Abstract
Objective This research aims to study the effectiveness of platelet-rich plasma (PRP) in the treatment of patients with rotator cuff impingement syndrome compared with the treatment with subacromial injection of corticosteroids.
Methods This is a double-blind, randomized, comparative clinical trial. The patients were clinically evaluated with the use of the Disabilities of the Arm, Shoulder and Hand (DASH) outcome measure, University of California Los Angeles (UCLA) shoulder rating scale and Constant-Murley shoulder outcome score (CMS) on the day of application, and then again after 1, 3 and 6 months.
Results No statistically significant differences were found ( p < 0.05) when comparing the results of the DASH outcome measure, UCLA shoulder rating scale and CMS of the two groups at baseline and after 1, 3, and 6 months of treatment with subacromial injection. After the treatment, both groups showed a significant improvement in the DASH and UCLA scores ( p < 0.05) when compared with the baseline. However, the CMS at 6 months after treatment with steroids was lower than the baseline.
Concusions These findings suggest that PRP is a safe treatment and can be a useful tool in the therapeutic arsenal against of the rotator cuff diseases, for there was no significant difference between the subacromial use of PRP and corticosteroids.
Keywords: platelet-rich plasma, shoulder impingement syndrome, adrenal cortex hormones
Introduction
Due to the chronicity of the clinical manifestations of the rotator cuff impingement syndrome, there is a need to find new therapies that collaborate to improve pain management.
Platelet-rich plasma (PRP) is an evolving treatment modality that has been gaining prominence in primary care, rehabilitation and sports medicine. Platelet-rich plasma is a concentrated platelet solution prepared with autologous blood, which makes this treatment safe for clinical use. 1 Platelet-rich plasma acts by the modulation of bioactive factors in the injured region, increasing the regeneration potential. 2 It increases the production of type I collagen and the proliferation of tenocytes, transforming growth factor beta-1 (TGF-β1), platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF) and epidermal growth factor (EGF), while also stimulating the synthesis of ligament matrix. 3 4 5 6
Corticosteroid injections are commonly administered in tendinous lesions. 7 Subacromial application is considered a cheap and effective therapeutic option, but the side effects of corticosteroids cause concern in clinical practice. Tendinous ruptures following local injections of corticosteroids have also been found in the repetition of the treatment or even after single application. 8 In addition, other noninfectious complications may occur, including nerve atrophy, hypopigmentation of the skin, dystrophic calcification around the joint capsule, hyperglycemia and inhibition of the pituitary hypothalamic axis for 1 to 2 weeks after application. 9
The current literature regarding PRP, as this is a new modality of treatment, is limited due to the lack of standardization of study protocols, PRP preparation techniques and methods of measuring clinical improvement, so new research needs to be performed for the concrete understanding of this modality of therapy.
The aim of this study is to analyze the therapeutic efficacy of subacromial infiltration of PRP in patients with rotator cuff impingement syndrome compared with subacromial corticosteroid injection.
Methods
This clinical trial is a double-blind, randomized, controlled, interventional study of patients with rotator cuff impingement syndrome. The patients were randomized into blocks and assigned to receive treatment with PRP or to receive corticosteroid injection. The sample consisted of 51 patients, 25 in the corticoid group and 26 in the PRP group. The number of patients in the sample estimated to have a confidence interval of 95%, and power of 80% to detect a difference of 15 points in the DASH score, with a standard deviation (SD) of 10 was 20.4 for each group. To allow for a conservative withdraw of ∼ 20%, we recruited a total of 51 patients. No imputation protocol was implemented regarding sample loss. The block randomization was performed using the online engine sealedenvelope.com, which generated a list of patient admission number and corresponding treatment. The researcher responsible for patient admission was not aware of the randomization or group allocation, and the order of admission was followed thoroughly.
Platelet-rich plasma was obtained through 15 ml of the patient's peripheral blood that underwent a double centrifugation protocol (1,500 rpm for 6 minutes, then 3,500 rpm for 15 minutes in a Coleman 80–2C Macro Centrifuge) and manual platelet separation with micropipettes, including the buffy coat and then transferred to test tube for concentration. The outcome is ∼ 3 ml of PRP, transferred to syringe for injection. All materials used were sterile and disposable. The corticosteroid used was betamethasone dipropionate. To maintain the double-blind characteristic, peripheral blood was collected from all patients, and the nature of the treatment was hidden from both the patient and care provider. One of the researchers was responsible for patient allocation, preparation of the treatment and assuring double blindness. The injections were made in the subacromial space through a posterior approach after anesthesia with 1% lidocaine, and they were not guided by ultrasound. All participants were instructed to rest the injected shoulder for 24 h. No changes to medication or rehabilitation program were recommended.
To evaluate the therapeutic response, the tools used were: University of California Los Angeles (UCLA) shoulder rRating scale, Constant-Murley Shoulder Outcome Score (CMS), and The The Disabilities of the Arm, Shoulder and Hand (DASH) outcome measure. The patients were evaluated before the procedure, and at 1, 3, and 6 months after the intervention. All patients were informed regarding possible side-effects throughout the follow-up period.
The inclusion criteria used were: age between 18 and 70 years old, positive Neer impingement test; no previous treatment of intravenous (IV), injectable, or oral corticosteroids in the last 12 months; hemoglobin ˃11 g/dl; platelet count ˃150,000/mm 3 , and signature of the informed consent form. The exclusion criteria were: association with adhesive capsulitis, complete rupture of the rotator cuff in ultrasonography (all other forms of tendinopathy were included), and use of oral or parenteral corticosteroids during the study.
This research was fully conducted at the deCós Day Hospital, in Aracaju, Brazil. Patient recruiting and follow-up were conducted from October 2015 to July 2016 and ended after 6 months follow-up of the last recruited patient. The data were tabulated and analyzed in the Statistical Package for Social Sciences (SPSS), version 19.0 (IBM Corp., Armonk, NY, USA).
In this research, the confidentiality and privacy of the participating professionals were assured, ensuring that the information of the questionnaire was not used to the detriment of the people involved. All patients signed an informed consent form. This study was approved by the research ethics committee of Tiradentes University - CEP/UNIT (CAAE: 49144515.90000.5371) and is registered in The Brazilian Registry of Clinical Trials—ReBEC (UTN: U1111–1195–9769).
Results
The mean age of the patients in this sample was 53 years old. A total of 64% of the patients were female, with pain in the right shoulder (45%), weighing an average 72 kg and measuring 1.6 m, and with a body mass index (BMI) of 28 kg/m 2 . The epidemiological profile of the sample is characterized in Table 1 . Of the patients studied, only 40 returned for evaluation after 1 month of treatment (19 in the corticoid group and 21 in the PRP group); 27 completed 3 months of treatment (10 in the corticoid group and 17 in the PRP group), and 22 patients completed 6 months of treatment (10 in the corticoid group and 12 in the PRP group). No imputation protocol was implemented in this study, and all data acquired was utilized in data analysis.
Table 1. Epidemiological profile of patients with rotator cuff impact syndrome.
| Treatament received | ||||
|---|---|---|---|---|
| PRP | Corticoid | Total | p -value | |
| Age – n (%) | ||||
| < 35 years old | 1 (4) | 1 (4) | 2 (4) | 0.41 |
| 36–45 years old | 4 (15) | 4 (16) | 8 (16) | |
| 46–55 years old | 9 (35) | 8 (32) | 17 (33) | |
| 56–65 years old | 10 (38) | 6 (24) | 16 (31) | |
| > 65 years old | 2 (8) | 2 (8) | 4 (8) | |
| Not informed | 0 (0) | 4 (16) | 4 (8) | |
| Total | 26 (49) | 25 (51) | 51 (100) | |
| Mean ± SD | 53.2 ± 9,4 | 53 ± 11 | 53.1 ± 10 | |
| Gender – n (%) | ||||
| Male | 11 (42) | 7 (28) | 18 (36) | 0.433 |
| Female | 15 (57) | 18 (72) | 33 (64) | |
| Affected side – n (%) | ||||
| Right shoulder | 11 (44) | 21 (80) | 23 (45) | 0.015 |
| Left shoulder | 11 (44) | 5 (20) | 16 (31) | |
| Anthropometric data – Mean ± SD | ||||
| Height (m) | 1.6 ± 0.1 | 1.6 ± 0.1 | 1.6 ± 0.1 | 0.054 |
| Weight (Kg) | 72.2 ± 13.7 | 71.8 ± 16.3 | 72.0 ± 14.7 | 0.196 |
| BMI (Kg/m 2 ) | 28.4 ± 3.7 | 27.6 ± 5.0 | 28.0 ± 4.3 | 0.258 |
Abbreviations: BMI, body mass, index; PRP, platelet-rich plasma; SD, standard deviation.
The values obtained through the questionnaires at the time before the intervention and after 1, 3, and 6 months were compared between the groups using the independent Student t -test and the Mann-Whitney test, and are shown in Table 2 .
Table 2. Comparison of the efficacy of the treatment of rotator cuff tendinopathy—platelet-rich plasma versus corticoid.
| Tratament received | ||||
|---|---|---|---|---|
| PRP | Corticoid | CI 95% | p -score | |
| DASH outcome | ||||
| Admission | 53.3 | 54.5 | [-52.9; 21.35] | 0.135 |
| 1 month | 32.5 | 22.9 | [-37.01; -0.85] | 0.205 |
| 3 months | 23.5 | 20.2 | [-104.76; 44.08] | 0.235 |
| 6 months | 21.6 | 17.7 | [-14.14; 18.57] | 0.824 |
| UCLA shoulder rating scale | ||||
| Admission | 13.4 | 14.9 | [-3,.02; 6.19] | 0.926 |
| 1 month | 23 | 23.9 | [-4.45; 6.07] | 0.832 |
| 3 months | 29.3 | 29.6 | [-9.54; 10.16] | 0.898 |
| 6 months | 27 | 27.6 | [-8.53; 9.73] | 0.005 |
| Constant shoulder score | ||||
| Admission | 45.9 | 49.8 | [-5.04; 12.80] | 0.049 |
| 1 month | 55.4 | 58.8 | [-4.43; 11.12] | 0.503 |
| 3 months | 59.8 | 68 | [-5.39; 21.74] | 0.848 |
| 6 months | 62.9 | 56.9 | [-21.45; 9.42] | 0.228 |
Abbreviations: CI, confidence interval; DASH, Disabilities of the Arm, Shoulder and Hand; PRP, platelet-rich plasma; UCLA, University of California Los Angeles.
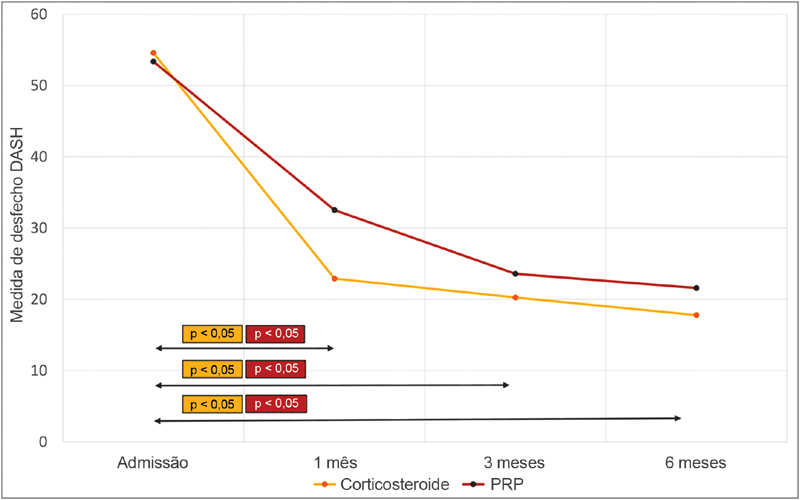
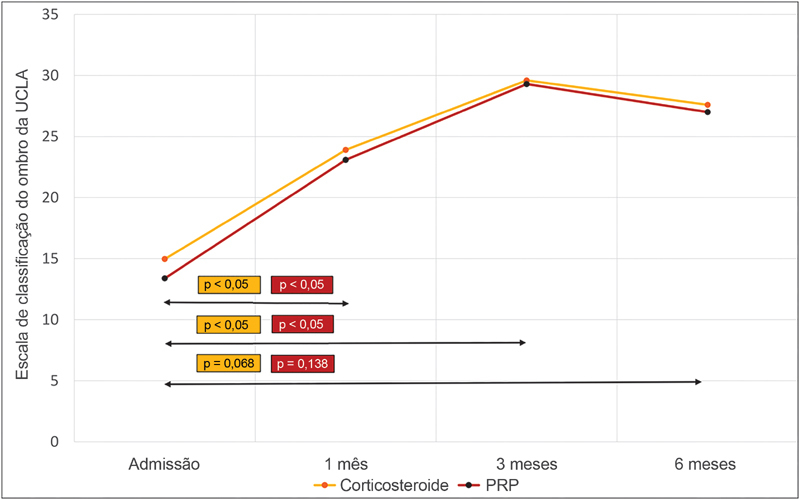
When comparing the results of the DASH outcome measure after 1, 3, and 6 months of treatment with the preintervention values, we identified a statistically significant difference ( p < 0.05) in both PRP and corticoid groups at all moments studied, as shown in Fig. 1 . Through the evaluation of the progression of the UCLA shoulder rating scale ( Fig. 2 ), we also identified that there were statistically significant differences ( p < 0.05) when comparing the scores at admission to the scores at 1 and 3 months of treatment in both groups.
Fig. 1.
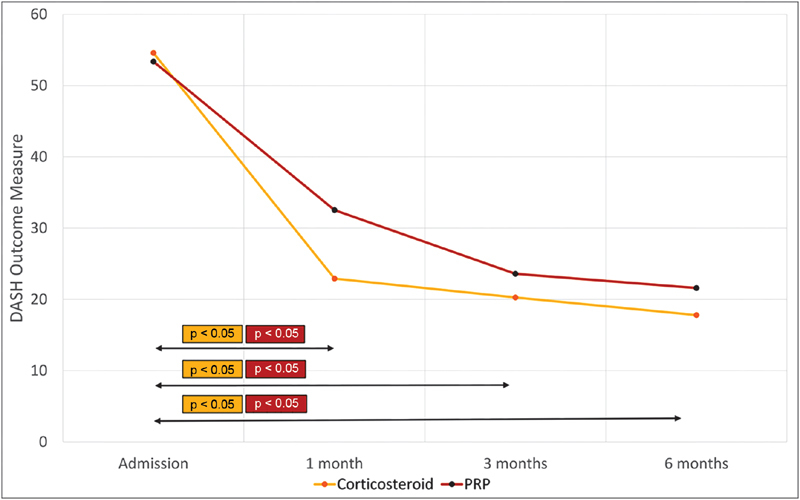
Evolution of the Disabilities of the Arm, Shoulder and Hand (DASH) score of patients with rotator cuff tendinopathy after 1, 3, and 6 months of treatment with corticosteroids and platelet-rich plasma. ( p -value shown represents statistical difference from that of admission). Abbreviations: DASH, Disabilities of the Arm, Shoulder and Hand; PRP, platelet-rich plasma.
Fig. 2.
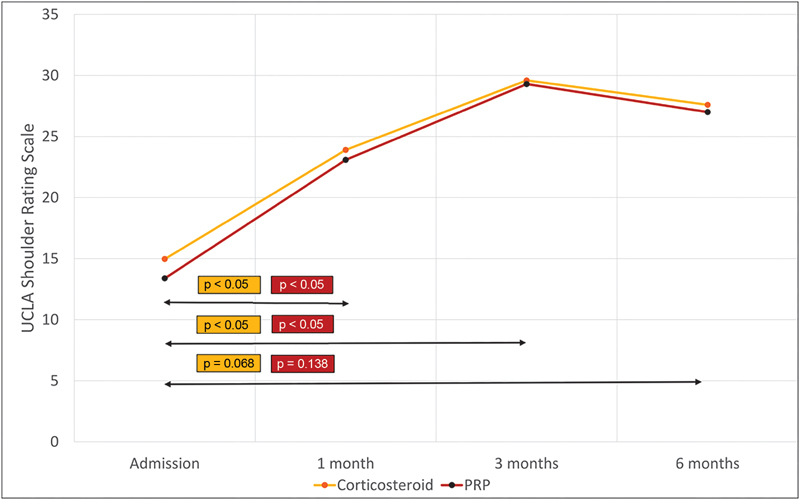
Evolution of the University of California Los Angeles UCLA shoulder rating scale of patients with rotator cuff tendinopathy after 1, 3, and 6 months of corticosteroids and platelet-rich plasma treatment. ( p -value shown represents statistical difference from that of admission). Abbreviations: UCLA, University of California Los Angeles; PRP, platelet-rich plasma.
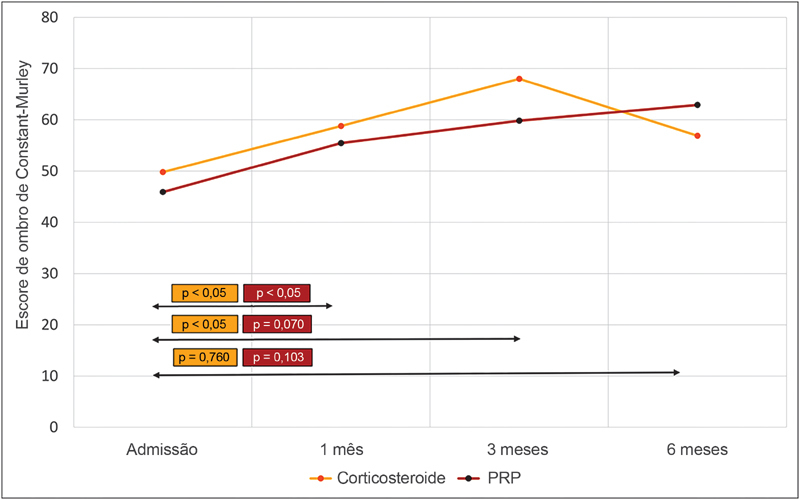
In the CMS, the difference between the values obtained during the follow-up of the PRP group was statistically significant after 1 month ( p < 0.05), but it was not statistically significant at 3 months ( p = 0.07) and at the 6 months' follow-up ( p = 0.103) in comparison to the score at admission, as shown in Fig. 3 . In the corticoid group, there was a statistically significant difference after 1 and 3 months of treatment ( p < 0.05). However, there was no statistically significant difference after 6 months ( p = 0.760) in comparison to the admission score. For statistical evaluation of progression among the treatment groups, the Student t -test with paired samples and the Wilcoxon test were applied.
Fig. 3.
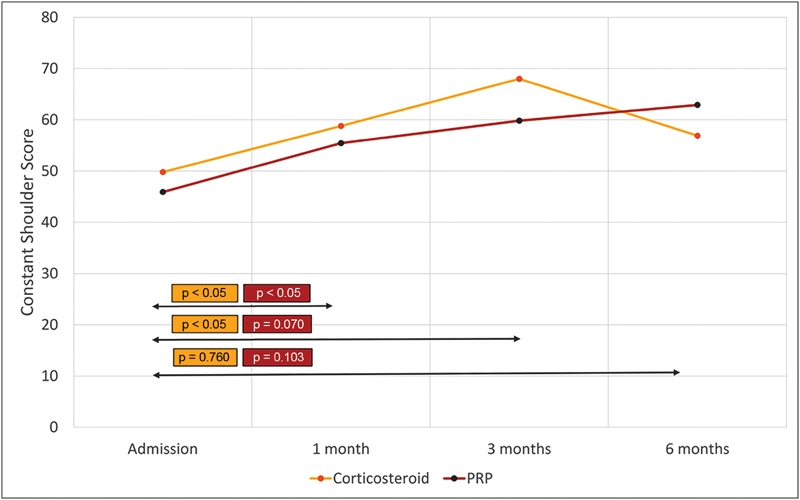
Evolution of the Constant-Murley shoulder outcome score (CMS)of patients with rotator cuff tendinopathy after 1, 3, and 6 months of corticosteroids and platelet-rich plasma treatment. ( p -value shown represents statistical difference from that of admission). Abbreviation: PRP, platelet-rich plasma.
Discussion
This randomized, controlled, double-blind, longitudinal study demonstrates the effects of treatment with a single infiltration of corticosteroids and PRP in the therapeutic process of rotator cuff tendinopathy.
In the present study, the patients who received PRP showed a mean difference of 20.8 points in the DASH score during the first month of follow-up, which already shows a significant improvement in pain and limb function in the short term (difference greater than 15 points). 10 On the other hand, the patients in the corticoid group had a mean difference of 31.6 points, which shows that both groups presented a significant reduction ( p < 0.05) of the short-term DASH score. The DASH scores remained significant in relation to admission even after 3 and 6 months of follow-up.
The group of patients that received corticosteroids, apparently, had a better response to pain and function at the 1 and 3 months follow-ups. At 6 months of follow-up, both groups presented similar results. Nevertheless, the differences presented between the groups at the 3 moments were not statistically significant ( p > 0.05). The positive and significant results in the DASH outcome measure symbolize that in both treatment modalities there was an improvement in the daily challenges associated with the painful shoulder in the patients' own perception, as well as a decrease in symptoms, and a lower influence of these symptoms on the psychosocial and occupational spheres.
The clinical improvement observed in the group that received PRP in this study was also observed by other authors. A longitudinal study 11 on the use of PRP in rotator cuff tendinopathy identified a gradual improvement in the visual analytical scale at 8 and 52 weeks of treatment. The authors used a different form of measurement of the therapeutic response, but noticed a gradual reduction of the symptoms, a finding also observed in the current research through the decreasing values in the DASH score.
The other scores used in this study showed similar results. The UCLA shoulder rating scale uses an association of subjective pain and function variables with objective variables of shoulder function to assess the therapeutic response after a procedure through pain, function, movement, strength, and patient satisfaction parameters. The therapeutic response was significant at 1 and 3 months of treatment ( p < 0.05), but the difference from the admission score was not significant at 6 months ( p = 0.138), which can be explained by the low number of participants who finished the study. One study 12 used intraoperative PRP in arthroscopic repairs of complete ruptures of the rotator cuff and found that PRP has positive results in the CMS and UCLA scores.
The CMS is a more objective questionnaire that measures the shoulder function through the range of motion and strength, with less relevance of the symptoms in the final score. The results of the CMS show that a measurable improvement in the shoulder function was only identified in the 1 st month after treatment with PRP up to 3 months after corticosteroid use, and, in the latter, there was a general worsening of function in relation to admission. When compared with the results found by another study 12 , the findings of the current study appear to be less significant, but this fact is probably associated with the association of surgical treatment with the PRP used by the authors. Platelet-rich plasma has been shown 13 to have improvement in several parameters of the CMS, including pain and range of motion up to 3 months after injection, showing similar results when compared with the present study.
A systematic review meta-analysis 14 has studied the efficacy of PRP on tendon and ligament healing using 37 articles. In this study, PRP groups showed significantly less pain in the long-term follow-up when compared with the control groups. This finding may correlate to the current study, when considering the long-term worsening found in the CMS in the corticoid group, while the PRP effects have shown more durability.
A prospective, randomized, controlled study 15 compared PRP and corticosteroid injection in 40 patients with partial rotator cuff tears. Both groups showed statistically significant better scores when compared with the baseline before injection. And when comparing the groups, the PRP group showed significantly better results at the 12 weeks evaluation, with no difference after 6 months.
In contrast, another comparative 16 study of the use of PRP and prednisone in the treatment of rotator cuff syndrome concluded that even though both treatments had positive results, their findings showed that patients who received corticoid had a significantly better clinical response than those who received PRP, both at 6 weeks and at 6 months. The present study agrees with both studies when showing positive results with both treatments; however, our findings agree with those of Shams et al when considering PRP equivalent or non-inferior when compared with corticosteroid injections. The present study concurs with the data found by Say et al regarding the short-term response, but disagrees with the long-term response, since the difference at 6 months between the two groups was not significant. This divergence has been prevalent in PRP literature, and these varying results may have been due to the different preparation protocols, the corticoid used, or the methodology of the study. New studies are still necessary for further understanding.
A randomized, double-blind, controlled clinical trial 17 was conducted with the use of PRP in the treatment of chronic tendinopathy of the rotator cuff. The authors found that there was no significant difference between the use of PRP and placebo in the Western Ontario Rotator Cuff (WORC) index, Shoulder Pain and Disability Index (SPADI) and visual analogue scale (VAS) scores throughout the study, concluding that PRP was no more effective than placebo in improving quality of life, pain, dysfunction, or range of motion. This study stands against the use of PRP to treat this condition, with a level 1 of evidence. This supports the hypothesis that corticosteroids may not have value in the long-term treatment of rotator cuff tendinopathies, since through the comparison performed in this study there was no significant difference between the therapeutic responses of corticosteroids and PRP. The authors also identified that there was a therapeutic improvement in the two groups studied, and hypothesized that improvement would also be observed if there was a group that was not submitted to any procedure, since just physical exercise is already associated with short and long term improvement of the rotator cuff tendinopathies. 18
The apparent improvement of patients that underwent subacromial infiltrations may also be associated with the dry needling performed to maintain the double-blind character of the investigations. 19 Authors identified an unexpected positive result in patients that received dry needling, which is explained as a stimulus to regeneration through extravasation of blood and subsequent local inflammatory reaction. Dry needling, although limited, is a mechanism that is similar to the use of PRP.
Despite the positive results with the subacromial use of corticosteroids, evidence in the literature does not value the use of this drug in rotator cuff diseases. A review 20 identifies two studies that favored the use of corticosteroids, two studies that did not observe a significant difference between corticoid and placebo, and a study favoring placebo results. In addition, there are studies 20 21 that have investigated the association of corticosteroids with NSAIDs compared with the use of NSAIDs alone, with no significant difference found between the two groups, suggesting that similar or better therapeutic responses can be achieved without exposing the patient to the possible side effects of corticosteroid injections.
Patients who underwent corticosteroid injections had to seek health services more frequently than patients who had only motor physical therapy during a 1 year follow-up due to persistence or relapse of symptoms, requiring new rounds of injections. 22 These findings are comparable to those encountered in the current study in the 6-month evaluation of the CMS and UCLA shoulder rating scale, since there was a decrease in these scores, symbolizing worsening of symptoms in relation to the previous evaluation and possibly indicating the need for new applications or other adjunctive therapy.
Due to its autologous characteristic, PRP is a safe treatment for clinical use. 1 The patients in the current study did not report any side effects during the whole follow-up period beyond the expected local pain up to 24 hours of the application, which is expected from the needle injection in the period after the end of the local anesthetic effect.
The limitations found in this study were: absence of a placebo group for comparison with the natural history of the disease, and the absence of complete 6-month follow-up of all patients in the sample. This work still opens the possibility of being optimized with protocols of PRP preparation, better concentrations and reproducibility. Current studies seem to indicate that multiple PRP applications may have value in increasing the clinical response to this treatment. The application of three doses of PRP has been shown to be significant in the treatment of early stages of osteoarthritis 23 and chronic patellar tendinopathy 24 , and this pattern can also be repeated for rotator cuff tendinopathies. In addition, PRP has been studied 25 to be used in conjunction with corticosteroid, as PRP does not affect the effects of dexamethasone on tenocytes and its antiinflammatory effect, showing that these treatments may have a synergic clinical response regarding pain and tissue regeneration.
The efficacy of PRP as a therapeutic modality still needs to be better clarified, but its characteristics make it a promising therapy in the treatment of rotator cuff tendinopathy. Corticosteroids, although well studied when their efficacy and side effects, remain rising concern in its chronic use in clinical practice.
Conclusion
This study concludes that subacromial injections of autologous PRP and corticosteroids have a positive and similar clinical response in the treatment of rotator cuff tendinopathies. When analyzing scores that consider the range of motion and strength, the patients only found significant results in the short term (1–3 months), and, in the corticosteroid group, functional worsening was observed at 6 months. These findings suggest that PRP is a safe treatment and may be a useful tool in the therapeutic arsenal against rotator cuff diseases, especially by avoiding possible adverse effects associated with the use of corticosteroids.
Conflitos de Interesse Os autores declaram não haver conflitos de interesse.
Trabalho feito no DeCós Day Hospital, Aracaju, SE, Brasil. Originalmente Publicado por Elsevier Editora Ltda.
Work performed at DeCós Day Hospital, Aracaju, SE, Brazil. Originally Published by Elsevier Editora Ltda.
Referências
- 1.Killian M L, Cavinatto L, Galatz L M, Thomopoulos S. Recent advances in shoulder research. Arthritis Res Ther. 2012;14(03):214. doi: 10.1186/ar3846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Molloy T, Wang Y, Murrell G. The roles of growth factors in tendon and ligament healing. Sports Med. 2003;33(05):381–394. doi: 10.2165/00007256-200333050-00004. [DOI] [PubMed] [Google Scholar]
- 3.Klein M B, Yalamanchi N, Pham H, Longaker M T, Chang J. Flexor tendon healing in vitro: effects of TGF-beta on tendon cell collagen production. J Hand Surg Am. 2002;27(04):615–620. doi: 10.1053/jhsu.2002.34004. [DOI] [PubMed] [Google Scholar]
- 4.Lynch S E, Nixon J C, Colvin R B, Antoniades H N. Role of platelet-derived growth factor in wound healing: synergistic effects with other growth factors. Proc Natl Acad Sci U S A. 1987;84(21):7696–7700. doi: 10.1073/pnas.84.21.7696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Varga J, Jimenez S A. Stimulation of normal human fibroblast collagen production and processing by transforming growth factor-beta. Biochem Biophys Res Commun. 1986;138(02):974–980. doi: 10.1016/s0006-291x(86)80591-5. [DOI] [PubMed] [Google Scholar]
- 6.Zhang F, Liu H, Stile F et al. Effect of vascular endothelial growth factor on rat Achilles tendon healing. Plast Reconstr Surg. 2003;112(06):1613–1619. doi: 10.1097/01.PRS.0000086772.72535.A4. [DOI] [PubMed] [Google Scholar]
- 7.Rees J D, Wilson A M, Wolman R L. Current concepts in the management of tendon disorders. Rheumatology (Oxford) 2006;45(05):508–521. doi: 10.1093/rheumatology/kel046. [DOI] [PubMed] [Google Scholar]
- 8.Kleinman M, Gross A E. Achilles tendon rupture following steroid injection. Report of three cases. J Bone Joint Surg Am. 1983;65(09):1345–1347. [PubMed] [Google Scholar]
- 9.Roberts W N., JrJoint aspiration or injection in adults: Technique and indicationsIn: UpToDate, Post TW, edotors, UpToDate, Waltham, MA. (acessado em: 21 de out. 2016).
- 10.Beaton D E, Davis A M, Hudak P, McConnell S. The DASH (Disabilities of the Arm, Shoulder and Hand) outcome measure: What do we know about it now? Br J Hand Ther. 2001;6(04):109–118. [Google Scholar]
- 11.Scarpone M, Rabago D, Snell E et al. Effectiveness of platelet-rich plasma injection for rotator cuff tendinopathy: a prospective open-label study. Glob Adv Health Med. 2013;2(02):26–31. doi: 10.7453/gahmj.2012.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malavolta E A, Gracitelli M E, Sunada E E et al. Platelet-rich plasma in arthroscopic repairs of complete tears of the rotator cuff. Rev Bras Ortop. 2015;47(06):741–747. doi: 10.1016/S2255-4971(15)30032-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tahririan M A, Moezi M, Motififard M, Nemati M, Nemati A.Ultrasound guided platelet-rich plasma injection for the treatment of rotator cuff tendinopathyAdv Biomed Res [Internet]. 27 de dezembro de 2016. Disponível em:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5220679/ [DOI] [PMC free article] [PubMed]
- 14.Chen X, Jones I A, Park C, Vangsness C T.The Efficacy of Platelet-Rich Plasma on Tendon and Ligament Healing: A Systematic Review and Meta-analysis With Bias AssessmentAm J Sports Med. 1o de dezembro de 2017;363546517743746. [DOI] [PMC free article] [PubMed]
- 15.Shams A, El-Sayed M, Gamal O, Ewes W. Subacromial injection of autologous platelet-rich plasma versus corticosteroid for the treatment of symptomatic partial rotator cuff tears. Eur J Orthop Surg Traumatol. 2016;26(08):837–842. doi: 10.1007/s00590-016-1826-3. [DOI] [PubMed] [Google Scholar]
- 16.Say F, Gurler D, Bulbul M. Platelet-rich plasma versus steroid injection for subacromial impingement syndrome. J Orthop Surg (Hong Kong) 2016;24(01):62–66. doi: 10.1177/230949901602400115. [DOI] [PubMed] [Google Scholar]
- 17.Kesikburun S, Tan A K, Yilmaz B, Yaşar E, Yazicioğlu K. Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: a randomized controlled trial with 1-year follow-up. Am J Sports Med. 2013;41(11):2609–2616. doi: 10.1177/0363546513496542. [DOI] [PubMed] [Google Scholar]
- 18.Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003;(02):CD004258. doi: 10.1002/14651858.CD004258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rha D W, Park G-Y, Kim Y-K, Kim M T, Lee S C. Comparison of the therapeutic effects of ultrasound-guided platelet-rich plasma injection and dry needling in rotator cuff disease: a randomized controlled trial. Clin Rehabil. 2013;27(02):113–122. doi: 10.1177/0269215512448388. [DOI] [PubMed] [Google Scholar]
- 20.Buchbinder R, Green S, Youd J M. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev. 2003;(01):CD004016. doi: 10.1002/14651858.CD004016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Min K S, St Pierre P, Ryan P M, Marchant B G, Wilson C J, Arrington E D. A double-blind randomized controlled trial comparing the effects of subacromial injection with corticosteroid versus NSAID in patients with shoulder impingement syndrome. J Shoulder Elbow Surg. 2013;22(05):595–601. doi: 10.1016/j.jse.2012.08.026. [DOI] [PubMed] [Google Scholar]
- 22.Rhon D I, Boyles R B, Cleland J A. One-year outcome of subacromial corticosteroid injection compared with manual physical therapy for the management of the unilateral shoulder impingement syndrome: a pragmatic randomized trial. Ann Intern Med. 2014;161(03):161–169. doi: 10.7326/M13-2199. [DOI] [PubMed] [Google Scholar]
- 23.Görmeli G, Görmeli C A, Ataoglu B, Çolak C, Aslantürk O, Ertem K. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(03):958–965. doi: 10.1007/s00167-015-3705-6. [DOI] [PubMed] [Google Scholar]
- 24.Charousset C, Zaoui A, Bellaiche L, Bouyer B. Are multiple platelet-rich plasma injections useful for treatment of chronic patellar tendinopathy in athletes? a prospective study. Am J Sports Med. 2014;42(04):906–911. doi: 10.1177/0363546513519964. [DOI] [PubMed] [Google Scholar]
- 25.Jo C H, Lee S Y, Yoon K S, Shin S. Effects of Platelet-Rich Plasma With Concomitant Use of a Corticosteroid on Tenocytes From Degenerative Rotator Cuff Tears in Interleukin 1β-Induced Tendinopathic Conditions. Am J Sports Med. 2017;45(05):1141–1150. doi: 10.1177/0363546516681294. [DOI] [PubMed] [Google Scholar]