Abstract
Objective:
To evaluate associations between perceived mental workload (number of hours spent studying and perceived mental intensity) and sleep quality among young adults.
Participants:
656 participants [62% male, median age (IQR)=20 (19, 21) years] recruited from a US college town
Methods:
As part of an online screener, participants answered questions about perceived workload and sleep quality (Pittsburgh Sleep Quality Index (PSQI)). Number of hours/day of mentally-engaging work/study, and mental intensity score were the exposures, categorized into quartiles. Linear regression models were used for continuous sleep quality score, and modified Poisson models were used for poor quality sleep (>5 PSQI score) and individual sleep components, adjusting for sex, age, race, physical activity, and caffeine intake.
Results:
Higher mental work-hours was associated with lower-quality sleep; those in the highest quartile of mental work-hours had a 28% higher likelihood of poor sleep quality (95% CI 2% to 62%). Higher mental intensity scores were also related to lower quality sleep; comparing the highest to the lowest quartiles, there was a 45% higher probability of being a poor sleeper (95% CI 15% to 83%). Associations with PSQI components were partly sex-specific: while both sexes had associations between mental intensity and short sleep, males had positive associations with poor sleep quality and sleep medication use. Conversely, females with higher mental intensity reported higher-quality sleep overall, lower sleep medication use but lower sleep efficiency.
Conclusions:
Higher mental workload is associated with lower overall sleep quality in young adults. Associations with individual sleep quality components differed by sex.
Keywords: academic workload, study, college, sleep duration, sleep medication
INTRODUCTION
Poor sleep among university students is a substantial public health concern, with an alarming 70% of college students reporting sleeping <7 hours per day and 60% meeting the threshold for poor quality sleep (Lund, Reider, Whiting, & Prichard, 2010). A recent survey of colleges across the US found that only 7% of college students reported feeling rested upon awakening in each of the 7 days prior to the survey(American College Health Association, 2017). Short sleep duration as well as poor quality sleep are associated with numerous health and academic outcomes among university student populations, including obesity and cardiometabolic morbidity (Quick et al., 2014), depression and anxiety (Concepcion et al., 2014), motor vehicle crashes (Taylor & Bramoweth, 2010), alcohol consumption and substance use (Hasler et al., 2017; Van Reen et al., 2016), and difficulties with learning, concentration, and lower grade point averages (Owens, Christian, & Polivka, 2017).
Increased independence, shared living quarters, and intake of substances such as alcohol and caffeine are all hallmarks of university life that may contribute to insufficient and poor sleep quality (Hershner, 2016; Owens et al., 2017). Additionally, young adults have a delayed circadian rhythm which encourages later bed and rise times compared to children and adults (Carskadon, Vieira, & Acebo, 1993; Crowley, Acebo, & Carskadon, 2007). University student populations also have high rates of mental health disorders (Pedrelli, Nyer, Yeung, Zulauf, & Wilens, 2015), which may be a cause (Wallace, Boynton, & Lytle, 2017) as well as a consequence of poor sleep. Yet, one substantial component of university life that has received relatively little attention in the epidemiological literature is how mental workload- the time allocated to and intensity of studying, homework, and reading- could contribute to poor sleep quality. Of the studies that have been conducted, findings are mixed. While students may cite heavy academic workloads as a reason for lack of sleep (Hershner, 2015), at least one epidemiological study found no association between the number of hours spent studying and sleep duration (Tsui & Wing, 2009). Similar to the sparse data on how amount of studying could impact sleep duration, only a few studies have examined academic workload in relation to the quality of sleep. One study among Nigerian undergraduates showed that a heavy workload before bed was associated with non-restorative sleep (Oluwole, 2010), and a study of Lithuanian university students found that greater amount of time spent studying, as well as studying before bed, were associated with worse quality sleep (Preišegolavičiūtė, Leskauskas, & Adomaitienė, 2010). In contrast, a study of Estonian medical students found that neither workload during the day nor at night were associated with sleep quality (Veldi, Aluoja, & Vasar, 2005). A remaining gap in the literature is whether the perceived intensity of studying may affect these associations. It is plausible that intense studying, which requires deep concentration and focus, might be particularly related to poor quality sleep, including difficulty falling asleep and staying asleep. Finally, previous studies did not consider the possibility of sex differences. Different rates of sleep disturbances have been documented in males compared to females (Mong & Cusmano, 2016); for example, women are known to have poorer sleep quality along with an earlier bedtime, rise time, and longer sleep latency than men(Tsai & Li, 2004). The experience of academic pressure and coping mechanisms employed may also vary by sex, as illustrated by a positive correlation between academic stress and the use of avoidance and self-punishment coping responses in college men but not in women in one study (Brougham, Zail, Mendoza, & Miller, 2009). How these different coping strategies relate to sleep quality remains unclear.
Many factors may affect poor sleep quality among college students, however, the influence of mental workload on sleep has received minimal investigation. The present study thus sought to evaluate whether mental workload- including number of hours spent studying as well as perceived mental intensity- may be another factor contributing to the high prevalence of poor quality sleep in college-age adults. We further evaluated sex-specific associations between perceived mental intensity and individual components of sleep quality, including subjective sleep quality, sleep duration, sleep latency, sleep disturbances, sleep efficiency, use of sleep medication, and daytime dysfunction. Findings may aid in the design of interventions to encourage healthy sleep habits in college-age adults as well as in the creation of healthy sleep policies at the classroom and university levels.
METHODS
Sample
The sample comprised young adults presumably attending a private engineering university in upstate New York who took part in a comprehensive screening questionnaire for an experimental study (designed to test the effects of liquid energy shot consumption on acute changes in mood and cognition). Subjects were recruited from the university and surrounding town (approximate total population 16,000) using the following strategies: 1) classroom announcements (in classes>50 students); 2) mass emails sent in the beginning of the fall, spring and summer semesters to students, faculty and staff; 3) flyers posted on campus and small businesses in the surrounding towns; and 4) word of mouth. The screening questionnaire was administered online using www.surveymonkey.com. All study protocols were approved by the Institutional Review Board at [redacted] (Approval # 16–34.1).
Exposures: Mental Workload
Questions concerning mental workload were taken from the Mental and Physical State and Trait Energy and Fatigue scales (O’Connor, 2006). Participants were asked about the number of days per week engaged in school/work, the number of hours per day spent on mentally-engaging tasks (“How many hours per day do you do mental work such as reading, learning, organizing or analyzing information or solving problems”), and the intensity of mental work performed on school/work days (“Rate the average intensity of mental work you do on a typical work day on a scale of 1–5”; higher scores indicated greater intensity). The number of credit hours was not included. The number of hours/day of mental work was categorized into quartiles, with the highest quartile corresponding to the highest number of hours/day. Perceived mental intensity was calculated as the reported number of school/work days times the number of hours of mental work performed on school/work days times the self-rated intensity of mental work performed on school/work days (O’Connor, 2006). Perceived mental intensity was similarly categorized into quartiles, with the highest quartile representing the highest mental intensity.
Outcome: Sleep Quality
The Pittsburgh Sleep Quality Index (PSQI) was administered to assess sleep quality (Buysse DJ, Reynolds CF, 3rd, Monk TH, 1989). This 19-question survey assesses seven underlying components including sleep quality, latency, duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction over the past month. The individual component scores (which each have a range of 0 to 3) are summed to create an overall sleep quality score, with higher scores indicating worse quality sleep (highest possible score=21). Poor sleep quality was defined as PSQI score>5(Buysse DJ, Reynolds CF, 3rd, Monk TH, 1989). Sleep quality was analyzed as a continuous score, as well as a dichotomous variable for poor sleep quality. Individual component scores were also evaluated as dichotomous variables, with cutoffs based on the distribution of scores in the population (e.g. poor subjective sleep quality defined as component score>1).
Covariates
The following covariates were selected a priori based on their plausible role as confounders: sex, age, race, physical activity, caffeinated beverage consumption, and symptoms of depression and anxiety. Demographic information including age, sex, and race were categorized as shown in Table 1.
Table 1.
Sociodemographic and lifestyle characteristics of a sample of 656 participants recruited from a US university
| Sociodemographic and lifestyle correlates | Median (IQR) or % |
|---|---|
| Sex | |
| Male | 62.8% |
| Race | |
| Caucasian | 83.5% |
| Age, years (median) | 20 (19, 21) |
| BMI (kg/m2) | 23 (21, 26) |
| Vigorous physical activity, METS/week | 36 (18, 68) |
| Moderate physical activity, METS/week | 5 (4, 6) |
| Caffeinated beverage consumption, serv/week | 9 (3, 18) |
| Depression symptoms, POMS score | 6 (5, 8) |
| Anxiety symptoms, POMS score | 7 (6, 9) |
| Hours spent in mental work/day | 6 (4, 8) |
| Mental intensity score | 105 (70, 160) |
| PSQI Sleep Quality continuous score | 5 (4, 7) |
| Poor quality sleep (>5 score) | 49.7% |
| Sleep duration, hours | 7.5 (7, 8) |
Physical activity was also calculated using the Mental and Physical State and Trait Energy and Fatigue Scale. Subjects were asked to report the number of hours per day and the number of days per week that they performed high and moderate intensity activities. To convert to metabolic equivalents (METS), the hours per week of high intensity were multiplied by 9 and the number of hours of moderate intensity were multiplied by 5. These weight values correspond to the approximate oxygen consumption requirement for each exercise intensity level (Ainsworth et al., 2011).
To estimate caffeinated beverage consumption, participants were asked to report their usual weekly intake of coffee, tea, soft drinks, energy drinks, frozen desserts containing caffeine, chocolate containing caffeine, and other items that may contain caffeine. Participants were also asked for the serving sizes of the products they consumed (Motl, O’Connor, & Dishman, 2003); this information was used to convert into the number of 8 oz servings of caffeine consumed per week.
The 30-item POMS-SF was used to assess mood over the previous 30 days (Curran, Andrykowski, & Studts, 1995). Reponses ranged from “Not at all” (scored as 0) to “Extremely” (scored as 4) over the past 30 days. For the present analysis, 2 continuous components were used, which were scored based on 5 items: tension/anxiety (α=.81) and depression (α=.94) (Curran et al., 1995; Terry, Lane, & Fogarty, 2003). These two components were selected based on the known relationships between anxiety, depression, and sleep quality (Nyer et al., 2013).
Data Analysis
First, bivariate associations were examined between the mental workload exposures (mental work hours and perceived mental intensity) and potential confounders. To do so, the mean ± SD mental work hours and perceived mental intensity were computed according to categories (quartiles unless otherwise mentioned) of the potential confounders. Tests for trends were assessed using linear regression models, with each mental workload exposure as a continuous outcome and a continuous exposure variable representing ordinal categories for each potential confounder (each confounder/outcome model run separately). Linear regression models with interaction terms for sex were used to evaluate potential interaction between sex and the confounders in relation to mental workload.
To evaluate the primary study question, linear regression models were used with PSQI score as a continuous outcome and indicator variables for quartiles of mental workload indices (separately) as predictors. The quartile approach was used in order to assess the dose-response relations, and to diminish the potential effects of mental workload outliers. A modified Poisson regression approach (Zou, 2004) was used to examine sleep quality as a dichotomous outcome (poor sleep quality). Both crude models (crude Poisson models not shown but available on request) as well as models adjusted for sex, age, race, caffeinated beverage intake, and weekly METS of moderate physical activity were run. Further adjustment for METS/week of vigorous physical activity, tension/anxiety scores, and depression scores did not substantially alter estimates and thus were not included in final models. To evaluate potential interaction with sex in each model, interaction terms for sex*mental workload indices were included, and the P for interaction was examined.
Finally, further analysis of the association between mental workload and sleep quality was conducted by examining each sleep quality component as a separate outcome. The modified Poisson regression approach was used to model each sleep quality component dichotomously, based on the distribution of the component scores in the study sample (e.g. short sleep duration was defined as reporting <6 hours of sleep on a typical night). As in prior analyses, interactions with sex were evaluated. All analyses were conducted in Stata 14.0 (College Station, Texas).
RESULTS
Of 718 respondents aged 18 to 45 years who finished the initial screening survey, there were 662 participants with information on both mental workload and sleep quality. Of these, 6 were excluded due to implausible values; thus the final sample size for the present analysis was 656. The majority of the sample was male, with a median (IQR) age of 20 years (19, 21; Table 1). Associations between sociodemographic and lifestyle characteristics and mental intensity are shown in Table 2.
Table 2.
Associations between potential confounders and mental intensity on work/school days among 656 participants recruited from a US university
| Sociodemographic and lifestyle correlates | N | Hours spent in mental work/day |
Mental intensity |
|---|---|---|---|
| Median (IQR) | Median (IQR) | ||
| Sex | |||
| Male | 412 | 5 (4, 8) | 100 (60, 142) |
| Female | 214 | 7 (5, 8) | 120 (80, 160) |
| P value | <0.0001 | <0.0001 | |
| Race | |||
| Caucasian | 548 | 6 (4, 8) | 105 (72, 160) |
| Other | 108 | 6 (4, 8) | 100 (60, 160) |
| P value2 | 0.70 | 0.98 | |
| Age group, years (y) | |||
| 18 or 19 y | 272 | 5 (4, 8) | 100 (60, 147) |
| 20 y | 112 | 6 (4, 8) | 108 (60, 160) |
| 21 y | 110 | 6 (4, 8) | 120 (75, 160) |
| 22 to 44 y | 162 | 6 (5, 8) | 116 (75, 160) |
| P value | 0.04 | 0.05 | |
| Vigorous physical activity, METS/week | |||
| Q1, 0 to 18 | 183 | 6 (4, 8) | 100 (60, 144) |
| Q2, 20.3 to 36 | 163 | 6 (4, 8) | 105 (70, 160) |
| Q3, 40.5 to 67.5 | 167 | 6 (4, 8) | 100 (75, 144) |
| Q4, 72 to 222.8 | 143 | 6 (4, 8) | 105 (60, 160) |
| P value | 0.94 | 0.97 | |
| Moderate physical activity, METS/week | |||
| Q1, 0 to 3.75 | 306 | 6 (4, 8) | 100 (63, 150) |
| Q2, 5 | 95 | 6 (4, 8) | 100 (60, 160) |
| Q3, 6.25 | 136 | 6 (4, 8) | 120 (75, 160) |
| Q4, 7.5 to 70 | 119 | 6 (4, 8) | 120 (75, 168) |
| P value | 0.14 | 0.04 | |
| Caffeinated beverage consumption, serv/week | |||
| Q1, 0 to 3 | 180 | 5 (4, 8) | 100 (60, 160) |
| Q2, 4 to 9 | 175 | 6 (4, 8) | 100 (60, 160) |
| Q3, 10 to 18 | 140 | 6 (4,8) | 120 (69, 160) |
| Q4, 20 to 60 | 161 | 6 (4,8) | 112 (75, 160) |
| P value | 0.15 | 0.14 | |
| Depression symptoms, POMS score | |||
| Q1, 5 | 275 | 6 (4, 8) | 105 (70, 160) |
| Q2, 6 | 106 | 6 (4, 8) | 105 (75, 168) |
| Q3, 7 or 8 | 127 | 6 (4, 8) | 105 (68, 160) |
| Q4, 9 to 25 | 148 | 6 (4, 8) | 100 (72, 157) |
| P value | 0.85 | 0.78 | |
| Anxiety symptoms, POMS score | |||
| Q1, 5 or 6 | 278 | 6 (4, 8) | 103 (63, 160) |
| Q2, 7 | 98 | 5 (4, 8) | 103 (70, 144) |
| Q3, 8 or 9 | 129 | 6 (4, 8) | 105 (63, 168) |
| Q4, 10 to 24 | 151 | 6 (4, 8) | 105 (75, 150) |
| P value | 0.58 | 0.61 |
The number of mental work hours/day was associated with poorer sleep quality, although the association was only statistically significant when sleep quality was considered dichotomously (PSQI score>5). As can be seen in Table 3, students in the 4th quartile of mental work hours/day had a 28% higher adjusted probability of poor quality sleep compared to those in the 1st quartile (95% CI 2% to 62%; P for trend=0.03). This association may be mostly attributed to the sleep duration component; e.g. those in the 4th quartile of mental work hours/day were 1.74 times more likely to obtain <6 hours of sleep (95% CI 1.10 to 2.75; P for trend=0.09).
Table 3.
Associations between mental intensity and sleep quality among 656 participants recruited from a US university
| N | Sleep Quality Score Unadjusted beta (95% CI) |
Sleep Quality Score Adjusted beta1 (95% CI) |
Sleep Quality Score>5 Adjusted Prevalence Ratio (95% CI) |
|
|---|---|---|---|---|
| Hours spent in mental work on school days | ||||
| Q1 (1 to 4 hrs per day) | 210 | Reference | Reference | Reference |
| Q2 (4.5 to 5.5 hrs per day) | 193 | 0.27 (−0.27, 0.82) | 0.18 (−0.36, 0.72) | 1.17 (0.94, 1.45) |
| Q3 (6 to 8 hrs per day) | 164 | 0.32 (−0.24, 0.89) | 0.13 (−0.45, 0.70) | 1.22 (0.98, 1.53) |
| Q4 (9 to 15 hrs per day) | 132 | 0.51 (−0.10, 1.12) | 0.38 (−0.24, 0.99) | 1.28 (1.02, 1.62) |
| P, trend | 0.10 | 0.29 | 0.03 | |
| Mental intensity on school days | ||||
| Q1 (8 to 60) | 182 | Reference | Reference | Reference |
| Q2 (63 to 96) | 180 | 0.49 (−0.08, 1.06) | 0.43 (−0.15, 1.00) | 1.23 (0.97, 1.57) |
| Q3 (100 to 140) | 194 | 0.48 (−0.08, 1.03) | 0.33 (−0.24, 0.90) | 1.29 (1.02, 1.62) |
| Q4 (144 to 420) | 143 | 0.87 (0.27, 1.48) | 0.72 (0.11, 1.34) | 1.45 (1.15, 1.83) |
| P, trend | 0.008 | 0.04 | 0.002 |
Includes adjustment for sex, age, race, weekly servings of caffeinated beverage intake, and weekly METS of moderate physical activity
In contrast to mental work hours/day, mental intensity score was robustly associated with worse quality sleep (Table 3). Students in the 4th quartile of mental intensity had 0.72 higher PSQI scores than students in the 1st quartile (95% CI 0.11 to 1.34; P for trend= 0.04), and a 45% higher probability of being classified as a poor quality sleeper (95% 15% to 83%; P for trend=0.002). Further, there was evidence of interaction by sex (P, interaction=0.05), such that the mental intensity-sleep quality association was stronger among females. For example, females in the 4th quartile of mental intensity had a 70% higher adjusted probability of poor quality sleep than females in the 1st quartile (95% CI 9% to 163%).
The association between mental intensity and sleep quality were further investigated by examining the individual sleep quality component scores (Figure 1). Of the 7 components, only the association between mental intensity and short sleep duration was statistically significantly related (112% higher probability of short sleep in the 4th compared to the 1st quartile; P for trend= 0.01). Consequently, there was evidence of interaction by sex with 2 of the components-sleep quality (P, interaction=0.006) and use of sleeping medication (P, interaction=0.04). Among males, higher mental intensity was associated with poor sleep quality and greater likelihood of using a sleeping medication. In direct contrast, females with higher mental intensity were less likely to use a sleeping medication and trended towards reporting higher quality sleep. However, females with higher mental intensity had shorter sleep duration (Figure 1) and lower sleep efficiency (PR of <85% sleep efficiency=1.99 with 95% CI 0.92 to 4.30 comparing the 4th quartile to the 1st).
Figure 1.
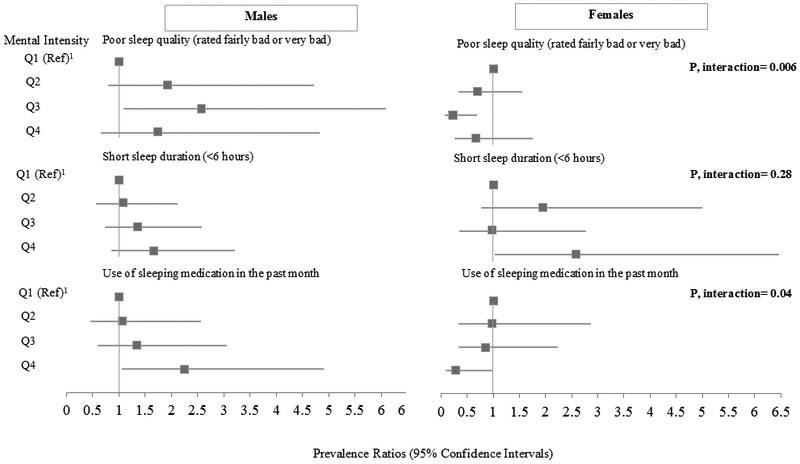
Mental intensity in relation to selected components of the PSQI, sex-stratified
1Q1 represents the lowest mental intensity in each. Sample sizes in each of the quartiles are as follows for Males: Q1=131, Q2= 105, Q3= 102, Q4= 74; and Females: Q1= 43; Q2= 62; Q3= 81; Q4= 58
DISCUSSION
In this sample of participants recruited from a small US college campus and surrounding town, we found that higher mental intensity was associated with poor sleep quality, an association that appeared to be only partially driven by actual quantity of work (number of study hours). Interestingly, whereas higher mental intensity was associated with short sleep duration in both males and females, associations with other sleep quality components differed by sex. While males with higher mental intensity reported lower quality sleep and higher usage of sleep medication, females with higher mental intensity had better sleep quality and were less likely to use sleep medication.
These findings add to the sparse data concerning mental workload and sleep quality in university students, and are in line with a few others from Nigeria and Lithuania (Oluwole, 2010; Preišegolavičiūtė et al., 2010) that have found associations between higher academic workloads and lower quality sleep. One obvious explanation for an association between mental workload and poor sleep quality is that students who spend more time studying devote less time to sleep. This assertion is consistent with our finding that a higher number of reported study hours was associated with lower quality sleep, most notably with the sleep duration component of overall sleep quality. Another explanation for an association between higher number of hours spent studying and lower sleep quality is that a longer amount of time spent studying is typically concomitant with sedentary behavior and high amounts of screen time, which have each been associated with lower quality sleep (Exelmans & Van Den Bulck, 2017; Pilcher, Morris, Bryant, Merritt, & Feigl, 2017; Wu, Tao, Zhang, Zhang, & Tao, 2015). In particular, studying performed at night on light emitting devices can increase nighttime alertness (Chang, Aeschbach, Duffy, & Czeisler, 2015).
Although there was an association between number of typical study hours and poor sleep quality, there was a stronger association between poor sleep quality and perceived mental intensity, a measure that incorporates both the number of study hours and perceived cognitive stimulation of the study time. While we could identify no studies within university populations that have examined this construct, our findings are in line with studies of adults in the workplace which have found that cognitively and emotionally demanding work is associated with sleep disturbances(T. Åkerstedt et al., 2002; Torbjörn Åkerstedt et al., 2015; Marquié, Foret, & Quéinnec, 1999). To highlight, a study of Swiss workers found that high work demand on one day, which was measured by “working very intensively”, “demanding too much effort”, and “not enough time to do everything”, was associated with more sleep disturbances that night(Torbjörn Åkerstedt et al., 2015).
There may be a few plausible explanations for association between mental intensity and poor sleep quality in our sample. First, after intense studying, particularly if done mostly at night, student may find it hard to transition into a relaxed state for sleep (Wuyts et al., 2012). Second, higher perceived mental intensity could be positively associated with academic-related stress, and stress is known to affect sleep quality in college students (Almojali, Almalki, Alothman, Masuadi, & Alaqeel, 2017). However, although no measures of stress were obtained in this study, it is of note that the POMS anxiety score was associated with sleep quality but not with perceived mental intensity.
We also found evidence that males and females respond differently to perceived mental intensity with respect to sleep quality characteristics. In particular, females with high mental intensity may have difficulties with falling and staying asleep (insomnia symptoms), as evidenced by the tendency towards lower sleep efficiency in our study. This is not necessarily surprising, as females are more likely to suffer from insomnia than men (Petrov, Lichstein, & Baldwin, 2014). Interestingly, women with higher mental intensity were also less likely to use sleep medications and to report high-quality sleep, which are paradoxically markers of better sleep health but not necessarily contradictory (e.g. it is possible to take a long time to fall asleep yet still experience high sleep quality once asleep). In contrast, males with high mental intensity had higher consumption of caffeinated beverages and were more likely to use sleep medication. In turn, these substances may be responsible for the lower ratings of subjective sleep quality (Ogeil & Phillips, 2015). A sleep medication may be a simple over the counter medication, however, it may also include other substances such as alcohol and marijuana (Hasler et al., 2017; Taylor & Bramoweth, 2010). For example, in a study among undergraduates from the US, 11% of non-abstainers reported using alcohol as a sleep aid in the past week (Taylor & Bramoweth, 2010).
There are both strengths and limitations in the present study. A strength was the relatively large sample size, as well as the inclusion of the mental intensity score, a construct that has not been previously considered in relation to sleep. The cross-sectional study design was a limitation, as it results in temporal ambiguity. Further, the questions pertaining to mental workload did not include a time reference, while the PSQI asked about sleep in the previous month. In addition, although the target population was university students, it is possible that adults residing in the surrounding town who were not university attendees took part in the study. Nonetheless, only 7.7% of our study sample were older than 25 years, indicating that the majority of the sample were in a typical age range for undergraduate college students. While this does not guarantee these participants were enrolled in a university, the likelihood is high given that [name redacted] is a small town of approximately 16,000 people that houses two universities. Further, it is possible that the >25 year old participants could be graduate students, as both universities also offer graduate programs. A related issue was that it was not possible to differentiate students by field of study (e.g. engineering versus other), which precludes examination of effect modification by academic major. Sleep quality was self-reported and thus may be subject to measurement error; nonetheless, this error may be non-differential with respect to the exposure and may only affect the precision of the estimates. There is also the possibility of unmeasured confounding. For example, participants were not asked about alcohol consumption, average daily screen time, or number of credit hours. Finally, they were not asked about the timing of study habits, so it was not possible to examine whether night-time studying had an impact on sleep quality or whether results differed if the study hours were typically continuous or intermittent. Future studies among college students that investigate the role of night-time studying habits versus those during the day are thus warranted.
In summary, we found that perceived mental intensity, a summary marker that includes both mental work hours as well as self-rated intensity, was associated with poor sleep quality among university students. This association was attributed to different sleep characteristics in males compared to females. Overall this study provides another perspective on why university students may benefit from information on sleep hygiene and health. Based on our findings, these messages might need to be tailored differently for university males and females.
Acknowledgments
Funding Details: Dr. Jansen was supported by the National Institutes of Health/National Heart, Lung, and Blood Institute grant 5T32HL110952–05.
Footnotes
Disclosure statement: None of the authors have any conflicts of interest.
REFERENCES
- Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C, … Leon AS (2011). 2011 compendium of physical activities: A second update of codes and MET values. Medicine and Science in Sports and Exercise. 10.1249/MSS.0b013e31821ece12 [DOI] [PubMed] [Google Scholar]
- Åkerstedt T, Garefelt J, Richter A, Westerlund H, Magnusson Hanson LL, Sverke M, & Kecklund G (2015). Work and Sleep—A Prospective Study of Psychosocial Work Factors, Physical Work Factors, and Work Scheduling. Sleep. 10.5665/sleep.4828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Åkerstedt T, Knutsson A, Westerholm P, Theorell T, Alfredsson L, & Kecklund G (2002). Sleep disturbances, work stress and work hours: A cross-sectional study. Journal of Psychosomatic Research. 10.1016/S0022-3999(02)00333-1 [DOI] [PubMed] [Google Scholar]
- Almojali AI, Almalki SA, Alothman AS, Masuadi EM, & Alaqeel MK (2017). The prevalence and association of stress with sleep quality among medical students. Journal of Epidemiology and Global Health, 7(3), 169–174. 10.1016/j.jegh.2017.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College Health Association. (2017). American College Health Association National College Health Assessment (ACHA-NCHA). American College Health Association National College Health Assessment, 20 Retrieved from http://www.acha-ncha.org/docs/NCHA-II_SPRING_2017_UNDERGRADUATE_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf [Google Scholar]
- Brougham RR, Zail CM, Mendoza CM, & Miller JR (2009). Stress, sex differences, and coping strategies among college students. Current Psychology. 10.1007/s12144-009-9047-0 [DOI] [Google Scholar]
- Buysse DJ, Reynolds CF 3rd, Monk TH, B. S. and K. D. (1989). The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res, (28), 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Carskadon MA, Vieira C, & Acebo C (1993). Association between puberty and delayed phase preference. Sleep, 16(3), 258–262. 10.1093/sleep/16.3.258 [DOI] [PubMed] [Google Scholar]
- Chang A-M, Aeschbach D, Duffy JF, & Czeisler CA (2015). Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proceedings of the National Academy of Sciences, 112(4), 1232–1237. 10.1073/pnas.1418490112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Concepcion T, Barbosa C, Vélez JC, Pepper M, Andrade A, Gelaye B, … Williams MA (2014). Daytime sleepiness, poor sleep quality, eveningness chronotype, and common mental disorders among chilean college students. Journal of American College Health, 62(7), 441–448. 10.1080/07448481.2014.917652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley SJ, Acebo C, & Carskadon MA (2007). Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Medicine, 8(6), 602–612. 10.1016/j.sleep.2006.12.002 [DOI] [PubMed] [Google Scholar]
- Curran SL, Andrykowski MA, & Studts JL (1995). Short form of the Profile of Mood States (POMS-SF): Psychometric information. Psychological Assessment, 7(1), 80–83. 10.1037/1040-3590.7.1.80 [DOI] [Google Scholar]
- Exelmans L, & Van Den Bulck J (2017). Binge viewing, sleep, and the role of Pre-Sleep Arousal. Journal of Clinical Sleep Medicine, 13(8), 1001–1008. 10.5664/jcsm.6704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedrich A, & Schlarb AA (2018). Let’s talk about sleep: a systematic review of psychological interventions to improve sleep in college students. Journal of Sleep Research. 10.1111/jsr.12568 [DOI] [PubMed] [Google Scholar]
- Hasler BP, Franzen PL, de Zambotti M, Prouty D, Brown SA, Tapert SF, … Clark DB (2017). Eveningness and Later Sleep Timing Are Associated with Greater Risk for Alcohol and Marijuana Use in Adolescence: Initial Findings from the National Consortium on Alcohol and Neurodevelopment in Adolescence Study. Alcoholism: Clinical and Experimental Research, 41(6), 1154–1165. 10.1111/acer.13401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hershner S (2015). Is sleep a luxury that college students cannot afford? Sleep Health. 10.1016/j.sleh.2014.12.006 [DOI] [PubMed] [Google Scholar]
- Hershner S (2016). Causes and consequences of sleepiness among college students Causes and consequences of sleepiness among college students. Nature and Science of Sleep, 6(April), 73–84. 10.2147/NSS.S62907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund HG, Reider BD, Whiting AB, & Prichard JR (2010). Sleep Patterns and Predictors of Disturbed Sleep in a Large Population of College Students. Journal of Adolescent Health, 46(2), 124–132. 10.1016/j.jadohealth.2009.06.016 [DOI] [PubMed] [Google Scholar]
- Marquié JC, Foret J, & Quéinnec Y (1999). Effects of age, working hours, and job content on sleep: A pilot study. Experimental Aging Research. 10.1080/036107399243896 [DOI] [PubMed] [Google Scholar]
- Mong JA, & Cusmano DM (2016). Sex differences in sleep: Impact of biological sex and sex steroids. Philosophical Transactions of the Royal Society B: Biological Sciences. 10.1098/rstb.2015.0110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motl RW, O’Connor PJ, & Dishman RK (2003). Effect of caffeine on perceptions of leg muscle pain during moderate intensity cycling exercise. The Journal of Pain, 4(6), 316–321. 10.1016/S1526-5900(03)00635-7 [DOI] [PubMed] [Google Scholar]
- Nyer M, Farabaugh A, Fehling K, Soskin D, Holt D, Papakostas GI, … Mischoulon D (2013). Relationship between sleep disturbance and depression, anxiety, and functioning in college students. Depression and Anxiety, 30(9), 873–880. 10.1002/da.22064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor PJ (2006). Mental and physical state and trait energy and fatigue scales. [Google Scholar]
- Ogeil RP, & Phillips JG (2015). Commonly used stimulants: Sleep problems, dependence and psychological distress. Drug and Alcohol Dependence, 153, 145–151. 10.1016/j.drugalcdep.2015.05.036 [DOI] [PubMed] [Google Scholar]
- Oluwole OSA (2010). Sleep habits in Nigerian undergraduates. Acta Neurologica Scandinavica, 121(1), 1–6. 10.1111/j.1600-0404.2009.01171.x [DOI] [PubMed] [Google Scholar]
- Owens H, Christian B, & Polivka B (2017). Sleep behaviors in traditional-age college students: A state of the science review with implications for practice. Journal of the American Association of Nurse Practitioners. 10.1002/2327-6924.12520 [DOI] [PubMed] [Google Scholar]
- Pedrelli P, Nyer M, Yeung A, Zulauf C, & Wilens T (2015). College students: Mental health problems and treatment considerations. Academic Psychiatry. 10.1007/s40596-014-0205-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrov ME, Lichstein KL, & Baldwin CM (2014). Prevalence of sleep disorders by sex and ethnicity among older adolescents and emerging adults: Relations to daytime functioning, working memory and mental health. Journal of Adolescence, 37(5), 587–597. 10.1016/j.adolescence.2014.04.007 [DOI] [PubMed] [Google Scholar]
- Pilcher JJ, Morris DM, Bryant SA, Merritt PA, & Feigl HB (2017). Decreasing sedentary behavior: Effects on academic performance, meta-cognition, and sleep. Frontiers in Neuroscience, 11(May). 10.3389/fnins.2017.00219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preišegolavičiūtė E, Leskauskas D, & Adomaitienė V (2010). Associations of quality of sleep with lifestyle factors and profile of studies among Lithuanian students. Medicina (Kaunas, Lithuania), 46(7), 482–9. https://doi.org/1007-08e [pii] [PubMed] [Google Scholar]
- Quick V, Byrd-Bredbenner C, White AA, Brown O, Colby S, Shoff S, … Greene G (2014). Eat, sleep, work, play: associations of weight status and health-related behaviors among young adult college students. Am J Health Promot, 29(2), e64–72. 10.4278/ajhp.130327-QUAN-130 [DOI] [PubMed] [Google Scholar]
- Taylor DJ, & Bramoweth AD (2010). Patterns and Consequences of Inadequate Sleep in College Students: Substance Use and Motor Vehicle Accidents. Journal of Adolescent Health, 46(6), 610–612. 10.1016/j.jadohealth.2009.12.010 [DOI] [PubMed] [Google Scholar]
- Terry PC, Lane AM, & Fogarty GJ (2003). Construct validity of the Profile of Mood States - Adolescents for use with adults. Psychology of Sport and Exercise, 4(2), 125–139. 10.1016/S1469-0292(01)00035-8 [DOI] [Google Scholar]
- Tsai LL, & Li SP (2004). Sleep patterns in college students: Gender and grade differences. Journal of Psychosomatic Research. 10.1016/S0022-3999(03)00507-5 [DOI] [PubMed] [Google Scholar]
- Tsui Y, & Wing Y (2009). A study on the sleep patterns and problems of university business students in Hong Kong. Journal of American College Health, 58(2), 167–176 10p. 10.1080/07448480903221418 [DOI] [PubMed] [Google Scholar]
- Van Reen E, Roane BM, Barker DH, McGeary JE, Borsari B, & Carskadon MA (2016). Current Alcohol Use is Associated with Sleep Patterns in First-Year College Students. Sleep, 39(6), 1321–1326. 10.5665/sleep.5862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veldi M, Aluoja A, & Vasar V (2005). Sleep quality and more common sleep-related problems in medical students. Sleep Medicine, 6(3), 269–275. 10.1016/j.sleep.2004.12.003 [DOI] [PubMed] [Google Scholar]
- Wallace DD, Boynton MH, & Lytle LA (2017). Multilevel analysis exploring the links between stress, depression, and sleep problems among two-year college students. Journal of American College Health, 65(3), 187–196. 10.1080/07448481.2016.1269111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X, Tao S, Zhang Y, Zhang S, & Tao F (2015). Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among Chinese college students. PLoS ONE, 10(3). 10.1371/journal.pone.0119607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wuyts J, De Valck E, Vandekerckhove M, Pattyn N, Bulckaert A, Berckmans D, … Cluydts R (2012). The influence of pre-sleep cognitive arousal on sleep onset processes. International Journal of Psychophysiology, 83(1), 8–15. 10.1016/j.ijpsycho.2011.09.016 [DOI] [PubMed] [Google Scholar]
- Zou G (2004). A Modified Poisson Regression Approach to Prospective Studies with Binary Data. American Journal of Epidemiology, 159(7), 702–706. 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]


