Abstract
The C1 lateral mass screw (LMS) is widely used as one of the screws for atlantoaxial fixation. Tight bicortical screwing from the posterior to anterior cortical margin of the atlas is recommended. However, important structures, such as the internal carotid artery, are located around this area so precision is required to avoid injuring them. We describe the usefulness of a new electronic conductivity device (ECD) with a pedicle probe and a multi-axis angiography unit for inserting the C1 LMS. Four consecutive patients who were treated with C1 and C2 posterior fixation using an ECD and a multi-axis angiography unit in the hybrid operating room were included. All patients were treated successfully. Seven of eight bicortical screws could be inserted into the perfectly ideal location. The median (interquartile range) distance from the anterior margin of the atlas to the tip of the screw was 0.81 mm (0.43, 1.21 mm). This study suggested that the ECD and multi-axis angiography unit are useful for inserting the C1 LMS safely and tightly.
Keywords: atlas, lateral mass screws, electric conductivity, bicortical screws
Introduction
The C1 lateral mass screw (LMS) is widely used as one of the screws for atlantoaxial fixation. Tight bicortical screwing from the posterior to anterior cortical margin of the atlas is recommended. However, important structures, such as the internal carotid artery, are located around this area so precision is required to avoid injuring them. Currier et al. presented a case where the internal carotid artery (ICA) was impinged on by the tip of a well-placed C1 and C2 transarticular screw.1) Estillore et al.2) presented injury to the ICA caused by exiting screw tips anterior to C1 is a potential life threatening complication of bicortical C1 lateral mass screw, and they measured the position of the ICA in relation to the anterior cortex of C1. In this technical note, we describe a procedure that enables surgeons to place a bicortical screw safely and tightly: a C1 LMS is inserted using a new electronic conductivity device (ECD) with a pedicle probe (PediGuard; Spine Guard, Paris, France) (Figs. 1A–1D) and a multi-axis angiography unit.3,4) ECD was designed as a free hand drilling instrument that measures electrical conductivity.5) Electrical conductivity is measured at the tip of the probe, allowing relative differentiation of tissue conductivity, which is measured at five samples per second, and then the information is converted to sound in real-time. The normal sound and pitch indicating cancellous bone will disappear as the probe gets close to cortical bone. Furthermore, the ECD emits a high frequency and pitch as a warning sound when the probe makes contact with soft tissue or a blood component slightly outside of the cortical bone.3,4) Bolger et al.5) reported that the detection rate of pedicle breaches during the actual pedicle drilling with ECD is superior to only sensation by surgeon.
Fig. 1.
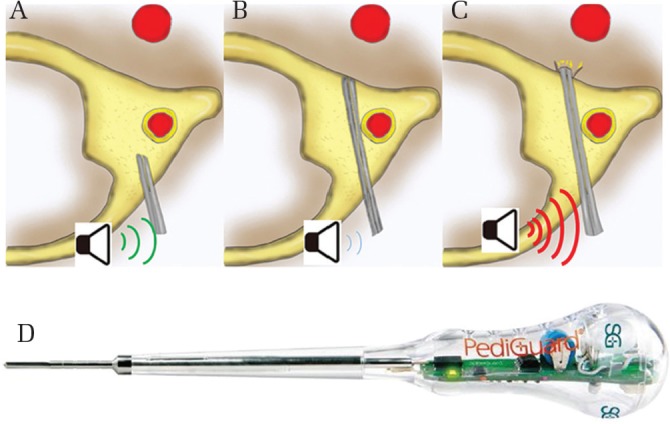
(A) The ECD is inserted into the cancellous bone of the lateral mass carefully while listening to the normal sound and pitch emitted from the device. (B) When the sound from the device disappears, the probe is approaching cortical wall at the anterior margin of the atlas. (C) When the ECD is advanced, it emits a high pitch and frequency as a warning sound, indicating slight penetration of the cortical bone. (D) It is ECD which is used in this procedure. There is an electromagnetic bipolar sensor at the tip (Φ3.2 mm) of equipment. Monitors real-time changes in electrical conductivity five times per second.
It is possible to insert the bicortical screw safely and easily by applying such a probe function. The C1 LMS is widely used as one of the screws for atlantoaxial fixation using Goel-Harms method.6,7) The cervical pedicle screw has adequate biomechanical strength when it is inserted into a hard, thin pedicle. It is easy to insert screws into a large, wide lateral mass at the C1 level, but the internal part of the mass is mostly soft because of the presence of cancellous bone.8) Therefore, it would be desirable to perform bicortical screwing from the posterior margin to the anterior margin of the C1 cortical bone to maintain the strength of the screw as an anchor.9,10) Generally, it is necessary to avoid injuring the ICA, which is located anteriorly to the atlas. Insertion of the pedicle probe into a lateral mass, slight perforation of the anterior wall of the atlas with the probe’s tip (until the warning sound is emitted), and then insertion of the bicortical screw after measuring the actual distance of the probe’s tip from the insertion site are possible with the ECD. These procedures are performed in the hybrid operating room that is equipped with a multi-axis angiography unit. Use of a high-resolution imaging system to obtain a computed tomography (CT)-like image just after screwing leads to accurate screw insertion. There has been a report of a successful, accurate insertion of screws, in which an ECD was used for screwing in the cervical vertebrae region while avoiding structures on the medial and lateral sides.11) However, this is the first report that (1) explains a procedure to obtain fixation tightly by performing bicortical screwing in a relatively easy manner by intentionally perforating the anterior margin of the cortical bone at the atlas, which is in the most remote part of the surgical field, with application of ECD functions and (2) indicates that further accuracy and safety is ensured by good visibility achieved by the high-resolution, real-time fluoroscopy with a multi-axis angiography unit.
Representative Case
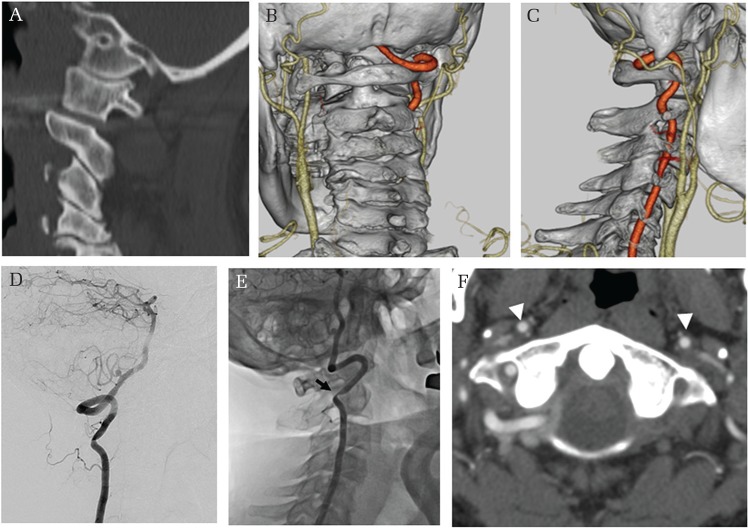
Informed consent was obtained from the patient to publish his case. A 56-year-old man experienced vertigo when his neck was rotated to the right while playing golf or driving his car. The neurological deficit caused recurrent cerebellar symptoms. Destruction of the C1/2 facet was found on the CT scan of the cervical spine. Angiography showed a stenotic right vertebral artery (VA) when his neck was rotated to the right, just distal to the C2 transverse foramen. Hypoplasty of the left VA was observed. He was diagnosed as having bow hunter’s syndrome of the right VA (Figs. 2A–2F).
Fig. 2.
Preoperative neuroimaging findings. (A) Computed tomography scan showing destruction of the C1/2 facet on the left side. (B and C) Three-dimensional computed tomography angiography showing hypoplasty of the left vertebral artery (VA). (D and E) Angiography showing normal flow of the right VA when the patient’s neck is straight and stenosis (arrow) in a portion of the C2 transverse foramen when his neck is rotated to the right. (F) Arrowheads indicate the internal carotid artery (IC). Distances from the anterior margin of the lateral mass to the IC are 3.3 mm on the right side and 4.5 mm on the left side.
Surgery
Surgery was performed with a multi-axis angiography unit (Artis Zeego, VC21-B, Siemens Healthcare, Erlangen, Germany) which is capable of obtaining high-quality intraoperative fluoroscopic images over a broad area in the hybrid operating room. C1 and C2 posterior fixation was conducted.12) For the therapeutic strategy, the bicortical LMS was inserted into the C1 vertebra using Tan’s method with real-time fluoroscopy, a multi-axis angiography unit, and the pedicle probe of the ECD. Additionally, pedicle screws were inserted as anchor screws into the C2 vertebra using navigation (Stealth Station, Medtronic, Broomfield, CO, USA) that was registrated with preoperative CT scan, and then rods were fastened bilaterally.12)
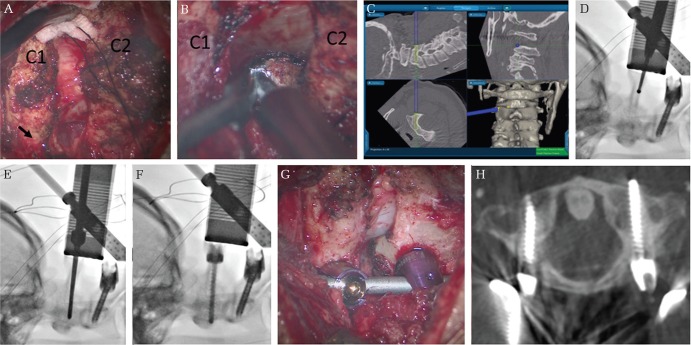
The patient was placed in the prone position, his head was fixed with a Mayfield fixator, and his position was checked using fluoroscopy. A midline skin incision measuring about 5 cm was made from the inferior margin of the external occipital protuberance to the C3 spinous process, exposing the occipital bone to the inferior margin of the lamina at the C2 level (Fig. 3A). Autogenous bone graft harvesting from the iliac crest was performed after the C2 root and venous plexus had been dissected at the margin of the C1/2 facet, and curettage of the C1/2 facet interface had been performed sufficiently with drilling (Fig. 3B). We also placed a navigation frame onto the tip of the spinous process at the C2 level, and C2 pedicle screws were inserted using navigation (Fig. 3C). Next, we placed the C1 LMS. The point of insertion was on just the posterior arch according to Tan’s method (Fig. 3A).12) The ECD was first used after drilling the hard cortical bone of the posterior arch (Fig. 3D). After checking the direction using lateral fluoroscopy with the multi-axis angiography unit, the following steps were performed. (1) The ECD was inserted into the cancellous bone of the lateral mass carefully while listening to the normal sound and pitch it emitted (Fig. 1A). (2) We obtained information that enabled us to lead the probe to cortical bone at the frontal surface of the atlas (i.e., when the normal sound disappeared) (Fig. 1B). (3) We carefully inserted the probe further, and the ECD emitted the warning sound (Figs. 1C and 3E). (4) Since we determined that the cortical bone was slightly perforated, the distance from the C1 posterior wall to the probe’s tip was measured. Then, we tightly, safely, and securely inserted the C1 LMS, which was 1 mm longer than the measured distance (Fig. 3F). We confirmed the actual screw position by obtaining a CT-like image with the multi-axis angiography unit after screw insertion (Figs. 3G and 3H). Finally, the surgical incision was closed with a suture.
Fig. 3.
(A) Operative view. The point of C1 lateral mass screw insertion using Tan’s method (arrowhead). (B) Curettage of the C1/2 facet interface is performed using a drill, and the C2 root is retracted to the cranial side. (C) C2 pedicle screwing is performed with navigation and based on the preoperative computed tomography scan. (D) Drilling is performed to pierce the hard cortical bone at the posterior margin of the arch of the atlas. (E) The probe of the electronic conductivity device is inserted into the cancellous bone of the lateral mass carefully while listening to the sound the device emits. (F) The C1 lateral mass screw is placed using the electronic conductivity device and fluoroscopy. (G) The C1 and C2 screws are placed. (H) The position of the C1 lateral mass screw is confirmed with a computed tomography-like image that was obtained using the multi-axis angiography unit.
Postoperative course
The occurrence of vertigo when the patient’s neck turned to the right disappeared, and postoperative neuroimaging showed that bicortical screwing resulted in complete C1 and C2 fixation.
At 1 year postoperatively, he did not have any problems.
Discussion
Although C1 and C2 posterior fixation has been established as a safe and easy operation with use of the Goel-Harms method, several risks remain with insertion of the C1 LMS and C2 pedicle screw as anchors.6,7) Some methods have been reported for C1 LMS due to the difference in screw insertion point.6,12–14) Each technique has its own advantages and disadvantages, although inserting the bicortical screw from the posterior cortical bone to the anterior side of the cortical bone of the atlas is commonly recommended to ensure sufficient strength of the LMS, which penetrates the soft cancellous bone.10) However, the internal carotid artery or hypoglossal nerve run in the tissues in the anterior region of the atlas.2,15) The shortest distance from the ventral surface of the lateral mass, as detected by preoperative CT angiography, was 3.85 mm (range 1.10–7.50 mm) according to Kim et al.16) In our patient, that distance was 3.56 mm (1.12–5.47 mm) so screw insertion could still injure the internal carotid artery in the case of unexpected changes in the insertion direction or surgical position (Table 1). Thus, insertion using the pedicle probe, which penetrates the cortical bone slightly about 1 mm from the edge of the anterior side of atlas and provides guidance by sound information, is very useful from the viewpoint of safe and strong screw insertion. Moreover, the sound guidance enabled us to prevent rupture of the inside of the spinal canal or outside of the transverse foramen.
Table 1.
Demographic characteristics of the four patients treated with the procedure
| Case no. | Age (years) | Sex | Diagnosis | Side | IC–AC1 distance (mm) | TS–AC1 distance (mm) |
|---|---|---|---|---|---|---|
| 1 | 69 | M | BHS | Rt | 3.08 | 0.48 |
| Lt | 4.67 | 1.26 | ||||
| 2 | 78 | M | AAD | Rt | 5.47 | −1.76 |
| Lt | 4.90 | 0.69 | ||||
| 3 | 51 | M | AAD | Rt | 1.43 | 1.04 |
| Lt | 1.12 | 0.93 | ||||
| 4 | 56 | M | BHS | Rt | 3.43 | 0.41 |
| Lt | 4.40 | 2.09 | ||||
| Median (IQR) | 3.92 (1.84, 4.84) | 0.81 (0.42, 1.21) |
AC1: anterior margin of C1, AAD: atlantoaxial dislocation, BHS: bow hunter’s syndrome, IC: internal carotid artery, IQR: interquartile range, Lt: left, No.: number, Rt: right, TS: tip of the screw.
The ECD is useful for the effective insertion of a C1 LMS for the following reasons: (1) the frequency and pitch of its digital sound can be discerned; (2) it is easy to detect the cortical bone at the anterior margin of the atlas by the absence of sound from the ECD; and (3) the probe can be inserted slowly until the warning sound is heard, resulting in slight perforation of the anterior wall of the C1 lateral mass, although pushing the probe of the ECD can result in an unstable situation. After measuring the actual probe length, the screw length can be decided, and bicortical screwing can be performed safely and tightly. Chaput et al.3) and Ovadia et al.17) reported accurate pedicle screw insertion with an ECD. Guillen et al.4) reported similar accuracy in a cadaveric study. Sandhu et al.18) reported the effective application of an ECD with the S2 alar-iliac screw, although different from the original application of the ECD. On the other hand, Kageyama et al. reported that the real-time imaging of the multi-axis angiography unit in the hybrid operating room was highly accurate and safe for lumbar pedicle screw insertion. Multi-axis angiography unit which is controlled by medical radiology technicians can store the position or angle of the robotic arm, and that function is useful for adjusting the arm repeatedly and rapidly for screwing. The CT-like imaging, that is obtained by the multi-axis angiography unit, further enables intraoperative confirmation of the screw position immediately after screwing.19) Here, we combined these two pieces of equipment and succeeded in obtaining good results.
Visualization with C-arm fluoroscopy and feeling with the Lenke probe ae currently the main techniques used to assist with probe and screw insertion, but their resolution and sensitivity are often insufficient. Navigation with preoperative CT imaging was commonly used from the 2000s.20,21) The conventional navigation system with the reference frame placed on the C2 spinous process is applicable for screw insertion at the C2 level with high accuracy. However, for the C1 LMS, the accuracy of this procedure is not ensured because of potential changes in the patient’s intraoperative position and operative manipulations, such as curettage of the interface of the C1/2 facet or bone grafting, which can cause a substantial gap, as determined by preoperative CT. Herein, we inserted a C2 pedicle screw under the guidance of CT navigation and a C1 LMS under the sound guidance of the ECD, both with high-resolution fluoroscopy using the multi-axis angiography unit.
In recent years, a new navigation system using the O-arm and mobile CT, which enable intraoperative imaging assessment of the patient’s position intraoperatively, results in high accuracy and reliability of pedicle screw insertion.21,22) The reference frame is usually placed at or near the C2 spinous process for C1 and C2 posterior fixation for safety purposes. Compared with these systems, real time and high resolution imaging with multi-axis angiography unit would be a great advantage over O-arm providing the virtual reality imaging constructed using the images obtained before.13)
We treated four patients with the procedure described herein and successfully placed seven of eight bicortical screws in the perfectly ideal location. The median (interquartile range) distance from the anterior margin to the tip of the screw was 0.81 mm (0.43, 1.21 mm) (Table 1). No deviation was observed inside and outside of the ideal position. The case of unsuccessful insertion demonstrated rupture of the anterior wall of the atlas on the postoperative CT scan, indicating successful anterior wall perforation during the probing stage, and the tip of the screw was placed at almost ideal location, cortical bone of the C1 anterior wall.
Before introduction of this method, the C1 LMS in our clinic was often just unicortical because the surgeon attempted to avoid excess anterior perforation. The unicortical screw exhibits strength23) however, many studies recommended bicortical screwing.
The probe of the ECD is disposable, and the equipment is a low-cost investment. Thus, this method is particularly beneficial in institutions where the O-arm or mobile CT is not feasible.
Although it is possible to precisely measure the lateral mass of the atlas punctured by the ECD, the definite measurement from the site of screw puncture of the anterior wall requires CT-like imaging, even if an appropriate length of screw has already been selected. The multi-axis angiography unit exhibits much better resolution than the conventional instrument, and the CT-like image obtained by the unit is has slightly poorer image quality than that obtained with postoperative CT. Thus, we did not successfully place the bicortical screws in all cases. This is a limitation of this method compared with that with mobile-CT and O-arm navigation with higher resolution.20–22) However, further understanding of the advantages and disadvantages of this method and instrument, and more experience will enable us to ultimately establish the appropriate maneuver.
Acknowledgment
The authors thank Cactus Communications, Inc. (www.editage.jp) for English language review.
Footnotes
Conflicts of Interest Disclosure
All authors have no conflicts of interest.
References
- 1).Currier BL, Todd LT, Maus TP, Fisher DR, Yaszemski MJ: Anatomic relationship of the internal carotid artery to the C1 vertebra: a case report of cervical reconstruction for chordoma and pilot study to assess the risk of screw fixation of the atlas. Spine (Phila Pa 1976) 28: E461–E467, 2003 [DOI] [PubMed] [Google Scholar]
- 2).Estillore RP, Buchowski JM, Minh do V, et al. : Risk of internal carotid artery injury during C1 screw placement: analysis of 160 computed tomography angiograms. Spine J 11: 316–323, 2011 [DOI] [PubMed] [Google Scholar]
- 3).Chaput CD, George K, Samdani AF, Williams JI, Gaughan J, Betz RR: Reduction in radiation (fluoroscopy) while maintaining safe placement of pedicle screws during lumbar spine fusion. Spine (Phila Pa 1976) 37: E1305–E1309, 2012 [DOI] [PubMed] [Google Scholar]
- 4).Guillen PT, Knopper RG, Kroger J, Wycliffe ND, Danisa OA, Cheng WK: Independent assessment of a new pedicle probe and its ability to detect pedicle breach: a cadaveric study. J Neurosurg Spine 21: 821–825, 2014 [DOI] [PubMed] [Google Scholar]
- 5).Bolger C, Kelleher MO, McEvoy L, et al. : Electrical conductivity measurement: a new technique to detect iatrogenic initial pedicle perforation. Eur Spine J 16: 1919–1924, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).Goel A, Kulkarni AG, Sharma P: Reduction of fixed atlantoaxial dislocation in 24 cases: technical note. J Neurosurg Spine 2: 505–509, 2005 [DOI] [PubMed] [Google Scholar]
- 7).Harms J, Melcher RP: Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 26: 2467–2471, 2001 [DOI] [PubMed] [Google Scholar]
- 8).Bianco RJ, Arnoux PJ, Wagnac E, Mac-Thiong JM, Aubin CÉ: Minimizing pedicle screw pullout risks: a detailed biomechanical analysis of screw design and placement. Clin Spine Surg 30: E226–E232, 2017 [DOI] [PubMed] [Google Scholar]
- 9).Seybold EA, Baker JA, Criscitiello AA, Ordway NR, Park CK, Connolly PJ: Characteristics of unicortical and bicortical lateral mass screws in the cervical spine. Spine (Phila Pa 1976) 24: 2397–2403, 1999 [DOI] [PubMed] [Google Scholar]
- 10).Eck JC, Walker MP, Currier BL, Chen Q, Yaszemski MJ, An KN: Biomechanical comparison of unicortical versus bicortical C1 lateral mass screw fixation. J Spinal Disord Tech 20: 505–508, 2007 [DOI] [PubMed] [Google Scholar]
- 11).Zeller R, Canavese F, Kulkarni AV, Drake J: Technique for drilling instrument monitoring electrical conductivity in pediatric cervical spine screw insertion: a preliminary report. J Pediatr Orthop 29: 760–764, 2009 [DOI] [PubMed] [Google Scholar]
- 12).Tan M, Wang H, Wang Y, et al. : Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine (Phila Pa 1976) 28: 888–895, 2003 [DOI] [PubMed] [Google Scholar]
- 13).Hong X, Dong Y, Yunbing C, Qingshui Y, Shizheng Z, Jingfa L: Posterior screw placement on the lateral mass of atlas: an anatomic study. Spine (Phila Pa 1976) 29: 500–503, 2004 [DOI] [PubMed] [Google Scholar]
- 14).Liu G, Buchowski JM, Shen H, Yeom JS, Riew KD: The feasibility of microscope-assisted “free-hand” C1 lateral mass screw insertion without fluoroscopy. Spine (Phila Pa 1976) 33: 1042–1049, 2008 [DOI] [PubMed] [Google Scholar]
- 15).Hong JT, Lee SW, Son BC, Sung JH, Kim IS, Park CK: Hypoglossal nerve palsy after posterior screw placement on the C-1 lateral mass. Case report. J Neurosurg Spine 5: 83–85, 2006 [DOI] [PubMed] [Google Scholar]
- 16).Kim MS, Kim JY, Kim IS, et al. : The effect of C1 bursting fracture on comparative anatomical relationship between the internal carotid artery and the atlas. Eur Spine J 25: 103–109, 2016 [DOI] [PubMed] [Google Scholar]
- 17).Ovadia D, Korn A, Fishkin M, Steinberg DM, Wientroub S, Ofiram E: The contribution of an electronic conductivity device to the safety of pedicle screw insertion in scoliosis surgery. Spine (Phila Pa 1976) 36: E1314–E1321, 2011 [DOI] [PubMed] [Google Scholar]
- 18).Sandhu FA, McGowan JE, Felbaum DR, Syed HR, Mueller KB: S2-AI screw placement with the aide of electronic conductivity device monitoring: a retrospective analysis. Eur Spine J 26: 2941–2950, 2017 [DOI] [PubMed] [Google Scholar]
- 19).Kageyama H, Yoshimura S, Uchida K, Iida T: Advantages and disadvantages of multi-axis intraoperative angiography unit for percutaneous pedicle screw placement in the lumbar spine. Neurol Med Chir (Tokyo) 57: 481–488, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Shin BJ, James AR, Njoku IU, Härtl R: Pedicle screw navigation: a systematic review and meta-analysis of perforation risk for computer-navigated versus freehand insertion. J Neurosurg Spine 17: 113–122, 2012 [DOI] [PubMed] [Google Scholar]
- 21).Ito H, Neo M, Yoshida M, Fujibayashi S, Yoshitomi H, Nakamura T: Efficacy of computer-assisted pedicle screw insertion for cervical instability in RA patients. Rheumatol Int 27: 567–574, 2007 [DOI] [PubMed] [Google Scholar]
- 22).Hecht N, Kamphuis M, Czabanka M, et al. : Accuracy and workflow of navigated spinal instrumentation with the mobile AIRO(®) CT scanner. Eur Spine J 25: 716–723, 2016 [DOI] [PubMed] [Google Scholar]
- 23).Elliott RE, Tanweer O, Smith ML, Frempong-Boadu A: Impact of starting point and bicortical purchase of C1 lateral mass screws on atlantoaxial fusion: meta-analysis and review of the literature. J Spinal Disord Tech 28: 242–253, 2015 [DOI] [PubMed] [Google Scholar]