcome Measure(s)
Lower extremity kinetics and kinematics during a jump-landing task and self-reported function were assessed before and after the 6-week training program.
Results
The hop-stabilization program resulted in improved self-reported function (P < .05), larger sagittal-plane hip- and knee-flexion angles, and greater ankle dorsiflexion (P < .05) relative to the control group. Reduced frontal-plane joint angles at the hip, knee, and ankle as well as decreased ground reaction forces and a longer time to peak ground reaction forces were observed in the hopping group compared with the control group after the intervention (P < .05).
Conclusions
The 6-week hop-stabilization training program altered jump-landing biomechanics in male collegiate basketball players with CAI. These results may provide a potential mechanistic explanation for improvements in patient-reported outcomes and reductions in injury risk after ankle-sprain rehabilitation programs that incorporate hop-stabilization exercises.
Keywords: hopping training, kinetics, kinematics, ankle injuries
Key Points
A 6-week hop-stabilization program resulted in improved jump-landing biomechanics of the ankle, knee, and hip in patients with chronic ankle instability.
A 6-week hop-stabilization program resulted in decreased ground reaction forces during a single-limb jump landing in patients with chronic ankle instability.
Ankle sprains are the most common injuries in collegiate athletes and represent a significant contribution to time lost from sports participation.1 Approximately 11 000 ankle sprains occur per year in US collegiate athletes, and ankle-ligament sprains were most frequent in men's basketball players.1 Unfortunately, ankle sprains are not a 1-time injury, and a common sequela is the development of chronic ankle instability (CAI), a condition characterized by recurrent sprains or repetitive giving way (or both) of the ankle.2 Approximately 40% of people who sustain a lateral ankle sprain will experience a recurrent sprain and residual symptoms, such as pain and instability that last for at least 12 months.3 Further, a link between CAI and posttraumatic ankle osteoarthritis has been established and is thought to be due, at least in part, to aberrant biomechanics.4
In addition to recurrent sprains and giving-way episodes, CAI is associated with a variety of sensorimotor adaptations, including biomechanical alterations. Individuals with CAI land in a more plantar-flexed5 and inverted position.6,7 Kinematic alterations have been identified proximal to the ankle joint during dynamic tasks.8,9 Altered kinetics, including greater ground reaction forces and loading rates, have also been observed in individuals with CAI during a landing task.10 These alterations are hypothesized to potentially increase an individual's risk for recurrent injury and ankle-joint degeneration.
A number of therapeutic interventions have been used to treat CAI-associated impairments. Balance training, a common intervention, was effective in improving postural control11 but only influenced some biomechanical outcomes in individuals with CAI.12 Hop-stabilization exercises represent a dynamic and fundamental movement in a variety of sports.13 Training programs that emphasize hop stabilization enhance function and postural control in individuals with CAI.14,15 In addition, plyometric-training programs that included a variety of hopping exercises improved lower extremity biomechanics in healthy control participants.16 Despite this evidence, it remains unclear how a hop-stabilization intervention would affect lower extremity jump-landing biomechanics in individuals with CAI.
Therefore, the purpose of our study was to determine the effects of a 6-week hop-stabilization training program on lower extremity jump-landing biomechanics (ie, kinematics and kinetics) in male collegiate basketball players with CAI. Based on the literature, we hypothesized that the hop-stabilization program would improve lower extremity jump-landing biomechanics relative to a control condition.
METHODS
Study Design
This investigation was part of a larger single-blinded randomized controlled trial.17 Participants were randomly assigned to either an experimental group (hopping program) or a control group. Using G*Power software (version 3.1.9.2; Kiel, Germany) and previous research,18 we estimated that 12 participants per group were needed to detect statistical significance at an α level of .05, 95% power, and an effect size of 0.79. All participants were enrolled, trained, and tested at a single site after reading and signing the informed consent form that was approved by the University of Tehran Institutional Review Board, which also approved the study.
Participants
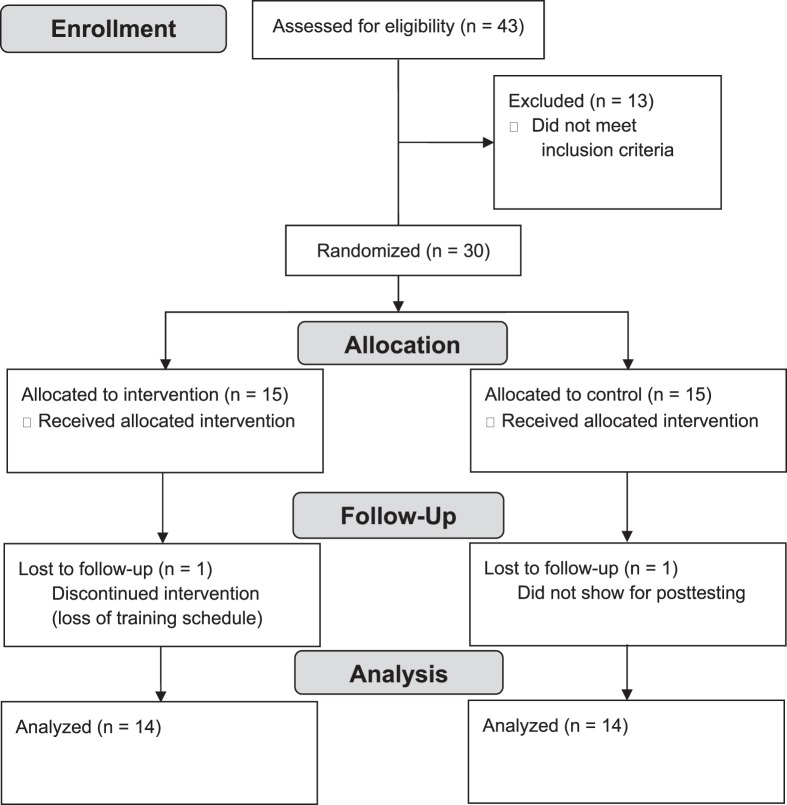
A total of 43 male collegiate basketball players expressed interest in participating. However, 13 failed to meet the CAI-specific inclusion criteria, as shown in the CONSORT diagram (Figure). Thus, 30 university male basketball players with CAI were enrolled, but 2 withdrew. The remaining 28 participants (14 per group) completed the investigation and were randomized to either the experimental group (age = 22.78 ± 3.09 years, mass = 82.59 ± 9.51 kg, height = 187.96 ± 7.93 cm, missed days of desired physical activity due to ankle injury = 10.5 ± 6.08) or control group (age = 22.57 ± 2.76 years, mass = 78.35 ± 7.02 kg, height = 185.69 ± 7.28 cm, missed days of desired physical activity due to ankle injury = 10.21 ± 5.60). Only men were enrolled in this investigation because of a lack of women's teams at this competition level in Iran and cultural constraints. All participants were required to be between 18 and 30 years of age, playing basketball at the university level, and actively practicing during the off-season at least 3 times per week for 2 hours per session. Chronic ankle instability-specific criteria were consistent with the recommendations of the International Ankle Consortium.2 Specifically, participants were required to have (1) at least 1 acute ankle-inversion sprain that resulted in swelling, pain, and dysfunction that occurred at least 12 months before the study (experimental group: 16.35 ± 3.70 months, control group: 17.21 ± 3.68 months); (2) at least 2 episodes of the ankle “giving way” within the past 6 months (experimental group: 6.14 ± 4.32, control group: 6.5 ± 3.77); (3) answered 4 or more questions with yes on the Ankle Instability Instrument; (4) a disability score of ≤90% on the Foot and Ankle Ability Measure (FAAM); and (5) a disability score ≤80% on the FAAM–Sport (FAAM-S). Additionally, CAI participants were required to score <75% in 3 or more categories on the Foot and Ankle Outcome Score, score <24 on the Cumberland Ankle Instability Tool, and have clinically negative anterior drawer and talar tilt tests. Ligamentous assessments were performed by a physical therapist with more than 10 years' experience. For those with bilateral ankle sprains, the ankle with the lowest self-reported questionnaire scores was selected. Exclusion criteria were neurologic or vision problems, any surgery to the musculoskeletal structures, or chronic musculoskeletal, severe acute lower extremity, or head injury.2
Figure.
CONSORT flow chart of participant enrollment, allocation, follow up, and analysis.
Procedures
Upon enrollment, participants completed the baseline jump-landing protocol. Reflective markers were placed using the modified Helen Hayes marker set, which consisted of the left and right anterior-superior iliac spine, midthigh, lateral knee, midshank, lateral malleolus, calcaneus, foot between the second and third metatarsal heads, and sacrum. Before completing the baseline assessment, participants were allowed to practice the jump-landing task. They were asked to stand on a 40-cm box adjacent to a 40- × 60-cm force platform (Advanced Medical Technologies Inc, Watertown, MA). Participants were then instructed to stand on the test limb and drop forward onto the force plate, where they were required to maintain the single-limb landing for 3 seconds. No constraints were placed on trunk or upper extremity placement or movement during the task. Three successful trials were recorded, and jump-landing attempts were separated by 60 seconds of rest.5,10 A successful trial was defined as the participant contacting the force plate cleanly without any loss of balance or any corrections after initial contact (eg, double hop, shifting, or sliding the stance limb). Kinetic data, collected at 2000 Hz, were synchronized with 6 infrared cameras (model Eagle; Motion Analysis Corporation, Santa Rosa, CA) that collected kinematic data at 200 Hz via Cortex software (version 5.5.0.1579; Motion Analysis Corporation). Both kinetic and kinematic data were filtered using a low-pass, zero lag, fourth-order Butterworth filter with a 12-Hz cutoff frequency. A global axis system was used based on a right-hand convention: positive kinematic values represented dorsiflexion, inversion, foot adduction, knee flexion, varus, internal rotation, hip extension adduction, and internal rotation.
Cortex software was used to ensure marker identification throughout the trial, and a custom MATLAB program (The MathWorks, Natick, MA) was used to complete data processing. The kinematic angles of interest were the hip, knee, and ankle joints in all 3 planes. These variables were extracted at initial contact and peak vertical ground reaction force. Initial contact was identified as the point when the vertical ground reaction force exceeded 10 N. Peak ground reaction force and time to peak force in the vertical, anterior, posterior, medial, and lateral directions were extracted and normalized to body weight (N). The loading rate, calculated as normalized peak vertical ground reaction force divided by the time to reach peak force, was calculated based on the following equation: loading rate = ({Peak Force [N]/Body Weight [N]}/Time to Peak Force [millisecond]). Three trial averages for all outcomes were used for further analysis. After baseline testing, participants were randomized to either the experimental or control group using a computer-generated table of random numbers and immediately started their assigned intervention. The posttest assessment was completed within 48 hours of the final training session. An independent assessor who was blinded to group assignment completed the baseline and posttest assessments on all participants. All testing took place in the biomechanics laboratory of the Sport Science Research Institute of Iran.
Intervention
Three supervised sessions occurred per week for 6 weeks (Table 1),17 and training volume increased during the program. Both M.K.A. and H.M. supervised all training sessions. Hopping exercises consisted of hopping side to side, hopping forward and backward, hopping forward,14 hopping in a figure 8,19 hopping in a zigzag pattern, and hopping in a 4-square shape.13 Briefly, the figure-8 hop involved hopping in a pattern that was 2 m in length. Side-to-side hopping required participants to hop back and forth laterally over a distance of 30 cm. Forward-and-backward hoping required the participant to hop back and forth sagittally over a 30-cm distance. Forward hops required the participant to hop forward 91.44 cm, stabilize, and hop the same distance again. The zigzag pattern required participants to hop diagonally in a zigzag pattern (45-cm wide) outlined on the floor with tape. They were instructed to hop diagonally over the 15-cm-wide line, alternating sides. The 4-square hop required participants to hop within each of the four 40- × 40-cm squares drawn on the floor. With the right limb, they hopped in a clockwise direction, and with the left limb, they hopped in a counterclockwise direction. All exercises were performed shod throughout the training program. Further descriptions of the exercises and the training specifications per week are provided in Table 1. Before each session, a standardized warmup consisting of 5 minutes of free running and 5 minutes of dynamic stretching was completed.13,14
Table 1.
Hop-Training Program
| Week |
Volume (Foot Contacts per Session, No.) |
Hopping Exercise |
Session Information |
Set × Repetitions |
| 1 | 80 | Hopping side to side on both legs | 1: Hands free 2: Arms across the chest 3: Hands behind head |
2 × 10 |
| Hopping forward and backward on both legs | 1: Hands free 2: Arms across the chest 3: Hands behind head |
2 × 10 | ||
| Hopping forward on both legs | 1: Hands free 2: Arms across the chest 3: Hands behind head |
2 × 10 | ||
| Hopping in figure-8 shape on both legs | 1: Hands free 2: Arms across the chest 3: Hands behind head |
2 × 10 | ||
| 2 | 100 | Hopping side to side on 1 leg | All: Hands free | 2 × 10 |
| Hopping forward and backward on 1 leg | All: Hands free | 2 × 10 | ||
| Hopping forward on 1 leg | All: Hands free | 2 × 10 | ||
| Hopping in figure-8 shape on 1 leg | All: Hands free | 2 × 10 | ||
| Hopping in zigzag shape on both legs | 1: Hands free 2: Arms across the chest 3: Hands behind head |
2 × 10 | ||
| 3 | 120 | Hopping side to side with 1 leg | All: Arms across the chest | 2 × 10 |
| Hopping forward and backward on 1 leg | All: Arms across the chest | 2 × 10 | ||
| Hopping forward on 1 leg | All: Arms across the chest | 2 × 10 | ||
| Hopping in figure-8 shape on 1 leg | All: Arms across the chest | 2 × 10 | ||
| Hopping in zigzag shape on 1 leg | All: Hands free | 2 × 10 | ||
| Hopping in 4-square shape on both legs | 1: Hands free 2: Arms across the chest 3: Hands behind head |
2 × 10 | ||
| 4 | 140 | Hopping side to side on 1 leg | All: Hands behind head | 3 × 10 |
| Hopping forward and backward on 1 leg | All: Hands behind head | 3 × 10 | ||
| Hopping forward on 1 leg | All: Hands behind head | 2 × 10 | ||
| Hopping in figure-8 shape on 1 leg | All: Hands behind head | 2 × 10 | ||
| Hopping in zigzag shape on 1 leg | All: Arms across the chest | 2 × 10 | ||
| Hopping in 4-square shape on 1 leg | All: Hands free | 2 × 10 | ||
| 5 | 160 | Hopping side to side on 1 leg | All: Hands behind head | 3 × 10 |
| Hopping forward and backward on 1 leg | All: Hands behind head | 3 × 10 | ||
| Hopping forward on 1 leg | All: Hands behind head | 3 × 10 | ||
| Hopping in figure-8 shape on 1 leg | All: Hands behind head | 3 × 10 | ||
| Hopping in zigzag shape on 1 leg | All: Hands behind head | 2 × 10 | ||
| Hopping in 4-square shape on 1 leg | All: Arms across the chest | 2 × 10 | ||
| 6 | 150 | Hopping side to side on 1 leg | All: Hands behind head | 3 × 10 |
| Hopping forward and backward on 1 leg | All: Hands behind head | 3 × 10 | ||
| Hopping forward on 1 leg | All: Hands behind head | 3 × 10 | ||
| Hopping in figure-8 shape on 1 leg | All: Hands behind head | 2 × 10 | ||
| Hopping in zigzag shape on 1 leg | All: Hands behind head | 2 × 10 | ||
| Hopping in 4-square shape on 1 leg | All: Hands behind head | 2 × 10 |
The total volume of landings started at 80 per session during the first week and increased by 20 for weeks 2 through 5. During the final week, the training volume was reduced slightly (from 160 to 150) to minimize the chance of fatigue on posttest assessments. During the first 3 weeks, participants were instructed to focus on stabilizing and landing with proper form.20 Proper form was determined by M.K.A. and H.M. and was defined as the participant (1) keeping his knees over his toes, (2) landing with flexed knees, (3) avoiding an erect posture while landing, and (4) landing with his feet shoulder-width apart. During the final 3 weeks, all exercises were performed at a speed of 2 Hz, using a metronome, in an effort to better replicate sport (ie, land, stabilize, and immediately repeat). Program difficulty was also enhanced during the study by increasing the number of exercises, constraining hand position, and transitioning from double-limb to single-limb landings (Table 1). More specifically, during the first week an exercise was introduced, it was performed with a double-limb landing. In all subsequent weeks, an exercise was completed with a single-limb landing.21 The support surface for the exercises changed during each session of a training week. Throughout the program, the exercises of the first, second, and third sessions of the week were performed on a firm surface, an artificial turf surface, and an unstable surface, respectively.14,16 Participants rested for 30 seconds between sets and for 1 minute between exercises. All exercises were performed in front of a mirror so that immediate visual feedback was available to all participants.20 Immediate oral feedback was also provided throughout the training program as needed (ie, when errors were noted). Oral feedback focused on decreasing knee valgus, landing softly, avoiding an erect posture while landing, and maintaining the proper alignment and position of the feet.20
Statistical Analysis
Demographic characteristics as well as baseline kinematic and kinetic variables were compared between groups using independent-samples t tests. Separate group × time repeated-measures multivariate analyses of variance were conducted to determine the effect of the hopping intervention on the kinematics at initial contact and at peak vertical ground reaction force and the kinetics. We calculated post hoc t tests to analyze changes between groups. Data were analyzed using SPSS (version 19.0; IBM Corp, Armonk, NY), and an a priori α level of .05 was set to determine statistical significance. The Hedges' g pretest-to-posttest between-groups effect sizes were also calculated and interpreted as small (<0.4), moderate (0.41–0.7), or large (>0.71) effects.
RESULTS
Demographic characteristics did not differ between groups (P > .05). At baseline, none of the dependent variables differed between groups (P > .05). The hopping intervention resulted in improvements in all self-reported questionnaires relative to the control condition (P < .05). Large effect sizes and 95% confidence intervals (CIs) were noted for all questionnaires and scales except for the Activities of Daily Living subscale of the Foot and Ankle Outcome Score. Means, standard deviations, and effect sizes for the self-reported questionnaires can be seen in Table 2.
Table 2.
Effect of Hop-Stabilization Training on Self-Reported Function Questionnaire
| Questionnaire |
Group, Mean ± SD |
Effect Size (95% Confidence Interval)c |
|||
| Experimental (n = 14) |
Control (n = 14) |
||||
| Pretest |
Posttest |
Pretest |
Posttest |
||
| Foot and Ankle Ability Measure, %a | 84.5 ± 4.3 | 92.4 ± 10.1b | 81.7 ± 6.2 | 81.6 ± 6.4 | 1.95 (1.03, 2.86) |
| Foot and Ankle Ability Measure-Sport, %a | 73.6 ± 10.7 | 89.2 ± 14.2b | 67.6 ± 9.3 | 70.7 ± 13.1 | 1.35 (0.51, 2.18) |
| Cumberland Ankle Instability Tool, scorea | 19.7 ± 3.7 | 24.0 ± 4.6b | 19.3 ± 3.2 | 20.0 ± 3.8 | 1.07 (0.26, 1.87) |
| Foot and Ankle Outcome Score, % | |||||
| Symptoma | 67.8 ± 12.8 | 82.6 ± 17.3b | 67.3 ± 10.9 | 68.1 ± 10.6 | 1.40 (0.56, 2.24) |
| Paina | 73.6 ± 10.2 | 89.0 ± 17.1b | 71.0 ± 13.8 | 78.3 ± 14.4 | 0.98 (0.18, 1.78) |
| Activities of Daily Living | 80.1 ± 3.7 | 84.5 ± 5.4b | 78.3 ± 5.4 | 79.3 ± 3.9 | 0.52 (−0.24, 1.29) |
| Sporta | 70.7 ± 6.4 | 95.2 ± 3.6b | 72.5 ± 6.7 | 71.8 ± 6.7 | 3.47 (2.27, 4.66) |
| Quality of Lifea | 71.4 ± 10.8 | 89.2 ± 20.4b | 71.8 ± 10.3 | 70.7 ± 9.3 | 1.19 (0.37, 2.00) |
Significant interaction (P < .05).
Difference between the pretest-to-posttest change of the experimental group relative to the control group (P < .05).
Hedges' g pretest-to-posttest between-groups effect size.
Compared with the control condition, the hop-stabilization intervention also resulted in changes in ankle, knee, and hip kinematics (P < .05; Table 3) and kinetics (P < .05; Table 4). All but 2 kinematic variables demonstrated large effect sizes with 95% CIs that did not cross zero. In general, more sagittal-plane flexion at all joints and less frontal-plane deviation at all joints were observed after the hopping intervention. All but 1 of the kinetic variables demonstrated a large effect size and 95% CIs that did not cross zero. The observed changes highlighted reductions in peak force and loading rate with a corresponding increase in the time to peak force.
Table 3.
Effect of Hop-Stabilization Training on Kinematic Variables of the Ankle, Knee, and Hip (°)
| Joint |
Kinematic Variable |
Group, Mean ± SD |
Effect Size (95% Confidence Interval)c |
|||
| Experimental (n = 14) |
Control (n = 14) |
|||||
| Pretest |
Posttest |
Pretest |
Posttest |
|||
| Ankle | Dorsiflexion-plantar flexion | |||||
| ICa | −41.89 ± 7.71 | −33.35 ± 7.43b | −42.14 ± 6.95 | −41.67 ± 6.14 | −1.89 (−2.77, −0.99) | |
| Peak VGRFa | −14.34 ± 6.44 | −9.11 ± 7.42b | −14.40 ± 5.07 | −14.42 ± 5.17 | −1.26 (−2.07, −0.44) | |
| Inversion-eversion | ||||||
| ICa | 2.90 ± 0.90 | 2.05 ± 0.97b | 2.93 ± 0.70 | 2.86 ± 0.95 | −0.97 (−1.75, −0.18) | |
| Peak VGRFa | 1.88 ± 0.90 | 0.90 ± 0.90b | 1.92 ± 0.70 | 1.87 ± 0.66 | −3.62 (−4.82, −2.41) | |
| Abduction-adduction | ||||||
| ICa | 3.13 ± 0.87 | 2.34 ± 0.80b | 3.05 ± 0.95 | 3.07 ± 0.96 | −0.66 (−1.42, 0.10) | |
| Peak VGRFa | 1.45 ± 0.87 | 0.76 ± 0.87b | 1.58 ± 0.95 | 1.63 ± 0.99 | −5.81 (−7.50, −4.11) | |
| Knee | Flexion-extension | |||||
| ICa | 6.24 ± 3.18 | 13.10 ± 3.19b | 5.55 ± 2.84 | 5.65 ± 2.64 | 1.53 (0.68, 2.37) | |
| Peak VGRFa | 20.68 ± 5.77 | 28.01 ± 4.09b | 20.40 ± 5.95 | 20.64 ± 6.02 | 1.64 (0.78, 2.49) | |
| Varus-valgus | ||||||
| ICa | −2.93 ± 1.29 | −2.07 ± 1.39b | −3.30 ± 1.54 | −3.30 ± 1.56 | −0.88 (−1.65, −0.10) | |
| Peak VGRFa | −4.19 ± 3.19 | −3.00 ± 1.89b | −4.81 ± 2.72 | −4.74 ± 2.42 | −0.69 (−1.45, 0.07) | |
| Internal-external rotation | ||||||
| ICa | 2.94 ± 1.09 | 1.60 ± 1.24b | 3.38 ± 1.89 | 3.49 ± 1.71 | −1.19 (−1.99, −0.38) | |
| Peak VGRFa | 6.79 ± 2.42 | 4.25 ± 2.36b | 7.61 ± 2.82 | 7.36 ± 3.02 | −1.47 (−2.30, −0.63) | |
| Hip | Flexion-extension | |||||
| ICa | 20.39 ± 5.28 | 28.75 ± 5.03b | 20.45 ± 5.40 | 20.75 ± 5.41 | 1.85 (0.96, 2.74) | |
| Peak VGRFa | 27.00 ± 8.44 | 35.23 ± 6.62b | 26.46 ± 8.18 | 26.70 ± 8.03 | 1.40 (0.57, 2.22) | |
| Abduction-adduction | ||||||
| ICa | −10.52 ± 4.24 | −8.39 ± 2.94b | −11.80 ± 4.85 | −11.94 ± 5.02 | −1.07 (−1.85, −0.27) | |
| Peak VGRFa | −11.12 ± 4.02 | −9.17 ± 3.82b | −13.46 ± 4.77 | −13.36 ± 4.68 | −1.01 (−1.79, −0.22) | |
| Internal-external rotation | ||||||
| ICa | −11.31 ± 1.43 | −9.24 ± 1.70b | −10.68 ± 1.23 | −10.66 ± 1.19 | −1.30 (−2.11, −0.48) | |
| Peak VGRFa | −12.26 ± 1.60 | −10.68 ± 1.97b | −12.03 ± 1.51 | −12.03 ± 1.34 | −1.05 (−1.84, −0.25) | |
Abbreviations: IC, initial contact; VGRF, vertical ground reaction force.
Significant interaction (P < .05).
Difference between the pretest-to-posttest change of the experimental group relative to the control group (P < .05).
Hedges' g pretest-to-posttest between-groups effect size. Positive kinematic values represented dorsiflexion, inversion, foot adduction, knee flexion, varus, internal rotation, hip extension adduction, and internal rotation.
Table 4.
Effect of Hop-Stabilization Training on Peak Ground Reaction Forces (Peak [%Body Weight]), Time to Peak Ground Reaction Force (TTP [ms]), and Vertical Loading Rates ([N/BW]/s) Between Groups
| Direction |
Kinetic Variable |
Group, Mean ± SD |
Effect Size (95% Confidence Interval)c |
|||
| Experimental (n = 14) |
Control (n = 14) |
|||||
| Pretest |
Posttest |
Pretest |
Posttest |
|||
| Medial | Peaka | 0.16 ± 0.02 | 0.13 ± 0.02b | 0.16 ± 0.03 | 0.16 ± 0.03 | −0.85 (−1.62, −0.07) |
| TTPa | 52.75 ± 1.29 | 56.57 ± 2.13b | 52.85 ± 1.54 | 52.50 ± 1.68 | 1.49 (0.64, 2.32) | |
| Lateral | Peaka | 0.27 ± 0.06 | 0.21 ± 0.05b | 0.27 ± 0.07 | 0.27 ± 0.07 | −1.12 (−1.91, −0.32) |
| TTPa | 46.69 ± 2.32 | 52.12 ± 4.59b | 46.75 ± 2.55 | 46.96 ± 3.27 | 1.29 (0.47, 2.09) | |
| Posterior | Peaka | 0.77 ± 0.09 | 0.68 ± 0.09b | 0.76 ± 0.09 | 0.76 ± 0.099 | −1.07 (−1.86, −0.27) |
| TTPa | 53.99 ± 4.62 | 59.17 ± 5.78b | 54.53 ± 4.91 | 54.84 ± 4.86 | 0.99 (0.20, 1.77) | |
| Anterior | Peaka | 0.06 ± 0.04 | 0.04 ± 0.03b | 0.10 ± 0.11 | 0.11 ± 0.11 | −1.26 (−2.07, −0.45) |
| TTP | 51.17 ± 3.28 | 54.90 ± 4.17b | 51.78 ± 3.11 | 51.86 ± 3.47 | 0.98 (0.29, 1.76) | |
| Vertical | Peaka | 3.81 ± 0.54 | 3.33 ± 0.68b | 3.89 ± 0.57 | 3.85 ± 0.62 | −0.79 (−1.55, −0.01) |
| TTPa | 58.18 ± 1.64 | 64.06 ± 3.28b | 58.66 ± 1.96 | 59.09 ± 3.52 | 1.14 (0.34, 1.93) | |
| Vertical loading rate | 0.12 ± 0.23 | 0.05 ± 0.008b | 0.06 ± 0.009 | 0.06 ± 0.01 | −0.29 (−1.03, 0.45) | |
Significant interaction (P < .05).
Difference between the pretest-to-posttest change of the experimental group relative to the control group (P < .05).
Hedges' g pretest-to-posttest between-groups effect size.
DISCUSSION
The purpose of our study was to determine the effects of a 6-week hop-stabilization training program on lower extremity jump-landing biomechanics (ie, kinematics and kinetics) in men's collegiate basketball players with CAI. Six weeks of hop-stabilization training altered lower extremity jump-landing biomechanics and improved self-reported function. These results support our a priori hypothesis.
Like other interventions, the current 6-week hopping program improved self-reported function in those with CAI. For example, improvements were noted after 4-week interventions that included hop-stabilization exercises.14,15,19 Additionally, the magnitude of the improvements we found were consistent with, if not larger than, those reported previously. The magnitudes of improvement on the FAAM and FAAM-S were also larger than previously established22 minimal clinically important difference scores (8% and 9%, respectively) for these questionnaires in patients with CAI. For example, earlier researchers19 noted an average Foot and Ankle Disability Index Sport change score of 11%, whereas our mean change score for the FAAM-S was 15%. It is possible that the greater volume of hop stabilizations performed in the current investigation or the longer duration of the intervention (6 versus 4 weeks) or both were responsible for the larger improvements, but future investigation is needed to confirm this hypothesis.
Plyometric and hop-stabilization training have been shown to positively influence the biomechanical profile (ie, reduce the magnitude of known lower extremity biomechanical injury risk factors) in healthy control participants16 and anterior cruciate ligament (ACL)-injured individuals.23 More specifically, the evidence shows hop-stabilization training reduced ground reaction forces, increased hip- and knee-flexion angles, and reduced knee valgus and varus torque. Interventions that focus on or include hop-stabilization exercises in CAI patients18,24 have also demonstrated biomechanical changes: increases in sagittal-plane kinematics (eg, hip- and knee-flexion angles, ankle dorsiflexion) occurred concurrently with reductions in frontal (eg, ankle inversion)- and transverse-plane (eg, hip internal rotation) motion.25 Increased dorsiflexion at initial foot contact decreased peak passive inversion moments as well as peak inversion joint angles,26 further highlighting how increasing sagittal-plane–flexion angles corresponds with reductions in frontal-plane motion.
Our observed kinematic changes in this investigation are consistent with findings in the literature. For example, reductions in ankle inversion, plantar flexion, and knee valgus were noted. Concurrently, increases in hip and knee flexion were observed. Given that these changes are associated with reductions in lower extremity joint injury risk factors and improvements in self-reported function, we speculate that they represent improvements in jump-landing kinematics. However, future research is needed to determine both the midterm and long-term positive and possible negative effects of altering jump-landing kinematics in those with CAI. It is also important to note that a link between a history of a lateral ankle sprain and an increased risk for ACL injury has been established.27 The kinematic changes in our study (eg, increased knee and hip flexion and decreased knee valgus and ground reaction forces) are associated with a decreased risk of ACL injury, so hop-stabilization training may also have the potential to decrease the risk of ACL injury in those with a history of ankle sprains. However, prospective studies of injury rates are needed to test this hypothesis.
Kinetically, those with CAI have been reported to have a higher magnitude of and quicker time to peak ground reaction force.10 Our results, illustrating a reduction in ground reaction forces and a slower time to peak force after the hop-stabilization exercises, is consistent with previous research in CAI patients28 and those with ACL injury.23 This finding is not surprising given the known relationship between a reduction in ground reaction force magnitude and concurrent increases in hip and knee flexion during landing23 and the fact that hip and knee flexion increased in our participants. As peak impact forces occur <30 to 50 milliseconds after initial contact, reductions in ground reaction force are likely the result of increased preparatory muscle activity. From the larger randomized controlled trial, we were able to illustrate that the hop-stabilization program also resulted in earlier onset times and greater preparatory muscle activity in the peroneus longus, lateral hamstrings, tibialis anterior, and gluteus medius.17 Thus, the cumulative results of our larger randomized controlled trial confirm the effectiveness of hop-stabilization training (ie, improved self-reported function) while highlighting plausible neurobiomechanical mechanisms underlying this effectiveness, at least in part.
Although evaluating effectiveness and providing insights into the underlying mechanisms are important, the motor-learning principles used in the current and previous intervention programs that resulted in observed changes are the most pertinent to clinical practice. Those with CAI have a more constrained sensorimotor system due to numerous sensory and motor impairments. These impairments decrease the adaptability for coordinating movements during changing task and environmental demands, resulting in a continuum of disability.29 Research11,14,15,17 has consistently shown that coordination training improved a variety of outcomes in those with CAI.
Maximizing the benefits of such interventions requires that the patient understand the movement goal (ie, how a task should be completed) and the purposeful manipulation of task and environmental demands as he or she progresses through the rehabilitation program. For example, to progress in a hop-training program, the task demands should be increased from simple to more complex (ie, double to single limb) and the environmental cues progressed from predictable to more unpredictable (ie, stable surface to unstable surface). Both task and environmental demands should be progressed in the context of sport-specific demands as the patient demonstrates movement proficiency (ie, achieves the movement goal) at each level. Such a progression is clinically important because the ability to perform a task in a controlled laboratory or rehabilitation environment may not translate to the field of play, where additional dynamic challenges, such as reacting to player and ball movement and adjusting for player-to-player contact occur.
We, like other investigators, chose to incorporate external visual and verbal feedback for 2 reasons. First, even if patients know what the movement goal is, it can be difficult for them to identify important movement errors from inherent feedback alone (eg, somatosensory input). Second, external feedback has been shown to positively influence movement patterns.30 Thus, incorporating external and inherent feedback may allow the patient to better triangulate when a movement error was made (ie, felt, saw, and told) and subsequently enhance the ability to learn better movement patterns. Thus, clinicians should (1) develop purposeful progressions of their chosen exercises to enhance adaptability and (2) provide external feedback to contextualize the errors. Most importantly, training volume must be high enough to ensure that the observed changes are learned (ie, permanent) and not just a transient practice effect.
Limitations
This study, like others, is not without limitations. For example, only male university basketball players were included, which may limit the generalizability of the results to different playing levels, different sports, and female athletes. Currently, no data suggest that CAI-associated impairments or responses to rehabilitation differ among these factors, but we have no data to indicate that they are equivocal. Our study design did not allow us to conclude that the hopping exercises were better or worse than other intervention programs as comparative effectiveness was not established. Finally, we quantified only the immediate effects of the intervention on a task (jump landing) that was similar to the training exercises (hopping). Thus, the retention of the program remains unknown, and it is unclear if the hop-stabilization program would cause improvements in a broader range of tasks and assessments such as cutting or jumping. Finally, the ability of the hopping training to limit recurrent injury is also unknown.
CONCLUSIONS
A 6-week hop-stabilization program changed jump-landing biomechanics (kinematics and kinetics) in male university basketball players with CAI. This program also resulted in improvements in multiple patient-reported outcomes. Landing from a jump is a frequent demand in basketball and a common mechanism for ankle sprains in basketball players. The current hop-stabilization program is an effective and reasonably sport-specific program that may reduce the lower extremity injury risk in this population.
ACKNOWLEDGMENTS
We thank the athletes who participated and the research assistants who were instrumental in the collection of the data.
REFERENCES
- 1.Roos KG, Kerr ZY, Mauntel TC, Djoko A, Dompier TP, Wikstrom EA. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. Am J Sports Med. 2017;45(1):201–209. doi: 10.1177/0363546516660980. [DOI] [PubMed] [Google Scholar]
- 2.Gribble PA, Delahunt E, Bleakley C, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. Br J Sports Med. 2014;48(13):1014–1018. doi: 10.1136/bjsports-2013-093175. [DOI] [PubMed] [Google Scholar]
- 3.Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123–140. doi: 10.1007/s40279-013-0102-5. [DOI] [PubMed] [Google Scholar]
- 4.Golditz T, Welsch GH, Pachowsky M, Hennig FF, Pfeifer K, Steib S. A multimodal approach to ankle instability: interrelations between subjective and objective assessments of ankle status in athletes. J Orthop Res. 2016;34(3):525–532. doi: 10.1002/jor.23039. [DOI] [PubMed] [Google Scholar]
- 5.Caulfield B, Garrett M. Functional instability of the ankle: differences in patterns of ankle and knee movement prior to and post landing in a single leg jump. Int J Sports Med. 2002;23(1):64–68. doi: 10.1055/s-2002-19272. [DOI] [PubMed] [Google Scholar]
- 6.Lin CF, Chen CY, Lin CW. Dynamic ankle control in athletes with ankle instability during sports maneuvers. Am J Sports Med. 2011;39(9):2007–2015. doi: 10.1177/0363546511406868. [DOI] [PubMed] [Google Scholar]
- 7.Delahunt E, Monaghan K, Caulfield B. Ankle function during hopping in subjects with functional instability of the ankle joint. Scand J Med Sci Sports. 2007;17(6):641–648. doi: 10.1111/j.1600-0838.2006.00612.x. [DOI] [PubMed] [Google Scholar]
- 8.Gribble P, Robinson R. Differences in spatiotemporal landing variables during a dynamic stability task in subjects with CAI. Scand J Med Sci Sports. 2010;20(1):e63–e71. doi: 10.1111/j.1600-0838.2009.00899.x. [DOI] [PubMed] [Google Scholar]
- 9.Gribble PA, Robinson RH. Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. J Athl Train. 2009;44(4):350–355. doi: 10.4085/1062-6050-44.4.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caulfield B, Garrett M. Changes in ground reaction force during jump landing in subjects with functional instability of the ankle joint. Clin Biomech (Bristol, Avon) 2004;19(6):617–621. doi: 10.1016/j.clinbiomech.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Wikstrom EA, Naik S, Lodha N, Cauraugh JH. Balance capabilities after lateral ankle trauma and intervention: a meta-analysis. Med Sci Sports Exerc. 2009;41(6):1287–1295. doi: 10.1249/MSS.0b013e318196cbc6. [DOI] [PubMed] [Google Scholar]
- 12.McKeon PO, Paolini G, Ingersoll CD, et al. Effects of balance training on gait parameters in patients with chronic ankle instability: a randomized controlled trial. Clin Rehabil. 2009;23(7):609–621. doi: 10.1177/0269215509102954. [DOI] [PubMed] [Google Scholar]
- 13.Shiner J, Bishop T, Cosgarea AJ. Integrating low-intensity plyometrics into strength and conditioning programs. Strength Cond J. 2005;27(6):10–20. [Google Scholar]
- 14.McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. Balance training improves function and postural control in those with chronic ankle instability. Med Sci Sports Exerc. 2008;40(10):1810–1819. doi: 10.1249/MSS.0b013e31817e0f92. [DOI] [PubMed] [Google Scholar]
- 15.Burcal CJ, Trier AY, Wikstrom EA. Balance training versus balance training with stars in patients with chronic ankle instability: a randomized controlled trial. J Sport Rehabil. 2017;26(5):347–357. doi: 10.1123/jsr.2016-0018. [DOI] [PubMed] [Google Scholar]
- 16.Makaruk H, Czaplicki A, Sacewicz T, Sadowski J. The effects of single versus repeated plyometrics on landing biomechanics and jumping performance in men. Biol Sport. 2014;31(1):9–14. doi: 10.5604/20831862.1083273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Minoonejad H, Karimizadeh Ardakani M, Rajabi R, Wikstrom AE, Sharifnezhad A. Hop stabilization training improves neuromuscular control in college basketball players with chronic ankle instability: a randomized controlled trial. J Sport Rehabil. 2019;28(6):576–583. doi: 10.1123/jsr.2018-0103. [DOI] [PubMed] [Google Scholar]
- 18.Huang PY, Chen WL, Lin CF, Lee HJ. Lower extremity biomechanics in athletes with ankle instability after a 6-week integrated training program. J Athl Train. 2014;49(2):163–172. doi: 10.4085/1062-6050-49.2.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hale SA, Hertel J, Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2007;37(6):303–311. doi: 10.2519/jospt.2007.2322. [DOI] [PubMed] [Google Scholar]
- 20.Chmielewski TL, Myer GD, Kauffman D, Tillman SM. Plyometric exercise in the rehabilitation of athletes: physiological responses and clinical application. J Orthop Sports Phys Ther. 2006;36(5):308–319. doi: 10.2519/jospt.2006.2013. [DOI] [PubMed] [Google Scholar]
- 21.Herrington L. The effects of 4 weeks of jump training on landing knee valgus and crossover hop performance in female basketball players. J Strength Cond Res. 2010;24(12):3427–3432. doi: 10.1519/JSC.0b013e3181c1fcd8. [DOI] [PubMed] [Google Scholar]
- 22.Eechaute C, Vaes P, Van Aerschot L, Asman S, Duquet W. The clinimetric qualities of patient-assessed instruments for measuring chronic ankle instability: a systematic review. BMC Musculoskel Disord. 2007;8:6. doi: 10.1186/1471-2474-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Padua DA, DiStefano LJ. Sagittal plane knee biomechanics and vertical ground reaction forces are modified following ACL injury prevention programs: a systematic review. Sports Health. 2009;1(2):165–173. doi: 10.1177/1941738108330971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim E, Choi H, Cha JH, Park JC, Kim T. Effects of neuromuscular training on the rear-foot angle kinematics in elite women field hockey players with chronic ankle instability. J Sports Sci Med. 2017;16(1):137–146. [PMC free article] [PubMed] [Google Scholar]
- 25.Kipp K, McLean SG, Palmieri-Smith RM. Patterns of hip flexion motion predict frontal and transverse plane knee torques during a single-leg land-and-cut maneuver. Clin Biomech. 2011;26(5):504–508. doi: 10.1016/j.clinbiomech.2011.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wright IC, Neptune RR, van den Bogert AJ, Nigg BM. The influence of foot positioning on ankle sprains. J Biomech. 2000;33(5):513–519. doi: 10.1016/s0021-9290(99)00218-3. [DOI] [PubMed] [Google Scholar]
- 27.Kramer LC, Denegar CR, Buckley WE, Hertel J. Factors associated with anterior cruciate ligament injury: history in female athletes. J Sports Med Phys Fitness. 2007;47(4):446–454. [PubMed] [Google Scholar]
- 28.O'Driscoll J, Kerin F, Delahunt E. Effect of a 6-week dynamic neuromuscular training programme on ankle joint function: a case report. Sports Med Rehabil Ther Technol. 2011;3:13. doi: 10.1186/1758-2555-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wikstrom EA, Hubbard-Turner T, McKeon PO. Understanding and treating lateral ankle sprains and their consequences: a constraints-based approach. Sports Med. 2013;43(6):385–393. doi: 10.1007/s40279-013-0043-z. [DOI] [PubMed] [Google Scholar]
- 30.Agresta C, Brown A. Gait retraining for injured and healthy runners using augmented feedback: a systematic literature review. J Orthop Sports Phys Ther. 2015;45(8):576–584. doi: 10.2519/jospt.2015.5823. [DOI] [PubMed] [Google Scholar]